Chapter 29 Dysrhythmias and Tachyarrhythmias
5 What should you think of when you see a very wide QRS (and no P waves)?
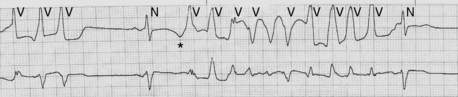
Hyperkalemia leads to baseline depolarization of cardiac cell membranes. This in turn results in an increased proportion of inactivated sodium channels. The global consequence of increased inactivation is decreased conduction velocity. In the atria this creates long low-amplitude P waves (which can be difficult to see), and in the ventricle it creates a very wide QRS. With sufficient hyperkalemia a sine wave–appearing rhythm can result. If the underlying rhythm is fast (e.g., sinus tachycardia) the wide QRS and apparent lack of P waves can be mistaken for VT. It is critical not to give sodium channel blocking antiarrhythmics (e.g., lidocaine) in this setting because they further increase sodium channel inactivation and can result in asystole and death. Treatment should be aimed at stabilizing the cell membrane (calcium) and reducing potassium (insulin, glucose, Kayexalate, and/or dialysis). See Figure 29-1.
6 What is torsades de pointes, and what predisposes a patient to it?
 Constellation of one long QT interval (QTc > 440 ms in men and > 460 ms in women)
Constellation of one long QT interval (QTc > 440 ms in men and > 460 ms in women)
 Initiation with a long-short interval (tachycardia begins after a pause [long cycle])
Initiation with a long-short interval (tachycardia begins after a pause [long cycle])
 Premature ventricular contraction that begins during the T wave (short cycle)
Premature ventricular contraction that begins during the T wave (short cycle)
Long QT (and torsade) can result from a congenital ion channel abnormality or ion channel blocking medication (see Fig. 29-2) and can be exacerbated by hypomagnesemia, hypokalemia, and hypocalcemia.
7 What drugs commonly used in the ICU can cause QT prolongation?
See Box 29-1. See also www.torsades.org.
Box 29-1 Drugs Commonly Used in the ICU that Can Cause QT Prolongation
| Amiodarone | Quinidine |
| Clarithromycin | Sotalol |
| Amitriptyline | Moxifloxacin |
| Haloperidol | Lithium |
| Methadone | Risperidone |
11 What is the main effect of adenosine on cardiac conduction?
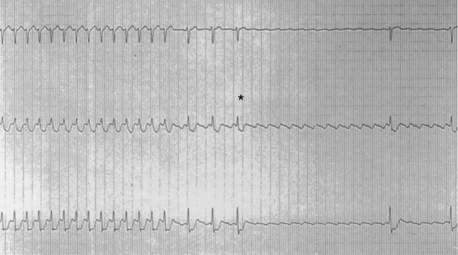
Adenosine’s main clinically relevant effect on cardiac conduction is transient AV nodal block. As such it can be used in the diagnosis of various narrow complex tachycardias where the P waves are difficult to discern on the surface ECG. A bolus of adenosine produces rapid-onset, short-duration AV block. This can result in unmasking of P waves previously obscured by the QRST complex. In AV node–dependent rhythms (such as AVRT and AVNRT [described later]) adenosine will cause termination of tachycardia. Thus adenosine injection can be a diagnostic and therapeutic maneuver. Termination of a narrow complex tachycardia by adenosine strongly suggests an AV node–dependent rhythm but rarely can indicate adenosine-sensitive focal atrial tachycardias. It is important always to have a 12-lead ECG running when giving adenosine. See Figure 29-3.
13 How do you treat hemodynamically stable tachycardias?
There are two issues to consider when identifying arrhythmias:
14 What drugs can be used to control ventricular response rate in a patient with hypotension and atrial fibrillation?
16 Who needs anticoagulation?
In patients with new-onset AF of less than 48 hours duration the need for anticoagulation before and after cardioversion may be based on the patient’s long-term risk for thromboembolism (see Table 29-1). For patients with AF of more than 48 hours duration anticoagulation should be initiated before cardioversion (for at least 3 weeks if possible or IV heparin if requiring immediate cardioversion for hemodynamic instability) and continued for 4 weeks. The decision for long-term anticoagulation is based on the CHA2DS2-VASc score. Patients with a score of 1 can receive either aspirin or full anticoagulation; patients with a score of 2 or more should receive long-term anticoagulation.
| Risk factor | Score |
|---|---|
| Congestive heart failure/LV dysfunction | 1 |
| Hypertension | 1 |
| Age > 75 y | 2 |
| Diabetes mellitus | 1 |
| Stroke/TIA/TE | 2 |
| Vascular disease (prior myocardial infarction, peripheral artery disease, aortic plaque) | 1 |
| Age 65-74 y | 1 |
| Sex category (i.e., female gender) | 1 |
LV, Left ventricular; TE, thromboembolism; TIA, transient ischemic attack.
From Lip GY, Nieuwlaat R, Pisters R, et al: Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach—The Euro Heart Survey on Atrial Fibrillation. Chest 137:263-272, 2010.
21 How do you describe the different degrees of AV block?
 First-degree heart block: conduction delay with PR interval > 200 ms. First-degree AV block is therefore a misnomer, and electrophysiology purists will use the term first-degree AV delay.
First-degree heart block: conduction delay with PR interval > 200 ms. First-degree AV block is therefore a misnomer, and electrophysiology purists will use the term first-degree AV delay.
 Second-degree heart block: periodic interruptions of AV conduction, leading to nonconducted beats. Second-degree heart block is divided into Mobitz type I (Wenckebach: progressive PR prolongation followed by a nonconducted beat) and Mobitz type II (intermittent nonconducted beats with a fixed PR interval that is typically not prolonged).
Second-degree heart block: periodic interruptions of AV conduction, leading to nonconducted beats. Second-degree heart block is divided into Mobitz type I (Wenckebach: progressive PR prolongation followed by a nonconducted beat) and Mobitz type II (intermittent nonconducted beats with a fixed PR interval that is typically not prolonged).
 Third-degree heart block: complete interruption of AV conduction, with AV dissociation (if there are ventricular escape beats) or ventricular asystole.
Third-degree heart block: complete interruption of AV conduction, with AV dissociation (if there are ventricular escape beats) or ventricular asystole.