CHAPTER 25 Dural Sinus Invasion in Meningiomas and Repair 
INTRODUCTION
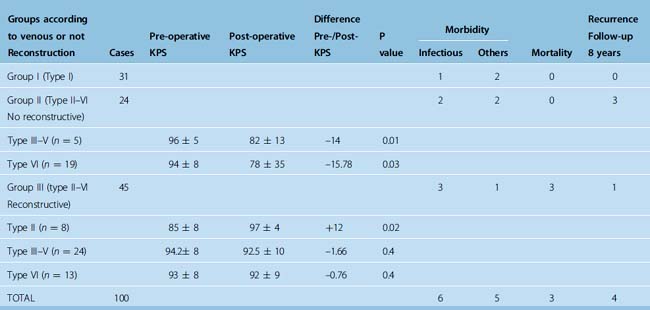
Surgery of meningiomas involving the major dural sinuses leaves the surgeon confronted with a difficult dilemma: leave the fragment invading the sinus in place and have a higher risk of recurrence, or attempt a total removal and expose the patient to a greater operative danger. The controversy of what constitutes the best treatment is still in debate.1 Some claim that leaving the intraluminal fragment in place is the best treatment, and others that attempt at total gross removal with venous reconstruction is preferable. The latter is our preference, based on a 20-year experience corresponding to a series of 100 meningiomas that were studied and then reported in 2006.2 The effects, in terms of recurrence rate and morbidity and mortality, of attempting complete removal including the invaded portion of the dural sinus, and in addition the consequences of restoring or not the venous circulation were studied. Our series consisted of 100 consecutive patients who underwent surgery between January 1980 and January 2001 (Table 25-1). Meningiomas originated at the superior sagittal sinus in 92 of the cases (28 in the anterior, 48 in the middle and 16 in the posterior third), the transverse sinus in 5, and the confluence of sinus in 3. A simplified classification scheme based on the degree of dural sinus involvement was applied:
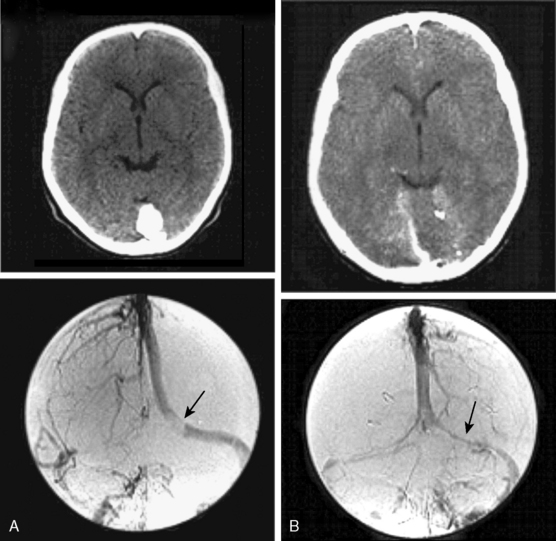
Gross tumor removal was achieved in 93% of the cases and reconstruction of the sinus was attempted in 45 (65%) of the 69 cases with wall and lumen invasion. The overall recurrence rate in the study was 4%, with a follow-up ranging from 3 to 23 years (mean 8 years). The mortality rate was 3%, all cases due to brain swelling after en bloc resection of a type VI meningioma without venous restoration. Eight patients who harbored a lesion in the middle third portion of the superior sagittal sinus had permanent neurologic aggravation, likely due to local venous infarction. Six of these patients had not undergone a venous repair procedure. Venous reconstruction did not increase the morbidity–mortality rate in our series. From this study we concluded the following: (1) the relatively low recurrence (4%) favors attempts at complete removal, including the portion invading the sinus; (2) because the subgroup of patients without venous reconstruction displayed statistically significant clinical deterioration after surgery compared with the other subgroups (P = 0.02), venous flow restoration seems justified when not too risky.2
CLASSIFICATION OF SINUS INVASION
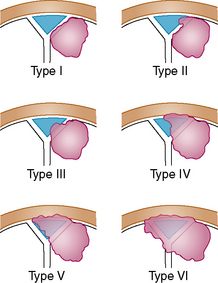
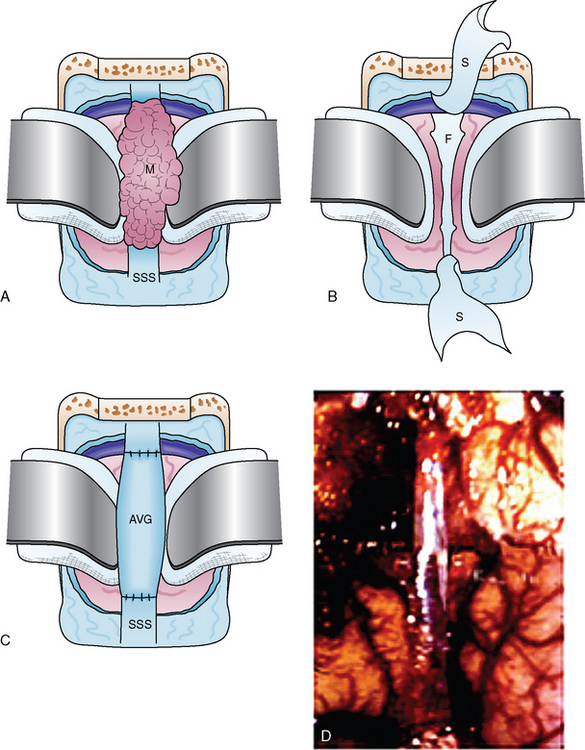
Different classifications of sinus invasion have been proposed by different authors, especially Krause (quoted by Merrem3) and Bonnal and Brotchi.4–7 For surgical purpose, we developed a simplified classification that we believe is easy to remember. This classification, developed for the sagittal sinus location shown in Figure 25-1, may also be applied to meningiomas involving the torcular and the transverse sinus.2
PREOPERATIVE INVESTIGATIONS
Selective bilateral internal and external carotid subtraction angiographies as well as vertebral angiography serve to determine the dural and cortical–pial supply ipsilateral or contralateral to the tumor. The arterial phase is useful to predict the difficulty of dissection of the capsule from the cortex. As we have shown in prior publications, dissection entails neurologic risk when a pial vascular supply is identified.8 When meningeal supply is important, preoperative embolization may be of some value in producing tumor necrosis and decreasing the operative risks to the patient by diminishing the blood loss that accompanies resection of these tumors.
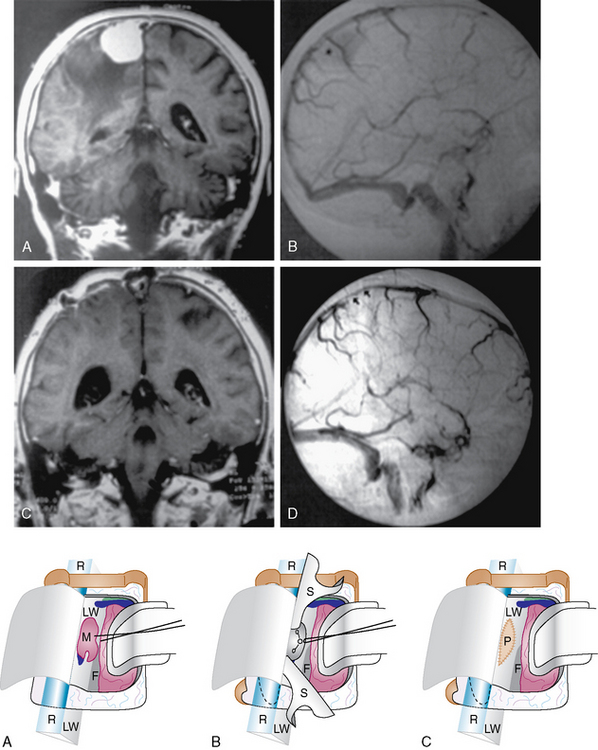
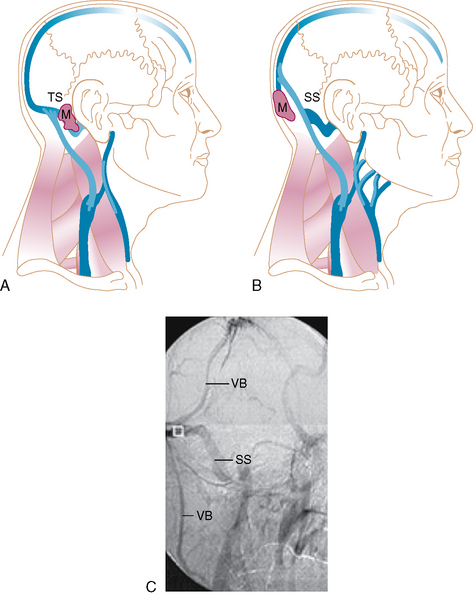
The late venous phases with bilateral filling of the sagittal sinus are required for the exact evaluation of sinus patency and collateral venous pathways. Oblique views can depict the superior sagittal sinus (SSS) throughout its entire course. Various degrees of sinus occlusion can be observed from simple compression with narrowing of the sinus lumen to intraluminal defect to total occlusion. Complete occlusion may be assumed from no visualization of segments of the sinus and from collateral venous channel development. The pattern of venous drainage and venous collateral channels must be established preoperatively to determine the surgical approach (Fig. 25-2).
SURGICAL TECHNIQUE
General Principles
Exposure and initial steps
Sinus surgery procedure
Postoperative care
Surgery of the Dural Sinus, According to the Degree of Invasion
CONSIDERATIONS FROM THE LITERATURE REVIEW
Surgical Venous Damage
Avoiding the interruption of a partially occluded sagittal sinus is a matter of strong consensus. The safety of resecting a totally occluded portion of a sinus, although classically accepted, is disputable; brain swelling, venous infarction, and cerebrospinal fluid (CSF) collection may occur when venous collateral circulation is impaired. In Hoessly and Olivecrona’s series,9 which included 196 parasagittal meningiomas, treated without venous reconstruction, morbidity amounted to 12.3%, with half of the cases involving venous damages. Their 10% mortality corresponded to 14 (12.8%) of the 109 tumors located in the middle, 3 (9.7%) of the 31 lesions in the posterior third, and 3 (5.3%) of the 56 lesions in the anterior third. In Bonnal and Brotchi’s study including 21 cases, one patient (4.8%) died after an en bloc resection of the tumor mass without venous restoration.5 In a recent article documenting the cooperative experience of 8 surgeons and the grouping of 108 cases, Di Meco and colleagues mentioned the occurrence of severe brain swelling in 3 (10%) of the cases treated with en bloc resection without venous reconstruction. Also, persistent subgaleal fluid collection likely corresponding to a default in CSF reabsorption and/or persistent postoperative high intracranial pressure from venous origin was observed in 11 of their patients (10%).10 In our series, morbidity and mortality related to venous damage and/or absence of venous flow reconstruction were estimated at 8% and 3%, respectively. Perhaps these patients would have had a better outcome if they had undergone venous repair, or perhaps shaving of the tumor outside the sinus with secondary stereotactic radiation would have been harmless, but we do not know the answer.
Dural Sinus Reconstruction
Reconstructions in the venous system are not new. Different techniques of dural sinus repair were reported long ago,11–33 and encouraging results of anastomosing cortical veins to the sinus venous graft have been reported more recently.34–38
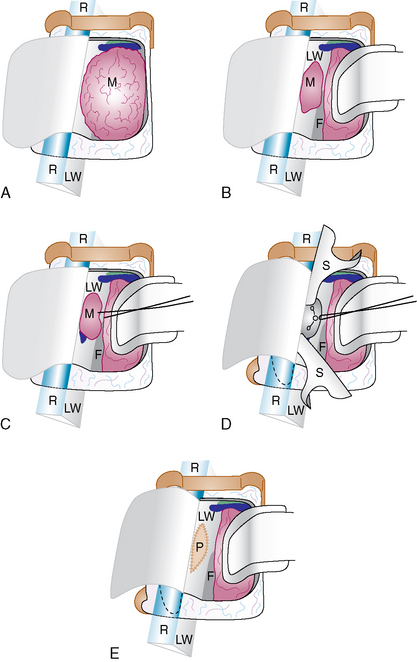
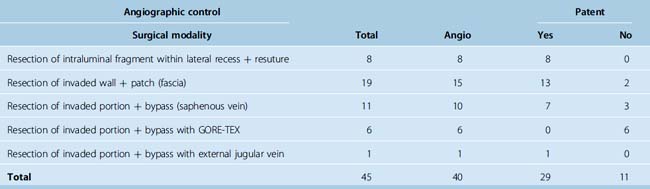
First Bonnal and Brotchi5 and then Hakuba and colleagues,13–16 Bederson and colleagues,11 Sekhar and associates,37 Steiger and colleagues,38 and Schmid-Elsaesser and colleagues39 reported satisfactory experiences patching with pieces of dura or autologous venous graft. In our series 13 (86.6%) of the 15 repairs with dura or fascia, confirmed angiographically, were patent.2 Harvesting autologous veins, theoretically the best material for patching the venous system, seemed too excessive for patching. According to our experience, the most appropriate material is the thin and glossy fascia temporalis. For performing bypasses, the internal saphenous vein for a long graft and the external jugular vein for a short graft were used in 12 patients. Eight (72.7%) of the 11 angiographically controlled bypasses were patent (Table 25-2; Fig. 25-6).
[1] Auque J. Le sacrifice veineux en neurochirurgie. Evaluation et gestion du risque. Neurochirurgie. 42(Suppl. 1), 1996.
[2] Sindou M., Alvernia J.E. Results of attempted radical tumor removal and venous repair in 100 consecutive meningiomas involving the major dural sinuses. J Neurosurg. 2006;105(4):514-525.
[3] Merrem G. [Parasaggital meningiomas. Fedor Krause memorial lecture]. Acta Neurochir (Wien). 1970;23(2):203-216.
[4] Bonnal J. La chirurgie conservatrice et réparatrice du sinus longitudinal supérieure. Neurochirurgie. 2001;28:147-172.
[5] Bonnal J., Brotchi J. Surgery of the superior sagittal sinus in parasagittal meningiomas. J Neurosurg. 1978;48:935-945.
[6] Bonnal J., Brotchi J., Stevenaert A., et al. Excision of the intrasinusal portion of rolandic parasaggital meningiomas, followed by plastic surgery of the superior of the superior longitudinal sinus. Neurochirurgie. 1971;17:341-354.
[7] Bonnal J., Buduba C. Surgery of the central third of the superior sagittal sinus. Experimental study. Acta Neurochir (Wien). 1974;30:207-215.
[8] Alvernia J.E., Sindou M. Preoperative neuroimaging findings as a predictor of the surgical plane of cleavage: prospective study of 100 consecutive cases of intracranial meningioma. J Neurosurg. 2004;100:422-430.
[9] Hoessly G.F., Olivecrona H. Report on 280 cases of verified parasagittal meningioma. J Neurosurg. 1955;12:614-625.
[10] Di Meco F., Li K.W., Casali C., et al. Meningiomas invading the superior sagittal sinus: Surgical experience in 108 cases. Neurosurgery. 2004;55(6):1263-1274.
[11] Bederson J.B., Eisenberg M.B. Resection and replacement of the superior sagittal sinus for treatment of a parasagittal meningioma: technical case report. Neurosurgery. 1995;37:1015-1018.
[12] Donaghy R.M.P., Wallman L.J., Flanagan M.J., Numoto M. Sagittal sinus repair. Technical note. J Neurosurg. 1973;38:244-248.
[13] Hakuba A. Surgery of the intracranial venous system. Heidelberg: Springer-Verlag, 1996.
[14] Hakuba A., Huh C.W., Tsujikawa S., Nishimura S. Total removal of a parasagittal meningioma of the posterior third of the sagittal sinus and its repair by autogenous vein graft. Case report. J Neurosurg. 1979;51:379-382.
[15] Hakuba A. Reconstruction of dural sinus involved in meningiomas. In: Al Mefty O., editor. Meningiomas. New York: Raven Press; 1991:371-382.
[16] Hakuba A., Tsurund T., Ohata K., et al. Microsurgical reconstruction of the intracranial venous system. In: Hakuba A., editor. Surgery of the Intracranial Venous System. Heidelberg: Springer-Verlag; 1996:220-225.
[17] Kang J.K., Jun S.S., Sung W.H., et al. Surgical management of meningioma involving the superior sagittal sinus. In: Hakuba A., editor. Surgery of the intracranial venous system. Heidelberg: Springer-Verlag; 1996:252-259.
[18] Kapp J.P., Gielchinsky I., Petty C., Mc Clure C. An internal shunt for use in the reconstruction of dural venous sinuses. Technical note. J Neurosurg. 1971;35:351-354.
[19] Kapp J.P., Gielchinsky I., Deardourff S.L. Operative techniques for management of lesions involving the dural venous sinuses. Surg Neurol. 1977:339-342.
[20] Logue V. Parasagittal meningiomas. In: Krayenbühl, editor. Advances and Technical Standards in Neurosurgery. Wien: Springer-Verlag; 1975:171-198.
[21] Masuzawa H. [Superior sagittal sinus plasty using flax flap in parasagittal meningioma (author’s transl)]. No Shinkei Geka. 1977;5:707-713.
[22] Meirowsky A.M. Wounds of the dural sinuses. J Neurosurg. 1953;10:496-514.
[23] Nagashima H., Kobayashi S., Takemae T., Tanaka Y. Total resection of torcular herophili hemangiopericytoma with radial artery graft: case report. Neurosurgery. 1995;36:1024-1027.
[24] Sekhar L.N., Tzortzidis F.N., Bejjani G.K., Schessel D.A. Saphenous vein graft bypass of the sigmoid sinus and jugular bulb during the removal of glomus jugular tumors. Report of two cases. J Neurosurg. 1997;86:1036-1041.
[25] Sindou M. Meningiomas invading the sagittal or transverse sinuses, resection with venous reconstruction. J Clin Neurosci. 2001;8(Suppl. 1):8-11.
[26] Sindou M., Alaywan F., Hallacq P. Chirurgie des grands sinus veineux duraux intracrâniens. Neurochirurgie. 1996;Suppl. 1:45-87..
[27] Sindou M.A. The intracranial venous system as a neurosurgeon’s perspective. Adv Tech Stand Neurosurg. 2000;26:131-216.
[28] Sindou M., Hallacq P. Microsurgery of the venous system in meningiomas invading the major dural sinuses. In: Hakuba A., editor. Surgery of the intracranial venous system. Heidelberg: Springer-Verlag; 1996:226-236.
[29] Sindou M., Hallacq P. Venous reconstruction in surgery of meningiomas invading invading the sagittal and transverse sinuses. Skull Base Surg. 1998;8:57-64.
[30] Sindou M., Hallacq P., Ojemann R.G., Laws E.R. Aggressive (Sindou, Hallacq) vs Conservative (Ojemann, Laws) treatment of parasagittal meningiomas involving the superior sagittal sinus. In: Al Mefty O., Origitano T.C., Harkey H.L., editors. Controversies in neurosurgery. New York: Thieme; 1996:80-89.
[31] Sindou M., Mazoyer J.F., Fischer G., et al. Experimental bypass for sagittal sinus repair. Preliminary report. J Neurosurg. 1976;44:325-330.
[32] Sindou M., Mazoyer J.F., Pialat J., et al. [Experimental intracranial venous microsurgery. Bypass of the sagittal sinus for arterial or venous repair and preoperative measurement of the cerebral impedance in the dog]. Neurochirurgie. 1975;21:177-189.
[33] Sindou M., Mercier P., Bokor J., Brunon J. Bilateral thrombosis of the transverse sinuses: microsurgical revascularization with venous bypass. Surg Neurol. 1980;13:215-220.
[34] Menousky T., De Vries J. Cortical vein end-to-end anastomosis after removal of a parasagittal meningioma. Microsurgery. 2002;22:27-29.
[35] Murata J., Sawamura Y., Saito H., Abe H. Resection of a recurrent parasagittal meningioma with cortical vein anastomosis: technical note. Surg Neurol. 1997;48:592-595.
[36] Sakaki T., Morimoto T., Takemura K., Miyamoto S., Kyoi S., Utsumi S. Reconstruction of cerebral cortical veins using silicone tubing. J Neurosurg. 1987;66:471-473.
[37] Sekhar L.N. The exposure, preservation and reconstruction of cerebral arteries and veins during the resection of cranial base tumors. In: Sekhar L.N., Schmamm V.L., editors. Tumors of the cranial base: diagnosis and treatment. Futura: Mount Kisko, NY; 1987:213-226.
[38] Steiger H.J., Reulen H.J., Huber P., Boll J. Radical resection of superior sagittal sinus meningioma with venous interposition graft and reimplantation of the rolandic veins. Acta Neurochir (Wien). 1989;100:108-111.
[39] Schmid-Elsaesser R., Steiger H.J., Yousry T., et al. Radical resection of meningiomas and arteriovenous fistulas involving critical dural sinus segments: experience with intraoperative sinus pressure monitoring and elective sinus reconstruction in 10 patients. Neurosurgery. 1997;41:1005-1018.