Chapter 16 Drugs to Treat Asthma and Chronic Obstructive Pulmonary Disease
| Abbreviations | |
|---|---|
| ACh | Acetylcholine |
| BLT | Leukotriene B receptor |
| cAMP | Cyclic adenosine monophosphate |
| CNS | Central nervous system |
| COPD | Chronic obstructive pulmonary disease |
| CysLT | Cys-leukotriene |
| Epi | Epinephrine |
| FEV1 | Forced expiratory volume in 1 second (liters) |
| GCs | Glucocorticoids |
| GI | Gastrointestinal |
| IgE | Immunoglobulin type E |
| IL | Interleukin |
| IV | Intravenous |
| LOX | Lipoxygenase |
| LTs | Leukotrienes |
| LTMs | Leukotriene modulators |
| MDI | Metered-dose inhaler |
| PDE | Phosphodiesterase |
| PEF | Peak expiratory flow |
| TNF | Tumor necrosis factor |
Therapeutic Overview
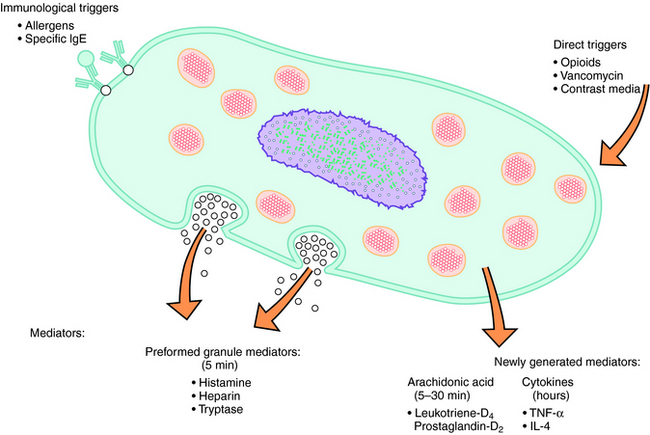
Normal bronchial smooth muscle tone is controlled by vagal innervation (see Chapter 9). Cholinergic activity or sensitivity is often increased in asthmatics, and increased cholinergic tone is the primary reversible component of COPD. However, most patients with asthma also have increased adrenergic activity (see Chapter 11), which manifests as increased wheezing if patients are treated with β adrenergic receptor blocking drugs (e.g., propranolol), which are contraindicated in asthma. A variety of agents can contribute to the inflammation of asthma; however, immediate hypersensitivity to common allergens is the most common cause. It is estimated that 80% of children and 50% of adults with asthma are allergic. The common allergens include seasonal outdoor allergens (e.g., ragweed pollen, grass pollen, and mold) or the year-round indoor allergens (dust mites, cockroaches, and domestic animal dander). Allergens cause release of the preformed granule mediator histamine, which can trigger bronchospasm. However, antihistamines (H1 receptor antagonists) are relatively ineffective in the treatment of asthma, demonstrating that other factors are key mediators of the asthma attack. In patients with asthma, in addition to the release of prestored mediators such as histamine from mast cells, other inflammatory mediators are synthesized and released including arachidonic acid, its metabolites, and several cytokines (Fig. 16-1). Leukotrienes (LTs), primarily LTD4, are implicated as major mediators of bronchoconstriction. Agents that inhibit the synthesis or action of the LTs, known as leukotriene modulators (LTMs), are useful for the treatment of asthma.
Asthma is treated using three main approaches. The first is avoidance of the causative factors, when possible, particularly for patients sensitive to indoor allergens. The second is the use of antiinflammatory drugs, including cromolyn and related agents, glucocorticoids (GCs) (see Chapter 39), and LTMs. If used regularly, these drugs can reduce the signs and symptoms of bronchial hyperactivity, characteristic of asthma. Third, drugs that can reverse or inhibit the development of bronchoconstriction are important; these compounds include methylxanthines, epinephrine (Epi) and selective adrenergic β2 receptor agonists (see Chapter 11), and the muscarinic receptor antagonists (see Chapter 10).
| Therapeutic Overview |
|---|
| Antiinflammatory Agents |
| Cromolyn and related agents control mediator release from mast and other cells and for their generalized membrane-stabilizing effects |
| Glucocorticoids, inhaled or systemic, for controlling transcription of mediator genes, and for controlling edema, mucus production, and eosinophil infiltration |
| Leukotriene modulators to decrease inflammatory mediator synthesis or antagonize inflammatory mediator receptors |
| Bronchodilators |
| Methylxanthines for reducing the frequency of recurrent bronchospasm |
| Adrenergic β2 receptor agonists for relaxing bronchial smooth muscle and decreasing microvascular permeability |
| Muscarinic receptor antagonists for inhibiting the bronchoconstrictor effects of endogenous acetylcholine |
Mechanisms of Action
Treatment of asthma and COPD involves the use of drugs with mechanisms that affect different aspects of these diseases. Table 16-1 summarizes these drugs and their mechanisms of action.
TABLE 16–1 Mechanisms of Action of Drugs to Treat Asthma and COPD
| Beneficial Effect | Drug Class | Cellular Mechanisms |
|---|---|---|
| Decreased inflammation | Chromones | Prevent the release of inflammatory mediators |
| Alter chloride ion channel function | ||
| Glucocorticoids (GCs) | Regulate gene expression | |
| Leukotriene modulators (LTMs) | Decrease leukotriene (LT) synthesis or prevent LT receptor activation | |
| Antihistamines | Prevent activation of histamine receptors | |
| Bronchodilation | Methylxanthines | Increase cAMP |
| Adenosine receptor antagonist | ||
| Adrenergic β2 receptor agonists | Increase cAMP | |
| Muscarinic antagonists | Block activation of muscarinic receptors by endogenous acetylcholine |
The GCs have multiple actions that decrease inflammation in asthma, which is key to improving asthmatic symptoms and preventing exacerbations. In controlling the inflammation of asthma, the primary effect of the GCs is to alter gene expression. The GCs, through activation of GC receptors (see Chapter 39), suppress the expression of genes for many inflammatory proteins. Inflammation is mediated by the increased expression of multiple inflammatory proteins including cytokines, chemokines, adhesion molecules, and inflammatory enzymes and receptors. The expression of most of these inflammatory proteins is regulated by increased gene transcription, which is controlled by proinflammatory transcription factors. The GCs are believed to switch off only inflammatory genes and do not suppress all activated genes because of the selective binding to coactivators that are activated by proinflammatory transcription factors.
GCs decrease bone marrow production of eosinophils and enhance their removal from the circulation by mediating their adherence to capillary walls (margination). GCs also reduce the local accumulation of eosinophils by inhibiting the release of eosinophil chemotactic factors such as LTB4 and cytokine tumor necrosis factor-α (TNF-α). The effect of the GCs on neutrophils is opposite to that on eosinophils. By inhibiting margination and stimulating bone marrow production, GCs lead to an increase in circulating neutrophils.
The LTs are potent inflammatory mediators generated from the metabolism of arachidonic acid through the 5-lipoxygenase (5-LOX) pathway (Fig. 16-2). These compounds, along with prostaglandins and related compounds, belong to a group of substances termed the eicosanoids (see Chapter 15). The LTs are synthesized in many inflammatory cells in the respiratory system including eosinophils, mast cells, macrophages, and basophils and are responsible for mediating numerous asthmatic symptoms via stimulation of specific LT receptors. LTB4 is a potent neutrophil chemotactic agent whose actions result from stimulation of members of the LTB receptor (BLT) family. Similarly, LTC4 and LTD4 cause bronchoconstriction, mucus hypersecretion, and mucosal edema and increase bronchial reactivity through activation of the Cys-leukotriene (CysLT, formerly known as the LTD4) receptor family. The effects of the LTs can be modulated either by inhibiting LT biosynthesis or by blocking activation of CysLT receptors. Zileuton* is an inhibitor of 5-LOX, thereby decreasing LT synthesis, whereas zafirlukast and montelukast are antagonists at Cys-LT1 receptors, thereby blocking receptor activation. These drugs are less effective antiinflammatory agents than the corticosteroids, but are preferable to long-term GC therapy because they have fewer adverse effects (see Chapter 39). They are used prophylactically in combination products.
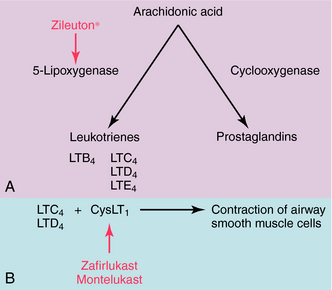
FIGURE 16–2 Newly generated lipid mast cell mediators depicting the sites of action of the LTMs. Zileuton* inhibits 5-lipoxygenase, thereby inhibiting the synthesis of the leukotrienes, whereas zafirlukast and montelukast are antagonists at the CysLT1 receptor. The inhibitory actions of the LTMs are shown in red.
Adrenergic β2 Receptor Agonists
Stimulation of adrenergic β2 receptors raises cAMP concentrations and inhibits smooth muscle contraction (see Chapter 9). Physiologically, bronchial smooth muscle relaxes, and the release of some mast cell-derived bronchoconstricting substances is inhibited. In addition, these drugs decrease microvascular permeability and suppress parasympathetic ganglionic activity (see Chapter 10). There is no evidence for an antiinflammatory effect of adrenergic agents or for any beneficial effect on bronchial hyperactivity.
Several β2 receptor agonists have been used therapeutically for the treatment of asthma. Epi and isoproterenol are highly effective but are reserved for special circumstances because of their nonselective activity, leading to β1 receptor-mediated cardiac stimulation. Short-acting selective β2 receptor agonists include albuterol,1 terbutaline, metaproterenol, bitolterol, and pirbuterol. Formoterol and salmeterol have been developed as highly lipid-soluble long-acting agents (t1/2 = 12 hours).
Muscarinic Receptor Antagonists
Bronchial smooth muscle is innervated mainly by the parasympathetic nervous system, and its activation causes bronchoconstriction (see Chapter 9). Before the development of modern pharmacology, leaves from the belladonna plant, which contain muscarinic antagonists (atropine and scopolamine) were smoked as a treatment for asthma. Atropine can be used as a bronchodilator and to reduce secretions, but its use is limited by autonomic and central nervous system (CNS) adverse effects. Ipratropium bromide is a quaternary nitrogen derivative of atropine that does not cross the blood-brain barrier but competitively inhibits muscarinic acetylcholine receptors in bronchial smooth muscle (see Chapter 10). Ipratropium is used as an inhaled preparation. Tiotropium is a long-acting muscarinic antagonist used as a bronchodilator that is useful for patients with COPD.
Anti-immunoglobulin Antibody
Omalizumab is a recombinant monoclonal antibody, which binds to and neutralizes human serum immunoglobulin type E (IgE) and prevents allergens from activating mast cells and other cells that release cytokines (see Chapter 6).
Pharmacokinetics
The pharmacokinetics for the GCs are presented in Chapter 39. When used for the treatment of asthma or COPD, responses to inhaled or oral steroids can occur within 4 hours but may take as long as 2 weeks, depending on the nature of the underlying lung disorder.
The LT receptor antagonists, montelukast and zafirlukast, as well as the 5-LOX inhibitor zileuton* are all orally administered, which is advantageous for treatment of children and other patients who have difficulty with or are noncompliant with inhaled therapies. Zileuton* has the disadvantage of requiring dosing four times per day. Montelukast and zafirlukast have similar pharmacokinetic profiles and may be administered once (montelukast) or twice (zafirlukast) daily. Zileuton* is also an inhibitor of hepatic CYP3A and will lead to increased levels of drugs metabolized by this CYP variant, including theophylline. This drug-drug interaction increases potential toxicity if the two drugs are administered concurrently.
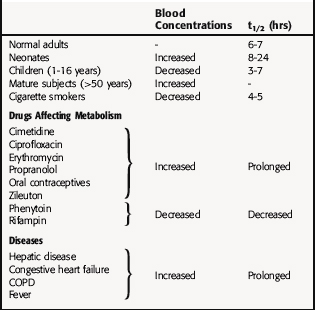
Theophylline clearance is influenced by food, smoking, age, disease, and other drugs metabolized by the liver (Table 16-2). Monitoring serum theophylline concentrations is necessary for any patient taking more than a minimal dose orally, especially sustained-release formulations, because of the multiple factors that influence blood concentrations and because the range of safe therapeutic concentrations is narrow. The therapeutic range is 5 to 15 µg/mL, and serious toxicity is increasingly likely at blood concentrations greater than 20 µg/mL, which results in a low therapeutic index.
When administered intravenously, theophylline can act rapidly on the lungs as a bronchodilator. However, this requires large bolus doses, which are used only occasionally because of toxicity. It is easier to maintain therapeutic blood concentrations by the oral route using sustained-release preparations, but this approach can lead to problems of cumulative toxicity.
Adrenergic β2 Receptor Agonists
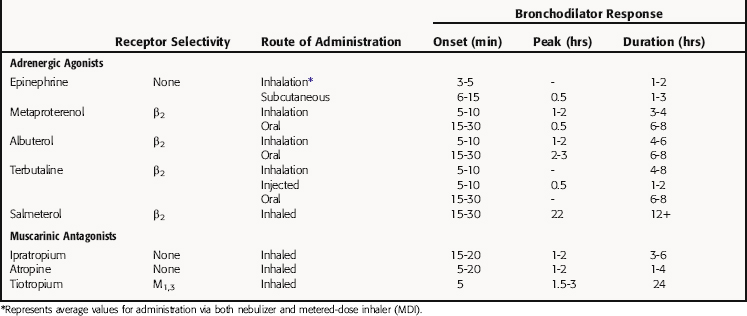
A general comparison of the pharmacokinetic profiles for these compounds is presented in Table 16-3. The bronchodilation that occurs in response to inhaled β2 receptor agonists has a fairly consistent onset at 5 to 30 minutes. Tightness of the chest will abate in most patients with asthma within 10 minutes after an injection of Epi. An optimal effect usually occurs within an hour and may last for 2 to 4 hours. In most circumstances β2 receptor agonists are effective for approximately 4 to 6 hours. Prolonged, repeated use of short-acting β2 receptor agonists, however, can cause a significant increase in heart rate in a small proportion of patients as a result of systemic absorption and concomitant stimulation of cardiac β1 receptors. With the development of a longer-acting β2 receptor agonist (salmeterol), which lasts for more than 12 hours, this problem may be partially resolved. However, unlike the short-acting β receptor agonists, salmeterol is not effective in treating acute episodes. Its major uses are in controlling nocturnal asthma and some cases of exercise-induced bronchospasm. The use of salmeterol alone has been associated with an increased risk of severe asthma exacerbations. Therefore it has been recommended that this agent be taken in fixed-dose combinations with an inhaled corticosteroid.
Muscarinic Receptor Antagonists
Inhaled ipratropium bromide is poorly absorbed and has few systemic side effects. The peak bronchodilator effect occurs 1 to 2 hours after inhalation, with a duration of action of 3 to 5 hours (see Table 16-3). Tiotropium, which exhibits selectivity at M1 and M3 receptors (see Chapter 10), has a duration of action of 24 hours. Both of these agents are used for management of the bronchoconstrictive component of COPD.
Relationship of Mechanisms of Action to Clinical Response
Reduced allergen exposure, inhaled cromolyn Na+ or nedocromil, inhaled GCs, or oral LTMs are antiinflammatory treatments that are each capable of reducing bronchial hyperactivity to help manage the problem. Cromolyn and related agents are used prophylactically only and are most effective for treating extrinsic asthma in children and young adults as well as exercise-induced bronchospasm.
Systemic GCs are the most effective treatment for both moderately severe and severe asthma and are used for treatment of acute exacerbations of COPD. However, these compounds lead to development of side effects after chronic administration (Chapter 39). The indication for oral corticosteroids is ongoing airway obstruction that is not relieved by other medicines within 1 to 2 days. Only a very small percentage of asthmatics (0.1%) become dependent on steroids, but this may represent as many as 10 patients per 100,000; thus it is a very important cause of iatrogenic disease.
Outpatient Treatment of Asthma
Antihistamines are generally not recommended for treatment of asthma. However, many allergic patients with rhinitis and asthma use antihistamines with no apparent harmful effects. Sedative antihistamines (see Chapter 14) should not be used in patients with acute bronchospasm. Antibiotics are commonly recommended for management of an exacerbation of asthma because of sputum production but should be reserved for those patients with bronchial infiltrates, fever, or sinusitis.
Exposure to allergens, particularly those found indoors, is well recognized as an important cause of asthma. Identification of sensitivity and education about measures necessary to decrease exposure are an important part of antiinflammatory treatment. For control of dust mites, enclosing the mattress and pillows in dust mite-proof covers, washing all bedding in boiling H2O, removing carpets, and using air filtration systems are important measures. Removing cats or dogs from the environment may be helpful; however, it will take weeks or months for the associated allergen levels to decrease. Cockroach eradication may be important for inner-city homes, in particular, and should involve such measures as enclosing all food, sealing gaps around pipes, and using poisonous bait. Special issues related to asthma are discussed in Box 16-1.
Pharmacovigilance: Side Effects, Clinical Problems, and Toxicity
The side effects of drugs used with asthma are summarized in the Clinical Problems Box.
The side effects of systemic corticosteroids are discussed in Chapter 39 and are mentioned here briefly in the context of pulmonary disease. The most important issue is the difference between short- and long-term use. Treatment with high-dose steroids, even short-term, can cause hypertension, diabetes, GI bleeding, and CNS disturbances. Elevations in blood glucose concentration and emotional changes are common but are usually easy to manage. Long-term steroid use produces a wide range of severe side effects, including thinning of the skin (striae, bruising), osteoporosis with rib fractures and vertebral compression, aseptic necrosis of the femoral head, which usually presents with pain, diabetes with complications, GI discomfort, ulceration and bleeding, cataract formation, and CNS disturbances, including frank psychosis. Prolonged oral use of steroids causes profound suppression of adrenal function. If patients are taking oral steroids for more than 7 days, the dose should be gradually reduced, because abrupt withdrawal can result in life-threatening adrenal insufficiency. Patients must be made fully aware of the harmful effects of long-term orally administered steroids.
Adverse effects of the leukotriene antagonists zafirlukast and montelukast are minimal, and generally, the drugs are well tolerated. However, rare cases of hepatotoxicity and eosinophilic vasculitis have occurred. The clinical features of the vasculitis are consistent with Churg-Strauss syndrome, a life-threatening condition typically treated with systemic corticosteroid therapy. The occurrence of the vasculitis syndrome appears to be linked with the decrease or withdrawal of oral corticosteroid therapy. Therefore the patient and the physician need to be acutely aware of symptoms related to eosinophilia, vasculitic rash, worsening of pulmonary symptoms, cardiac complications, and developing neuropathies.
Zileuton* can produce elevated liver enzymes, typically in the first few months of therapy. It also inhibits hepatic CYP3A, which metabolizes many drugs, including theophylline. Considering the correlation of serum levels of theophylline to therapeutic and toxic effects, patient monitoring is necessary if the two drugs are used concurrently.
Adrenergic β2 Receptor Agonists
The primary side effects of adrenergic agonists are cardiac stimulation, hypertension, tremor, and restlessness (see Chapter 11). The use of selective β2 receptor agonists decreases the risk of some of these effects. Inhaled β2 receptor agonists generally produce fewer side effects than oral preparations. Nonetheless, tachycardia and muscle tremor still occur. Continued use of these agents may result in the desensitization of β receptors (see Chapter 1); however, GC therapy can prevent or partially reverse this phenomenon. Epi can ameliorate severe life-threatening asthma attacks when administered subcutaneously. However, there are very few indications for this form of treatment in older patients or in those with underlying cardiovascular disease. Although there was a concern that chronic use of short-acting β2 receptor agonists would worsen asthma, this has not proven to be the case.
New Horizons
LTB4 is a proinflammatory lipid mediator generated from arachidonic acid through the action of 5-LOX that is implicated in many inflammatory disorders including asthma. BLT1, a G-protein-coupled receptor, is specific for LTB4, and the LTB4-BLT1 pathway is a novel future target for the treatment of asthma. Different immunosuppressive treatments, including methotrexate and tacrolimus, have been used in patients with severe or steroid-dependent asthma with variable degrees of success. Epidemiological evidence indicates an association of severity of asthma with fungus infections, and treatment with systemic antifungals (fluconazole or itraconazole, see Chapter 50) may be helpful for asthma in some cases.
* In the United Kingdom and Japan the drug name is salbutamol.
† Long-acting agents not suitable for emergency use. The use of these agents has been recommended to be taken only in fixed-dose combinations with an inhaled corticosteroid to avoid increased risk of severe asthma exacerbations with one of these agents alone.
‡ In the United Kingdom the drug name is sodium cromoglycate; in Japan the drug name is cromoglycate sodium.
Acetylcholine (ACh) is synthesized and secreted by non-neuronal cells and modifies their behavior. This “non-neuronal cholinergic system” is present in airway inflammatory cells where ACh has both proinflammatory and antiinflammatory activity, depending on the cell type. The function of this system can be modified by nicotine in cigarette smoke, the inflammation of asthma and COPD, and the drugs used in treating these diseases.
Anonymous. Drugs for allergic disorders. Treat Guidel Med Lett. 2007;60:71-80.
Anonymous. Drugs for asthma. Treat Guidel Med Lett. 2005;3:33-38.
Morrow T. Implications of pharmacogenomics in the current and future treatment of asthma. J Manag Care Pharm. 2007;13:497-505.
Weiss et al. 2006 Weiss ST, Litonjua AA, Lange C, et al. Overview of the pharmacogenetics of asthma treatment. Pharmacogenomics J. 2006;6:311-326.