71 Drowning
Drowning is usually related to a leisure situation that turned into a dramatic, life-threatening event. Parents, friends, relatives, babysitters, or guardians may feel not only profound loss and grief but also either guilt for failure to fulfill protection responsibilities or intense anger at others who did not provide adequate supervision or medical care. Nevertheless, drowning is a neglected public health problem.1 Each year, drowning is responsible for an estimated 500,000 deaths around the world. The exact number is unknown because many deaths go unreported.2
Age, gender, alcohol use, socioeconomic status (as measured by income and/or education), and lack of supervision are key risk factors for drowning. Considering all ages, males die five times more often from drowning than females. An estimated 40% to 45% of deaths occur during swimming.3 Young children, teenagers, and older adults are at highest risk of drowning.4 In the age group of 5 to 14 years, drowning is the leading cause of death worldwide among males and the fifth leading cause of death for females.4 The patterns of drowning are highly dependent on geographic factors. In the United States, drowning is the third most common cause of unintentional injury death for all ages and ranks second for people aged 5 to 44 years.5 Considering all deaths by drowning in United States (3443 in 2007), 53% occurred in swimming pools.3
Drowning is the second leading cause of death for children aged 1 to 14 years and third cause of injury death for all ages in Brazil. With a population of 190 million inhabitants in 2007, a total of 7009 deaths by drowning in 2007 (3.7 per 100,000 inhabitants) were reported.6 Ironically, 90% of all drowning deaths occur within 10 m of safety.2 On Rio de Janeiro beaches, precipitant causes are discernable in 13% of all cases, with the most frequent being alcohol (37%), seizures (18%), trauma (including boating accidents; 16.3%), cardiopulmonary diseases (14.1%), snorkeling and SCUBA diving (3.7%), diving resulting in head or spinal cord injuries, and others (e.g., homicide, suicide, syncope, cramps, immersion syndrome (11.6%). It is important to recognize a precipitant cause to drowning, as this may guide specific approaches to rescue and resuscitation. In Brazil, freshwater drowning occurs more commonly in rivers and lakes, contributing to half of deaths by drowning.7
 A New Definition
A New Definition
Sound epidemiologic data on drowning are lacking. Data collection for such purposes has been hampered by the absence of a uniform and internationally accepted definition. A lack of consensus is present with respect to definitions and terminology used by different water safety and health organizations, experts in the field, papers in the scientific medical literature, and laypersons.8 Within the framework of the first World Congress on Drowning (WCOD), a definition was developed to provide a common basis for future epidemiologic studies in all parts of the world. The following definition was adopted in June 2002: “Drowning is the process of experiencing respiratory impairment from submersion or immersion in liquid.”
The drowning process is a continuum beginning when the patient’s airway is below the surface of the liquid, usually water, which—if this process continues—may or may not lead to death. A patient can be rescued at any time during the process and be given appropriate resuscitative measures, in which case the process is interrupted. Furthermore, any submersion or immersion incident without evidence of liquid aspiration should be considered a water rescue (i.e., events where no respiratory impairment is evident, whether with or without other injury or hypothermia). The term near-drowning was abandoned. Confusing terms like dry drowning and secondary drowning (delayed onset of respiratory distress) are now eliminated.9
 Pathophysiology
Pathophysiology
Despite pathophysiologic differences between drowning in fresh or salt water in experimental models, from a clinical and therapeutic view, there are no important differences in humans. The most significant pathophysiologic alteration in drowning relates to hypoxia.10 When there is no way to keep the airways out of water, breath holding is the first automatic response when there is no hypoxia and consciousness is still preserved. Water in the mouth is spit out or swallowed actively. When the first involuntary aspiration of water occurs, it produces coughing or rarely laryngospasm (less than 2%), leading to hypoxia. If laryngospasm occurs, hypoxia will lead to its rapid termination. More water is gradually aspirated into the lungs, leading to further hypoxia, loss of consciousness, irreversible apnea, and then asystole.
The respiratory disturbances depend less on the composition of the water and more on the amount of water aspirated. The aspiration of either fresh or salt water produces surfactant destruction, alveolitis, and a noncardiogenic pulmonary edema resulting in increased intrapulmonary shunt and hypoxia.11 In animal research, the aspiration of 2.2 mL of water per kilogram of body weight decreases the arterial oxygen pressure (PaO2) to approximately 60 mm Hg within 3 minutes.12 In humans, it seems that as little as 1 to 3 mL/kg of water aspiration produces profound alterations in pulmonary gas exchange and decreases pulmonary compliance by 10% to 40%.11 Humans rarely aspirate sufficient amounts of water to provoke significant electrolyte disturbances, and victims need no initial electrolyte correction.13
Ventricular fibrillation in humans, when it occurs, is related to hypoxia and acidosis, not to hemolysis and hyperkalemia. Hypoxia produces a well-established sequence of cardiac deterioration, with tachycardia, then bradycardia, then a pulseless phase of ineffective cardiac contractions (PEA phase) followed by complete loss of cardiac rhythm and electrical activity (asystole). Decreased cardiac output, arterial hypotension, increased pulmonary arterial pressure, and pulmonary vascular resistance are the results of hypoxia.11 Intense peripheral vasoconstriction can also be caused by hypoxia, catecholamine release, and hypothermia.
 Chain of Survival, Prevention to Hospital
Chain of Survival, Prevention to Hospital
In 2007, the United States Lifesaving Association reported 74,463 rescues on the shores of U.S. beaches, with estimates of 683 cases of rescues for each reported death (www.usla.org/Statistics/public.asp). On Rio de Janeiro beaches, approximately 290 rescues for each reported death (0.34%) occurred, and there was one death for each 10 victims admitted for medical care in the Drowning Resuscitation Center (DRC). In the past 31 years of work, the Rescue Service of Rio de Janeiro made approximately 166,000 rescues by lifeguards on the beaches, and 8500 victims needed medical attention in the DRC.14 For drowning, rescue is an essential component to keep the patient alive, and the initial evaluation is made in a hostile environment (water). Therefore, it is essential for physicians to be aware of the drowning chain of survival,15 from prehospital care to hospital admission (Figure 71-1).15

Figure 71-1 Drowning chain of survival.
(Adapted from Szpilman D, Morizot-Leite L, Vries W, et al. First aid courses for the aquatic environment. In: Bierens J, ed. Handbook on Drowning: Prevention, Rescue, and Treatment. Berlin: Springer-Verlag, 2006:342-7.)
Prevention
Despite the emphasis on immediate treatment, the definitive therapy for drowning is prevention (Table 71-1). Prevention remains the most powerful therapeutic intervention and can be effective in more than 85% of drownings.
|
Watch children carefully; 84% of drownings occur because of inadequate adult supervision. Begin swimming lessons from 2 years of age.
|
| Beaches | Pools and Similar |
|---|---|
|
Do not overestimate your swimming capability—46.6% of drowning victims thought they knew how to swim.
|
Recognition of the Incident
Initiation of help to a drowning victim must be preceded by a recognition that someone is drowning. Contrary to popular opinion, the victim (especially males) does not wave or call for help.16 The victim is typically in an upright posture, with arms extended laterally, thrashing and slapping the water. Individuals close by may not recognize that the victim is struggling and may assume that the victim is playing and splashing in the water. The victim may submerge and resurface several times during this phase. Children can struggle for only 10 to 20 seconds before final submersion, and adults may be able to struggle for up to 60 seconds.16 Because breathing instinctively takes precedence, the drowning victim is usually unable to cry for help.
In-Water Basic Life Support and Rescue
For nonlifeguards, an attempt to help without becoming a second victim is the priority. If possible, potential rescuers can use techniques like “throw before you go and reach (with long objects) before you assist” or can advise the victim on how to get out of this situation (e.g., choosing a better way to escape, swim, float, reassuring the victim that assistance is coming). The decision when to do basic water life support (BWLS)15 is based on the victim’s consciousness level. If conscious, rescue to land without any further medical care is the protocol.17 The panicked and struggling victim can be dangerous to a would-be rescuer. A victim attempting to cling to life and breathe can drown a potential rescuer. For this reason, it is always best to approach a struggling victim with an intermediary object. Lifeguards use rescue or torpedo buoys for this purpose that also can double as a thorax and face flotation device to keep the head out of the water and the airways free.16
For an unconscious victim, the most important step is the immediate institution of resuscitative measures. Hypoxia caused by submersion results first in cessation of breathing, leading to cardiac arrest within a variable but short time interval if not corrected. In-water resuscitation (ventilation only) provides the victim a 3.15 times better chance of survival without sequelae. Rescuers should check ventilation and, whenever possible and if indicated, attempt to provide mouth-to-mouth resuscitation while still in the water. Unfortunately, external cardiac compressions cannot be performed effectively in the water, so assessment for pulse and compression must be delayed until the victim is out of the water.17 Very few studies have examined how often in-water cervical spine injury (CSI) occurs. In one study concerning sand beaches, 46,060 water rescues were retrospectively evaluated; this study found that the incidence of CSI in this setting was very low (0.009%).18 In another retrospective survey of more than 2400 drownings, only 11 (<0.5%) had CSI, and all of these had a history of obvious trauma from diving, falling from height, or a motor vehicle accident.19 Other water locations may have different rates of CSI depending on a wide variety of elements. Furthermore, any time spent on immobilizing the cervical spine in unconscious victims with no signs of trauma could lead to cardiopulmonary deterioration and even death.
Considering the low incidence of CSI and the high risk of wasted time in ventilation when needed, routine cervical spine immobilization of water rescues without reference to whether a traumatic injury was sustained is not recommended.18,19 Rescuers who suspect a spinal cord injury should float the victim supine in a horizontal position, allowing the airways to be out of the water, and check to see if there is spontaneous breathing. If the victim is not breathing, protocols should be started for in-water resuscitation (mouth-to-mouth) while maintaining the head in a neutral position as much as possible. The rescuer should then use a jaw thrust without head tilt or chin lift to open the airway, without risking him- or herself or the victim. If there is spontaneous breathing, the rescuer’s hands should be used to stabilize the victim’s neck in a neutral position. If possible, a back-support device should be applied before moving the individual from the water. The victim should be rescued to a dry place, maintaining the neck in a neutral position as much as possible. The head, neck, chest, and body should be kept in alignment if the victim must be moved or turned.10
On-Land Basic Drowning Life Support
Removal of the victim from the water should be performed according to their level of consciousness, but preferably a vertical position should be adopted to avoid vomiting and further complications to the airways.20 If the victim is exhausted, confused, or unconscious, transport should be in as near a horizontal position as possible but with the head still maintained above body level20 (keep horizontal if prolonged immersion or a history of immersion in cold water). The airways must be kept open at all times. The first procedure in on-land basic drowning life support (BDLS) should be placing the victim in a position parallel to the waterline,20 as horizontal as possible, lying supine, far enough away from the water to avoid incoming waves. If conscious, reposition the victim supine with head up. If breathing, place in recovery position (lateral decubitus position).20 In a 10-year study in Australia, vomiting occurred in more than 65% of victims who needed rescue breathing and in 86% of those who required both rescue breathing and chest compressions.21 Even in victims who required no interventions after water rescue, vomiting occurred in 50% once they reached shore. The presence of vomitus in the airway can result in further aspiration and impairment of oxygenation by airway obstruction; it can also discourage rescuers from attempting mouth-to-mouth resuscitation.21 The abdominal thrust (Heimlich) maneuver should never be used as a means of expelling water from the lungs; it is ineffective and carries significant risks. During resuscitation, attempts at active drainage by placing the victim head down increases the risk of vomiting more than fivefold and leads to a small but significant increase in mortality (19%) when compared with keeping the victim in a horizontal position.20 If vomiting occurs, turn the victim’s mouth to the side, and remove the vomitus with a finger sweep, a cloth, or use of suction.
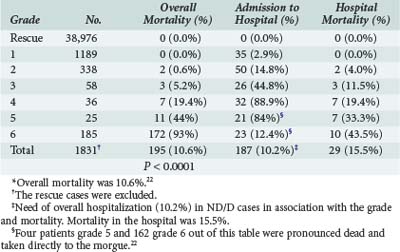
One of the most difficult medical decisions a lifeguard or an emergency medical technician (EMT) must make is how to treat a drowning victim appropriately. A cardiopulmonary or an isolated respiratory arrest occurs in approximately 0.5% of all rescues. The questions that arise are should the rescuer administer oxygen, call an ambulance, transport the person to a hospital, or observe for a time at the site? Even emergency physicians may be in doubt as to the most appropriate immediate support measures; drowning victims vary in the severity of injury. Based on these needs, a classification system was developed in Rio de Janeiro (Brazil) in 1972 and updated in 199722 to assist lifeguards, ambulance personnel, and physicians with treatment priorities. It was based on analysis of 41,279 rescues, of which 2304 (5.5%) needed medical attention. The system was revalidated in 2001 by a 10-year study with 46,080 rescues.23 This classification (see Algorithm 71-1)22 encompasses all support from the site of the accident to the hospital, recommends treatment, and shows the likelihood of death based on the severity of injury. Severity is easily assessed by an on-scene rescuer, EMT or physician using only clinical variables.22
Advanced Drowning Life Support on Site
Grade 6: Cardiopulmonary Arrest
Resuscitation started by layperson or lifeguard at the scene must be continued by advanced life support (ALS) personnel until successful, or if there is no way to warm the victim appropriately at the scene. In this case, the victim should be transported while receiving resuscitation to a hospital where advanced warming measures can be accomplished. The first priority is adequate oxygenation and ventilation. The medical staff must keep doing cardiac compression while starting artificial ventilation using bag and facemask with 15 liters of oxygen until an orotracheal tube can be inserted. Once intubated, victims can be oxygenated and ventilated effectively even through copious pulmonary edema fluid. The Sellick maneuver should be used if possible during intubation to prevent regurgitation and aspiration. Aspirate the orotracheal tube only when fluid interferes with effective ventilation. Semiautomatic external defibrillation may have a role in cardiac rhythm monitoring. If the drowning victim is pulseless and hypothermic (<34°C), CPR must be continued. Although ventricular fibrillation (VF) is uncommon, especially in pediatric victims, some adults may develop VF as a consequence of coronary artery disease or from ALS therapies such as epinephrine. Peripheral venous access is the preferred route for drugs. Although some drugs can be administered endotracheally despite copious noncardiogenic pulmonary edema fluid, whether the drugs are absorbed and what doses to use are unresolved issues.16 The epinephrine dose for resuscitation is still a controversial issue in the setting of a drowning, where the time elapsed to start resuscitation can be much longer and outcome much different from other causes. Both beneficial and toxic physiologic effects of epinephrine administration during CPR have been shown in animal and human studies. Initial or escalating high-dose epinephrine has occasionally resulted in return of spontaneous circulation and improved early survival. Higher doses of epinephrine have not improved long-term survival and neurologic outcome when used as initial therapy, but higher doses have not definitively been shown to cause harm either. Therefore, high-dose epinephrine is not recommended for routine use but can be considered if 1-mg doses fail.24 Our recommendation is to use a first dose of 0.01 mg/kg IV after 3 minutes of CPR26 and if no response is achieved, increase to 0.1 mg/kg each 3 minutes of CPR.10
Grade 4: Acute Pulmonary Edema With Hypotension
Oxygen with mechanical ventilatory support is the first-line therapy. Initially, oxygen should be administered by facemask at 15 L/min until an orotracheal tube can be inserted. Grade 4 needs early intubation in all cases, which is an optimal provision of positive airway pressure. Mechanical ventilation is indicated for SaO2 of less than 90% with the use of 15 liters of oxygen by facemask, a PaCO2 of more than 45 mm Hg, an abnormally high respiratory rate, or excessive patient effort to maintain adequate arterial blood gases (ABG), such that the patient is consuming large amounts of energy breathing and is likely to tire.16 Patients should be sedated to tolerate intubation and artificial mechanical ventilation providing tidal volume of at least 5 mL/kg of body weight. FIO2 can start at 1.0, but as soon as possible (usually less than 20 minutes) should be reduced to 0.45 or less to avoid oxygen toxicity. Positive end-expiratory pressure (PEEP) should be added initially at a level of 5 cm H2O and then increased by 2 to 3 cm H2O increments until the desired intrapulmonary shunt (QS : QT) of 20% or less, or PaO2:FIO2 of 250 or more is achieved. If low blood pressure is not corrected by oxygen, a rapid crystalloid infusion (independent of drowning water type) should be used before trying to reduce PEEP.11,27
Hospital
Hospital admission in severe cases (grades 4 to 6) is only possible if adequate and prompt BDLS and ADLS prehospital care was accomplished. If this is not the case, the appropriate approach is to follow ADLS on-site protocols. Hospital care is recommended for grades 2 to 6. Decision making in the emergency department about admission to an intensive care unit (ICU) or hospital bed versus observation in an emergency department or discharge home should include a thorough history of the accident and previous illness, physical examination, and diagnostic studies including chest radiography and ABG measurement. Electrolytes, blood urea nitrogen, creatinine, and hemoglobin also should be assessed serially, although perturbations in these laboratory tests are unusual. In some cases, a toxicologic screen for suspected alcohol or drug ingestion might be warranted. Patients grade 3 to 6 should be admitted to an ICU for close observation and therapy. Patients grade 2 can be observed in the emergency room for 6 to 24 hours, but grade 1 and rescue cases with no complaints or associated illness or trauma should be released home. Table 71-2 shows general mortality rates for each grade of severity, hospitalization need, and prehospital and in-hospital mortality rates.
Despite aggressive management, neurologic injury and sequelae, including persistent vegetative state, can occur in grade 6 drowning victims. In patients who are hemodynamically unstable or have severe pulmonary dysfunction (grade 4 to 6), pulmonary artery catheterization may provide useful information concerning Starling forces in the lungs and may help in managing pulmonary edema. Vasopressors should only be used in refractory hypovolemia when replacement with crystalloid was not enough to restore blood pressure. No evidence exists to support routine administration of hypertonic solutions and transfusions for fresh water drowning; similarly, there are no data to recommend use of hypotonic solutions in salt-water cases.11,27 Echocardiography to assess cardiac function and ejection fractions can help to guide the clinician in titrating inotropic agents, vasopressors, or both if volume crystalloid replacement had failed. Some studies have shown that cardiac dysfunction with low cardiac output is common immediately after severe drowning cases (grades 4 to 6).11 Important supportive measures include Foley catheter placement to monitor urine output. Low cardiac output is associated with high pulmonary capillary occlusion pressure, high central venous pressure, and high pulmonary vascular resistance and can persist for days after correction of oxygenation and perfusion abnormalities in drowning victims. Despite depressed cardiac output, furosemide therapy is not generally indicated. One study even has suggested that volume infusion benefits drowning victims. Studies suggest that dobutamine infusion to improve cardiac output is the most logical and potentially beneficial therapy in such cases.
Metabolic acidosis occurs in 70% of patients arriving at the hospital after a drowning episode.13 It should be corrected when pH is lower than 7.2 or the bicarbonate is less than 12 mEq/L if the victim has adequate ventilatory support.27 Significant depletion of bicarbonate is rarely present in the first 10 to 15 minutes of CPR, and its use is not indicated in the initial resuscitation period.26
Pools and beaches generally have insufficient bacteria to promote pneumonia in the immediate postdrowning period.28 If the victim needs mechanical respiratory assistance, the incidence of secondary pneumonia increases from 34% to 52% in the third or fourth day of hospitalization when pulmonary edema is resolving.29 Vigilance not only for pulmonary but also other infectious complications is important. Prophylactic antibiotics are of doubtful value in the intensive care management and tend to select out only more resistant and more aggressive organisms. An altered chest x-ray should not be interpreted as pneumonia, because it is usually the result of pulmonary edema and aspirated water in the alveoli and bronchi. It is preferable to monitor tracheal aspirates daily with Gram stain, culture, and sensitivity. At the first sign of pulmonary infection, usually after the first 48 to 72 hours (as gauged by prolonged fever, sustained leukocytosis, persistent or new pulmonary infiltrates, and leukocyte response in the tracheal aspirate), antibiotic therapy can be initiated on the basis of predominant organism and sensitivities. Fiberoptic bronchoscopy may be useful for evaluation of infection by obtaining quantitative cultures, determining the extent and severity of airway injury in cases of aspiration of solids, and for the rare occasions where therapeutic clearing of sand, gravel, and other solids is indicated. Corticosteroids for pulmonary injury are at best of doubtful value and should not be used except for bronchospasm.
The clinician must be aware of and constantly vigilant for potential complications associated with beta-adrenergic bronchodilators and underlying pulmonary injury in the drowning victim, especially volutrauma and barotrauma.28 Spontaneous pneumothoraces are common (10%) secondary to positive-pressure ventilation and local areas of hyperinflation. Any sudden change in hemodynamic stability after mechanical ventilation should be considered to be due to pneumothorax or other barotrauma until proved otherwise. After a secure airway is established, nasogastric tube placement reduces gastric distention and prevents further aspiration. Rarely, drowning victims who seem healthy on assessment in the emergency department, including having normal chest radiography, develop fulminant pulmonary edema as long as 12 hours after the incident. Whether this late-onset pulmonary edema is delayed ARDS or neurogenic pulmonary edema secondary to hypoxia is unclear. Renal insufficiency or renal failure is rare in drowning victims but can occur secondary to anoxia, shock, or hemoglobinuria.
The most important complication after a drowning episode, beyond reversible pulmonary injury, is anoxic-ischemic cerebral insult. Most late deaths and long-term sequelae of drowning are neurologic in origin.28 Although the highest priority in resuscitation after drowning is restoration of spontaneous circulation, every effort in the early stages after rescue should be directed at resuscitating the brain and preventing further neurologic damage. These steps include providing adequate oxygenation (Sat O2 > 92% but not 100%) and cerebral perfusion (mean arterial pressure around 100 mm Hg). Any victim who remains comatose and unresponsive after successful CPR or deteriorates neurologically should undergo careful and frequent neurologic function assessment for the development of cerebral edema and should be treated with the following measures:
New therapeutic interventions for drowning victims such as extracorporeal membrane oxygenation, artificial surfactant, nitric oxide, and liquid lung ventilation are still in the investigational stage.30
 Outcome and Scoring Systems
Outcome and Scoring Systems
Drowning victims with severities of grade 3 to 6 have the potential to develop multisystem organ failure.16 Despite this, the prognosis for such patients is primarily based on neurologic outcome.2 Drowning grade 1 to 5 patients return home safely without sequelae in 95% of cases.22 Of major concern among researchers are grade 6 victims. Both at the rescue site and in the hospital, no one indicator for grade 6 appears to be absolutely reliable in terms of defining outcome.31 Based on the longest submersion time registered in cold water (66 minutes) with complete recovery,16 resuscitation should be started without delay in each victim without carotid palpable pulse who has been submerged for less than 1 hour or does not present obvious physical evidence of death (rigor mortis, putrefaction or dependent lividity).
Contrary to some research that affirms that prolonged submersion and successful resuscitation is only possible after exposure to cold or icy water, some anecdotal cases in warm water were described to survive without sequelae.22,32,33 Multiple studies have established that outcome is almost solely determined by a single factor: duration of submersion (Table 71-3).17,21,22,28,32–36 Basic and advanced life support enable victims to achieve their best outcome possible when the time of duration cardiopulmonary arrest (submersion time included) is minimized. Based on a report of a drowning victim successfully resuscitated after 2 hours of CPR,28 efforts should stop only if asystole persists after rewarming the victim above 34°C.
TABLE 71-3 Probability of Neurologically Intact Survival to Hospital Discharge*
| Duration of Submersion | Death or Severe Neurologic Impairment |
|---|---|
| 0 to <5 minutes | 10% |
| 5 to <10 minutes | 56% |
| 10 to <25 minutes | 88% |
| >25 minutes | 100% |
* Based on duration of submersion.35 Note in these data how 5 more minutes of submersion in the 5 to <10-minute group increases mortality almost 6 times compared to the 0 to <5-minute group.
Prognostic scoring systems have been developed to predict which patients will do well with standard therapy and which are likely to have a significant cerebral anoxic encephalopathy and will require aggressive measures to protect the brain. One of the best characterized prognostic factors is consciousness level related to the Glasgow Coma Scale at the period immediately after resuscitation (first hour; Conn & Modell Neurological Classification).28,37 Because of the typical delay of 2 to 6 hours between rescue and transfer from an outlying emergency facility to a pediatric ICU, many patients with severe anoxic-ischemic cerebral insults and coma have had multiple determinations of neurologic status and level of consciousness before definitive therapy is begun. Data suggest that patients who remain profoundly comatose (i.e., decorticate, decerebrate, or flaccid) 2 to 6 hours after the drowning accident are brain dead or have moderate to severe neurologic impairment. Patients who are improving but remain unresponsive have a 50% likelihood of a good outcome. Most patients who are clearly improving and are alert, or are stuporous or obtunded but respond to stimuli 2 to 6 hours after the incident, have normal or near-normal neurologic outcomes. These prognostic variables are important in counseling family members of drowning victims in the early stages after the accident and in deciding which patients are likely to have a good outcome with standard supportive therapy and which victims should be candidates for more agressive attempt to cerebral resuscitation therapies33,35 (Table 71-4).
TABLE 71-4 Clinical Prognostic Score for the Immediate Period Post Successful CPR*
| Neurologic Prognostic Score | |
| (Post Successful CPR on Drowning) | |
| A—First Hour | B—After 5 to 8 Hours |
Recovery Without Sequelae
Szpilman D, Handley AJ, Bierens J, Quan L, Vasconcellos R. Drowning. In: Field JM, editor. The Textbook of Emergency Cardiovascular Care and CPR. Philadelphia: Lippincott Williams & Wilkins; 2009:477-489. Co-sponsored by AHA & ACEP
Field JM, editor. Drowning. In ACLS Resource Text for Instructors and Experienced Providers. Dallas: American Heart Association Inc.; 2008:301-317.
Bierens J, editor. Handbook on Drowning: Prevention, Rescue and Treatment. Heidelberg, Germany: Springer-Verlag, 2006.
Orlowski JP, Szpilman D. Drowning. Rescue, resuscitation, and reanimation. Pediatr Clin North Am. 2001;48(3):627-646.
Szpilman D. Near-drowning and drowning classification: a proposal to stratify mortality based on the analysis of 1831 cases. Chest. 1997;112(3):660-665.
Bierens JJ, van der Velde EA, van Berkel M, van Zanten JJ. Submersion in The Netherlands: prognostic indicators and results of resuscitation. Ann Emerg Med. 1990;19(12):1390-1395.
Cummins RO, Szpilman D. Submersion. In: Cummins RO, Field JM, Hazinski MF, editors. ACLS—The Reference Textbook. Vol 1. ACLS for Experienced Providers. Dallas: American Heart Association Inc.; 2003:97-107.
1 Murray CJL. Quantifying the burden of disease: the technical basis for disability-adjusted life years. Bull World Health Organ. 1994;72:429-445.
2 DeNicola LK, Falk JL, Swanson ME, Gayle MO, Kissoon N. Submersion injuries in children and adults. Critical Care Clinics. 1997 july;13(3):P477-P502.
3 Branche CM. What is really happening with Drowning Rates in the United States? In: Fletemeyer JR, Freas SJ, editors. Drowning-New Perspectives on Intervention and Prevention. CRC Press; 1998:P31-P42.
4 World Health Organization. Bulletin report on injury—a leading cause of the global burden of disease@. WHO; 1998.
5 Centers for Disease Control. Fatal injuries to children: United States, 1986. MMWR Morb Mortal. 1990;39:442-451.
6 Szpilman D. Drowning in Brazil—179,000 deaths in 25 years—are we stepping down?. Porto, Portugal: World Water Safety Congress; 2007 September.
7 Szpilman D, Handley AJ, Bierens J, Quan L, Vasconcellos R. Drowning. In: Field JM, editor. The Textbook of Emergency Cardiovascular Care and CPR. Philadelphia: Lippincott Williams & Wilkins; 2009:477-489. Co-sponsored by AHA & ACEP
8 Szpilman D, Orlowski JP, Cruz-Filho FES, Elmann J. HEY “Near-drowning”, You’ve Been Messing Up Our Minds!. Amsterdam: World Congress on Drowning; 2002. Book of Abstracts, P114
9 Beeck EF, Branche CM, Szpilman D, Modell JH, Birens JJLM. A new definition of drowning: towards documentation and prevention of a global health problem; Bulletin of World Health Organization 2005;83(11).
10 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science, Circulation 2010 November 2;122(3):18. Part 12: Cardiac Arrest in Special Situations, p. S847-8 and S771-3.
11 Orlowski JP, Abulleil MM, Phillips JM. The hemodynamic and cardiovascular effects of near-drowning in hypotonic, isotonic, or hypertonic solutions. Ann Emerg Med. 1989;18:1044-1049.
12 Modell JH, Moya F, Newby EJ, Ruiz BC, Showers AV. The effects of fluid volume in seawater drowning. Ann Intern Med. 1967;67:68-80.
13 Szpilman D. Afogamento, Revista Bras. Med Esporte—Vol 6, N4—Jul/Ago. 2000:P131-P144.
14 Szpilman D. Drownings on the Beaches of Brazil. In: Fletemeyer JR, Freas SJ, editors. Drowning—New Perspectives on Intervention and Prevention. CRC Press; 1998:P125-P146.
15 Szpilman D, Morizot-Leite L, Vries W, et al. First aid courses for the aquatic environment. In: Bierens J, editor. Handbook on Drowning: Prevention, Rescue, and Treatment. Berlin: Springer-Verlag; 2006:342-347.
16 Orlowski JP, Szpilman D. “Drowning—Rescue, Resuscitation, and Reanimation” Pediatric Critical Care: A New Millennium, W. B. Saunders Company Pediatric Clinics Of North America—V48, N3. 2001 June.
17 Szpilman D, Soares M. In-water resuscitation—is it worthwhile? Resuscitation. 2004;63:25-31.
18 Wernick P, Fenner P, Szpilman D. Immobilization and extraction of spinal injuries. In: Bierens J, editor. Handbook on Drowning: Prevention, Rescue, and Treatment. Berlin: Springer-Verlag; 2006:291-295.
19 Watson RS, Cummings P, Quan L, Bratton S, et al. Cervical spine injuries among submersion victims. J Trauma. 2001;51:658-662.
20 Szpilman D, Handley A. Positioning the drowning victim. In: Bierens J, editor. Handbook on drowning prevention, Rescue and Treatment. Berlin: Springer-Verlog; 2006:334-341.
21 Manolios N, Mackie I. Drowning and near-drowning on Australian beaches patrolled by life-savers: a 10-year study, 1973-1983. Med J Aust. 1988;148:165-167. 170-1
22 Szpilman D. Near-drowning and drowning classification: a proposal to stratify mortality based on the analysis of 1831 cases. Chest. 112(3), 1997.
23 Szpilman D, Elmann J, Cruz-Filho RES. Drowning classification: a revalidation study based on the analysis of 930 cases over 10 years. Amsterdam: World Congress on Drowning; 2002. Book of Abstracts, p. 66
24 Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care (ECC). Circulation. 2000 August 22;102(8):129.
25 Nichter MA, Everett PB. Childhood near-drowning: Is cardiopulmanry resuscitation always indicated? Crit Care Med. 1989;17:993-995.
26 Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care (ECC). JAMA. 1992 October 28;268:16.
27 Bierens JJLM, Huet RCG, Turner NM, Berkel M, Knape JTA. Resuscitation guidelines; controversies and pitfalls in case of submersion. expert observation.
28 Orlowski JP. Drowning, near-drowning, and ice water submersion. Pediatr Clin North Am. 1987;34:92.
29 Berkel M, Bierens JJLM, Lierlk, et al. Pulmonary Oedema, Pneumonia and Mortality in Submersions Victims. A Retrospective study in 125 patients. Int C Md. 1996;22:101-107.
30 Wang CH, Chou CC, Ko WJ, et al. Rescue a drowning patient by prolonged extracorporeal membrane oxygenation support for 117 days. Am J Emerg Med. 2010 Jul;28(6):750.e5-750.e7.
31 Bierens JJLM, Velde EA, Berkel M, Zanten JJ. Submersion in the Netherlands; prognostic indicators and results of resuscitation. Annals of Emerg Medicine. 1990;19:1390-1395.
32 Szpilman D. A case report of 22 minutes submersion in warm water without sequelae. In: Bierens J, editor. Handbook on Drowning: Prevention, Rescue, and Treatment. Berlin: Springer-Verlag; 2006:375-376.
33 Allman FD, Nelson WB, Gregory AP, et al. Outcome following cardiopulmonary resuscitation in severe near-drowning. Am J Dis Child. 1986;140:571-575.
34 Orlowski JP. Prognostic factors in pediatric cases of drowning and near-drowning. Journal of the College of Emergency Physicians. 1979;8:176-179.
35 Cummings P, Quan L. Trends in unintentional drowning: the role of alcohol and medical care. JAMA. 1999;281:2198-2202. 1990;86:586-93
36 Cummins RO, Szpilman D. Submersion. In: Cummins RO, Field JM, Hazinski MF, editors. ACLS-the Reference Textbook; volume II: ACLS for Experienced Providers. Dallas, TX: American Heart Association; 2003:97-107.
37 Layon AJ, Modell JH. Drowning: Update 2009. Anesth. 2009;110(6):1390-1401.