Chapter 151 Dorsal Thoracic and Lumbar Combined and Complex Techniques
Length of Construct
In adults, including the L5-S1 disc space in the fusion should be considered in any long construct that otherwise would have ended in the caudal lumbar spine. As outlined by Bridwell, indications for fusion to the sacrum in adults in a long construct include (1) L5-S1 spondylolisthesis, (2) previous L5-S1 laminectomy, (3) central or foraminal stenosis at L5-S1, (4) oblique takeoff of L5, and (5) “severe” degeneration of the disc.1 Although fusing to the sacrum does decrease a significant amount of motion, there is a significant risk of adjacent segment degeneration when the construct is stopped at L5 in the adult degenerative deformity population. A retrospective study by Edwards et al. found that in a population of patients who had undergone a thoracolumbar construct that ended caudally at L5 who preoperatively had a “healthy” L5-S1 disc, 61% of patients had developed advanced degenerative disease at this level over a mean follow-up of 5.6 years.2
Because of the risk of pseudarthrosis at the L5-S1 space, many authorities have advocated for the use of interbody support at this level. Polly et al. found that L5-S1 interbody support increases biomechanical stability, restores junctional lordosis, improves the lumbosacral fusion rate, and increases disc and foraminal height, thus decreasing foraminal stenosis.3 In the adult deformity patients undergoing spine fusion, the restoration or maintenance of sagittal balance has been found to have a significant impact on outcome.4 Restoring junctional lordosis at L5-S1 through placement of an interbody graft is a powerful technique to correct sagittal imbalance. This is due to the long moment arm that occurs when the L5-S1 disc space angulation is altered relative to the C7 vertebral body on which sagittal balance is based. To maximize the footprint of the graft as well as the restoration of lordosis, an anterior lumbar interbody fusion (ALIF) is a better procedure than a transforaminal lumbar interbody fusion (TLIF) at L5-S1.5 One must weigh the benefit of a larger interbody device against the morbidity of an anterior approach when selecting an anterior approach versus a TLIF or posterior lumbar interbody fusion (PLIF).
Long constructs that extend to the sacrum can be problematic from a fixation standpoint. Although the S1 pedicles are large, the sacrum is composed of primarily cancellous bone, resulting in a decreased pull-out strength compared with other pedicle screws. This has prompted many to attempt to place bicortical pedicle screws to capture the anterior and posterior cortical bone to increase the strength of the screw. Lehman et al. showed that the highest bone mineral density, and therefore the greatest insertional torque for pedicle screws, was in the anterior sacral promontory, so that from a biomechanical standpoint, the strongest S1 screws are the so-called “tricortical” screws. When screws are placed in this fashion, there is almost a 99% increase in the insertional torque.6 In addition to an L5-S1 interbody and the placement of tricortical S1 pedicle screws, iliac screws have been advocated as another method to offload the S1 pedicles to allow for a solid arthrodesis at L5-S1. Indications for iliac screws include constructs greater than three levels that end in the sacrum, revision surgery for L5-S1 pseudarthorsis, high-grade spondylolisthesis, or trauma or pathology that does not allow for adequate sacral fixation.7 Kuklo et al. evaluated 81 patients who underwent fusion procedures that included the L5-S1 space using S1 and iliac screws. Approximately 50% (n = 42) were for isthmic spondylolisthesis, whereas the remainder (n = 39) were for long constructs to the sacrum. The researchers found that even in patients who had previous iliac crest grafts taken, 94% (34/36) had iliac screws placed without screw loosening or iliac crest fracture. Overall, the fusion rate, to include revision surgeries, was 95.1%.8
Junctional Kyphosis
One of the reasons to plan and execute an appropriate-sized construct is to avoid proximal junctional kyphosis (PJK). In 1999, Lee et al. looked at 69 patients with adolescent idiopathic scoliosis (AIS) who underwent fusion up to T3. The investigators defined PJK as greater than 5 degrees above the summed normal of the angular segments from the proximal instrumented segment to T2. They found a 46% incidence of PJK. As would be expected, a predictor of postoperative PJK was preoperative kyphosis of more than 5 degrees above the proposed proximal instrumented level, indicating that these levels should be included in the construct to avoid this complication.9
In the adult deformity population, Kim et al. evaluated 161 patients with a minimum 5-year follow-up who had undergone long (more than five segments) dorsal constructs to determine the incidence and outcomes associated with PJK. The researchers found that at mean follow-up of 7.8 years, there was a 39% incidence of PJK defined either as a proximal junction sagittal Cobb angle of more than 10 degrees or as a proximal junction sagittal Cobb angle at least 10 degrees greater than the preoperative measurement. The time periods most notable for worsening of PJK were at 8 weeks postoperatively (59%) or after 2 years until final follow-up (35%). Scoliosis Research Society outcome measures did not show any significant difference in those with PJK as compared with those without except with self-image when PJK was more than 20 degrees. Age older than 55 years and combination anterior-posterior surgery were the only significant risk factors identified.10 The time course between the identification of PJK suggests two different populations, given that one group was relatively close to surgery, whereas the other was more remote. Further understanding of the similarities and differences of the early and late group may lead to changes in treatment strategies to better prevent PJK.
Another technique used to avoid PJK as well as strengthen the screw pull-out strength is vertebroplasty. Recently there has been some controversy over the effectiveness of this procedure in the setting of compression fractures, but the concept is applied differently in deformity surgery. At the proximal and sometimes distal screws, polymethylmethacrylate (PMMA) is injected under fluoroscopy into the screw tracks or through the screws themselves if the screw design allows it. Care is taken that there are no pedicle wall breaches allowing the egress of PMMA into the spinal canal or the production of embolic material. Once the PMMA is in place, typically 1 to 2 mL per side, then the pedicle screw is placed. Another scenario is to perform vertebroplasty at the level cephalad to the proximal instrumented vertebrae to prevent compression fractures leading to PJK (Fig. 151-1). Alternatively, this procedure can be performed in a postoperative setting. Preoperative PMMA augmentation of the planned proximal instrumented bodies is not recommended because it increases the difficulty of placement of the instrumentation.
In a cadaveric study designed to look at effects of cement augmentation of pedicle screws compared with extension with a flexible rod, Tan et al. found that in a corpectomy model, cement augmentation significantly reduced the range of motion and resulted in a more stable construct.11 In another cadaveric study, Becker et al. found that pedicle screws augmented with PMMA in an osteoporotic model had increased pull-out strength compared with non-PMMA augmented screws.12 In a cost-effectiveness analysis published in 2008, Hart et al. evaluated 28 women older than 60 years of age who had undergone fusion to the thoracolumbar region. Fifteen of these patients had undergone vertebroplasty in the adjacent level cranial to the proximal instrumented vertebrae. Proximal collapse occurred in none of the patients who had PMMA augmentation and in two (15.3%) patients who did not. Assuming a 15% decrease in the incidence of this problem, the researchers determined that the cost to prevent a single proximal junctional collapse was $46,240 using vertebroplasty, whereas the cost of revising the instrumentation in a patient with proximal junctional collapse was $77,432.13
Interbody Fusion
Interbody fusions are achieved by removing the intervertebral disc and placing fusion material such as autograft, allograft, or osteobiologics. Achieving fusion across the disc space has been shown to provide a biomechanically stiffer construct.3 But can interbody constructs stand alone? In 2006, Anjarwalla et al. evaluated their ALIF patients and divided them into four cohorts: stand-alone ALIF, ALIF with translaminar screws, ALIF with unilateral pedicle screws, and ALIF with bilateral pedicle screws. Using thin-section CT, the investigators reported a fusion rate of 51% in the stand-alone ALIF population, 58% in the ALIF population with translaminar screws, 89% in the ALIF population augmented by unilateral screws, and 88% fusion with ALIF augmented by bilateral pedicle screws.14 Some studies have advocated the use of percutaneous pedicle screws to augment ALIF with good clinical and radiographic results.15 Cadaveric studies have looked at the difference between stand-alone ALIF, ALIF with anterior plate, and ALIF with pedicle screws and found that augmentation of a stand-alone ALIF significantly reduced the range of motion and increased the stiffness of the construct. Overall, there was no consistent significant difference between an anterior plate and pedicle screws except that pedicle screws more effectively limited lateral bending.16,17
Osteotomies
From a spine perspective, osteotomies are cuts made through the spine to allow its mobilization and realignment—typically to correct kyphosis or to enhance lordosis. In general, there are three main types of osteotomies: Ponte or Smith-Petersen osteotomies (SPOs), pedicle subtraction osteotomies (PSOs), and vertebral column resections (VCRs). In ascending order, each of these osteotomies offers greater correctional power and can be used in combination to achieve optimal deformity correction. Prior to the application of osteotomies, one must have a firm understanding of why correction is important as well as the goals of correction.
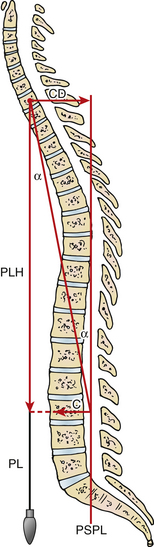
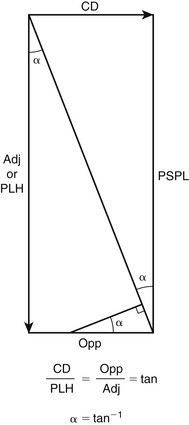
Sagittal balance has been shown to be the single most important factor affecting outcome in adult deformity surgery.4 Sagittal balance is measured by drawing a C7 plumb line and measuring the linear distance from this line to the posterior sacral promontory. Measurements greater than 5 cm correlate with poorer longer-term outcomes. Therefore, the goal is to correct the sagittal balance to within the normal range. However, osteotomies are measured in degrees, not centimeters of correction. Therefore, one must convert the degrees of correction achieved by an osteotomy to a linear distance to ensure successfully restoring sagittal balance.
Global sagittal plane correction is most reliably calculated using the tangent function as described by Ondra et al. (Figs. 151-2 and 151-3).18 This technique allows the conversion of the distance of correction needed to an angle that can be used to determine the size of the osteotomies required. In most radiology systems, this can easily be performed by drawing a C7 plumb line and a sagittal vertical line from the posterior sacral promontory to the center of the C7 vertebral body. This angle represents the overall degree of sagittal plane correction needed for the patient to be in sagittal balance. Once this angle is known, preoperative planning of osteotomies can then be matched with the amount of correction needed. Placement of osteotomies more caudally has a greater effect on sagittal balance as opposed to those that are placed in a more cephalad fashion. The goal is to place the appropriate type, size, and number of osteotomies so that sagittal plane alignment can occur.
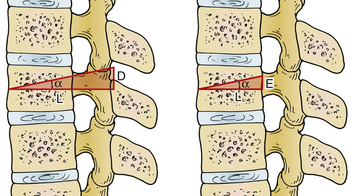
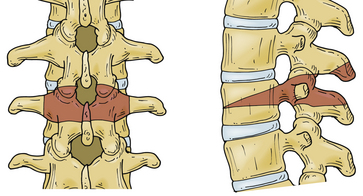
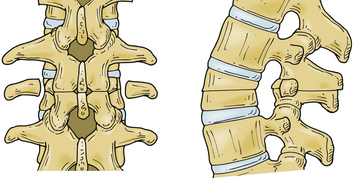
As discussed by Bridwell, SPOs, PSOs, and VCRs can be used to correct fixed sagittal and/or coronal imbalance.19 Although it is beyond the scope of this chapter to discuss details in performing osteotomies, a general understanding is important. An SPO, also termed a chevron osteotomy because of its shape, is performed by removing the posterior column, bone, and ligament, between the facet joints at one or multiple levels while leaving the middle and anterior columns intact. With posterior compression, the anterior column opens through the disc space, providing increased lordosis. In general, an SPO can provide 5 to 10 degrees of lordosis. An important caveat in performing an SPO is to ensure complete removal of the superior facet so that compression does not entrap the exiting nerve root within the foramen.
A PSO is a V-shaped resection through the posterior elements, pedicles, and vertebral body that hinges through the bone. Dorsal compression results in bone on bone closure that can provide 25 to 35 degrees of lordosis. Including the disc space above can provide additional corrective forces and is sometimes referred to as a 1½ PSO or an extended PSO. PSOs are often used in the lumbar spine and are useful in correction of iatrogenic flat back deformity (Figs. 151-4 to 151-8).
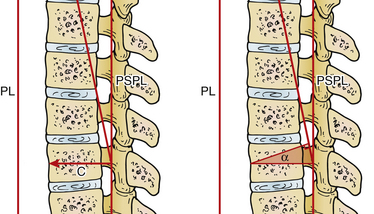
FIGURE 151-4 Applying the geometric proof illustrated in Figure 151-3 to the spine, the angle of correction (α) required is cut through the vertebral body. PL, plumb line; PSPL, posterior sacral promontory line .
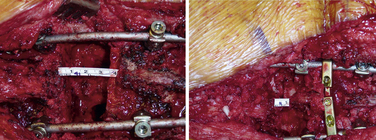
FIGURE 151-8 Intraoperative pictures showing a completed pedicle subtraction osteotomy before and after compression.
When a pedicle subtraction osteotomy or vertebral column resection is performed, one side of the construct has a temporary rod to prevent spinal column translation. After the osteotomy is complete, compression is required to close the construct to gain the correction for which the osteotomy was performed. Often this is done by placing a permanent rod on the contralateral side and compressing against the pedicle screws. The potential problem with this is that the compression places an extra force on the pedicle screw, which may result in the screw breaking out of the pedicle, losing an important fixation point in the construct. An alternative method is to place two temporary rods on each side of the construct where the free ends of the rods meet at the osteotomy site. Domino connectors are then placed across the rods and tightened. The same is performed on the other side, and the rod is secured to the pedicle screw heads. After gaining control of the construct with bilateral compression devices, the screws for either the cephalad or caudal rod are loosened. Compression can occur across the connector. It is important that with bilateral compression the same rod, either rostral or caudal, is chosen to be tightened so that symmetrical compression can occur. Although compression still occurs on one set of the pedicle screws, it can be alternated so smaller amounts of force are required for closure. Alternatively, others have described using laminar hooks rostral and caudal to the osteotomy site in a claw construct and closing the osteotomy with a temporary rod that spans the laminar hooks. This takes all force off of the pedicle screws until the permanent rod is placed.
Cross-Fixators
Cross-fixators are not an unusual component of instrumentation, and it is worth discussing their rationale and use. The purpose of placing cross-links, also termed transverse connectors, is to reduce rotational forces on the spine. Although cadaveric studies have shown that cross-fixators increase rotational, lateral bending, and flexion stiffness, resistance to rotation has been the most consistent finding.20,21 In one such study by Kuklo et al., the authors found that a pedicle screw construct from T4-10 with 5.5-mm- diameter titanium pedicle screws with 5.5-mm titanium rods resulted in a 65% decrease in the range of motion compared with the uninstrumented spine. The addition of one cross-fixator anywhere along the construct resulted in decreased rotational motion, but it was the placement of a second cross-fixator, one at the rostral and one at the caudal portion of the construct, which provided the greatest stability with a 35% reduction in rotational motion compared with no cross-fixators. Flexion-extension and lateral bending were not significantly affected by the addition of cross-fixators. The authors concluded that in the thoracic spine, where the primary motion is rotation, the use of two cross-fixators provides superior resistance to that motion and therefore a more stable construct.21
Hybrid Constructs
Pedicle screws provide for three-column control of the spine, allowing for greater forces to be imparted in order to achieve deformity correction. Currently, the role of hooks is often relegated as a revision strategy if placement of the pedicle screw fails. However, there is some thought that using hooks in combination with pedicle screws, a hybrid construct, theoretically provides a construct resistant to different modes of failure. When evaluating resistance to failure from dorsally directed forces in a cadaveric model, Coe et al. showed that laminar hooks were superior to spinous process wires and pedicle screws.22 Hilibrand et al. showed that combining a supralaminar hook with a pedicle screw provided increased pull-out strength in models replicating osteoporotic or compromised pedicle. There was no difference, however, between the two when the pedicle was intact.23 In the osteoporotic spine, where the cortical bone is spared relative to the cancellous bone, a fixation technique that relies more on the cortical bone, such as a hook, can be used. Typically, hooks are used in a hybrid fashion on one side of the cranial aspect of the construct (Fig. 151-9). Hooks do not have the same corrective power as pedicle screws and do not provide a construct as stiff as that of pedicle screws. Jones et al. evaluated whether a short-segment thoracic hybrid construct is equivalent to a pedicle screw construct. They found that there was a greater force required for construct failure in the pedicle screw group and that these constructs were significantly stiffer than the hybrid constructs.24 In 2007, Lowenstein et al. looked at a cohort of 34 patients, comparing an all-pedicle-screw construct with a hybrid construct consisting of lumbar pedicle screws and thoracic hooks in a population with AIS. The investigators found that there were no statistically significant differences between the two constructs in coronal plane sagittal balance correction, although there was a significant differences in kyphosis correction.25 Kuklo et al. looked at the revision rates of various constructs in patients with AIS. These researchers found that hybrid constructs had a statistically significant higher failure rate than pedicle constructs.26 The population with AIS, with relatively healthy bone, likely would not see the benefits of a hybrid construct, compared with the osteoporotic spine where hooks can take advantage of the relatively stronger cortical bone.
Multirod Constructs
On rare occasions, revision cases sometimes require a multirod construct. These are constructs where the rods are placed in alternating pedicle screws. The rods are attached to each other with connectors and cross-fixators to make an integrated rod system. The focus of such a construct is to provide alternating stress points and to distribute the force along the construct more evenly. This concept has been described by Shen et al., where researchers used four rods to cross the lumbosacral junction.27 By using four different anchoring points within the pelvis, the rods span the junction to the lumbar fixation points and are coupled using cross-fixators.
Bridwell K.H. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976). 2006;31:S171-S178.
Bridwell K.H. Selection of instrumentation and fusion levels for scoliosis: where to start and where to stop. Submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1:1-8.
Edwards C.C.II, Bridwell K.H., Patel A., et al. Thoracolumbar deformity arthrodesis to L5 in adults: the fate of the L5-S1 disc. Spine (Phila Pa 1976). 2003;28:2122-2131.
Glassman S.D., Bridwell K., Dimar J.R., et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30:2024-2029.
Ondra S.L., Marzouk S., Koski T., et al. Mathematical calculation of pedicle subtraction osteotomy size to allow precision correction of fixed sagittal deformity. Spine (Phila Pa 1976). 2006;31:E973-E979.
Polly D.W.Jr., Klemme W.R., Cunningham B.W., et al. The biomechanical significance of anterior column support in a simulated single-level spinal fusion. J Spinal Disord. 2000;13:58-62.
1. Bridwell K.H. Selection of instrumentation and fusion levels for scoliosis: where to start and where to stop. Submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1:1-8.
2. Edwards C.C.II, Bridwell K.H., Patel A., et al. Thoracolumbar deformity arthrodesis to L5 in adults: the fate of the L5-S1 disc. Spine (Phila Pa 1976). 2003;28:2122-2131.
3. Polly D.W.Jr., Klemme W.R., Cunningham B.W., et al. The biomechanical significance of anterior column support in a simulated single-level spinal fusion. J Spinal Disord. 2000;13:58-62.
4. Glassman S.D., Bridwell K., Dimar J.R., et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30:2024-2029.
5. Hsieh P.C., Koski T.R., O’Shaughnessy B.A., et al. Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine. 2007;7:379-386.
6. Lehman R.A.Jr., Kuklo T.R., Belmont P.J.Jr., et al. Advantage of pedicle screw fixation directed into the apex of the sacral promontory over bicortical fixation: a biomechanical analysis. Spine (Phila Pa 1976). 2002;27:806-811.
7. Tumialan L.M., Mummaneni P.V. Long-segment spinal fixation using pelvic screws. Neurosurgery. 2008;63:A183-A190.
8. Kuklo T.R., Bridwell K.H., Lewis S.J., et al. Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine (Phila Pa 1976). 2001;26:1976-1983.
9. Lee G.A., Betz R.R., Clements D.H.III, Huss G.K. Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine (Phila Pa 1976). 1999;24:795-799.
10. Kim Y.J., Bridwell K.H., Lenke L.G., et al. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976). 2008;33:2179-2184.
11. Tan J.S., Singh S., Zhu Q.A., et al. The effect of cement augmentation and extension of posterior instrumentation on stabilization and adjacent level effects in the elderly spine. Spine (Phila Pa 1976). 2008;33:2728-2740.
12. Becker S., Chavanne A., Spitaler R., et al. Assessment of different screw augmentation techniques and screw designs in osteoporotic spines. Eur Spine J. 2008;17:1462-1469.
13. Hart R.A., Prendergast M.A., Roberts W.G., et al. Proximal junctional acute collapse cranial to multi-level lumbar fusion: a cost analysis of prophylactic vertebral augmentation. Spine J. 2008;8:875-881.
14. Anjarwalla N.K., Morcom R.K., Fraser R.D. Supplementary stabilization with anterior lumbar intervertebral fusion—a radiologic review. Spine (Phila Pa 1976). 2006;31:1281-1287.
15. Lee S.H., Kang B.U., Jeon S.H., et al. Revision surgery of the lumbar spine: anterior lumbar interbody fusion followed by percutaneous pedicle screw fixation. J Neurosurg Spine. 2006;5:228-233.
16. Gerber M., Crawford N.R., Chamberlain R.H., et al. Biomechanical assessment of anterior lumbar interbody fusion with an anterior lumbosacral fixation screw-plate: comparison to stand-alone anterior lumbar interbody fusion and anterior lumbar interbody fusion with pedicle screws in an unstable human cadaver model. Spine (Phila Pa 1976). 2006;31:762-768.
17. Johnson W.M., Nichols T.A., Jethwani D., Guiot B.H. in vitro biomechanical comparison of an anterior and anterolateral lumbar plate with posterior fixation following single-level anterior lumbar interbody fusion. J Neurosurg Spine. 2007;7:332-335.
18. Ondra S.L., Marzouk S., Koski T., et al. Mathematical calculation of pedicle subtraction osteotomy size to allow precision correction of fixed sagittal deformity. Spine (Phila Pa 1976). 2006;31:E973-E979.
19. Bridwell K.H. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976). 2006;31:S171-S178.
20. Lynn G., Mukherjee D.P., Kruse R.N., et al. Mechanical stability of thoracolumbar pedicle screw fixation. The effect of crosslinks. Spine (Phila Pa 1976). 1997;22:1568-1572.
21. Kuklo T.R., Dmitriev A.E., Cardoso M.J., et al. Biomechanical contribution of transverse connectors to segmental stability following long segment instrumentation with thoracic pedicle screws. Spine (Phila Pa 1976). 2008;33:E482-E487.
22. Coe J.D., Warden K.E., Herzig M.A., McAfee P.C. Influence of bone mineral density on the fixation of thoracolumbar implants. A comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine (Phila Pa 1976). 1990;15:902-907.
23. Hilibrand A.S., Moore D.C., Graziano G.P. The role of pediculolaminar fixation in compromised pedicle bone. Spine (Phila Pa 1976). 1996;21:445-451.
24. Jones G.A., Kayanja M., Milks R., Lieberman I., et al. Biomechanical characteristics of hybrid hook-screw constructs in short-segment thoracic fixation. Spine (Phila Pa 1976). 2008;33:173-177.
25. Lowenstein J.E., Matsumoto H., Vitale M.G., et al. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine (Phila Pa 1976). 2007;32:448-542.
26. Kuklo T.R., Potter B.K., Lenke L.G., et al. Surgical revision rates of hooks versus hybrid versus screws versus combined anteroposterior spinal fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2007;32:2258-2264.
27. Shen F.H., Harper M., Foster W.C., et al. A novel “four-rod technique” for lumbo-pelvic reconstruction: theory and technical considerations. Spine (Phila Pa 1976). 2006;31:1395-1401.