CHAPTER 51 Dorsal Radiocarpal Ligament Tears
Various authors have cast light on the importance of the dorsal radiocarpal ligament (DRCL) in maintaining carpal stability.1–4 Tears of the DRCL have been linked to the development of volar and dorsal intercalated segmental instabilities and may be implicated in the development of midcarpal instability.5–7 Despite this growing body of evidence, there is still a paucity of literature on the incidence of DRCL tears. An isolated tear of the DRCL also can be a source of chronic wrist pain.8 The existence of a DRCL tear when combined with a tear of a primary wrist stabilizer indicates a chronic lesion, which may negatively affect the prognosis after treatment.9,10
In most series, the DRCL is overlooked during the typical arthroscopic examination of the wrist. It is hard to visualize a DRCL tear through the standard dorsal wrist arthroscopy portals because the torn edge of the DRCL tends to float up against the arthroscope while viewing through the 3,4 and 4,5 portals, which makes identification and repair of the DRCL tear cumbersome. It can be seen obliquely through the 1,2 and 6U portals, but visualization of the DRCL across the radiocarpal joint may be laborious in a tight or small wrist, especially if synovitis is present. Wrist arthroscopy through a volar radial portal (VR) is the ideal way to assess the DRCL because of the straight line of sight.11–13
Clinical Relevance
Elsaidi and colleagues14 showed the importance of the DRCL on scaphoid kinematics through a series of sectioning studies. They sequentially divided the radioscaphocapitate, long radiolunate, radioscapholunate, and short radiolunate ligaments. They next divided the central and proximal scapholunate interosseous ligament (SLIL), then the dorsal SLIL, and finally the dorsal capsule insertion on the scaphoid. There was no appreciable change in the radiographic appearance of this wrist. When the DRCL was divided, a dorsal intercalated segmental instability deformity occurred.
In another series of biomechanical studies on ligament sectioning using 24 cadaver arms, Short and coworkers15 determined that the SLIL is the primary stabilizer of the scapholunate articulation, and that the DRCL, the dorsal intercarpal ligament, the scaphotrapezial ligament, and the radioscaphocapitate ligament are secondary stabilizers. They found that dividing the dorsal intercarpal or scaphotrapezial ligament alone followed by 1000 cycles of wrist flexion-extension and radial-ulnar deviation had no effect on scaphoid and lunate kinematics. Dividing the DRCL alone did cause increased lunate radial deviation when the wrist was in maximum flexion. Dividing the SLIL after any of the ligaments tested produced increased scaphoid flexion and ulnar deviation while the lunate extended. Short and coworkers15 also hypothesized that cyclic motion seems to cause further deterioration in carpal kinematics owing to plastic deformation in the remaining structures that stabilize the scapholunate.
These data provide a rationale for repairing the DRCL. The data also suggest that consideration should be given to augmenting the stability of the scaphotrapezial ligaments concomitant with treatment of the SLIL instability. Similar studies have established that the triangular fibrocartilage complex (TFCC) and the dorsal and volar radioulnar ligaments are primary stabilizers of the ulnocarpal joint.16 DRCL tears that are found during the arthroscopic treatment of ulnar-sided lesions are handled in a similar fashion.
Indications
Geissler and colleagues17 proposed an arthroscopic grading scale of interosseous ligament instability that has gained wide acceptance. In Geissler grade 1 and 2 lesions, there is no to minimal instability owing to ligament attenuation, but no tearing; these are synonymous with a dynamic instability. Grade 3 and 4 lesions represent partial and complete tears with greater degrees of carpal instability. This classification quantifies the resultant instability, and not the actual size of the tear. Based on this grading scale, an arthroscopic classification of DRCL tears is proposed in Table 51-1.
TABLE 51-1 Classification of Dorsal Radiocarpal Ligament Tears*
| Stage 1 | Isolated DRCL tear |
| Stage 2 | DRCL tear with associated SLIL or LTIL instability (Geissler grade 1/2) and/or TFCC tear |
| Stage 3A | DRCL tear with associated SLIL or LTIL tear (Geissler grade 3) and/or TFCC tear |
| Stage 3B | DRCL tear with associated SLIL or LTIL tear (Geissler grade 4) and/or TFCC tear |
| Stage 4 | Chondromalacia with widespread carpal pathology |
DRCL, dorsal radiocarpal ligament; LTIL, lunotriquetral interosseous ligament; SLIL, scapholunate interosseous ligament; TFCC, triangular fibrocartilage complex.
* The ligament with the highest Geissler grade determines the stage.
The treatment of DRCL tears is summarized in Table 51-2. An arthroscopic repair is indicated for isolated DRCL tears, which often leads to resolution of the wrist pain.8,10 DRCL tears are commonly associated with SLIL tears or instability or both. Geissler grade 1 and 2 SLIL injuries are still amenable to arthroscopic treatment. In these situations, an arthroscopic repair of any associated DRCL tears is indicated because it may augment the coronal stability of the SLIL repair.8–10 In open SLIL repairs, sagittal plane stability is often supplemented by adding a dorsal capsulodesis or using a tendon weave, such as the modified Brunelli procedure. Arthroscopic thermal shrinkage of the scaphotrapezial ligaments also theoretically may enhance the sagittal plane stability of the scapholunate joint. This is currently under investigation, but no data are available to recommend this procedure as yet.
TABLE 51-2 Treatment of Dorsal Radiocarpal Ligament Tears
| Stage 1 | Arthroscopic DRCL repair |
| Stage 2 | Arthroscopic DRCL repair, SLIL or LTIL débridement ± shrinkage, TFCC repair/débridement ± wafer |
| Stage 3A | Arthroscopic DRCL repair, SLIL or LTIL shrinkage + pinning, TFCC repair/débridement ± wafer (consider scaphotrapezial ligament shrinkage) |
| Stage 3B | Open SLIL repair/reconstruction ± capsulodesis, LTIL repair/reconstruction, TFCC repair/débridement ± wafer/ulnar shortening |
| Stage 4 | Partial carpal fusion versus PRC |
DRCL, dorsal radiocarpal ligament; LTIL, lunotriquetral interosseous ligament; PRC, proximal row carpectomy; SLIL, scapholunate interosseous ligament; TFCC, triangular fibrocartilage complex.
Geissler grade 3 SLIL injuries represent a relative gray area for arthroscopic treatment methods alone. Investigators have shown, however, that this type of ligament injury can be treated successfully with thermal shrinkage and pinning. In the author’s view, any associated DRCL tears should be repaired arthroscopically at the same time. Tears or instability of the lunotriquetral interosseous ligament are treated in similar fashion to the SLIL. DRCL repairs are indicated for Geissler grade 1 and 2 lunotriquetral interosseous ligament injuries and can be combined with lunotriquetral interosseous ligament shrinkage and débridement with or without pinning. Because there is a marked association of DRCL tears in the presence of long-standing TFCC tears, in my view DRCL repairs should be performed concomitantly with débridement or repair of the TFCC tear.
Contraindications
In cases in which the treatment of an SLIL tear or dynamic scapholunate instability includes some type of dorsal capsulodesis, the dorsal incision followed by the creation of a dorsal capsular checkrein to restrain palmar flexion of the scaphoid renders any separate treatment of the DRCL tear unfeasible. When the DRCL tear is seen in association with palmar midcarpal instability, a soft tissue repair of the dorsal ligaments would not by itself correct the midcarpal instability.18 The results of a DRCL repair in association with two or more other intracarpal lesions are often inconsistent, and open repair methods should be considered, especially if they include a Geissler grade 3 ligament injury.9 Geissler grade 4 ligament injuries are beyond the realm of arthroscopic treatment and require open repair or reconstruction (see Table 51-2).
Surgical Technique (Video)
A 2.7-mm, 30-degree arthroscope is inserted through the cannula. The repair is performed by spearing the radial side of the DRCL tear with a curved 21-gauge spinal needle placed through the 3,4 portal while viewing through the arthroscope in the VR portal. A 2-0 absorbable suture is threaded through the spinal needle and retrieved with a grasper or suture snare inserted through the 4,5 portal (Fig. 51-1A-F). A curved hemostat is used to pull either end of the suture underneath the extensor tendons, and the knot is tied either at the 3,4 portal or at the 4,5 portal. The repair is augmented with thermal shrinkage if the torn edge of the DRCL is voluminous and still protrudes into the joint after the sutures are tied (Fig. 51-1H).
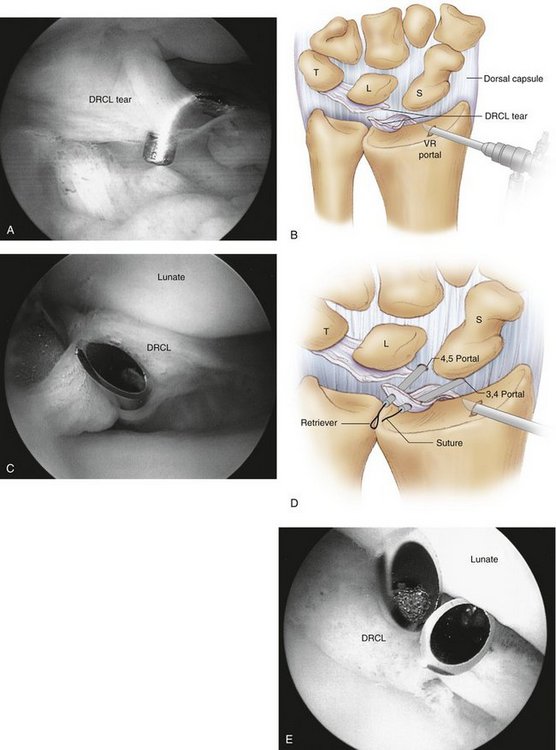
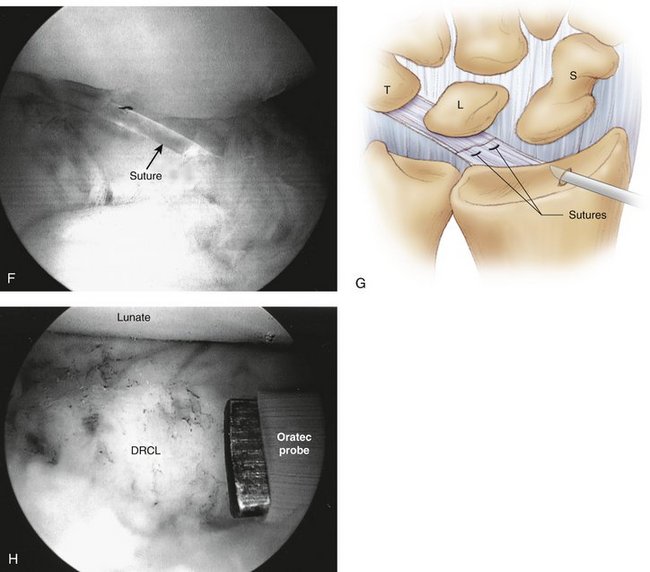
FIGURE 51-1 Outside-in dorsal radiocarpal ligament (DRCL) repair technique. A, Arthroscopic view of DRCL tear from the VR portal. B, Drawing of DRCL tear. C, Insertion of curved spinal needle through edge of DRCL tear. D, Drawing of outside-in technique using two spinal needles and a suture retriever. E, Insertion of second spinal needle. F, Arthroscopic view of suture loop before tying. G, Drawing of completed repair. H, Repair augmented with thermal shrinkage after suture has been tied.
(A, C, E, F, and H from Slutsky DJ: Clinical applications of volar portals in wrist arthroscopy. Tech Hand Upper Extrem Surg. 2004; 8:229-238; B, D, and G from Slutsky DJ: Arthroscopic repair of dorsal radiocarpal ligament tears. J Arthrosc Related Surg. 2005; 21:1486e1-1486e8.)
Clinical Studies
A retrospective chart review of 21 patients who underwent a DRCL repair was published in 2005. None of the wrists showed a static carpal instability pattern on x-ray. Preoperative magnetic resonance imaging (MRI) was performed by the referring physician in six patients. Preoperative arthrograms were performed as a part of the diagnostic workup for wrist pain in 20 patients. None of the DRCL tears in this series were identified with preoperative arthrography or MRI. Preoperative MRI in one patient with a DRCL tear was misinterpreted as representing a dorsal wrist ganglion. There were 6 men and 16 women. The average patient age was 40 years (range 25 to 62 years). All patients failed a trial of conservative treatment with wrist immobilization, cortisone injections, and work restrictions. The average length of conservative treatment was 7 months. The time interval between injury and surgical intervention averaged 25 months (range 8 to 53 months).
The four patients who underwent an isolated DRCL repair were satisfied with the outcome of surgery and would repeat the surgery again because it improved their symptoms. All four patients graded their pain as none or mild. None of these patients were taking pain medications. All returned to their previous occupations without restriction. Their wrist motion was unchanged compared with the preoperative status. Grip strengths were 90% to 130% of the opposite side.
A dorsal capsulodesis was performed as the primary treatment for an SLIL tear or a dynamic scapholunate instability in seven patients instead of a DRCL repair. The capsulodesis was ineffective in controlling pain in the remaining four patients, three of whom had additional wrist pathology. This is consistent with other studies, which have shown that although pain is improved, it does not resolve completely after a dorsal capsulodesis in most cases.19 Cadaver studies suggest that dynamic scaphoid instability results from an isolated injury to the SLIL without damage to the dorsal intercarpal and DRCL ligaments.4 I found the corollary to hold true in that four of seven patients with dynamic scapholunate instability had a DRCL tear, but an intact scapholunate ligament.
1. Short WH, Werner FW, Green JK, et al. The effect of sectioning the dorsal radiocarpal ligament and insertion of a pressure sensor into the radiocarpal joint on scaphoid and lunate kinematics. J Hand Surg [Am]. 2002;27:68-76.
2. Mitsuyasu H, Patterson RM, Shah MA, et al. The role of the dorsal intercarpal ligament in dynamic and static scapholunate instability. J Hand Surg [Am]. 2004;29:279-288.
3. Viegas SF, Yamaguchi S, Boyd NL, et al. The dorsal ligaments of the wrist: anatomy, mechanical properties, and function. J Hand Surg [Am]. 1999;24:456-468.
4. Ruch DS, Smith BP. Arthroscopic and open management of dynamic scaphoid instability. Orthop Clin North Am. 2001;32:233-240.
5. Viegas SF, Patterson RM, Peterson PD, et al. Ulnar-sided perilunate instability: an anatomic and biomechanic study. J Hand Surg [Am]. 1990;15:268-278.
6. Moritomo H, Viegas SF, Elder KW, et al. Scaphoid nonunions: a 3-dimensional analysis of patterns of deformity. J Hand Surg [Am]. 2000;25:520-528.
7. Horii E, Garcia-Elias M, An KN, et al. A kinematic study of luno-triquetral dissociations. J Hand Surg [Am]. 1991;16:355-362.
8. Slutsky DJ. Arthroscopic repair of dorsal radiocarpal ligament tears. Arthroscopy. 2002;18:E49.
9. Slutsky D. Arthroscopic repair of dorsoradiocarpal ligament tears. J Arthrosc Related Surg. 21:1486e1-1486e8, 2005.
10. Slutsky DJ. Management of dorsoradiocarpal ligament repairs. J Am Soc Surg Hand. 2005;5:167-174.
11. Slutsky DJ. Wrist arthroscopy through a volar radial portal. Arthroscopy. 2002;18:624-630.
12. Slutsky DJ. Volar portals in wrist arthroscopy. J Am Soc Surg Hand. 2002;2:225-232.
13. Slutsky DJ. Clinical applications of volar portals in wrist arthroscopy. Tech Hand Upper Extrem Surg. 2004;8:229-238.
14. Elsaidi GA, Ruch DS, Kuzma GR, et al. Dorsal wrist ligament insertions stabilize the scapholunate interval: cadaver study. Clin Orthop. 2004;425:152-157.
15. Short WH, Werner FW, Green JK, et al. Biomechanical evaluation of the ligamentous stabilizers of the scaphoid and lunate: part III. J Hand Surg [Am]. 2007;32:297-309.
16. Palmer AK, Werner FW. The triangular fibrocartilage complex of the wrist—anatomy and function. J Hand Surg [Am]. 1981;6:153-162.
17. Geissler WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357-365.
18. Goldfarb CA, Stern PJ, Kiefhaber TR. Palmar midcarpal instability: the results of treatment with 4-corner arthrodesis. J Hand Surg [Am]. 2004;29:258-263.
19. Moran SL, Cooney WP, Berger RA, et al. Capsulodesis for the treatment of chronic scapholunate instability. J Hand Surg [Am]. 2005;30:16-23.