CHAPTER 10 Dorsal Plate Fixation
The dorsal approach to treating distal radius fractures has fallen into disfavor during the past few years because of reports of problems with tendon irritation, ruptures, and fracture collapse that occurred with plates that were anatomically correct but had a relatively high profile.1–3 Discouraged by these results, the focus turned to the volar approach,4,5 and the dorsal plates went out of fashion even though new plates with a lower profile were introduced to the market. Lately, new literature has confirmed that the results of dorsal plating are comparable to those of the volar approach.6,7 The use of low-profile, anatomically contoured plating systems results in a reduction of extensor tendon irritation while providing stable bony fixation. To our minds, the big advantage of the dorsal plate fixation for dorsally displaced fractures is the direct visualization of the dorsal defects that are created by the collapse and multifragmentation present in most of these injuries, especially in the senior population. We have been placing two different types of plates in the distal radius: a stainless steel, nonlocking plate (Locon-T by Wright Medical, Arlington, TN) and a titanium locking plate (Stryker Universal distal radius system by Stryker, Kalamazoo, MI). The Locon-T plate is 1.2-mm thick with the screws fully engaged. The distal radius T portion varies and can accommodate from 3 to 5 2.7-mm screws, depending on the size of the plate. The stem is 3.5-cm long and accepts 3.5-mm screws. The advantages of the stainless steel plate are malleability and a very anatomical design. The advantages of the titanium plates are the strength and the locking screws, with virtually no profile increase, both important in the treatment of osteopenic patients.
Indications
The ideal candidate for low-profile dorsal plating is a patient with a multifragmented dorsally displaced fracture of the distal radius with dorsal bony defects, due to a high-velocity injury or the presence of osteoporosis. The indications include unstable fractures that have previously undergone closed reduction and splinting with unsuccessful reduction or loss of reduction. This includes extra-articular fractures (AO type A), intra-articular shear fractures (AO type B), and comminuted intra-articular fractures with metaphyseal comminution (AO type C). Some authors use the criteria of more than 20 degrees of dorsal angulation, radial shortening of more than 2 mm, or articular incongruity between 1 and 2 mm.6 The age range of patients for the procedure encompasses adolescents at the age of closure of the epiphyses to those in their nineties. It is often better to wait 5 to 7 days after injury to treat these fractures if there is no neurologic or vascular compromise. The reasons are better visualization of the fracture fragments, stabilization of health situations, decrease in the edema of the wrist and fingers, and better understanding of the procedure by patients and their families. We have used the dorsal plates in all types of fractures of the distal radius, including complex intra-articular multifragmented fractures, classified as C1, C2, and C3 by the AO classification system. In C3.3 fractures there might be a call for additional stabilization of the radius shaft fracture component, and we obtain reduction with extra screws taken from the distal radius set or an occasional Kirshner wire.
Surgical Technique
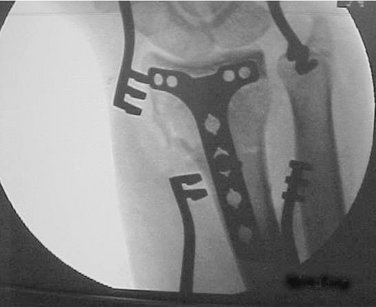
Under general or brachial block anesthesia, the forearm is prepped and draped to the elbow area. A fluoroscopy preliminary film is obtained to confirm the deformities and the initial impressions. Following that, traction is applied to the index and ring fingers by Chinese finger traps with cords that are attached to a traction apparatus clamped to the operating-hand-procedure side table (Schlein Hand Positioner with rail attachment; Allen Medical Systems, Acton, MA) (Fig. 10-1). In case of doubt and in severe multifragmented fractures, the fluoroscopy film is repeated after traction has been applied. This is a very useful maneuver because in some situations the real severity of the comminution is revealed in this post-traction film rather than in the resting position.
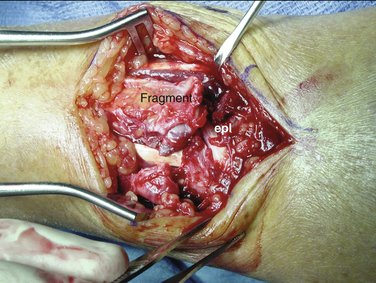
Under tourniquet control, a 5- to 6-cm dorsal longitudinal incision is made spanning the wrist joint and the distal forearm and deepened to the extensor retinaculum. The third dorsal space is incised obliquely following the direction of the extensor pollicis longus (EPL) tendon (Fig. 10-2). A hematoma is often present in the third dorsal space, and the identification of the tendon direction is facilitated by the presence of blood. At this point, we also open the second dorsal space longitudinally, exposing the extensor carpi radialis longus and brevis and freeing the tubercle of Lister. One of the interesting findings in severely comminuted fractures is that the EPL tendon can be caught between the displaced fracture fragments, and one has to extricate the tendon from the fragments (Fig. 10-3). In those cases, immediate visualization of the tendon is not easy and the surgeon might have to look for the tendon more distally and follow it to the fracture site. That happens in 2% of cases, in our empirical observation, but it is significant because traction applied to the hand and wrist will push the tendon farther into the separation between the fragments, making the reduction of the fracture impossible prior to dissection and extraction of the tendon. This situation would be impossible to recognize if such a fracture were being treated using the volar approach.
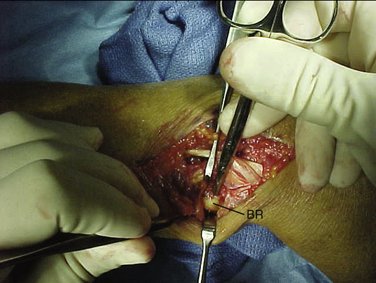
If the radial fracture fragment is translated toward the radial side and it involves a large portion of the radius styloid, it may not be reducible by traction alone. In these situations, we perform a tenotomy of the brachioradialis tendon as it inserts into the displaced fragment. The first dorsal space tunnel is incised and the contents are exposed. At the floor of that space, one can encounter the tendon of the brachioradialis, which is separate from the extensor pollicis brevis and the abductor pollicis longus.10 The brachioradialis tendon is tenotomized transversely, which greatly facilitates the reduction maneuvers for that fragment (Fig. 10-4).
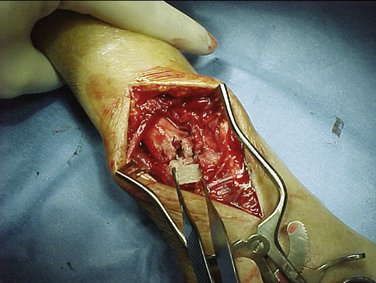
Usually in an elderly patient there is a large bone defect in the dorsal aspect of the radius (Fig. 10-5). For many years now, we have been using iliac crest bone allograft chips previously reconstituted in saline to fill this void (Fig. 10-6). The bone chips are excellent in this situation because they provide internal support and augment the bone stock, preventing collapse of the distal fragments.
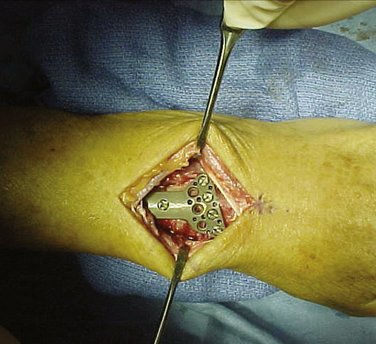
A dorsal plate is chosen according to the size of the radius and the side affected, and it is temporarily applied to the reduced fracture. Usually we use Locon-T plates because they fit the fractures well, have variable sizing, and are malleable. The other plate that we have used is the Stryker plate, which has the advantage of having locking screws; therefore it is used in situations in which there is great comminution in a severely osteoporotic patient. Nevertheless, the Stryker plate is somewhat bulky and stiff, making it less versatile (Fig. 10-7).
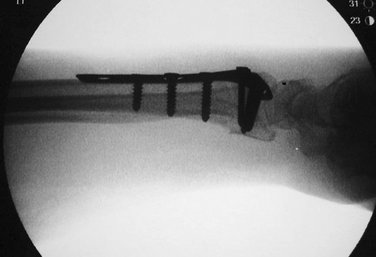
The position of the plate is chosen under fluoroscopy. One of the advantages of the Locon-T plate is that it can be positioned all the way to the edge of the dorsal radius distally to treat a shearing fracture that does not have a large distal fragment. Once the size and position of the plate have been established, the first screw is applied. Often the plate is separated from the bone by a couple of millimeters, and placement of the first screw brings the plate into intimate contact with the dorsal cortex. One should be able to estimate the length of the screw to be applied by subtracting the cortex/plate separation ahead of time; otherwise the first screw will be too long and have to be replaced later. The first 3.5-mm screw is placed in the oblong screw hole, which is located in the shaft portion of the plate. Another film is obtained after the placement of the first screw so as to demonstrate the new position of the plate after tightening the screw. Often we have to move the plate distally or proximally when distal fragments are pushed volarly by the first screw and plate. Therefore, in most cases it is wise to place the first screw in the middle of the oblong hole so that one has the leeway to move the plate either way, if necessary (Fig. 10-8).
The distal screws are applied at this time. Distal measurements can be a problem because of the poor quality of bone in the elderly and the comminution of the fracture. Added to that difficulty is the fact that the drill used distally is a 2-mm drill. Therefore, after the placement of the first 2.7-mm screw distally, a lateral film should be performed to determine whether the screw is of adequate size. The other screws are applied following that guideline (Fig. 10-9). As a very crude practical rule, the distal screws are roughly 4 mm longer than the most distal screw placed in the shaft; hence, an 18-mm distal shaft screw would correspond to a 22-mm distal fragment screw.
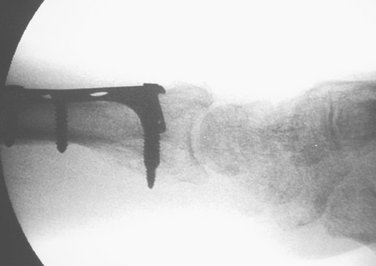
After all screws have been applied distally, assessment of the final fixation is made. Sometimes a small intra-articular dorsal fragment is left unsecured after the plate has been applied. In those cases we use the small extender that is provided in the tray. This extender fits distally and it has two holes, one that attaches to the plate with a regular 2.7-mm screw and one that is placed on top of the unsecured fragment and accepts a 1.8-mm screw. The extender can be attached to any dorsal screw hole and has helped on many occasions to secure a central fragment (Fig. 10-10) or a fragment in the radial or ulnar side of the distal radius (Fig. 10-11).
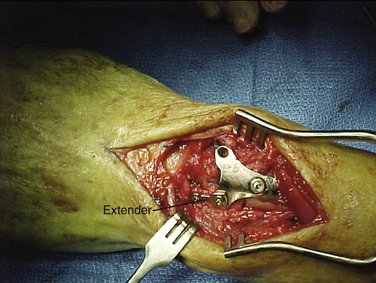
FIGURE 10-10 Plate extender (Extender) in place, securing a small, centrally located fracture fragment.

FIGURE 10-11 Radiograph of Locon-T plus extender (Extender) securing radially placed dorsal fragment.
After placement of all screws, final films are obtained, and the extensor retinaculum is closed partially, leaving the EPL free dorsal to the repair. Skin is approximated using horizontal mattress sutures of 5-0 nylon, and a large dressing and a volar splint are applied. A typical moderately severe case is illustrated in Figures 10-12 through 10-16.
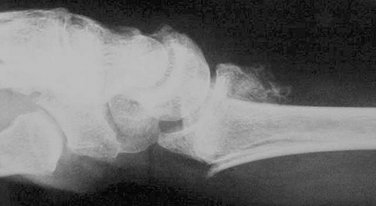
FIGURE 10-13 Radiograph, same fracture, lateral view with greater than 20 degrees of dorsal displacement.
Rehabilitation
Virtually all patients whose distal radius fractures are reduced surgically are treated as outpatients. The dressing is changed 2 days later in the office and a plaster splint is applied. The postsurgical regimen consists of immobilization for 3 weeks in a splint or cast. Range of motion exercises in the hand therapy department start after cast removal. We have attempted immediate mobilization as described in the literature4 but have found that patients tolerate the exercises better and experience less swelling and pain if the therapy is started at 3 weeks. Strengthening starts at 5 to 7 weeks, and the patients are reviewed for the last time prior to discharge at 3 months.
Complications
Aside from the usual complications related to residual stiffness of flexion-extension and pronation-supination that are inherent in any treatment of distal radius fractures, the complications to be expected from the dorsal approach are irritation of the extensor tendons by tendinitis and possible rupture and loosening of the screws.1,9 Tendinitis has not been a major concern when plates are employed. After the insertion of more than 100 plates, only two patients experienced tendinitis—one 2 months after surgery and one 2 years after surgery. The second one may have had an intersection syndrome unrelated to the plate. Both of them were treated with rest and nonsteroidal anti-inflammatory drugs and responded well.
Screw loosening at the distal fragment is a slightly bigger problem with Locon-T plates; we have seen it happen in roughly 5% of patients. We have removed only two screws that were very prominent during the past 7 years of using the plate. No plate removals were necessary. In contrast, there has been no screw-loosening problem with the Stryker plate. It is therefore a better option for the very osteopenic patient. The design of the screw hole in the Stryker plate permits locking with no increase in the profile and allows for locking the screws at various angles, which is a distinct advantage in situations where poor bone stock or a lot of comminution is present.
Results
The objectives of our treatment were:
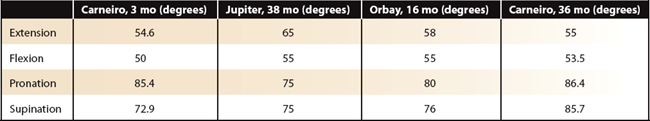
The results were measured initially at 3 months, when the patients were discharged from therapy. The patients were recalled at 36 months and re-examined. Flexion-extension and pronation-supination figures were compared to two articles in the literature—one utilizing dorsal and volar approaches (Jupiter and colleagues11) and one employing a volar approach only (Orbay and colleagues4). These articles referred to 20 patients measured at 38 months and 26 patients measured at 16 months, respectively. The comparison is illustrated in Table 10-1.
Additional Comments
Because the approach is simple and relatively quick, there is no justification for doing lesser procedures in the elderly with the excuse of saving anesthesia time. Our tourniquet time has ranged from 37 to 45 minutes in the past 70 cases. This is less time than is required for other approaches in our hands, except for closed pinning without the addition of bone graft, which has been abandoned because it is unreliable in the elderly.8 Our surgical time corresponds with the experience of one surgeon (RSC) and is in sharp contrast to the reported tourniquet times of 105.3 minutes for dorsal plating with Pi plates reported by Grewal and colleagues.9 Their study included six orthopaedic surgeons, and the reported tourniquet times may reflect variables other than simply the dorsal approach and plate design.
None of my patients has suffered from sympathetic dystrophy, even though one has had a presympathetic dystrophy condition that is characterized by an increase in swelling and discoloration of the skin, with a sudden increase in pain and decrease of motion (a “flare reaction”). Our very attentive hand therapist brought this patient to my attention early, and she was treated with an oral steroid dose pack and experienced an excellent response.
Conclusion
1. Ring D, Jupiter JB, Brennwald J, et al. Prospective multicenter trial of a plate for dorsal fixation of distal radius fractures. J Hand Surg [Am]. 1997;22:777-784.
2. Ruch DS, Papadonikolikis A. Volar versus dorsal plating in the management of intra-articular distal radius fractures. J Hand Surg [Am]. 2006;31:9-16.
3. McKay SD, MacDermid JC, Roth JH, et al. Assessment of complications of distal radius fractures and development of a complication checklist. J Hand Surg [Am]. 2001;26:916-922.
4. Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg [Am]. 2002;27:205-215.
5. Musgrave DS, Idler RS. Volar fixation of dorsally displaced distal radius fractures using the 2.4 mm locking compression plates. J Hand Surg [Am]. 2005;30:743-749.
6. Simic PM, Robinson J, Gardner MJ, et al. Treatment of distal radius fractures with a low-profile dorsal plating system: an outcome assessment. J Hand Surg [Am]. 2006;31:382-386.
7. Kamth AF, Zurakowski D, Day CS. Low-profile dorsal plating for dorsally angulated distal radius fractures: an outcome study. J Hand Surg [Am]. 2006;31:1061-1067.
8. Harley BJ, Scherfenberger A, Beaupre LA, et al. Augmented external fixation versus percutaneous pinning and casting for unstable fractures of the distal radius: a prospective randomized trial. J Hand Surg [Am]. 2004;29:815-824.
9. Grewal R, Perey B, Wilmik M, et al. A randomized prospective study on the treatment of intra-articular distal radius fractures: open reduction and internal fixation with dorsal plating versus mini open reduction, percutaneous fixation and external fixation. J Hand Surg [Am]. 2005;30:764-772.
10. Koh S, Andersen CR, Buford WL, et al. Anatomy of the distal brachioradialis and its potential relationship to distal radius fractures. J Hand Surg [Am]. 2006;31:2-8.
11. Jupiter JB, Ring D, Weitzel PP. Surgical treatment of redisplaced fractures of the distal radius in patients older than 60 years. J Hand Surg. [Am]. 2002;27:714-723.