CHAPTER 48 Dorsal Capsulodesis
Rationale and Basic Science Pertinent to the Procedure
Scapholunate dissociation is the most frequently diagnosed pattern of carpal instability.1 If left untreated, it leads to scapholunate advanced collapse and progressive painful arthritis of the wrist.2 Treatment for scapholunate dissociation remains controversial and has varied from limited wrist arthrodeses3–6 to soft tissue procedures, including dorsal capsulodesis7–11 and scapholunate interosseous ligament reconstruction using tendon graft.12–14
Soft tissue reconstructions have several theoretical advantages that make them attractive alternatives to other procedures. In contrast to arthrodeses, soft tissue reconstructions preserve more intercarpal motion, including scaphoid flexion and extension with radial and ulnar wrist deviation. Arthrodeses limit motion. The scaphotrapeziotrapezoid limited arthrodesis results in a loss of 16% to 45% of wrist flexion, 25% of wrist extension, and 45% of radial deviation.3–6 Scaphocapitate arthrodesis, also advocated for scapholunate dissociations, has been shown to produce similar reductions in wrist range of motion and in relative intercarpal motion to scaphotrapeziotrapezoid arthrodesis.15 There has been a renewed interest in tendon reconstructions12,14; however, historically early results, although promising, have not stood the test of time.13
With a dorsal capsulodesis procedure, which is a soft tissue procedure rather than an arthrodesis, greater intercarpal motion is preserved, including scaphoid flexion and extension with radial and ulnar wrist deviation. Blatt7 popularized the capsulodesis using a radius-based flap of wrist capsule inserted into the distal pole of the scaphoid. That procedure has been reported to result in a significant decrease in wrist flexion by some investigators, however, including Blatt, who reported a mean loss of 20 degrees of flexion.7,16 Although it corrects the flexed posture of the scaphoid by crossing the radiocarpal joint and tethering the scaphoid, it nevertheless fails to correct the diastasis between the scaphoid and lunate seen radiographically.
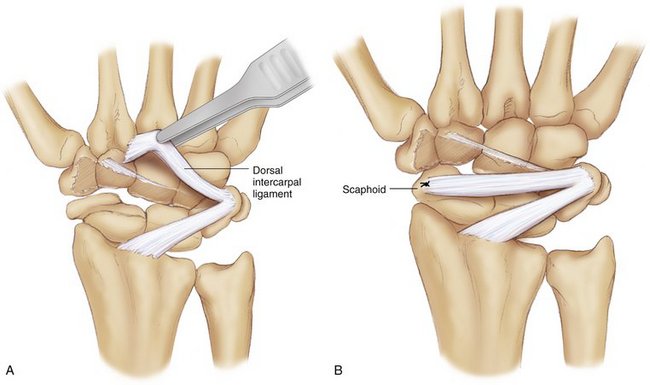
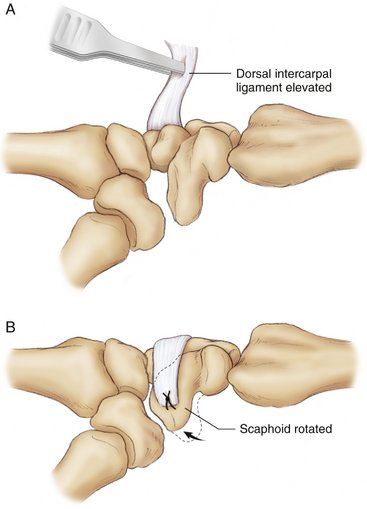
Seeking to address these problems, we developed the dorsal intercarpal ligament capsulodesis (DILC) for the treatment of scapholunate dissociation based on the dorsal intercarpal ligament of the wrist. In a cadaver model, we tested our hypothesis that the DILC can restore the scapholunate relationship with improved wrist range of motion and function.17 In our model, the scapholunate interosseous ligament was sectioned, and the results of the DILC were compared with the results of a Blatt capsulodesis.17 To perform the capsulodesis using the dorsal intercarpal ligament, a 5-mm strip of the portion of the ligament that inserts onto the trapezoid was dissected free. The dorsal intercarpal ligament has some fibers that insert onto the dorsal ridge of the scaphoid, but none that insert onto the distal pole of the scaphoid; the remainder of the ligament inserts onto the trapezoid. The scaphoid and lunate were reduced anatomically. The prepared dorsal intercarpal ligament was rotated proximally on its origin from the triquetrum, stretched as tightly as possible, and held in position with a forceps. The ligament was secured to the distal pole of the scaphoid with a suture anchor (Figs. 48-1 and 48-2).
Contraindications
The procedure may be relatively contraindicated in patients who require high demand of wrist strength as judged by the physician and patient. These patients may be best served by a scaphocapitate or scaphotrapeziotrapezoid arthrodesis, although those procedures also have not provided a predictable solution to this problem.3,4
Surgical Technique
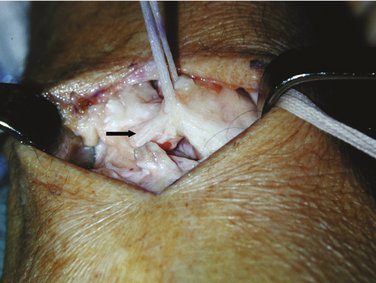
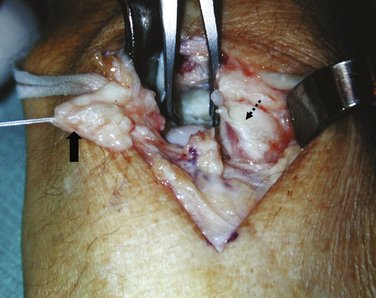
A longitudinal skin incision is made dorsally over the patient’s wrist, centered over Lister’s tubercle. The superficial soft tissues are dissected off the extensor retinaculum, being careful to avoid injuring the cutaneous branches of the ulnar and radial nerves. The extensor pollicis longus is unroofed by incising the retinaculum over the third extensor compartment in a step-cut fashion to facilitate subsequent closure, and the tendon is retracted radially. A surgical sponge is used to wipe the dorsal ligamentous and capsular structures clean so that the interval between the dorsal radiocarpal and the dorsal intercarpal ligament can be identified in line with the long finger. An umbilical tape is passed around the dorsal intercarpal ligament, which is dissected out as it traverses the operative field (Fig. 48-3). It is then divided off its insertion on the trapezoid and trapezium (Fig. 48-4). A 5-mm-wide strip of the ligament is harvested and reflected ulnarly, exposing the scaphocapitate and scaphotrapeziotrapezoid joints (Fig. 48-5).
Appropriate reduction and wire placement are confirmed by direct inspection and intraoperative fluoroscopy. Particular attention is paid to the scapholunate gap on the anteroposterior view, the scapholunate angle on the lateral view, and the alignment of the distal scaphoid and the trapezium on the lateral view (Fig. 48-6). The remnant of the scapholunate interosseous ligament is reattached when possible using 4-0 nonabsorbable sutures via drill holes in a roughened spot in the dorsal proximal pole of the scaphoid, or alternatively via a small suture anchor.
A bony trough is prepared on the dorsal surface of the distal pole of the scaphoid adjacent to the scaphotrapezial joint, well distal to the scaphoid’s axis of rotation. A mini-Statack suture anchor (Zimmer, Inc., Warsaw, IN) attached to a 2-0 braided polyester suture is drilled into place at the base of the trough. One end of the suture anchor is passed through the end of the dorsal intercarpal ligament and then brought back out creating a Krackow stitch,18 which is tied securely to bring the ligament firmly and snugly down into the trough on the scaphoid. Additional 4-0 nonabsorbable sutures are used to secure further the transferred ligament to its new insertion. The capsule is closed over the scapholunate interval, the extensor pollicis longus is replaced in its compartment, and the retinaculum is closed over the extensor tendons. The skin is closed in routine fashion.
Postoperatively, the extremity is immobilized in a bulky thumb spica dressing that extends above the elbow, reinforced with plaster splints. After 8 to 10 days, the sutures are removed, and the dressing is changed to a thumb spica cast extending above the elbow for 3 weeks followed by a below-elbow thumb spica cast for an additional 4 weeks. The K-wires are removed 8 weeks after surgery, at which time gentle range of motion exercises under supervision are begun; a removable protective splint is worn between exercise sessions. Immobilization is discontinued 3 months after surgery. Patients are instructed to avoid forceful axial loading of the wrist, particularly in extension, such as with weightlifting or pushups, for 6 months after surgery.
Controversies
Although we were encouraged from biomechanical studies and early clinical follow-up of the DILC, we noted that many other soft tissue capsulodesis techniques were reportedly successful at 1- or 2-year follow-up. Moran and associates11 reviewed their intermediate-term results (average 54 months) after Blatt or Mayo capsulodesis, and noted that the results of their capsulodesis did not hold up over time. Although dorsal capsulodesis provided pain relief for patients with dynamic and static scapholunate instability, it did not provide maintenance of radiographic carpal alignment in cases of chronic scapholunate dissociation.11 It remains controversial whether soft tissue procedures or limited arthrodesis is better. Zarkadas and colleagues19 performed a study to evaluate the practice pattern of specialized hand surgeons in the management of acute and chronic scapholunate instability. They mailed a survey to the 1628 members of the American and Canadian Societies for Surgery of the Hand and received 468 responses from hand surgeons. The study showed that the management of chronic scapholunate instability varied greatly among the respondents. Favored management of chronic scapholunate dissociation included the Blatt capsulodesis alone, capsulodesis combined with a scapholunate ligament repair, or scaphotrapeziotrapezoid arthrodesis.19 Treatment of chronic scapholunate dissociation remains an unsolved problem.
Results
Previous studies have reported good clinical results using a dorsal capsulodesis to treat static scapholunate instability. Blatt7 reported good results in 12 patients and a mean recovery of 80% of grip strength. Lavernia and colleagues8 reported good results in 17 of 21 patients treated with scapholunate interosseous ligament repair combined with a dorsal capsulodesis procedure. Wintman and coworkers16 showed that dorsal capsulodesis also can be used effectively to treat dynamic scapholunate instability. In a series of 20 procedures in 19 patients, subjective and objective evaluations improved substantially after surgery. After surgery, the symptoms of pain and clunking decreased significantly. Functional status was improved, most strikingly in the tasks of opening jars, sweeping, shoveling, and throwing. The investigators noted a meaningful improvement in wrist stability determined by the scaphoid shift maneuver.
One problem with these previously described procedures is that they limit wrist motion, particularly flexion, because the transferred capsule tethers the distal pole of the scaphoid to the distal radius. In Blatt’s series,7 loss of wrist flexion averaged 20 degrees. In the series reported by Lavernia and coworkers,8 mean loss of flexion was 17 degrees. Wintman and colleagues16 reported a mean loss of 12 degrees of flexion. In addition, none of the described procedures were successful at decreasing the scapholunate gap directly.
DILC conceptually has certain advantages over other soft tissue techniques. Because it links the triquetrum to the distal pole of the scaphoid directly, DILC seems to keep the proximal carpal row linked together to function as a unit. Our cadaver study confirmed that DILC decreased the scapholunate diastasis better than a Blatt capsulodesis, even when maximally loaded in the clenched fist position. We believe that the direction of the soft tissue tether in DILC may partly or entirely account for the observed decreased diastasis. We also believe that with DILC, the reduction of the scapholunate angle is accomplished in part because the transferred dorsal intercarpal ligament rests over the proximal pole of the capitate, which acts as a pulley to support the ligament and prevent the distal pole of the scaphoid from flexing excessively. DILC links the proximal carpal row together to decrease the scapholunate diastasis that develops after scapholunate interosseous ligament disruption. It decreases the diastasis better than a Blatt capsulodesis, and it corrects the scapholunate angle equally well. Neither DILC nor the Blatt capsulodesis restores normal wrist mechanics completely. The finding that DILC was strong enough to restore scapholunate gap and angle to near-normal conditions, even with loads applied across the wrist, was encouraging enough for us to start offering this procedure to patients.
We reported the results of a prospective study of 21 patients (22 wrists), 16 to 62 years old, followed 1 to 4 years.10 For this study, all patients returned to complete a questionnaire and have a physical examination performed by physicians and therapists independent of the treating surgeons, and to obtain standardized radiographs of the wrists. Patient demographics, mechanism of injury, range of motion, and grip strength were recorded. Patients completed the Mayo wrist, Short-Form-12, and Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaires. The scapholunate angle improved significantly (P < .01) from a mean preoperative value of 65 degrees to 54 degrees immediately postoperatively and remained at 50 degrees at final follow-up (P < .01). The scapholunate gap improved significantly from a mean preoperative value of 4.5 mm to 2.6 mm immediately postoperatively and remained at 2.7 mm at final follow-up (P < .01). There was no significant change in grip strength. Wrist flexion decreased by 10% postoperatively compared with a 15% decrease in wrist extension. Radial deviation decreased by 20%, whereas ulnar deviation decreased by 11% postoperatively.
1 Gelberman RH, Cooney WP3rd, Szabo RM. Carpal instability. Instr Course Lect. 2001;50:123-134.
2 Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg [Am]. 1984;9:358-365.
3 Kleinman WB. Long-term study of chronic scapho-lunate instability treated by scapho-trapezio-trapezoid arthrodesis. J Hand Surg [Am]. 1989;14:429-445.
4 Kleinman WB, Carroll CT. Scapho-trapezio-trapezoid arthrodesis for treatment of chronic static and dynamic scapho-lunate instability: a 10-year perspective on pitfalls and complications. J Hand Surg [Am]. 1990;15:408-414.
5 Watson H, Hempton R. Limited wrist arthrodesis, I: the triscaphoid joint. J Hand Surg [Am]. 1980;5:320-327.
6 Watson HK, Belniak R, Garcia-Elias M. Treatment of scapholunate dissociation: preferred treatment—STT fusion vs other methods. Orthopedics. 1991;14:365-368. discussion 368-370
7 Blatt G. Capsulodesis in reconstructive hand surgery: dorsal capsulodesis for the unstable scaphoid and volar capsulodesis following excision of the distal ulna. Hand Clin. 1987;3:81-102.
8 Lavernia CJ, Cohen MS, Taleisnik J. Treatment of scapholunate dissociation by ligamentous repair and capsulodesis. J Hand Surg [Am]. 1992;17:354-359.
9 Wyrick JD, Youse BD, Kiefhaber TR. Scapholunate ligament repair and capsulodesis for the treatment of static scapholunate dissociation. J Hand Surg [Br]. 1998;23:776-780.
10 Szabo RM, Slater RRJr, Palumbo CF, et al. Dorsal intercarpal ligament capsulodesis for chronic, static scapholunate dissociation: clinical results. J Hand Surg [Am]. 2002;27:978-984.
11 Moran SL, Cooney WP, Berger RA, et al. Capsulodesis for the treatment of chronic scapholunate instability. J Hand Surg [Am]. 2005;30:16-23.
12 Garcia-Elias M, Lluch AL, Stanley JK. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg [Am]. 2006;31:125-134.
13 Glickel SZ, Millender LH. Ligamentous reconstruction for chronic intercarpal instability. J Hand Surg [Am]. 1984;9:514-527.
14 Brunelli GA, Brunelli GR. A new technique to correct carpal instability with scaphoid rotary subluxation: a preliminary report. J Hand Surg [Am]. 1995;20:S82-S85.
15 Garcia-Elias M, Cooney WP, An KN, et al. Wrist kinematics after limited intercarpal arthrodesis. J Hand Surg [Am]. 1989;14:791-799.
16 Wintman BI, Gelberman RH, Katz JN. Dynamic scapholunate instability: results of operative treatment with dorsal capsulodesis. J Hand Surg [Am]. 1995;20:971-979.
17 Slater RRJr, Szabo RM, Bay BK, et al. Dorsal intercarpal ligament capsulodesis for scapholunate dissociation: biomechanical analysis in a cadaver model. J Hand Surg [Am]. 1999;24:232-239.
18 Krackow KA, Thomas SC, Jones LC. A new stitch for ligament-tendon fixation: brief note. J Bone Joint Surg [Am]. 1986;68:764-766.
19 Zarkadas PC, Gropper PT, White NJ, et al. A survey of the surgical management of acute and chronic scapholunate instability. J Hand Surg [Am]. 2004;29:848-857.