8 Distal Upper Extremity Block
Ulnar, Median, and Radial Block at the Elbow
Placement
At the Elbow
Anatomy
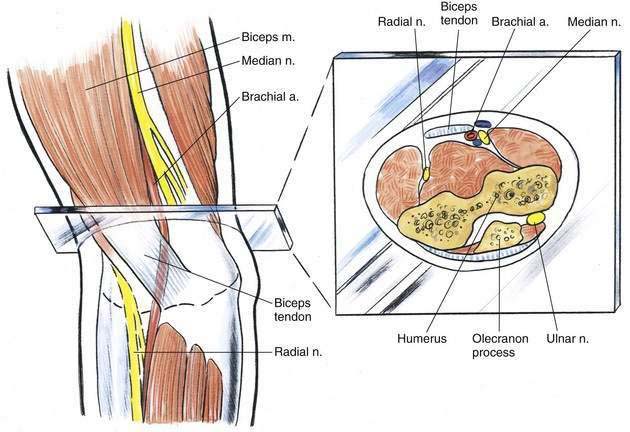
Of the three major nerves at the elbow—radial, median, and ulnar—the ulnar is most predictable in location. As illustrated in Figure 8-1, the ulnar nerve is located in the ulnar groove, which is a bony fascial canal between the medial epicondyle of the humerus and the olecranon process. This area is extremely well protected by fibrous tissue and, although it may seem at first like an easy site to carry out block, the nerve is well protected (and potentially vulnerable) in the ulnar groove. The median nerve at the elbow lies medial to the brachial artery, which lies just medial to the biceps muscle. Conversely, the radial nerve has a somewhat variable course; it pierces the lateral intramuscular septum on its way to the forearm, and lies between the brachialis muscle and the brachioradialis muscle in the distal aspect of the upper arm. It is more effectively blocked in the axilla than at the elbow.
Position
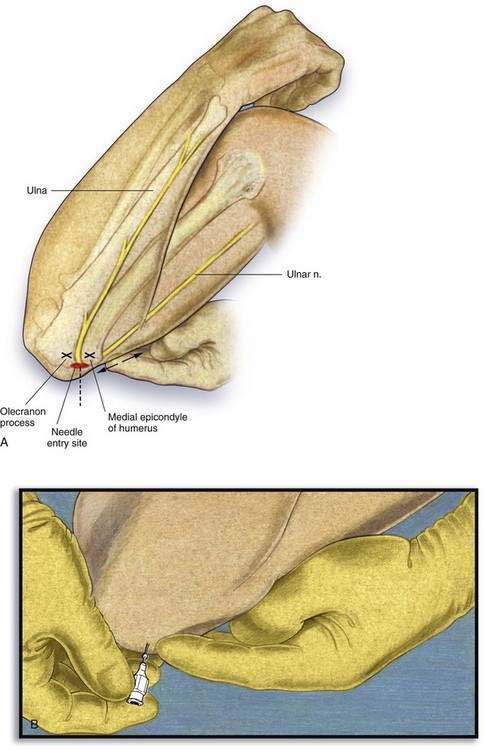
All three of these nerves are blocked with the patient in the supine position and the arm supinated and abducted at the shoulder at a 90-degree angle. In addition, when the ulnar nerve block is performed, the forearm is flexed on the upper arm to more easily identify the ulnar groove (as illustrated in Fig. 8-3).
Needle Puncture: Median Nerve Block
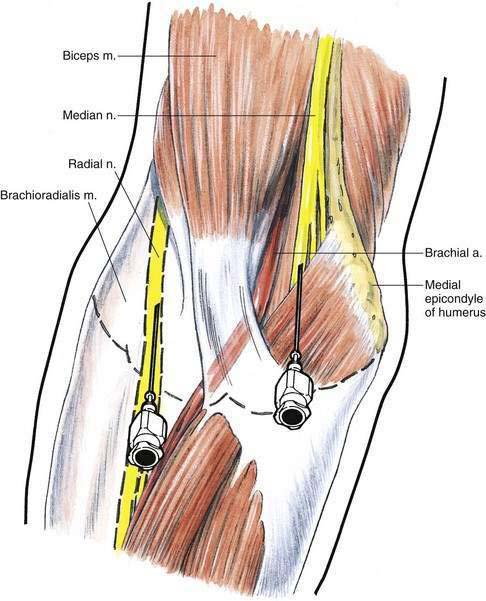
A line should be drawn between the medial and lateral epicondyles of the humerus (at the level of the “pane of glass” shown in Fig. 8-1). Immediately medial to the brachial artery, the needle is inserted in the plane of the pane of glass, and a paresthesia is sought or a nerve stimulator or ultrasonographic guidance is used to direct the needle (Fig. 8-2). After the needle is positioned, 3 to 5 mL of solution is injected medial to the brachial artery.
Needle Puncture: Radial Nerve Block
The radial nerve is likewise blocked at the level of the pane of glass in Figure 8-1. The biceps tendon at that level should be identified, and then a mark is made 1 to 2 cm lateral to the tendon. Again, a small-gauge, 3-cm needle is inserted through the mark in the plane of the pane of glass, and a paresthesia is sought or a nerve stimulator or ultrasonographic guidance is used to direct the needle, and 3 to 5 mL of solution is injected at that site (see Fig. 8-2).
Needle Puncture: Ulnar Nerve Block
As illustrated in Figure 8-3, the forearm is flexed on the upper arm and the ulnar groove is palpated. At a point approximately 1 cm proximal to a line drawn between the olecranon process and the medial epicondyle, a small-gauge, 2-cm needle is inserted. A paresthesia should be easily obtainable, and once it is, the needle is withdrawn 1 mm, and 3 to 5 mL of local anesthetic is injected through the needle. A larger volume of solution should not be injected directly into the ulnar groove because high pressure in this tightly contained fascial space may increase the risk of nerve injury.
At the Wrist
Anatomy
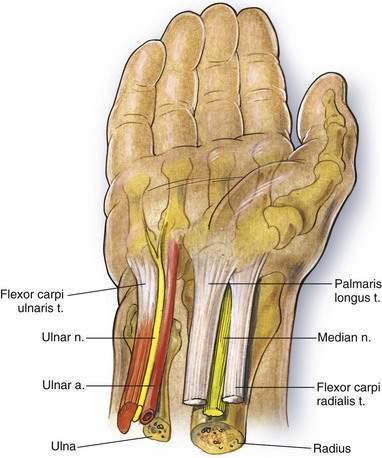
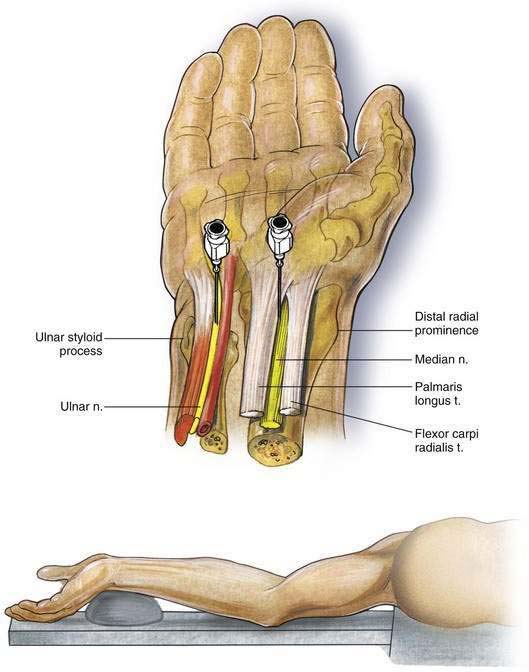
The ulnar nerve lies immediately lateral to the tendon of the flexor carpi ulnaris muscle and immediately medial to the ulnar artery (Fig. 8-4). The median nerve lies between the tendon of the palmaris longus muscle and the tendon of the flexor carpi radialis muscle. That places the median nerve in the long axis of the radius. The radial nerve at the wrist has already divided into a number of its peripheral branches, and effective radial block requires a field block along the radial aspect of the wrist.
Position
For a peripheral block at the wrist, the patient rests supine while the arm is extended at the shoulder and supported on an arm board (Fig. 8-5). The wrist is flexed over a small support, and the most effective position for the anesthesiologist is to stand in the long axis of the arm board. Thus, while performing the block, the anesthesiologist may observe the patient’s face.