Disorders of the wrist
Disorders of the inert structures
Limited range: capsular pattern
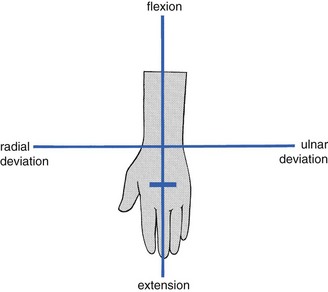
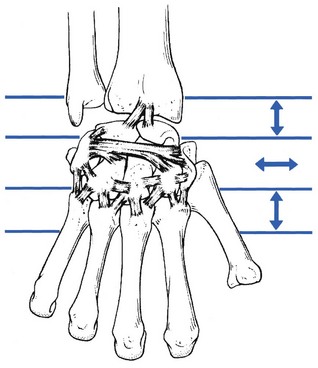
The capsular pattern is an equal degree of limitation of flexion and extension (Fig. 23.1). In advanced arthritis, fixation of the wrist in the neutral position takes place.
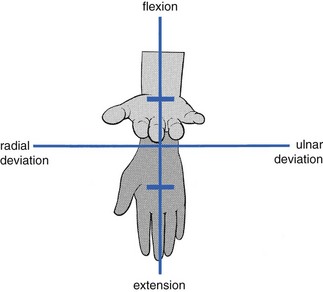
Fig 23.1 The capsular pattern at the wrist.
Traumatic arthritis
The discovery of a capsular pattern following a trauma should always induce further examination. Uncomplicated traumatic arthritis is rare and the finding of a post-traumatic capsular pattern is highly suggestive of a fracture. The radiographic picture is unreliable because it may take up to several weeks for radiological evidence of a fracture to be conclusive.1 This delay may be responsible for serious complications because failure to diagnose and immobilize carpal fractures often leads to non-union and avascular necrosis.2,3 However, the clinical picture is so evident that the diagnosis should not be missed: any case of traumatic arthritis of the wrist lasting for longer than 2 days should be considered as a fracture.
History and examination
Inspection shows swelling of the wrist. On examination, a capsular pattern is found: passive flexion and extension are very painful and limited. The end-feel is that of a vibrant twang caused by a protective muscle spasm. Passive deviation of the wrist towards the painful side also increases the pain – a compression phenomenon that provides further evidence of a bony lesion. Careful palpation of the bones reveals localized tenderness. Most often the scaphoid bone is involved.4 In this case, tenderness will be elicited in the anatomical snuffbox.5 This is often described as a classic sign of scaphoid fracture and has a reported sensitivity of 90% but a low specificity of 40%.6 The scaphoid compression test also has a high sensitivity but a better specificity for scaphoid fractures. This test is performed by grasping the thumb and applying an axially directed compressive force along the line of the thumb metacarpal; wrist pain indicates a positive result.7
The scaphoid bone spans the joint between the proximal and distal rows of carpal bones and is most vulnerable: scaphoid fracture comprises between 51 and 78% of all carpal fractures.8–11 Young males and persons between 10 and 19 years of age are at highest risk for scaphoid fracture.12–14
Scaphoid fractures occur most easily during loading of a hyperextended wrist, possibly in combination with ulnar deviation. This movement tightens the palmar ligaments (the radiocapitate and radioscaphoid ligaments), so stabilizing the scaphoid against the radius. As the proximal pole is strongly stabilized, further loading and extension of the wrist causes bending forces on the distal pole, which may result in fracture.15,16
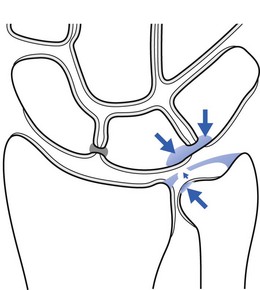
Fractures may occur at any level in the scaphoid but the more proximal the fracture, the greater the chance of avascular necrosis of the proximal fragment.17,18 The main reason for this is the special nature of the scaphoid’s blood supply.19 The blood supply to the scaphoid can be divided into extraosseous and intraosseous sources. The extraosseous blood supply is primarily derived from a branch of the radial artery, the artery to the distal ridge of the scaphoid.20 The branches of this vessel enter the scaphoid through a foramen at the dorsal ridge at the level of the wrist (Fig. 23.2). These vessels then run proximally and palmarly within the medullary chamber, forming the intraosseous supply to the proximal pole.21 Since vascularity of the proximal pole is limited and dependent on intraosseous flow, acute proximal pole fractures have a potentially prolonged healing period, averaging 3–6 months, and there is higher incidence of non-union.
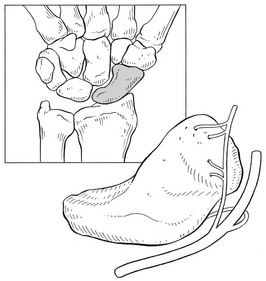
Fig 23.2 Vascular supply to the scaphoid.
Because of the danger of avascular necrosis developing, it is important to recognize a scaphoid fracture as quickly as possible. Acute scaphoid fractures are often missed on initial plain radiographs. Therefore an initial negative radiograph does not alter the clinical diagnosis. When clinical suspicion of a scaphoid fracture is high and plain films are negative, the traditional recommendation is for these patients to be immobilized in a thumb spica splint or cast, with repeat radiographs after about 2 weeks.22
Alternative imaging modalities for diagnosis include bone scans and magnetic resonance imaging (MRI). A bone scan reportedly shows focally increased uptake within 72 hours and is very sensitive for detecting a fracture, but may not be extremely specific.23–25 MRI has been reported to have 95–100% sensitivity and almost 100% specificity for scaphoid fractures.26–28 Additional advantages of MRI include its potential to assess vascularity of the proximal scaphoid pole when a fracture is present.29
Treatment
Treatment consists of immediate immobilization of the wrist, which is protective and can decrease the incidence of non-union and avascular necrosis.30 The best position remains unclear. Several dissection studies have come to different conclusions.31–34 Immobilization seems to be best performed with a thumb–spica cast, holding the thumb in the palmar abducted position and the wrist in the mid-position but with an element of deviation towards the site of the fracture, which, for the scaphoid, would be radial deviation. This helps to press the fractured surfaces together and stimulates the healing process.15 The time needed for a scaphoid fracture to heal is variable, from a minimum of 6 weeks to as long as 9 months,35 but 90% of fresh fractures heal with adequate treatment.30
Fractures of the other carpal bones can occur. Frequently, multiple radiographic views and/or follow-up studies with tomograms or bone scans may be necessary for a definitive diagnosis.36 Displaced fractures may require open reduction and internal fixation.37,38
Rheumatoid arthritis
The wrist can become affected by any type of rheumatic disorder, such as systemic lupus erythematosus, progressive systemic sclerosis, psoriatic arthritis, gout and pseudogout, ankylosing spondylitis and sarcoidosis, but rheumatoid arthritis is one of the commonest, frequently affecting both wrists39 and often following involvement of the fingers. In the acute stage a capsular pattern is found on examination, together with swelling, warmth and synovial thickening. At this stage MRI can be a useful technique for reaching a diagnosis.40 Recently joint ultrasound has also proved to be an important tool to evaluate synovitis of the wrist.41 In addition to pain, the more chronic cases present with gross limitation of movement. At this stage, there is no longer any warmth and even the swelling has diminished; diagnosis is easily made on conventional radiographs.
Limited range: non-capsular pattern
Carpal subluxation
History and examination
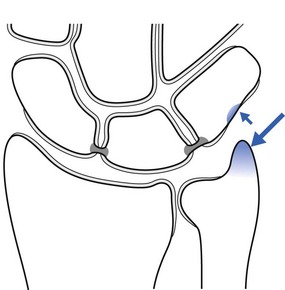
On examination, signs of internal derangement are found (Fig. 23.3): one movement, most often extension, is limited with – certainly in acute cases – an end-feel of muscle spasm. Other movements are full-range, although often painful – the result of overstretching the irritated ligaments (see p. 34). The bony subluxation may be visible and palpable if the wrist is held in flexion. There is local tenderness in the ligaments.
The radiograph is negative: the edge of the subluxated bone appears merged with the others and cannot be visualized separately on the radiograph, nor can its position be measured against the superimposed margins of the other bones (Cyriax:43 p. 184).
Palmar subluxation, mostly of the lunate bone, is very exceptional. It gives rise to (slight) limitation of flexion and may compress a palmar branch of the median nerve, causing paraesthesia in the corresponding territory (see online chapter Nerve lesions and entrapment neuropathies of the upper limb).
Differential diagnosis
• A ganglion at the dorsum of the wrist usually feels softer on palpation. It does not respond to manipulative treatment but can be diagnosed and treated by puncture.
• Kienböck’s disease, un-united fracture and isolated arthrosis have a different history and can easily be detected on radiography (see p. 337).
Treatment
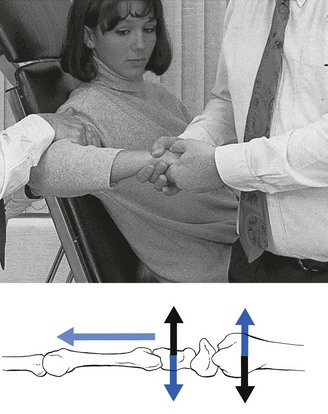
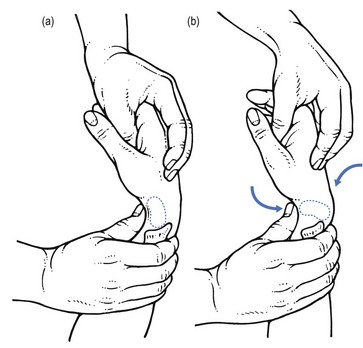
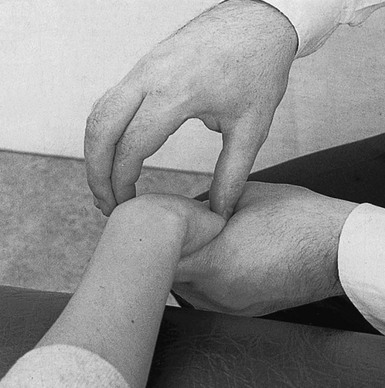
Basic technique: manipulation for carpal subluxation
The aim of the manipulation is to perform a gliding movement between the rows of carpal bones during traction. The technique is executed as follows. The manipulator leans sideways but makes sure that the pull is only carried out with the distal hand, so as to obtain traction on the wrist. After the slack has been taken up, both hands are moved vertically up and down in opposite directions (Fig. 23.4). The little finger of the contralateral hand is kept in the palm of the patient’s hand to control movement; the manœuvre should result in a pure gliding movement and flexion–extension should be avoided.
When this technique does not lead to full recovery, the next manœuvre is tried.
Second technique: manipulation for carpal subluxation
The patient, assistant and manipulator maintain the same positions as in the previous technique. The manipulator’s distal hand is now moved slightly downwards, so that it grasps the patient’s hand at the level of the bases of the metacarpal bones. Using the other hand, the patient’s wrist is approached from above and encircled with thumb and index finger. The metacarpophalangeal joint of the index finger is placed on the subluxated bone. The manipulator’s forearm is held vertically (Fig. 23.5). The manipulator leans sideways, applying traction with the distal hand and, having taken up the slack, executes a short, sharp squeezing manœuvre.
Alternative technique: manipulation for carpal subluxation
The patient stands next to the couch, with the forearm, stabilized by the other hand, placed on the couch, the distal part level with the edge. The manipulator stands in front of the patient and grasps the hand in such a way that one thumb, reinforced with the other, is placed dorsally on the subluxated bone, while one index finger, reinforced by the other, is placed on the palmar aspect of it. The little fingers are placed in the palm of the patient’s hand, in order to prevent flexion–extension movements during the manipulation (Fig. 23.6).
Other joint problems
The four following disorders, all visible on radiograph, give rise to limited extension only.
Aseptic necrosis of the lunate bone (Kienböck’s disease)
Avascular necrosis of the lunate was first described by Peste in 1843.44 The condition was then forgotten until 1910, when Kienböck recorded lunatomalacia, which he assumed had a vascular traumatic aetiology.45 Despite recognition of this disease entity for the past 100 years, its cause is still debated. Some investigators relate it to a stress fracture that leads to devascularization of the major segment of the lunate. Other authors consider the avascular necrosis to be the result of interruption of the vascularization of the lunate bone following excessive shear forces caused by acute trauma or repeated microtrauma.46 This would happen more easily in those lunate bones that are supplied by a single volar or dorsal blood vessel.47 Others suggest that a vascular non-traumatic process, with a minor infarction pattern in the proximal subchondral area, may be nearer to the truth.48
Avascular necrosis usually affects the dominant hands of males between 20 and 40 years of age.49,50 The symptoms come on spontaneously or as the result of minor injury, and usually interfere very significantly with work-related activities. The initial symptoms are pain and stiffness, which may vary from moderate to severe and incapacitating. The patient may also mention reduced strength in the hand.51
The classification of Kienböck’s disease is based on its roentgenological appearance.52,49,53:
• Stage 1 consists of small fracture lines – bone scintigraphy54 or MRI55 will be required for diagnosis.
• Stage 2 is rarification along the fracture line, usually on the volar pole.
• Stage 3 shows sclerosis of the bone dorsal to the fracture site.
• Stage 4 shows sclerosis of the bone dorsal to the fracture site, and collapse and secondary fracture with loss of architectural integrity of the lunate.
Treatment methods extend from immobilization to revascularization surgery on the affected bone. However, there is still no gold standard for the treatment of Kienböck’s disease.56 A recent systematic review showed that, to date, there are insufficient data to determine whether the outcomes of any intervention are superior to placebo or the natural history of the disease.57
Avascular necrosis in other carpal bones has been described but is rare.58,59
Carpal boss
This bony prominence at the base of the second and third metacarpals adjacent to the capitate and trapezoid bones may represent degenerative osteophyte formation and/or the presence of an os styloideum, an accessory ossification centre that occurs during embryonic development. The symptoms of a carpal boss may result from an overlying ganglion or bursitis, an exterior tendon slipping over this bony prominence, or from osteoarthritic changes at this site. Diagnosis is by X-ray.60
Full range
Ligamentous lesions
Ligamentous injuries range from minor sprains with no instability (which are discussed here) to complete rupture with gross instability (see p. 341).61
Sprain of the ulnar collateral ligament
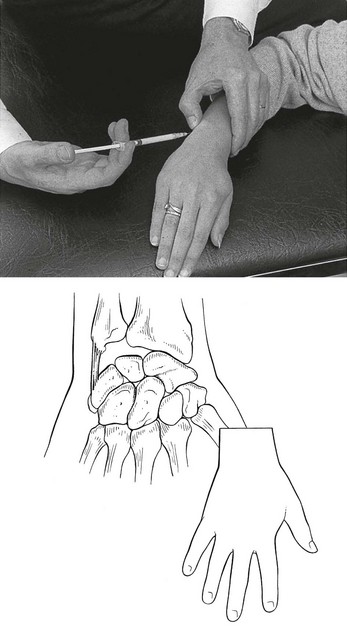
Technique: infiltration
A 1 mL syringe, filled with 10 mg of triamcinolone acetonide, and a 2 cm needle are used. The patient’s arm rests in pronation on the couch. The hand is brought into slight radial deviation. The tender spot is identified, and the infiltration given with bony contact and ligamentous resistance (Fig. 23.7).
Sprain of the radial collateral ligament
This rare disorder results in pain felt at the radial aspect of the wrist during passive ulnar deviation. A more common cause of these symptoms is a tendinous lesion in the extensor pollicis brevis and abductor pollicis longus tendons (see p. 354). Differential diagnosis is easy because, in tendinitis, resisted movements are also positive.
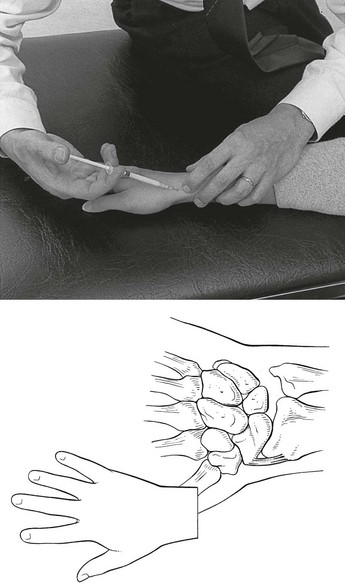
Technique: infiltration
The patient sits with the forearm in the neutral position and the hand on the couch. The wrist is brought into slight ulnar deviation. The tender spot is palpated and 10 mg of triamcinolone acetonide is infiltrated using a 2 cm needle (Fig. 23.8). During infiltration, ligamentous resistance and bony contact should be felt. Care must be taken to avoid puncture of the radial artery.
Sprain of the dorsal ligaments
Technique: deep transverse friction
The patient sits with the hand over the edge of the couch. The therapist sits facing the patient’s wrist, which is flexed with one hand within the limits of pain. Friction is imparted with the other hand. The direction depends on the course of the ligamentous fibres: the radiocarpal and carpometacarpal ligaments are aligned in the same longitudinal axis as the forearm, while the intercarpal ligaments have a more or less transverse direction (Fig. 23.9). For a radiocarpal or carpometacarpal ligament, the direction of the friction is transverse on the ulnar–radial axis. Friction is given with either the index finger, reinforced with the middle finger (Fig. 23.10), or with the thumb. As the lesion is very localized, the therapist must make sure that the finger remains deep between the extensor tendons and does not pass over them.

Fig 23.10 Friction to the dorsal carpal ligaments.
An intercarpal ligament is given friction with the thumb and in a proximo–distal direction (see Fig. 23.9).
Wrist impaction syndromes
Ulnar impaction syndrome
Ulnar impaction syndrome, also known as ulnar abutment or ulnocarpal loading, is a degenerative condition characterized by ulnar wrist pain related to excessive load bearing across the ulnar aspect of the wrist. Chronic impaction between the ulnar head and ulnar carpus results in periostitis and degeneration of the lunate bone, triquetral bone and distal ulnar head, and degenerative tears of the triangular fibrocartilage complex (Fig. 23.11).62
Radiographic changes include subchondral sclerosis and cystic changes in the ulnar head, ulnar aspect of the proximal lunate bone, and proximal radial aspect of the triquetral bone. MRI is helpful in detecting occult disease in the early stage.63
Treatment will depend on the severity of the lesions. Periostitis responds well to local infiltration with 10 mg of triamcinolone acetonide, provided that further irritation is avoided. This can be done by avoiding the extremes of wrist movement in the loaded position or by the application of a splint or a cast. In more advanced cases or in lesions of the triangular fibrocartilage complex, arthroscopy and surgery will be needed.64,65
Ulnar styloid impaction syndrome
This ulnar-sided wrist pain is caused by impaction between an excessively long ulnar styloid process and the triquetral bone.66 The ulnar styloid process is a continuation of the prominent subcutaneous ridge of the shaft of the ulna, which projects distally towards the triquetral bone for a variable distance (2–6 mm).67 A single or repetitive impaction between the tip of the ulnar styloid process and the triquetral bone results in contusion, which leads to periostitis of the opposing surfaces. If a single-event trauma is forceful enough, fracture of the dorsal triquetral bone may occur.68
The diagnosis of this condition is made on the basis of pinching pain during ulnar deviation and radiographic evidence of an excessively long ulnar styloid process. MRI may show chondromalacia of the ulnar styloid process and proximal triquetral bone (Fig. 23.12).69
Radial impaction syndrome
Pain at the dorsal aspect of the wrist may occur as the result of repetitive extension movements during weight bearing, as frequently happens in gymnastics or other high-energy sports; this may lead to periostitis at the distal epiphysis of the radius or the proximal carpal bones,70,71 described as ‘wrist impingement’ syndrome72 or ‘stress reaction’.73 The pain is elicited each time the patient puts weight on an extended wrist.
Periostitis responds well to local infiltration with 10 mg of triamcinolone acetonide, provided that further irritation is avoided. This can be done by avoiding the extremes of wrist movement in the loaded position or by the application of a splint or a cast, if necessary. Surgery can be performed in recurrent cases or to avoid long-term complications.74
Repetitive compressive loading may result in stress fractures of the distal part of the radius, the scaphoid and the capitate bones. Scintigraphy and MRI are diagnostic and immobilization in a cast is therapeutic.75,76
Ganglion
A ganglion is a fluid-filled cavity that originates from the joint capsule or tendon sheath. It is very common at the wrist. It occurs dorsally, most often over the scapholunate joint, as well as at the palmar aspect, usually at the trapezioscaphoid joint.77 Its aetiology has been debated for many years and various hypotheses have been presented: retention cyst, herniation of tendon or capsular synovia, bursal transformation, neoplasia, or mucinous degeneration of fibrous tissue, the last of these being the most widely accepted theory.78
The main complaint is the presence of a swelling that was not there before. It may sometimes be painful either at rest or during movement. The size may vary and so does its consistency: it can be either very soft or quite hard, giving the impression of a bony structure. When the ganglion grows, the neighbouring tissues may become compressed and there may be pressure on nervous tissue as well (see online chapter Nerve lesions and entrapment neuropathies of the upper limb).
Many techniques have been used to treat this condition, varying from crushing the ganglion (e.g. pressure with the thumbs or a firm slap with a book) to aspiration and infiltration with a steroid or sclerosant solution. These measures usually lead to temporary cure but recurrences are frequent because the cause has not been treated. More consistent results are obtained by surgical removal, although the risks associated with surgery may be more undesirable than the minor symptoms associated with the presence of a ganglion.79
Excessive range
Ligamentous instability
According to Ekenstam, instability of the wrist is ‘a condition of altered joint kinematics in which one or several carpal bones are permitted abnormal patterns of motion as a result of bony abnormalities, ligamentous lesions or joint laxity’.80
Carpal instability remains a very controversial topic. Since 1943, when Gilford et al81 first mentioned instability of the wrist, many authors have worked on the subject. They have developed several hypotheses and proposed different methods of classification. This variability indicates the difficulty in reaching a consensus on such a vague topic as ‘instability’ in the complex area that is the wrist. There is still a lack of standardization in evaluation methods and in the findings and radiographic criteria. Arthroscopy, however, has helped to provide a clearer picture of the possible underlying mechanisms.82
Aetiology
Wrist instability is generally believed to be caused by post-traumatic stretching or rupture of one or several radiocarpal or intercarpal ligaments. The injury is usually hyperextension combined with radial or ulnar deviation and/or pronation or supination.83According to some authors, however, it can also be the result of anatomical changes and malalignment subsequent to radial or carpal fracture. Other possible causes of ligamentous laxity are degenerative and inflammatory conditions (i.e. crystal synovitis, rheumatoid arthritis), as well as iatrogenic causes.84
Epidemiology and classification
Epidemiological data on carpal instability are still not available, although wrist injuries occur in 28.6% of all accidents.85 Several methods of classification have been described.86
Taleisnik87,88 has proposed a theory based on the columnar concept of Navarro.89 This concept recognizes three vertical columns in the wrist: (a) the central (flexion/extension) column contains two blocks – one on the lunate bone and one on the trapezium, trapezoid, capitate and hamate bones; (b) the radial column comprising the mobile scaphoid bone; and (c) the ulnar (rotating) column,which includes the triquetral bone and the pisiform. Taleisnik therefore classifies wrist instability as being radial, ulnar or proximal.90
This concept does not mention the transverse or perilunar patterns (stages I–IV), which were later described by Mayfield et al,91 or the more recently discussed mid-carpal instability, proximal row instability and miscellaneous instability.
The Mayo Clinic proposes a classification, based on the work of Amadio, Cooney, Dobyns and Linscheid.92–96
The Lichtman classification97 deviates from the columnar wrist concept and the consequent longitudinal classification system. It is based on the ‘carpal ring concept’ – the distal and proximal rows are joined by two links: on the radial side the mobile scaphotrapezial joint and on the ulnar side the rotatory triquetrohamate joint. This concept includes the perilunate and mid-carpal instabilities.
Other classification systems – for example, the Barton classification – have also been proposed.
We consider Saffar’s classification86 to be a clinical and useful approach.
1. Static or dynamic instabilities
Dynamic instability only shows when, during movement of the wrist or under specific loading, symptoms can be elicited. Static instability is fixed, cannot be corrected by the patient and shows an abnormal position of the bone.
Proximal row instability is the most frequent type of instability:
(a) Scapholunate: there is a malalignment between the scaphoid and the lunate. This condition may lead to arthrotic changes.
(b) Triquetrolunate is the result of a complete or partial rupture of the triquetrolunate ligament.
(a) Ligament attenuation or tear after light trauma in hyperlax persons: this results in a malalignment between the proximal and middle row of carpal bones.
(b) Ligament tear after rotational injury: there is a rupture or elongation of the ligaments that stabilize the mid-carpal joint.
Proximal instability (radiocarpal) with the two Taleisnik stages:
Clinical diagnosis
The patient has a history of past trauma with or without fracture or of past inflammatory disease. There is wrist pain mostly during or after activity, which may be accompanied by a feeling of weakness or of snapping during movement. Information about the type of injury should be obtained but the patient often does not recall such features.98 The localization of the pain is also very informative and points towards specific possibilities. The passive movements are full or even excessive in range and, although they are performed very gently, they may cause pain at the end of the movement.
Provocative tests can be performed:99
1. For scapholunate instability
• The scaphoid bell sign: the examiner grasps the patient’s scaphoid bone between thumb and index finger and controls its movement while the patient is actively moving from radial to ulnar deviation. The movement of the scaphoid should be smooth. If this is not the case, the test is considered positive.
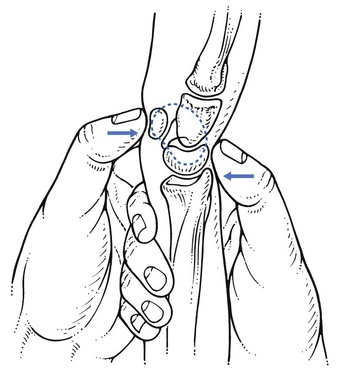
• Watson’s test:100,101 the examiner puts the patient’s hand in ulnar deviation. With the other hand the scaphoid bone is grasped between thumb (on the tubercle) and index finger. The hand is then brought into radial deviation and resists flexion movement of the scaphoid by the thumb. In instability this results in the proximal pole shifting backwards, which can be felt at the dorsal aspect (Fig. 23.13).
• Lane’s test (the scaphoid shift test):102 the examiner assesses the anteroposterior gliding of the scaphoid.
2. For triquetrolunate instability
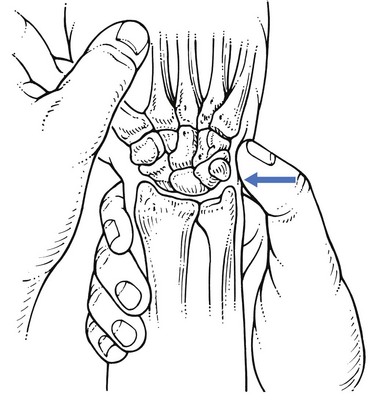
• Kleinman’s shear test:103 the examiner grasps the patient’s distal forearm and puts the fingers on the most distal and dorsal aspect of the ulna. The thumb is placed on the pisiform bone. The ulna is so stabilized and a posterior pressure exerted on the pisiform. Pain may be produced (Fig. 23.14).
• Linscheid’s test:104 the examiner grasps the patient’s distal forearm and puts the finger on the most distal and radial aspect of the radius. The thumb is placed at the ulnar aspect on the triquetral bone (Fig. 23.15). The radius is stabilized and pressure exerted laterally on the triquetrum. Pain may be produced.
• Mid-carpal shift test:105 the examiner exerts axial compression on the wrist via the hand and asks the patient to move the wrist actively. A painful click may be produced. The click will not be present when pressure is brought to bear on the pisiform or during active contraction of the hypothenar muscles.
• Apprehension test:106 when the capitate bone is glided in a posterior direction, pain and/or apprehension are produced.
• Metacarpal gliding:107 the wrist is placed in ulnar deviation and the metacarpals glided in a palmar direction. Pain may be elicited.
4. For radiocarpal instability
• Medial radiocarpal drawer test:108 pressure is exerted on the posterior aspect of the triquetral bone and counterpressure is on the radius. The test is positive when painful.
Disorders of the contractile structures
Resisted extension
Pain
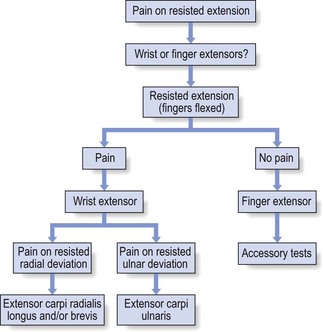
Differentiation between wrist and finger extensors can be made by testing extension first with the fingers relaxed and then actively flexed, which inhibits the action of the finger extensors. When an extensor of the wrist is at fault, it is possible to differentiate between the radial extensors and the ulnar extensor by testing resisted radial and ulnar deviation (Fig. 23.16).
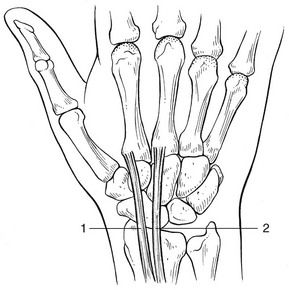
Extensor carpi radialis longus and/or brevis
A lesion of the extensor carpi radialis longus and/or brevis (Fig. 23.17) is usually the result of overuse.109,110 The patient complains of local pain during activity.
Technique: deep transverse friction
The patient sits with the arm resting on the couch, the hand lying over its edge. The therapist sits lateral to the patient’s hand. To stretch the tendon, the patient’s wrist is flexed but this should not provoke pain. The index finger of the other hand, reinforced with the middle finger, is placed on the tender spot. Counterpressure is applied with the thumb at the ulnar aspect of the wrist (Fig. 23.18). The friction starts at the radial side of the tendon and, when the finger has passed over the tendon, the movement restarts. This results in a to-and-fro movement, the active phase being the movement towards the therapist.
Technique: infiltration
This treatment is only applied to insertion tendinitis on the base of the second and/or third metacarpal bones. Ten milligrams of triamcinolone acetonide are infiltrated at the tender area, using a 2 cm needle. The infiltration is given when tendinous resistance is felt and the needle is in contact with the bone. If the palpating finger is kept on the tender spot during the whole procedure (Fig. 23.19), the exact location of the infiltration can be confirmed.
Extensor carpi ulnaris
The tendon is the second most common site of tendinitis in the upper limb.111,112 A tendinitis of the extensor carpi ulnaris (Fig. 23.20) usually develops after a strain or overuse. A tenosynovitis is a rheumatoid manifestation.

Fig 23.20 The extensor carpi ulnaris.
‘The arrangement of the fibrous septa about the ECU [extensor carpi ulnaris] creates an angular approach of the tendon to its insertion in the position of full supination. This angle results in an ulnar translocation stress on the tendon sheath during ECU contraction, particularly with the forearm in supination and the wrist ulnarly deviated.’113
Post-traumatic rupture of the subsheath or of the extensor retinaculum may result in recurrent subluxation of the tendon. The patient feels a sudden snap on certain movements – for example, active supination with the wrist slightly flexed.114 During the clinical examination, an attempt can be made to reproduce the instability using isometric stress in supination. Treatment is surgical reconstruction.115
Technique: deep transverse friction
The patient’s pronated arm rests on the couch. The therapist, sitting at the medial aspect of the patient’s arm, stretches the tendon by bringing the patient’s hand into radial deviation. Depending on the extent of the tenderness, friction is applied with the fingertips of one, two or three fingers, or the index finger is reinforced by the middle finger (Fig. 23.21). Counterpressure is applied to the radial and distal aspect of the forearm. The finger is placed at the palmar aspect of the tendon and then moved upwards over the tendon. Repetition of this movement results in up-and-down friction.

Fig 23.21 Friction to the extensor carpi ulnaris.
Technique: infiltration at the tenoperiosteal junction
The patient’s forearm rests on the couch in the same position as for friction. Ten milligrams of triamcinolone acetonide are infiltrated with a 2 cm needle at the insertion of tendon at the fifth metacarpal bone, while one finger of the other hand ensures that the agent is placed at the correct spot (Fig. 23.22).
The extensor carpi ulnaris and its related structures
This structure is closely connected to the distal radioulnar joint (DRUJ) and to the triangular fibrocartilage complex (TFCC). The distinct subsheath blends proximally with the capsule of the DRUJ and distally with the TFCC, and explains the phenomenon of ‘transmitted stress’ which is particularly present at this level. Resisted extension and ulnar deviation of the wrist may be positive in lesions of the inert structures (DRUJ and TFCC). The reverse also holds: passive supination may hurt in a lesion of the extensor carpi ulnaris (see p. 345). The phenomenon can be reduced to a minimum by making sure that all examination tests are performed in a starting position which is technically correct (see Ch. 20).
Extensor indicis proprius
Lesions of the extensor indicis proprius are rare and result from overuse.
Weakness
Bilateral weakness
If examination shows that only wrist extension is weak, lead poisoning is a possibility. Involvement of motor function in the peripheral nervous system is one of the main features, in addition to those arising from haematopoietic, central nervous, gastrointestinal and renal involvement.116
Unilateral weakness
• C6 root palsy: in a C6 root palsy, flexion of the elbow is weak as well.
• C7 root palsy: weakness of extension of the wrist is exceptional in C7 root palsy but extension of the elbow and flexion of the wrist are normally found to be weak.
• C8 root palsy: this is suspected when the extensor carpi ulnaris and flexor carpi ulnaris are weak. Consequently, the hand deviates radially when resisted extension of the wrist is tested. Extension and adduction of the thumb are also weak.
• Radial palsy: pressure on the radial nerve in the arm gives rise to radial palsy. The causes may be pressure from a crutch in the axilla, the edge of a chair or, in acute circumstances, fracture of the humerus at mid-shaft (see online chapter Nerve lesions and entrapment neuropathies of the upper limb).
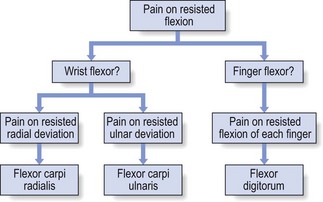
Resisted flexion
Pain
The first question that arises is: is there a lesion of either the flexors of the wrist or the flexors of the fingers, and, if a wrist flexor is at fault, is it the radial or the ulnar tendon? Radial and ulnar deviation, tested against resistance, as well as resisted flexion of each finger in turn, should define the affected structure (Fig. 23.23).
Flexor carpi radialis
Lesions of the flexor carpi radialis (Fig. 23.24) are not very common117 but typically occur in women (75% of cases)118 and are the outcome of overuse, either recreational or occupational. Pain is felt at the palmar aspect of the wrist during movements such as grasping and lifting with the fingers outstretched.
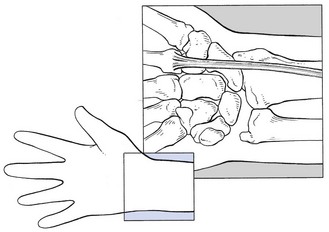
Fig 23.24 The flexor carpi radialis.
On examination, resisted flexion and resisted radial deviation of the wrist are painful. Tenderness can be palpated either over the whole distal extent of the tendon or at the insertion of the tendon at the base of the second metacarpal bone.119
Technique: deep transverse friction
The patient sits with the supinated arm lying on the couch and the hand over its edge. The therapist faces the patient and extends the patient’s wrist with the ipsilateral hand. With the fingers of the other hand, friction is imparted to either the body of tendon or the insertion on the second metacarpal bone (Fig. 23.25). Friction is started at the ulnar aspect of the tendon and, during the active phase, the fingers are moved to the radial aspect.

Fig 23.25 Friction to the flexor carpi radialis.
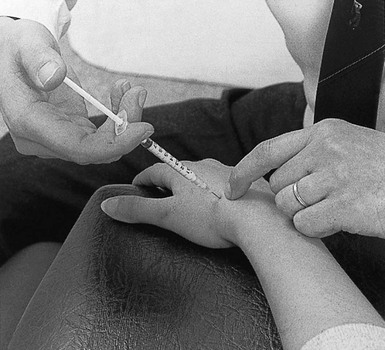
Technique: infiltration
The patient sits and places the supinated forearm on a high couch, the wrist slightly extended. A 1 mL syringe is filled with 10 mg triamcinolone acetonide and fitted with a 2 cm needle. The tendon and its insertion at the base of the second metacarpal bone are difficult to identify through the muscles of the thumb. Therefore, the base of the second metacarpal is palpated at the dorsum by the index finger while the thumb presses on the palmar side. The needle is inserted through the thenar muscles and directed towards the palpating index finger (Fig. 23.26). Before it touches bone, the resistance of a tendinous structure is felt. Infiltration is then performed.
Flexor carpi ulnaris
Tendinitis is more common at the ulnar flexor tendon (Fig. 23.27) than at the radial flexor tendon because of the greater mobility at the ulnar side.120 This lesion usually arises after a single excessive strain.
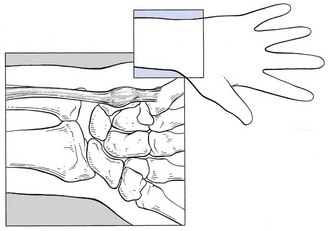
Fig 23.27 The flexor carpi ulnaris.
Usually, the patient can precisely locate the symptoms to the palmar and ulnar aspect of the wrist. Pain is elicited during resisted flexion and resisted ulnar deviations of the wrist. Palpation discloses the exact site of the lesion: distal to the pisiform bone – at the tenoperiosteal junction at the fifth metacarpal bone – or proximal to the pisiform bone in the body of the tendon.121
Technique: deep transverse friction
The patient sits with the arm held in supination and the hand hanging over the edge of the couch. The therapist, facing the patient, extends the patient’s wrist with the contralateral hand and imparts friction with the thumb of the other hand. Counterpressure is given at the dorsal aspect of the patient’s wrist (Fig. 23.28). Friction starts at the radial aspect of the tendon and finishes at the ulnar aspect.

Fig 23.28 Friction to the flexor carpi ulnaris.
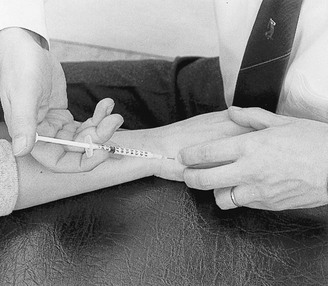
Technique: infiltration
This technique is particularly useful for a lesion at the insertion of the tendon onto the fifth metacarpal bone. The patient’s hand is brought into the same position as for friction. A 1 mL syringe, filled with 10 mg of triamcinolone acetonide and fitted with a 2 cm needle, is used. The tender area is located by palpation. The operator keeps the thumb on the painful spot during the whole procedure. After the needle is inserted, tendinous resistance should be felt before a series of droplets are deposited in contact with the bone (Fig. 23.29).
Pisotriquetral disorders
Disorders of the joint between the pisiform and the palmar surface of the triquetrum may occur and, because of the attachment of the tendon to the pisiform bone, give rise to the same signs as in flexor carpi ulnaris tendinitis.122 Disorders at the joint have been described as pisotriquetral arthritis123 and pisotriquetral instability.124 Direct pressure on the pisiform elicits pain. Side-to-side passive motion of the pisiform on the triquetrum will also lead to pain and crepitus. If pisotriquetral disorder is suggested, intra-articular steroid is required.125 In recurrent cases, surgical removal of the pisiform may be necessary.126,127
Flexor digitorum profundus
A rheumatoid tenovaginitis is usually confined to one flexor tendon near the carpus. Early in its progress, diffuse swelling and local warmth on the palmar aspect of the forearm are the only signs.128 Later, tenderness of the tendon may be found over a greater extent than that which occurs in overuse. After a few weeks, the swelling becomes nodular and local warmth persists.
The symptoms abate after one or two infiltrations with triamcinolone.
Swelling on a digital flexor tendon may sometimes lead to compression of the median nerve distal to the carpal tunnel, thus causing a partial syndrome (see the online chapter Nerve lesions and entrapment neuropathies of the upper limb).
Technique: deep transverse friction (mechanical tenosynovitis)
The patient sits at the couch with the forearm supinated, the hand hanging over the edge of the couch. The therapist approaches the patient’s arm from the radial side. With the ipsilateral hand, the wrist and fingers are brought into extension. The friction is applied with two or three fingertips of the other hand. Counterpressure is maintained with the thumb at the radial aspect of the patient’s forearm (Fig. 23.30).
Weakness
• C7 root palsy: in addition, there is marked weakness of extension of the elbow; the triceps jerk is seldom affected.
• C8 root palsy: both the extensor carpi ulnaris and the flexor carpi ulnaris are weak. The result is that the wrist moves radially when resisted flexion is tested. Resisted extension and adduction of the thumb are also weak.
Disorders of the contractile structures are summarized in Box 23.2.
References
1. Tiel-van Buul, MM, van Beek, EJ, Broekhuizen, AH, et al, Diagnosing scaphoid fractures: radiographs cannot be used as a gold standard!. Injury. 1992;23(2):77–79. ![]()
2. Dias, JJ, Brenkel, IJ, Finlay, DB, Patterns of union in fractures of the waist of the scaphoid. J Bone Joint Surg Br. 1989;71(2):307–310. ![]()
3. Steinmann, SP, Adams, JE, Scaphoid fractures and nonunions: diagnosis and treatment. J Orthop Sci 2006; 11:424–431. ![]()
4. Larsen, CF, Brøndum, V, Skov, O, Epidemiology of scaphoid fractures in Odense, Denmark. Acta Orthop Scand. 1992;63(2):216–218. ![]()
5. Calandra, JJ, Goldner, RD, Hardaker, WT, Scaphoid fractures: assessment and treatment. Orthopedics. 1992;15(8):931–937. ![]()
6. Hunter, JC, Escobedo, EM, Wilson, AJ, et al, MR imaging of clinically suspected scaphoid fractures. AJR Am J Roentgenol. 1997;168(5):1287–1293. ![]()
7. Rizzo, M, Shin, AY, Treatment of acute scaphoid fractures in the athlete. Curr Sports Med Rep. 2006;5(5):242–248. ![]()
8. Borgeskov, S, Christiansen, B, Kjær, AM, et al, Fractures of the carpal bones. Acta Orthop Scand 1966; 37:276. ![]()
9. Sherman, SB, Greenspan, A, Normal, A, Osteonecrosis of the distal pole of the carpal scaphoid following fracture – a rare complication. Skeletal Radiol 1983; 9:189. ![]()
10. Leslie, JJ, Dickson, RA, The fractured carpal scaphoid. J Bone Joint Surg. 1981;63(B):225. ![]()
11. Amadio, PC, Taleisnik, J, Fractures of the carpal bones. Operative Hand Surgery. Green, DP, eds. Operative Hand Surgery; vol 1. Churchill Livingstone, New York, 1993:799–860.
12. Van Tassel, DC, Owens, BD, Wolf, JM, Incidence estimates and demographics of scaphoid fracture in the U.S. population. J Hand Surg Am. 2010;35(8):1242–1245. ![]()
13. Amadio, PC, Scaphoid fractures. Orthop Clin North Am. 1992;23(1):7–17. ![]()
14. Green, MH, Hadres, AM, LaMont, RL, Scaphoid fractures in children. J Hand Surg 1984; 9A:536. ![]()
15. Weber, ER, Chao, EYS, An experimental approach to the mechanism of scaphoid waist fractures. J Hand Surg 1978; 3:142–148. ![]()
16. Mayfield, JK, Mechanism of carpal injuries. Clin Orthop Rel Res 1980; 149:45–54. ![]()
17. Adams, JE, Steinmann, SP, Acute scaphoid fractures. Orthop Clin North Am. 2007;38(2):229–235. ![]()
18. Donatelli, R, Wooden, MJ. Orthopaedic Physical Therapy. New York: Churchill Livingstone; 1989.
19. Berger, RA, The anatomy of the scaphoid. Hand Clin. 2001;17(4):525–532. ![]()
20. Gelberman, RH, Menon, J, The vascularity of the scaphoid bone. J Hand Surg 1980; 5A:508–513. ![]()
21. Taleisnik, J, Kelly, PJ, The extraosseous and intraosseous blood supply of the scaphoid bone. J Bone Joint Surg 1966; 48A:1125. ![]()
22. Tiel-van Buul, MMC, van Beek, EJR, Broekhuizen, AH, Diagnostic problems of scaphoid fractures: the value of radionuclide bone scintigraphy. Neth J Surg 1990; 42:50–52. ![]()
23. Nielsen, PT, Hedeboe, J, Thommasen, P, Bone scintigraphy in the evaluation of fracture of the carpal scaphoid bone. Acta Orthop Scand 1983; 54:303–306. ![]()
24. Stein, F, Miale, A, Stein, A, Enhanced diagnosis of hand and wrist disorders by triple phase radionucleide bone imaging. Bull Hosp J Dis 1984; 44:477–484. ![]()
25. Stordahl, A, Schjoth, A, Woxholt, G, et al, Bone scanning of fractures of the scaphoid. J Hand Surg 1984; 9B:189–190. ![]()
26. Bretlau, T, Christensen, OM, Edstrom, P, et al, Diagnosis of scaphoid fracture and dedicated extremity MRI. Acta Orthop Scand. 1999;70(5):504–508. ![]()
27. Breitenseher, MJ, Metz, VM, Gilula, LA, et al, Radiographically occult scaphoid fractures: value of MR imaging in detection. Radiology. 1997;203(1):245–250. ![]()
28. Brooks, S, Wluka, AE, Stuckey, S, Cicuttini, F, The management of scaphoid fractures. J Sci Med Sport. 2005;8(2):181–189. ![]()
29. Adams, JE, Steinmann, SP, Acute scaphoid fractures. Orthop Clin North Am. 2007;38(2):229–235. ![]()
30. Fisk, GR, The wrist. J Bone Joint Surg 1984; 66B:396. ![]()
31. Weber, ER, Chao, EY, An experimental approach to the mechanism of scaphoid wrist fractures. J Hand Surg 1978; 3A:142. ![]()
32. Bongers, KJ, Ponsen, RJG, Operative and nonoperative management of fractures of the carpal scaphoid: five years’ experience. Neth J Surg. 1980;32(4):142. ![]()
33. Cooney, WP, Dobyns, JH, Linscheid, RL, Fractures of the scaphoid: a rational approach to management. Clin Orthop Rel Res 1980; 149:90. ![]()
34. King, RJ, MacKenney, RP, Elnur, S, Suggested method for closed treatment of fractures of the carpal scaphoid: hypothesis supported by dissection and clinical practice. J Roy Soc Med 1982; 75:860. ![]()
35. Cooney, WP, Dobyns, JH, Linscheid, RL. Fractures of the scaphoid: a rational approach to management. Clin Orthop Rel Res. 1986; 202:79.
36. Tiel-van Buul, MMC, van Beek, EJR, Broekhuizen, AH, et al, Radiography and scintigraphy of suspected scaphoid fractures. J Bone Joint Surg. 1993;75B(1):61–65. ![]()
37. Herbert, TJ, Use of the Herbert bone screw in surgery of the wrist. Clin Orthop Rel Res 1986; 202:79. ![]()
38. Markiewitz, AD, Ruby, LK, O’Brien, ET. Carpal fractures and dislocations. In: Lichtman DM, Alexander AH, eds. The Wrist and its Disorders. 2nd ed. Philadelphia: Saunders; 1997:189–233.
39. Rodman GP, Schumacher R, eds. Primer on the Rheumatic Diseases, 8th ed, Atlanta: Arthritis Foundation, 1983.
40. Cimmino, MA, Bountis, C, Silvestri, E, et al, An appraisal of magnetic resonance imaging of the wrist in rheumatoid arthritis. Semin Arthritis Rheum. 2000;30(3):180–195. ![]()
41. Filippucci, E, Iagnocco, A, Meenagh, G, et al, Ultrasound imaging for the rheumatologist. Clin Exp Rheumatol 2006; 24:1–5. ![]()
42. Clayton, ML, Ferlic, DC, Arthrodesis of the arthritic wrist. Clin Orthop Rel Res 1984; 187:89. ![]()
43. Cyriax, JH. Textbook of Orthopaedic Medicine, vol I, Diagnosis of Soft Tissue Lesions, 8th ed. London: Baillière Tindall; 1982.
44. Peste: [Discussion]. Bull Soc Anat Paris. 1843; 18:169–170.
45. Kienböck, R. Über traumatische Malazie des Mondbeins und ihre Folgezustände: Entartungsformen und Kompressionsfrakturen. Fortsch Röntgenstrahlen. 1910; 16:78–103.
46. Almquist, EE, Kienböck’s disease. Hand Clin 1987; 3:141–148. ![]()
47. Alexander, CE, Alexander, AH, Lichtman, DM. Kienböck’s disease and idiopathic necrosis of carpal bones. In: Lichtman DM, Alexander AH, eds. The Wrist and its Disorders. 2nd ed. Philadelphia: Saunders; 1997:329–346.
48. Irisarri, C, Aetiology of Kienböck’s disease. Handchir Mikrochir Plast Chir. 2010;42(3):157–161. ![]()
49. Lichtman, DM, Alexander, AH, Mack, GR, Gunther, SF, Kienböck’s disease – update on silicone replacement arthroplasty. J Hand Surg 1982; 7A:343–347. ![]()
50. Alexander, AH, Lichtman, DM. The Kienböck’s dilemma – how to cope. In: Nakamura R, Linscheid RL, Miura T, eds. Wrist Disorders: Current Concepts and Challenges. Tokyo: Springer; 1992:79–87.
51. Lind, J, Hansen, LB, Lunatum malaci. Nord-Med. 1991;106(10):258–260. ![]()
52. Stahl, F. On lunatomalacia (Kienböck’s disease), a clinical and roentgenological study, especially on its pathogenesis and the late results of immobilization treatment. Acta Chir Scand. 1947; 126(suppl):1–133.
53. Lichtman, DM, Mack, GR, MacDonald, RI, et al, Kienböck’s disease: the role of silicone replacement arthroplasty. J Bone Joint Surg 1977; 59A:899–908. ![]()
54. Sundberg, SB, Linscheid, RL, Kienböck’s disease: results of treatment with ulnar lengthening. Clin Orthop Rel Res 1984; 187:43–51. ![]()
55. Jackson, MD, Barry, DT, Geiringer, SR, Magnetic resonance imaging of avascular necrosis of the lunate. Arch Phys Med Rehabil. 1990;71(7):510. ![]()
56. Horch, RE, Unglaub, F, Dragu, A, et al, Kienböck’s disease. Diagnosis and therapy. Chirurg. 2008;79(5):452–460. ![]()
57. Innes, L, Strauch, RJ, Systematic review of the treatment of Kienböck’s disease in its early and late stages. J Hand Surg Am. 2010;35(5):713–717. ![]()
58. Rahme, H, Idiopathic avascular necrosis of the capitate bone – case report. Hand. 1983;15(3):274–275. ![]()
59. Murakami, S, Nakajima, H, Aseptic necrosis of the capitate bone in two gymnasts. Am J Sports Med. 1984;12(2):170–173. ![]()
60. Park, MJ, Namdari, S, Weiss, AP, The carpal boss: review of diagnosis and treatment. J Hand Surg Am. 2008;33(3):446–449. ![]()
61. Jones, WA, Beware the sprained wrist: the incidence and diagnosis of scapholunate instability. J Bone Joint Surg 1988; 70B:293. ![]()
62. Friedman, SL, Palmer, AK, The ulnar impaction syndrome. Hand Clin 1991; 7:295–310. ![]()
63. Imaeda, T, Nakamura, R, Shionoya, K, Makino, N, Ulnar impaction syndrome: MR imaging findings. Radiology 1996; 201:495–500. ![]()
64. Dailey, SW, Palmer, AK, The role of arthroscopy in the evaluation and treatment of triangular fibrocartilage complex injuries in athletes. Hand Clin 2000; 16:461–476. ![]()
65. Leclercq, C, Arthroscopic treatment of the ulnar impaction syndrome. Chir Main. 2006;25(Suppl 1):S209–S213. ![]()
66. Topper, SM, Wood, MB, Ruby, LK, Ulnar styloid impaction syndrome. J Hand Surg [Am] 1997; 22:699–704. ![]()
67. Biyani, A, Mehara, A, Bhan, S, Morphological variations of the ulnar styloid process. J Hand Surg [Br] 1990; 15:352–354. ![]()
68. Garcia-Elias, M, Dorsal fractures of the triquetrum: avulsion or compression fractures? J Hand Surg [Am] 1987; 12:266–268. ![]()
69. Coggins, CA, Imaging of ulnar-sided wrist pain. Clin Sports Med. 2006;25(3):505–526. ![]()
70. Linscheid, RL, Dobyns, JH, Athletic injuries of the wrist. Clin Orthop Rel Res 1985; 198:141–151. ![]()
71. Dobyns, JH, Gabel, GT, Gymnast’s wrist. Hand Clin 1990; 6:493–505. ![]()
72. Snook, G, Injuries in women’s gymnastics. A five year study. Am J Sports Med. 1979;7(4):242. ![]()
73. Roy, S, Carne, D, Singer, K, Stress changes of the distal radial epiphysis in young gymnasts. Am J Sports Med 1985; 13:301–308. ![]()
74. Le, TB, Hentz, VR, Hand and wrist injuries in young athletes. Hand Clin. 2000;16(4):597–607. ![]()
75. Read, MT, Stress fractures of the distal radius in adolescent gymnasts. Br J Sports Med 1981; 15:272–276. ![]()
76. Hanks, G, Kalenak, A, Bowman, L, et al, Stress fracture of the carpal scaphoid: a report of four cases. J Bone Joint Surg 1989; 71A:938–941. ![]()
77. Schultz, RJ, Kearns, RJ, Tumors in the hand. J Hand Surg 1983; 8:803–806. ![]()
78. Angelides, AC, Wallace, PF, The dorsal ganglion of the wrist: its pathogenesis, gross and microscopic anatomy, and surgical treatment. J Hand Surg 1976; 1:228. ![]()
79. Bogumill, GP. Tumors of the wrist. In: Lichtman DM, Alexander AH, eds. The Wrist and its Disorders. 2nd ed. Philadelphia: Saunders; 1997:563–581.
80. Ekenstam, FA. Wrist stability/wrist instability. In: Büchler U, ed. Wrist Instability. Federation of European Societies for Surgery of the Hand. London: Martin Dunitz; 1996:25.
81. Gilford, W, Bolton, R, Lambrinudi, C. The mechanism of the wrist joint. Guy’s Hosp Rep. 1943; 92:52–59.
82. Ruch, DS, Bowling, J, Arthroscopic assessment of carpal instability. Arthroscopy. 1998;14(7):675–681. ![]()
83. Mayfield, JK. Pathogenesis and pathokinetics of wrist ligament instability. In: Lichtman DM, Alexander AH, eds. The Wrist and its Disorders. 2nd ed. Philadelphia: Saunders; 1997:55–72.
84. Larsen, CF, Amadio, PC, Gilula, LA, Hodge, JC, Analysis of carpal instability. I. Description of the scheme. J Hand Surg 1995; 20A:757–764. ![]()
85. Angermann, P, Lohmann, M, Injuries to the hand and wrist. A study of 50,272 injuries. J Hand Surg 1993; 18B:642–644. ![]()
86. Saffar, P. Classification of carpal instabilities. In: Büchler U, ed. Wrist Instability. Federation of European Societies for Surgery of the Hand. London: Martin Dunitz; 1996:29–33.
87. Taleisnik, J, The ligaments of the wrist. J Hand Surg 1976; 1:110–118. ![]()
88. Taleisnik, J, Post-traumatic carpal instability. Clin Orthop Rel Res 1980; 149:73–82. ![]()
89. Navarro, A. Luxaciones del carpo. An Fac Med (Montevideo). 1921; 6:113.
90. Taleisnik, J. Carpal instability. In: Tubiana R, ed. The Hand. Philadelphia: Saunders; 1985:986–1000.
91. Mayfield, JK, Johnson, RP, Kilcoyne, RF, Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg 1980; 5:226–241. ![]()
92. Amadio, PC, Pain dysfunction syndromes. J Bone Joint Surg. 1988;70A(6):944–949. ![]()
93. Amadio, PC, Epidemiology of hand and wrist injuries in sports. Hand Clin. 1990;6(3):379–381. ![]()
94. Linscheid, RL, Dobyns, JH, Beabout, JW, Bryan, RS, Traumatic instability of the wrist: diagnosis, classification and pathomechanics. J Bone Joint Surg 1972; 54A:1612–1632. ![]()
95. Linscheid, RL, Dobyns, JH, Beckenbaugh, RD, et al, Instability patterns of the wrist. J Hand Surg 1983; 8A:682–686. ![]()
96. Cooney, WP, Dobyns, JH, Linscheid, RL, Arthroscopy of the wrist: anatomy and classification of carpal instability. Arthroscopy 1990; 6:133–140. ![]()
97. Lichtman, DM. Introduction to the carpal instabilities. In: Lichtman DM, Alexander AH, eds. The Wrist and its Disorders. 2nd ed. Philadelphia: Saunders; 1997:187.
98. Taleisnik, J, Current concepts review. Carpal instability. J Bone Joint Surg 1988; 70A:1262–1268. ![]()
99. Dumontier, C. The clinical diagnosis of wrist instability. In: Büchler U, ed. Wrist Instability. Federation of European Societies for Surgery of the Hand. London: Martin Dunitz; 1996:35–44.
100. Watson, HK, Black, DM, Instability of the wrist. Hand Clin 1987; 3:103–111. ![]()
101. Watson, HK, Ashmead, D, Makhoulf, MV, Examination of the scaphoid. J Hand Surg 1988; 13A:657–660. ![]()
102. Lane, LB, The scaphoid shift test. J Hand Surg 1993; 18A:366–368. ![]()
103. Ambrose, L, Posner, MA, Lunate-triquetral and midcarpal joint instability. Hand Clin 1992; 8:653–668. ![]()
104. Linscheid, RL, Dobyns, JH. Physical examination of the wrist. In: Post M, ed. Physical Examination of the Musculoskeletal System. Chicago: Year-Book; 1987:80–94.
105. Lichtman, DM, Schneider, JR, Swafford, AR, Mack, GR, Ulnar midcarpal instability – clinical and laboratory analysis. J Hand Surg 1981; 6A:515–523. ![]()
106. Johnson, RP, Carrera, GF, Chronic capitolunate instability. J Bone Joint Surg 1986; 68A:1164–1176. ![]()
107. Truong, NP, Mann, FA, Gilula, LA, Kang, SW, Wrist instability series: increased yield with clinical–radiologic screening criteria. Radiology 1994; 192:481–484. ![]()
108. Schernberg, F. Le Poignet – anatomie radiologique et chirurgie. Paris: Masson; 1992.
109. Grundberg, AB, Reagan, DS, Pathologic anatomy of the forearm: intersection syndrome. J Hand Surg. 1985;10A(2):299. ![]()
110. Futami, T, Itoman, M, Extensor carpi ulnaris syndrome. Findings in 43 patients. Acta Orthop Scand. 1995;66(6):538–539. ![]()
111. Wood, MD, Dobyns, JH, Sports related extraarticular wrist syndrome. Clin Orthop Rel Res 1986; 202:93–102. ![]()
112. Crimmins, CA, Jones, NF, Stenosing tenosynovitis of the extensor carpi ulnaris. Ann Plast Surg. 1995;35(1):105–107. ![]()
113. Bowers, WH, Zelouf, DS. Treatment of chronic disorders of the distal radioulnar joint. In: Lichtman DM, Alexander AH, eds. The Wrist and its Disorders. 2nd ed. Philadelphia: Saunders; 1997:440.
114. Montalvan, B, Parier, J, Brasseur, JL, et al, Extensor carpi ulnaris injuries in tennis players: a study of 28 cases. Br J Sports Med. 2006;40(5):424–429. ![]()
115. Inoue, G, Tamura, Y, Recurrent dislocation of the extensor carpi ulnaris tendon. Br J Sports Med. 1998;32(2):172–174. ![]()
116. Linden, MA, Manton, WI, Stewart, M, et al, Lead poisoning from retained bullets. Ann Surg 1982; 195:305. ![]()
117. Bishop, AT, Gabel, GT, Carmichael, SW, Flexor carpi radialis tendonitis. Part I: Operative anatomy. J Bone Joint Surg 1994; 76A:1009–1013. ![]()
118. Gazarian, A, Foucher, G, La Tendinite du grand palmaire: à propos de vingt-quatre cas. Ann Chir Main Memb Super. 1992;11(1):14. ![]()
119. Gabel, G, Bishop, AT, Wood, MB, Flexor carpi radialis tendinitis. J Bone Joint Surg 1994; 76A:1015–1018. ![]()
120. Kulund, DN. The Injured Athlete, 2nd ed. Philadelphia: Lippincott; 1988.
121. Wick, MC, Weiss, RJ, Arora, R, et al, Enthesiopathy of the flexor carpi ulnaris at the pisiform: findings of high-frequency sonography. Eur J Radiol. 2011;77(2):240–244. ![]()
122. Beckers, A, Koebke, J, Mechanical strain at the pisotriquetral joint. Clin Anat. 1998;11(5):320–326. ![]()
123. Helal, B, Racquet players pisiform. Hand 1978; 10:87–91. ![]()
124. Buterbaugh, GA, Brown, TR, Horn, PC, Ulnar-sided wrist pain in athletes. Clin Sports Med. 1998;17(3):567–583. ![]()
125. Palmieri, TJ, Pisiform area pain treatment by pisiform excision. J Hand Surg 1982; 7:477–480. ![]()
126. Carroll, RE, Coyle, MP, Dysfunction of the pisotriquetral joint: treatment by excision of the pisiform. J Hand Surg 1985; 10A:703–707. ![]()
127. Gómez, CL, Renart, IP, Pujals, JI, et al, Dysfunction of the pisotriquetral joint: degenerative arthritis treated by excision of the pisiform. Orthopedics. 2005;28(4):405–408. ![]()
128. Alnot, JY, Rheumatoid arthritis of the wrist with adult onset. Acta Orthop Belg. 2000;66(4):329–336. ![]()