Disorders of the sacroiliac joint
Introduction
After the fifth decade of life, fibrosis takes place between the cartilage surfaces and by the seventh decade the joint has usually undergone fibrous ankylosis. The available range of movement decreases as fibrous ankylosis increases.1
Most pain in the sacroiliac or gluteal region does not originate from the sacroiliac joint but is referred pain of discodural origin (see Ch. 33); every diagnosis of a ‘sacroiliac lesion’ should be made with caution and only after other common sources of ‘sacroiliac pain’ have been ruled out.
The pathological conditions affecting the sacroiliac joint are inflammatory and mechanical. The latter is usually referred to as ‘sacroiliac joint syndrome’.2 The exact nature of the syndrome is not known but it is generally accepted that mechanical pain stems from minor subluxations and/or ligamentous strain.
Sacroiliac arthritis
Ankylosing spondylitis
Introduction
Once considered a rare disease, ankylosing spondylitis (AS) is now recognized as relatively common, affecting up to 0.5–1.0% of the population.3 The ratio of occurrence in males and females is approximately 5 : 1, although it was previously thought to be 20 : 1. Several studies now suggest that it may occur almost as frequently in females as in males, although in a milder form and with more peripheral localization.4,5 The disease is characterized by fibrosis and ossification of ligaments and capsules rather than the joint destruction so typical of rheumatoid disease.6
Ankylosing spondylitis almost invariably starts at the sacroiliac joints and then extends upwards to involve the spine at increasingly higher levels. However, the sacroiliitis very often remains silent. It has been estimated that no more than 1 case in 10 ever has pain in the buttock. Most spondylitis begins as a diffuse lumbar ache, and sometimes the earlier symptoms are thoracic or cervical (Cyriax7: p. 366). AS frequently involves extraspinal joints, tendons and ligaments. The disorder may affect all body systems: iritis, pulmonary diseases, chronic prostatitis and cardiovascular diseases are now recognized as possible complications of the disease.8–12
Diagnosis of AS is not always easy, particularly in the early stages when only the pelvis is affected. Clinical criteria have been developed during recent decades.13,14 These criteria are usually not appropriate. Radiologically documented sacroiliitis is obligatory for making a definite diagnosis but it may take years before the radiological abnormalities of the sacroiliac joints can be demonstrated without doubt.15,16 Recently, magnetic resonance imaging (MRI) has proven its value in the early detection of sacroiliitis, with an estimated sensitivity and specificity of about 90%.15 Active sacroiliitis on MRI precedes the future appearance of sacroiliitis on radiographs by 8–9 years.17,18 The clinical criteria, such as decreased chest expansion and symmetrical limitation of spinal movements, also occur relatively late in the course of AS, at a time when the disease should be obvious on other grounds (Box 43.1).
The natural history of the disease in an individual is extremely difficult to define or predict. Some patients have disease limited to the pelvis and the majority have a good outlook for a successful life pattern. Only in a small minority of patients does AS progress to the well-known total ankylosis.19
Sacroiliitis
Symptoms
The patient is usually between 15 and 40 years old and complains of unilateral gluteal pain. Because the sacroiliac joints are largely derived from the first and second sacral segments, the pain commonly radiates to the back of the leg as far as the heel. The localization of the pain is thus the same as in S1 or S2 nerve root compression. However, in sacroiliac arthritis it never spreads to the foot, and paraesthesia is absent. As in discodural problems, coughing (which increases intra-abdominal pressure) may cause pain in the buttock and down the leg. The localization and extent of pain, together with the painful cough, may lead to the assumption that an ordinary discoradicular conflict is present.20 Some specific characteristics then help to distinguish sacroiliac arthritis from disc diseases. The main feature is that the pain comes and goes in an irregular and unpredictable way. During a flare-up, the pain is constantly present; during remission, the patient can exercise freely without an increase in symptoms. An attack is usually unprovoked: if pain is present it is usually increased by exertion, but if it is absent it cannot be stimulated. This is the reverse of the history in disc lesions, where the pain always follows certain activities and subsides after their avoidance. Another important feature is that sacroiliac pain often alternates from one side to the other, though it is seldom bilateral except when it changes sides.21
Signs
Given the similarity with S1 or S2 root compression, the index of suspicion usually remains low and the diagnosis is often missed (Table 43.1).
Table 43.1
Differential diagnosis of sacroiliac arthritis and S1–S2 disc lesions
| Arthritis | S1–S2 root compression | |
| History | ||
| Gluteal pain | Spreading in S1–S2 dermatomes | Spreading in S1–S2 dermatomes |
| Flaring/constant pain | Flares | Constant |
| Coughing | Painful | Painful |
| Morning symptoms | Pain on awakening, improved by walking | Pain on getting out of bed |
| Prolonged morning stiffness | ||
| Association with activity | Pain irrespective of exertion | Pain follows certain activities |
| Pain localization | Alternating | Unilateral |
| Not beyond the ankle | Often in the foot | |
| Paraesthesia | Never present | In foot or toes |
| Clinical examination | ||
| Extension and side flexion | Full | Often limited |
| Flexion | May be slightly limited | Usually grossly limited |
| Straight leg raising | May be painful at the end | Usually limited |
| Sacroiliac distraction test | Painful | Painless |
During the examination in a standing position no suspicion arises. There may be a slight increase in gluteal pain during extension and bending towards the painful side; flexion is limited because of increasing pain in the buttock and thigh; and sometimes a slight deviation towards the painful side can be noted during flexion.22 Straight leg raising may also cause pain at the end of range.23
It is only when the anterior part of the sacroiliac joint is tested (see Ch. 41) that the diagnosis becomes obvious. Unilateral or gluteal or posterior crural pain during the test incriminates the sacroiliac joint. This manœuvre is an extremely sensitive method of deciding whether the sacroiliac joint is affected, and a positive distraction test often precedes radiological evidence of sacroiliac arthritis by years. Although many other tests for the sacroiliac joints have been described, the distraction technique as described earlier is the most significant test of the status of the joint; it applies immediate stress to the anterior part of the joint, without using a lever – distraction forces using the patient’s femur as a lever are very non-specific and should therefore not be used as screening tests. Because of the specificity of the sacroiliac distraction test, it is an essential part of the routine clinical examination of the lumbar spine.
Although some authors find tenderness over the sacroiliac joint highly indicative of the existence of sacroiliac arthritis,24 we believe that palpating for tenderness adds no further information and only confuses the examiner. First, the joint, covered as it is by the overhang of the ilium and the sacral extent of the sacrospinalis muscle, remains beyond the direct reach of the palpating finger. Second, the sacroiliac region is a common site for referred tenderness in lumbar discodural conflicts.
Further examination
Radiological evidence of sacroiliitis is accepted as being obligatory for the diagnosis of AS. However, the clinical symptoms may predate the radiological abnormalities by months or even years. In the early stages, when radiological signs are minimal and of questionable significance, it may help to use computed tomography (CT) for demonstrating joint narrowing and fusion.25
The changes are classified according to the New York criteria in five grades (grades 0–IV; Table 43.2). Initially, there is patchy periarticular osteoporosis, leading to loss of definition of the subchondral bone plate. The joint thus appears to be widened. Further evolution of the process results in superficial erosion, together with focal sclerosis of subchondral bone. Further proliferative changes result in irregular bridging across the articular cavity. This causes blurring and indistinct margins on both sides of the joint. Finally, the radiograph shows complete osseous fusion.
Table 43.2
Sacroiliac changes in ankylosing spondylitis26
| Grade | Changes |
| 0 | None |
| I Suspicious | Patchy periarticular osteoporosis |
| II Minimal | Loss of definition at the edge of the joints |
| Some sclerosis | |
| Minimal erosion | |
| III Definite | Definite sclerosis on both sides |
| Blurring and indistinct margins | |
| Loss of joint space | |
| IV Ankylosis | Complete fusion of the joint |
The best way to detect active sacroiliitis is on MRI. An MRI is considered as ‘positive’ if the areas of bone marrow oedema (BME) are located at typical sites, i.e. they are periarticular to the sacroiliac joints. When only one BME lesion is visible on an MRI slice, it should be clearly visible on consecutive slices. Enthesitis, capsulitis and synovitis reflect active inflammation as well and are certainly compatible with AS; however, they are not sufficient for a ‘positive’ MRI if present without concomitant BME.27
Association with HLA-B27
The association between the genetic marker HLA-B27 and AS is well known.28,29 The frequency of HLA-B27 in healthy populations is between 1% (Japanese and African) and 14% (Caucasian), whereas the marker is present in 90% of the AS population.17 However, the presence of HLA-B27 plays little or no role in diagnosis of the disease: a patient with repeatedly normal radiographs is unlikely to have the disease, regardless of HLA status; in contrast, a B27-negative individual with symptoms suggesting AS has the disease if the radiograph shows the typical changes.30
Natural history
The prognosis for an individual is difficult to predict. In some patients the disorder is limited to the pelvis, whereas others quickly develop spinal and extraskeletal disease. The younger the patient is at the age of onset, the worse the outcome, and men usually fare worse than women.31 When sacroiliac arthritis appears after the age of 25 years, the disease is likely to follow a mild course: bilateral sacroiliitis continues flaring up and subsiding for some years until bony ankylosis is complete and the pain disappears. If the disease spreads upwards, its spread is very slow and the thoracic spine is only affected when the patient is 40 or 50 years of age. In these patients the cervical spine usually remains unaffected and the hips retain full mobility. In contrast, when sacroiliac arthritis appears before the age of 20 years, or spondylitis has reached the lumbar spine before the age of 25 years, early and severe disablement is very probable; pain and stiffness spread upwards along the spine very quickly and there is also a strong chance of hip involvement within 20 years of onset.32
Treatment
Pain and inflammation are treated by non-steroidal anti-inflammatory drugs (NSAIDs). Indometacin is considered the drug of choice. The patient must be informed that therapy should be continuous and that the purpose of medication is to allow normal activities to be pursued and the daily posture and exercise routine to be carried out. Anti-tumour necrosis factor (TNF) agents are recommended in the case of NSAID failure.33 Over the past few years, several placebo-controlled and open trials have shown a dramatic response in active AS to TNFα-blocking agents (infliximab and etanercept). In these trials, 50–70% of patients showed an improvement of 50% or more.34,35
Psoriasis
The true prevalence of sacroiliitis in psoriasis is unknown. The majority of estimates are in the range of 20–30%.36,37 The link between the skin condition and the joint disease is unknown. The disease is frequently unilateral or asymmetrical, and can be asymptomatic. The clinical presentation is pain and a positive sacroiliac distraction test – the same as in AS. Treatment of the sacroiliitis is with NSAIDs.
Reiter’s syndrome
Although a high percentage (more than 30%) of patients with the syndrome show severe radiological sacroiliitis,38 only a small percentage develop clinical evidence of unilateral or bilateral sacroiliac arthritis. Clinical evidence of sacroiliac joint involvement may occur as early as 3 months from the onset of the illness.39
Septic arthritis
A pyogenic infection of the sacroiliac joints is rare, although in recent years more reports have been published on this topic.40–42 The infection reaches the joint by the haematogenous route or by direct extension from a contiguous abscess. Predisposing factors are pregnancy, intravenous drug abuse and immunosuppression.
The initial diagnosis is often overlooked because of its rarity and the poorly localized symptoms and signs. The condition should be considered in cases of acute or subacute onset of pain in the gluteal region, hip or low back, accompanied by fever. An apparent acute abdomen may be present, especially in children.43,44
The diagnosis is strongly suspected when the ‘sign of the buttock’ is found during clinical examination of the back (see p. 637). Roentgenograms are often normal. CT scan and MRI may be useful tools but radionuclide scanning with 99mTc or 67Ga usually affords early confirmation of the condition.45–47 Generally, antibiotic treatment leads to complete recovery.
Gout
Gout is usually considered to be a disorder of the peripheral joints. However, since 1965, it has been recognized that the sacroiliac joint is also radiologically affected at a late stage in a significant percentage (7–17%) of patients with tophaceous gout.48,49 The sacroiliitis usually remains clinically silent, acute attacks being rare.50
Sacroiliac joint syndrome
Introduction
The ability of mechanical lesions of the sacroiliac joint to cause backache and referred pain to the buttock and posterior leg was first recognized by Goldthwait and Osgood in 1905.52
Some schools of thought have put great emphasis on the joint and consider the sacroiliac joint syndrome as a common source of low back and pelvic pain.53 Although it is generally accepted that most pain in the sacroiliac region is of dural origin and has nothing to do with an actual lesion of the joint,7,54 it is logical to accept the sacroiliac joint as a prime cause of pain because it is a synovial joint and thus subject to the same dysfunctional conditions that affect other synovial joints. It is not difficult to accept ligamentous sprain and overuse phenomena in and around the sacroiliac joint as possible sources of ‘dysfunctional’ pain. It is, however, more difficult to identify a ‘blocked sacroiliac subluxation’ as the main cause of the dysfunction.
Numerous tests to detect dysfunction of the sacroiliac joint have been described in the chiropractic and manual medicine literature. Although commonly used, many of these tests are difficult to perform or to interpret, and consequently their intertester reliability is low (see p. 599). In particular, those tests that assess motion (or the lack of it) in a sacroiliac joint are not reliable. Pain provocation tests – stressing the structures in an attempt to reproduce the patient’s symptoms – have a much better intertester reliability and can be used to detect sacroiliac joint syndrome.
We therefore do not discuss blocked sacroiliac joints as a possible source of sacroiliac dysfunction. The issue is too controversial and today there exists no clear evidence for the disorder. Sacroiliac strain, by contrast, is a well-delineated entity with typical signs and symptoms. Recent studies demonstrated temporary pain relief after local blocks of the sacroiliac joint, thus confirming the sacroiliac joint as a real source of low back pain.55–57 However, it is worth repeating that the diagnosis requires typical physical findings and that tenderness over the sacral sulcus and the posterior sacroiliac joint line are not sufficient in themselves to make the diagnosis.
History
Sacroiliac joint syndrome or strain usually occurs in women between the ages of 15 and 35 years. The ligaments may have been strained by a fall on the buttocks or a motor vehicle accident. Other more trivial mechanisms of injury may also be linked to the development of sacroiliac joint syndrome, such as stepping into an unexpected hole or miscalculating a height.58 Alternatively, the strain can be associated with pregnancy. Hormonal changes can cause relaxation of the sacroiliac ligaments; during pregnancy and parturition, the joint will therefore be more susceptible to strain.
Pain is usually unilateral (although bilateral pain may occur), is never alternating, and is localized in the sacroiliac region with reference to the buttock and the posterolateral aspect of the thigh and calf.59
The pain has typical postural characteristics in that it appears only after prolonged or increased loading of the ligaments. It is therefore typical that pain is brought on by the maintenance of prolonged postures.60 As a rule, it is increased by excessive standing or by strolling, and is abolished by correction of posture or by movement. Resting will also decrease the symptoms, although lying down – for example, in a fixed position – may cause pain. Pain is often aggravated by bending and by climbing stairs. Dural signs, such as pain during coughing and sneezing, are absent. Neurological symptoms – paraesthesia and weakness – do not occur.
The condition is persistent, though rare cases of spontaneous recovery do occur.
Clinical examination
As pain at the sacroiliac area is usually of dural origin, the diagnosis of sacroiliac strain (summarized in Box 43.2) must always be made sparingly. Examination of the lumbar spine shows a full range of movement, sometimes with pain at the end of range of flexion or extension. There may be pain if weight is borne on the ipsilateral extremity. Straight leg raising is full-range, although pain at the end of range may be encountered.61 In severe cases, some hip movements (flexion, medial rotation and extension) may be painful at the end of range. Resisted abduction and resisted extension of the leg may also provoke pain.
It is possible for the sacroiliac distraction test (included in the basic lumbar clinical examination) to remain negative. As this test pulls on the anterior ligaments only, the stress is not always adequate to provoke pain in the posterior ligaments. More vigorous movements, performed with leverage of the hip, will then be required to stress the posterior ligaments (see pp. 949–952). It is worth emphasizing again that most of these tests are non-specific in that they assume that the hip is completely normal. A positive test is therefore significant only when the clinical examination has ruled out lumbar and hip disorders.62
Treatment
Training programme
Vleeming et al consider an inadequate ‘force closure’ of the sacroiliac joints as an important cause of sacroiliac strain. Force closure is defined as the compressive stabilizing forces exerted by ligaments and coupled bilateral gluteal and back muscles. The authors hypothesize that ligaments alone are not capable of transferring lumbosacral load effectively from the spine to the iliac bones. This is particularly the case in heavy load situations and conditions of sustained load, such as sitting and standing for a long time in a relatively counternutated position of the sacrum.63–66 Muscle weakness and inadequate coordination between muscles diminish force closure, which consequently increases the load on the pelvic ligaments. The ligaments become strained, leading to pain and laxity.
Belt
The symptoms may be abolished permanently if the joint and the ligaments are protected for a month or so by the wearing of an appropriate belt. The most suitable type is a very tight, non-elastic 6 cm wide belt, placed around the pelvis between the iliac crest and the greater trochanter (Fig. 43.1).
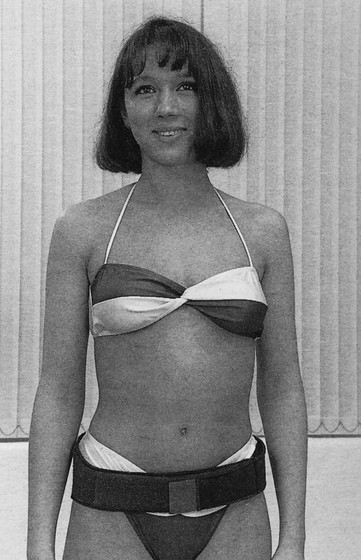
Fig 43.1 A belt for sacroiliac strain.
The biomechanical effects of such a belt in human pelvis–spine preparations were studied by Vleeming et al,65 who found that it led to a significant decrease in rotation at the sacroiliac joints. Both the location of the belt and the degree of loading were crucial. An optimal decrease in movement was reached with a belt worn at the level just cranial to the trochanter.
The active straight leg raising test, described by Mens et al,67 seems to have some prognostic value. Lying supine, the patient is asked to lift the leg about 5 cm off the couch. In a serious pelvic dysfunction the patient is unable to do so or the strength on one side is considerably less. The test is repeated after stabilizing the pelvis with a belt or by manual pressure on the iliac spines from the lateral side. If this lateral pressure converts a painful active straight leg raising test into a painless one, wearing a belt will lead to a good result.
Sclerosing injections
If wearing a pelvic belt fails to improve the patient’s condition, sclerosing injections into the posterior sacroiliac ligaments are indicated. We use Ongley’s solution (2% phenol, 25% dextrose, 15% glycerol). This mixture has a good safety record and, apart from considerable pain for up to 2 days after the injection, it causes no side effects. It induces an inflammatory response, which leads to fibroblast proliferation and new collagen production (see pp. 112–114). Because of pain, the solution must be mixed with 2% lidocaine, in a proportion of 80% sclerosant and 20% lidocaine.
Usually all the sacroiliac ligaments are treated at their ligamentoperiosteal junction. Although it is possible to be very selective and to infiltrate only small groups of ligaments, better results will be achieved if all the ligaments on both sides are infiltrated.68
A 10 mL syringe, filled with 8 mL sclerosant and 2 mL lidocaine, is fitted to a 7 cm long needle.
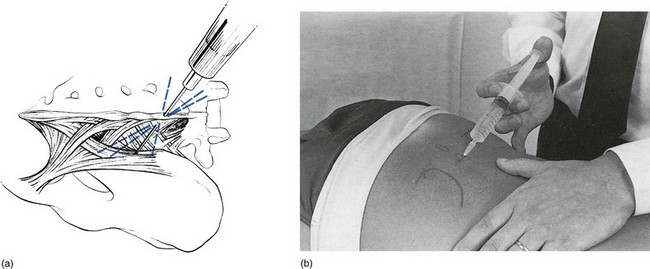
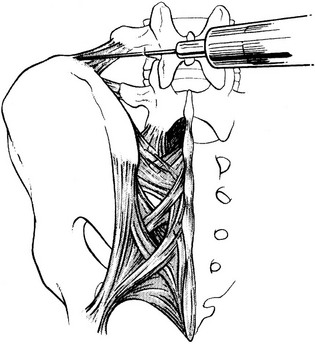
The skin is punctured at the level of the tip of the first sacral spine. From here, the following ligaments on both sides can be infiltrated: the posterior sacroiliac, the interosseous sacroiliac, the sacrotuberous and the sacrospinous (the latter two form the sacral attachments). To reach the posterior sacroiliac ligament, the tip of the needle is directed at an angle of 30° to the skin and thrust laterally until it touches bone. Four to five small injections are made along the posterior aspect of the posterior superior spine. It should be stressed that no fluid is introduced unless the tip of the needle is felt to impinge on bone (Fig. 43.2).
The iliac insertion of the iliolumbar ligament is infiltrated via a separate skin puncture. The needle is inserted about 3 cm lateral to the fifth supraspinous process. The palpating thumb is placed at the medial edge of the iliac crest. The tip of the needle is thrust in very obliquely in the direction of the thumb, until it is felt to traverse a resistant ligament before touching bone (Fig. 43.3). An infiltration of 1 mL is performed along the border, deeply and superficially, by multiple withdrawals and reinsertions. Care is taken to inject only when the needle touches bone.
Bony disorders of the pelvis
Tumours
Sacral tumours, both primary and secondary, are rare lesions. They often escape early diagnosis.
Most patients with sacral tumours have a non-specific complaint of low back pain. However, the history will reveal some unusual features typical of non-mechanical lesions in the lumbar spine, currently referred to as ‘warning symptoms’ (see Ch. 39):
• Continuous pain, not altered by changing positions or activities
Clinical examination may reveal local tenderness and swelling. Both lumbar examination and sacroiliac pain provocation tests may be positive. The most striking clinical finding is usually the appearance of a ‘sign of the buttock’ (see p. 637), which draws immediate attention to a serious pelvic lesion.
Radical resection is the treatment of choice for sacral chordomas. Addition of radiation after subtotal resection improves the disease-free interval, although radiation therapy can generally be used only once.69,70
Fractures of the sacrum
The diagnosis and treatment of these lesions are beyond the scope of this book. However, insufficiency fractures of the sacrum usually develop in the absence of obvious trauma and must therefore be included in the differential diagnosis of sacroiliac lesions. Insufficiency fractures of the sacrum usually occur in elderly women with postmenopausal osteoporosis. They are often confused with disc lesions, spinal stenosis and cauda equina syndrome. Sacroiliac tests are very painful and there is a ‘sign of the buttock’ (see p. 637).
A CT scan is often necessary to demonstrate the fracture line. Treatment consists of rest.71,72
References
1. Bowen, V, Cassidy, JD, Macroscopic and microscopic anatomy of the sacroiliac joint from embryonic life until the eighth decade. Spine 1981; 6:620–628. ![]()
2. Bernard, TN, Cassidy, JD. The sacroiliac joint syndrome. In: Frymoyer JW, ed. The Adult Spine: Principles and Treatment. New York: Raven Press; 1991:2107–2130.
3. Gran, JT, Husby, G, Hordvik, M, Prevalence of ankylosing spondylitis in males and females, in a young middle-aged population in Tromsö, northern Norway. Ann Rheum Dis 1985; 44:359. ![]()
4. Calin, A, Fries, JF, The striking prevalence of ankylosing spondylitis in ‘healthy’ W27 positive males and females. A controlled study. N Engl J Med 1975; 293:835. ![]()
5. Dequeker, J, Decock, T, Walravens, M, Van de Putte, I, A systematic survey of the HLA-B27 prevalence in inflammatory rheumatic diseases. J Rheumatol 1978; 5:453. ![]()
6. Ball, J, Enthesopathy of rheumatoid and ankylosing spondylitis. Ann Rheum Dis 1971; 30:213. ![]()
7. Cyriax, JH. Textbook of Orthopaedic Medicine. vol 1, 8th ed. London: Baillière Tindall; 1982.
8. Blumberg, B, Ragan, C, The natural history of rheumatoid spondylitis. Medicine 1956; 35:1. ![]()
9. Anonymous, The lungs in ankylosing spondylitis (editorial). BMJ 1971; 3:492. ![]()
10. Mason, RM, Murray, RS, Oates, JK, Prostatitis and ankylosing spondylitis. BMJ 1958; 1:748. ![]()
11. Tucker, CR, Fowles, RE, Calin, A, Aortitis in ankylosing spondylitis: early detection of aortic root abnormalities with two-dimensional echocardiography. Am J Cardiol 1982; 9:680. ![]()
12. Bergfeldt, L, HLA B27 associated rheumatic diseases with severe cardiac bradyarrhythmias: clinical features and prevalence in 223 men with permanent pacemakers. Am J Med 1983; 75:210. ![]()
13. Van der Linden, SJ, Valkenburg, HA, Cats, A, Evaluation of diagnostic criteria for ankylosing spondylitis. Arthritis Rheum 1984; 27:361. ![]()
14. Cats, A, Van der Linden, SJ, Goeithe, HS, Khan, MA, Proposals for diagnostic criteria of ankylosing spondylitis and allied disorders. Clin Exp Rheumatol 1987; 5:167–171. ![]()
15. Rudwaleit, M, Khan, MA, Sieper, J, The challenge of diagnosis and classification in early ankylosing spondylitis: do we need new criteria? Arthritis Rheum 2005; 52:1000–1008. ![]()
16. Agarwal, A. Pre-ankylosing spondylitis. In: Moll JMH, ed. Ankylosing Spondylitis. New York: Churchill Livingstone, 1980.
17. Rostom, S, Dougados, M, Gossec, L, New tools for diagnosing spondyloarthropathy. Joint Bone Spine 2010; 77:108–114. ![]()
18. Bennett, AN, McGonagle, D, O’Connor, P, et al, Severity of baseline magnetic resonance imaging-evident sacroiliitis and HLA-B27 status in early inflammatory back pain predict radiographically evident ankylosing spondylitis at eight years. Arthritis Rheum 2008; 58:3413–3418. ![]()
19. Calin, A. Ankylosing spondylitis. In: Fries JF, Ehrlich GE, eds. Prognosis: Contemporary Outcomes of Disease. Bowie, MD: The Charles Press; 1981:357–359.
20. Rosen, PS, Graham, DC. Ankylosing (Strumpell–Marie) spondylitis – a clinical review of 128 cases. Arch Interam Rheum. 1962; 5:158.
21. Ogryzlo, MO, Ankylosing spondylitisHollander JL, McCarthy DJ, eds. Arthritis and Allied Conditions. Lea & Febiger: Philadelphia, 1972:699–723. ![]()
22. Solonen, KA, The sacroiliac joint in the light of anatomical, roentgenological and clinical studies. Acta Orthop Scand. 1957;27(suppl):1–127. ![]()
23. Grieve, GP, The sacro-iliac joint. Physiotherapy 1976; 62:384–400. ![]()
24. Bellamy, N, Park, W, Rooney, PJ, What do we know about the sacro-iliac joint? Sem Arthritis Rheum. 1983;12(3):282–313. ![]()
25. Wilkinson, M, Meikle, JAK, Tomography of the sacro-iliac joints. Ann Rheum Dis 1966; 25:433–439. ![]()
26. Gofton, JP, Report from the subcommittee on diagnostic criteria for ankylosing spondylitisBennett PH, Wood PHN, eds. Population Studies of the Rheumatic Disease. International Congress, Series 148. Excerpta Medica Foundation: Amsterdam, 1968. ![]()
27. Rudwaleit, M, Jurik, AG, Hermann, KG, et al, Defining active sacroiliitis on magnetic resonance imaging (MRI) for classification of axial spondyloarthritis: a consensual approach by the ASAS/OMERACT MRI group. Ann Rheum Dis 2009; 68:1520–1527. ![]()
28. Brewerton, DA, Caffrey, M, Hart, FD, Ankylosing spondylitis and HL-A 27. Lancet 1973; 1:994. ![]()
29. Schlosstein, L, Trasaki, PI, Bruestone, R, et al, High association of an HL-A antigen W27, with ankylosing spondylitis. N Engl J Med 1973; 288:704. ![]()
30. Calin, A, HLA-B27 in 1982. Reappraisal of a clinical test. Ann Intern Med 1982; 96:114. ![]()
31. Marks, SH, Barnett, M, Calin, A, Ankylosing spondylitis in women and men: a case-controlled study. J Rheumatol 1983; 10:624–628. ![]()
32. Calin, A, Elswood, J. Ankylosing spondylitis (AS) – a nationwide analytical review: entry variables determining surgical intervention and outcome. Br J Rheumatol. 1987; 26(suppl):53.
33. Braun, J, Davis, J, Dougados, M, et al, First update of the international ASAS consensus statement for the use of anti-TNF agents in patients with ankylosing spondylitis. Ann Rheum Dis 2006; 65:316–320. ![]()
34. Brandt, J, Khariouzov, A, Listing, J, et al, Six-month results of a double-blind, placebo-controlled trial of etanercept treatment in patients with active ankylosing spondylitis. Arthritis Rheum 2003; 48:1667–1675. ![]()
35. van der Heijde, D, Dijkmans, B, Geusens, P, et al, Efficacy and safety of infliximab in patients with ankylosing spondylitis: results of a randomized, placebo-controlled trial (ASSERT). Arthritis Rheum 2005; 52:582–591. ![]()
36. Barraclough, D, Russel, AS, Percy, JS, Psoriatic spondylitis: a clinical, radiological and scintigraphic survey. J Rheumatol 1977; 4:282–287. ![]()
37. Moller, P, Vinje, O, Arthropathy and sacroiliitis in severe psoriasis. Scand J Rheumatol 1980; 9:113–117. ![]()
38. McEwen, C, Di Tata, D, Lincc, C, et al, Ankylosing spondylitis and spondylitis accompanying ulcerative colitis, regional enteritis, psoriasis and Reiter’s disease: a comparative study. Arthritis Rheum 1971; 14:291. ![]()
39. Russel, AS, Davis, P, Percy, JS, et al, The sacroiliitis of acute Reiter’s syndrome. J Rheumatol 1977; 4:293–296. ![]()
40. Haug, M, Ovesen, J, Psoas abscess in pyogenic sacroiliitis. J Ugeskr Laeger. 1999;161(8):1123–1124. ![]()
41. Gutierrez Macias, A, Barreiro Garcia, G, Ribacoba Bajo, L, et al, Pyogenic sacroiliitis. Presentation of 10 cases. C Rev Clin Esp. 1993;193(5):235–238. ![]()
42. Moyer, RA, Bross, JE, Harrington, TM, Pyogenic sacroiliitis in a rural population. J Rheumatol. 1990;17(10):1364–1368. ![]()
43. Cohn, SM, Schouetz, DJ, Pyogenic sacro-iliitis: another imitator of the acute abdomen. Surgery 1989; 100:95. ![]()
44. Melis, K, Roland, J, Appel, B, et al. Pyogene sacro-iliitis bij kinderen. Tijdschr Genees. 1994; 50:14–15.
45. Lenfant, J, Journeau, P, Touzet, P, et al, Pyogenic sacroiliitis in children. Apropos of 11 cases. Rev Chir Orthop Reparatrice Appar Mot. 1997;83(2):139–147. ![]()
46. Haliloglu, M, Kleiman, MB, Siddiqui, AR, et al, Osteomyelitis and pyogenic infection of the sacroiliac joint. MRI findings and review. Pediatr Radiol. 1994;24(5):333–335. ![]()
47. Bittini, A, Dominguez, PL, Martinez, P, et al, Comparison of bone and gallium-67 imaging in heroin user’s arthritis. J Nucl Med 1985; 26:1377–1381. ![]()
48. Malawista, SE, Seegmiller, JE, Hathaway, BE, et al, Sacroiliac gout. JAMA 1965; 194:106–108. ![]()
49. Alarcon-Segovia, D, Cetina, JA, Diaz-Jouanen, E, Sacro-iliac joints in primary gout. Am J Roentgenol 1973; 118:438–443. ![]()
50. Lipson, RL, Slocumb, CH, The progressive nature of gout with inadequate therapy. Arthritis Rheum 1965; 8:80–81. ![]()
51. Cohen, AS, McNeil, JM, Calkins, E, et al, The ‘normal’ sacroiliac joint: analysis of 88 sacroiliac joints. Am J Roentgenol 1967; 100:559–563. ![]()
52. Goldthwait, JE, Osgood, RB. A consideration of the pelvic articulations from an anatomical, pathological and clinical stand-point. Boston Med Surg J. 1905; 152:593–601.
53. Bernard, TN, Jr., Kirkaldy-Willis, WH, Recognizing specific characteristics of nonspecific low back pain. Clin Orthop 1987; 217:266–280. ![]()
54. Macnab, I. Backache. Baltimore: Williams & Wilkins; 1983.
55. Maigne, J-Y, Aivalikis, A, Pfefer, F, Results of sacroiliac joint double block and the value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine. 1996;21(16):1889–1892. ![]()
56. Broadhurst, NA, Bond, MJ, Pain provocation tests for the assessment of sacroiliac joint dysfunction. J Spinal Disord. 1998;11(4):341–345. ![]()
57. Laslett, M, Young, SB, Aprill, CN, McDonald, B, Diagnosing painful sacroiliac joints: A validity study of a McKenzie evaluation and sacroiliac provocation tests. Aust J Physiother. 2003;49(2):89–97. ![]()
58. Slipman, CW, Whyte, WS, Chow, DW, Sacroiliac joint syndrome. Pain Physician 2001; 4:143–152. ![]()
59. Wurff van der, P, Buijs, EJ, Groen, GJ, Intensity mapping of pain referral areas in sacroiliac joint pain patients. J Manipulative Physiol Ther 2006; 29:190–195. ![]()
60. Troisier, O. Sémiologie et traitement des algies discales et ligamentaires du rachis. Paris: Masson; 1973.
61. Buijs, E, Visser, L, Groen, G, Sciatica and the sacroiliac joint: a forgotten concept. Br J Anaesth. 2007;99(5):713–716. ![]()
62. Laslett, M, Aprill, CN, McDonald, B, Young, SB, Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005;10(3):207–218. ![]()
63. Vleeming A. The sacroiliac joint. A clinical, biomechanical and radiological study (dissertation). Rotterdam Erasmus University, 1990.
64. Vleeming, A, Stoeckaert, R, Volkers, ACW, Snijders, CJ, Relation between form and function in the sacroiliac joint. Part 1: Clinical anatomical aspects. Spine 1990; 15:130–132. ![]()
65. Vleeming, A, Stoeckaert, R, Volkers, ACW, Snijders, CJ, Relation between form and function in the sacroiliac joint. Part 2: Biomechanical aspects. Spine 1990; 15:130–132. ![]()
66. Pool-Goudzwaard, AL, Vleeming, A, Stoeckaert, R, et al, Insufficient lumbopelvic stability: a clinical, anatomical and biomechanical approach to ‘a specific’ low back pain. Manual Therapy. 1998;3(1):12–20. ![]()
67. Mens, JMA, Vleeming, A, Snijders, CJ, et al, Active straight leg raising. A clinical approach to the load transfer function of the pelvic girdle Rotterdam ECOVleeming A, ed. Second Interdisciplinary World Congress on Low Back Pain and its Relation to the Sacro-iliac Joint, 1995:207–220.
68. Barbor, R, Sclerosant therapy. Orthopaedic Medicine. 8th ed. Cyriax, JH, eds. Orthopaedic Medicine; vol II. Baillière Tindall, London, 1974.
69. York, JE, Kaczaraj, A, Abi-Said, D, et al, Sacral chordoma: 40-year experience at a major cancer center. Neurosurgery. 1999;44(1):74–79. ![]()
70. Cheng, EY, Ozerdemoglu, RA, Transfeldt, EE, et al, Lumbosacral chordoma. Prognostic factors and treatment. Spine. 1999;24(16):1639–1645. ![]()
71. West, SG, Troutner, JL, Baker, MR, et al, Sacral insufficiency fractures in rheumatoid arthritis. Spine. 1994;19(18):2117–2121. ![]()
72. Mumber, MP, Greven, KM, Haygood, TM, Pelvic insufficiency fractures associated with radiation atrophy: clinical recognition and diagnostic evaluation. Skeletal Radiol 1997; 26:94–99. ![]()