114 Disorders of the Pancreas
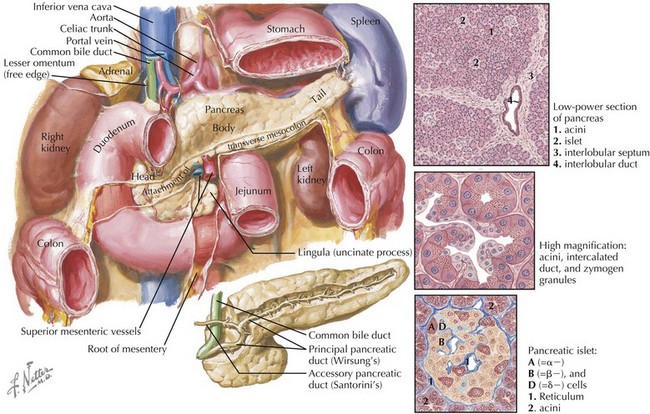
Disorders of the pancreas (Figure 114-1) are rare in childhood but can be associated with significant morbidity and mortality. Pancreatitis occurs less frequently in children than in adults and can be either acute or chronic in nature. It can be complicated by shock, hypocalcemia, pseudocyst formation, or necrosis, but these complications are rare. Pancreatic insufficiency (PI), defined as insufficient lipase secretion resulting in fat malabsorption, affects about 80% to 90% of patients with cystic fibrosis (CF). Congenital anomalies of the pancreas, such as pancreas divisum and annular pancreas, are found in approximately 10% of the general population and are generally asymptomatic but can be associated with pancreatitis (pancreas divisum) or duodenal obstruction (annular pancreas).
Etiology and Pathogenesis
Pancreatitis
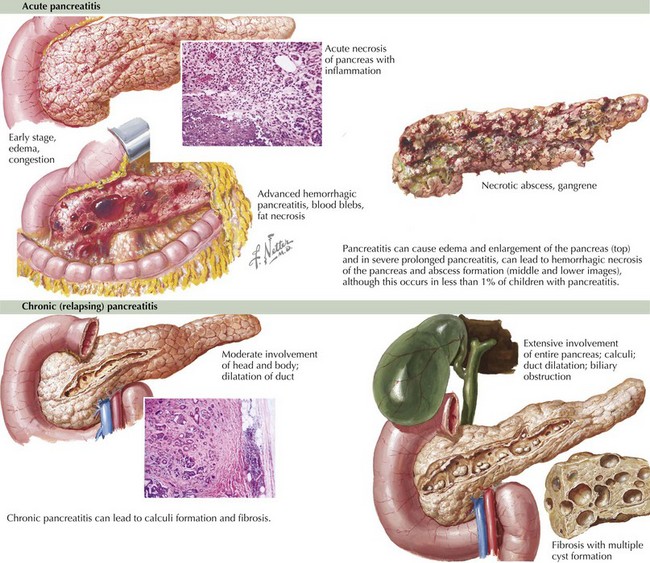
Pancreatitis occurs when intracellular trypsinogen and other digestive enzymes are activated, leading to damage of the pancreatic acinar cells. This damage leads to pancreatic edema (Figure 114-2), a local inflammatory response, and the initiation of autodigestion of the pancreas. These pancreatic secretions may form a collection that becomes walled off by granulation tissue to form a pseudocyst.
Chronic pancreatitis occurs with recurrent episodes of acute pancreatitis, leading to chronic inflammation as well as end-stage fibrosis (see Figure 114-2). The most common causes of chronic pancreatitis in children are CF, hereditary pancreatitis including mutations in the SPINK1, CFTR, and PRSS1 genes, and idiopathic causes.
Cystic Fibrosis
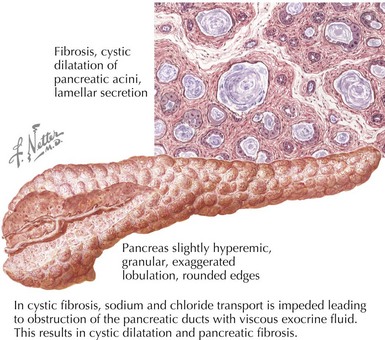
Pancreatic insufficiency in patients with CF is caused by dysfunction of the CFTR gene (Figure 114-3). This leads to impaired transport of sodium and chloride and subsequent obstruction of the pancreatic ducts with viscous exocrine fluid. These patients have diminished secretion of amylase, lipase, colipase, and phospholipases, as well as a decreased concentration of bicarbonate in their pancreatic secretions.
Congenital and Inherited Anomalies
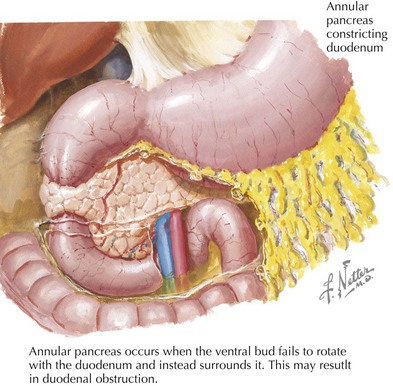
Congenital anomalies of the pancreas arise during fetal development. The pancreas forms from fusion of dorsal and ventral buds, which develop from the embryonic foregut. The ventral process rotates at about the eighth week of gestation and settles posterior and inferior to the dorsal portion of the pancreas. Pancreas divisum is the most common pancreatic anomaly and occurs when the dorsal and ventral portions fail to fuse. Annular pancreas occurs when the ventral bud fails to rotate with the duodenum and instead surrounds it (Figure 114-4).
Clinical Presentation
Evaluation and Management
Pancreatitis
A thorough history is important to distinguish pancreatitis from other causes of acute abdominal pain. It is important to determine the onset and the character of the pain, as well as any other associated symptoms. A complete list of current medications is important to obtain because many medications may cause pancreatitis, including nonsteroidal antiinflammatory drugs, corticosteroids, antibiotics (sulfonamides, tetracyclines), diuretics (thiazides, furosemide), azathioprine, and mercaptopurine, to name a few. The laboratory evaluation should include amylase and lipase levels, which may be elevated more than three times the upper limit of normal but can be unreliable because they may be elevated for reasons other than pancreatitis (Table 114-1). An ultrasound may reveal an enlarged pancreas with an alteration in echogenicity and can also identify the presence of a pseudocyst. Other findings on ultrasound may include gallstones or biliary sludge in the case of gallstone pancreatitis, pancreatic calcifications, choledochal cysts, dilated pancreatic ducts, or dilated common or hepatic bile ducts. Magnetic resonance cholangiopancreatography can be helpful in further identifying ductal abnormalities. In patients with recurrent or chronic pancreatitis, genetic testing for SPINK1, CF, and cationic trypsinogen (PRSS1) can be helpful. Additionally, an elevated triglyceride level may indicate hyperlipidemia as a cause of recurrent pancreatitis.
| Amylase | Lipase |
|---|---|
ERCP, endoscopic retrograde cholangiopancreatography.
De Matos V, Mascarenhas M. Cystic fibrosis. In: Liacouras C, Piccoli D, editors. Pediatric Gastroenterology: The Requisites in Pediatrics. St. Louis: Mosby Elsevier; 2008:315-316.
Gelrud D, Gress F. Approach to the patient with elevated serum amylase or lipase. www.uptodate.com/contents/approach-to-the-patient-with-elevated-serum-amylase-or-lipase.
Lowe ME, Greer JB. Pancreatitis in children and adolescents. Curr Gastroenterol Rep. 2008;10(2):128-135.
Nousia-Arvanitakis S. Cystic fibrosis and the pancreas: recent scientific advances. J Clin Gastroenterol. 1999;29(2):138-142.
Sreedharan R, Mamula P. Congenital anomalies. In: Liacouras C, Piccoli D, editors. Pediatric Gastroenterology: The Requisites in Pediatrics. St. Louis: Mosby Elsevier; 2008:307-313.
Verma R, Wong T. Pancreatitis. In: Liacouras C, Piccoli D, editors. Pediatric Gastroenterology: The Requisites in Pediatrics. St. Louis: Mosby Elsevier; 2008:322-328.
Zyromski NJ, Sandoval JA, Pitt HA, et al. Annular pancreas: dramatic differences between children and adults. J Am Coll Surg. 2008;206(5):1025-1027.