Disorders of the neuromuscular junction
Disorders of the neuromuscular junction (NMJ) are uncommon. The most common is myasthenia gravis (MG), with an annual incidence of 1 per 100 000 and a prevalence of 8–15 per 100 000. There is a bimodal age of onset, affecting young adults, especially females aged 15–30 years, and predominantly males aged 50–70 years. It is important to diagnose MG as it is a dangerous illness that is very amenable to treatment. Other rare disorders of the NMJ are shown in Table 1.
Table 1 Other rare disorders of the neuromuscular junction
| Disorder | Mode of action | Comments |
|---|---|---|
| Neonatal MG (born to mothers with MG) | Autoimmune, as MG | Hypotonia starts by third day and persists until antibodies leave the baby’s system, 2–12 weeks, may have skeletal deformities |
| Congenital myasthenia | Non-autoimmune | MG-type eye and facial weakness, responds poorly to treatment |
| Botulism (canned food is the usual source) | Botulinum toxin blocks acetylcholine release | Typically acute onset with muscarinic features, e.g. tachycardia and pupil dilatation, as well as weakness Recently been seen in IV drug users |
| Acute organophosphate (insecticide) poisoning | Irreversible inhibition of cholinesterase | Presents with cholinergic crisis and confusion. Treatment: atropine for muscarinic effects, ventilatory support, pralidoxime ‘releases’ cholinesterase |
| Pseudocholinesterase deficiency | Unable to break down suxamethonium | Prolonged postoperative paralysis due to persisting NMJ block, supportive therapy only required |
| Snake venom | Alpha-bungarotoxin binds acetylcholine receptor | Long-lasting weakness as binding is irreversible |
MG, myasthenia gravis; NMJ, neuromuscular junction
Myasthenia gravis
Pathophysiology
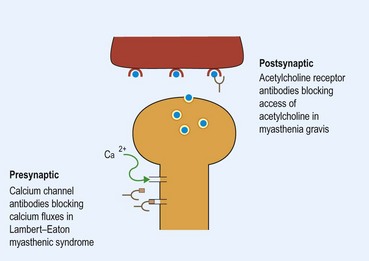
MG is an organ-specific autoimmune disease, with antibodies directed against the acetylcholine receptor. These antibodies compete with acetylcholine released by the nerve terminal, interfering with neuromuscular transmission (Fig. 1). Thymic hyperplasia occurs in 65% of patients, most commonly in young adults. Thymic tumours occur in 15% of patients, usually older men, and 25% of these tumours are malignant, with local invasion; the tumours need treatment in their own right. Antibodies to striated muscle are found in nearly 50% of later-onset patients and 84% of those with thymic tumours. The thymus appears to be important in the pathogenesis of the disease, but its exact role is unclear. Rarely, MG may be due to the drug penicillamine.
Symptoms and signs
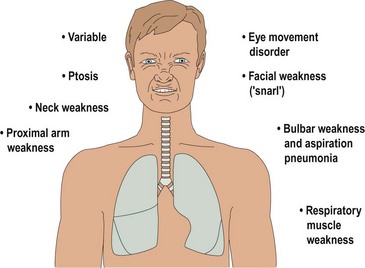
The cardinal symptom of MG is variable muscle weakness (Fig. 2). Usually it is possible to elicit a history of fatiguability; the more a muscle is used, the weaker it becomes. The distribution of muscle weakness is different from most other conditions: eye movements, eyelids, facial, neck, bulbar and proximal arm muscles, with relative sparing of the lower limbs. Respiratory muscles are commonly affected. Fifty per cent of patients present with ptosis or diplopia and these muscles are affected eventually in over 90%. Typically, diplopia and ptosis develop through the day but have gone the next morning after a night’s rest.
In MG, muscle appearance, tone, reflexes and sensation are normal. In mild cases, power may be normal until the muscles are fatigued (Box 1). More commonly, there is clear weakness. Typically the defective eye movements of myasthenia do not correspond to any single nerve lesion but MG may mimic any pattern of deficit, including internuclear ophthalmoplegia.
Differential diagnosis
Investigations
Investigations are directed at confirming the diagnosis and identifying associated thymus disease.
The tests should only be done where there are resuscitation facilities available. Predosing with atropine reduces the complications. A CT or MRI scan of the thorax can be used for thymoma or thymic hyperplasia.
Lambert–Eaton myasthenic syndrome (LEMS)
This rare disorder usually affects men. It occurs alone or in association with carcinoma of lung, breast, prostate, stomach or lymphoma. LEMS is due to antibodies to presynaptic voltage-gated calcium channels, which lead to reduced release of acetylcholine from the presynaptic terminal (see Fig. 1). There is often a mild coexisting neuropathy.