Chapter 656 Disorders of the Mucous Membranes
Cheilitis
Inflammation of the lips (cheilitis) and angles of the mouth (angular cheilitis or perlèche) (Fig. 656-1) are most commonly due to dryness, chapping, and lip licking. Excessive salivation and drooling, particularly in children with neurologic deficits, may also cause chronic irritation. Lesions of oral thrush may occasionally extend to the angles of the mouth. Protection can be provided by frequent applications of a bland ointment such as petrolatum. Candidosis should be treated with an appropriate antifungal agent, and contact dermatitis of the perioral skin should be treated with a low-potency topical corticosteroid ointment preparation and frequent use of petrolatum or a similar emollient.
Mucocele
Mucus retention cysts are painless, fluctuant, tense, 2- to 10-mm, bluish papules on the lips (Fig. 656-2), tongue, palate, or buccal mucosa. Traumatic severance of the duct of a minor salivary gland leads to submucosal retention of mucus secretion. Those on the floor of the mouth are known as ranulas when the submaxillary or sublingual salivary ducts are involved. Fluctuations in size are usual, and the lesions may disappear temporarily after traumatic rupture. Recurrence is prevented by excision of the mucocele.
Aphthous Stomatitis (Canker Sores)
Aphthous stomatitis consists of solitary or multiple painful ulcerations occur on the labial (Fig. 656-3), buccal, or lingual mucosa and on the sublingual, palatal, or gingival mucosa (Chapter 307). Lesions may manifest initially as erythematous, indurated papules that erode rapidly to form sharply circumscribed, necrotic ulcers with a gray fibrinous exudate and an erythematous halo. Minor aphthous ulcers are 2-10 mm in diameter and heal spontaneously in 7-10 days. Major aphthous ulcers are >10 mm in diameter and take 10-30 days to heal. A third type of aphthous ulceration is herpetiform in appearance, manifesting as a few to numerous grouped 1- to 2-mm lesions that tend to coalesce into plaques that heal over 7-10 days. Approximately 30% of patients with recurrent lesions have a family history of the disorder (Chapter 307 for differential diagnosis).
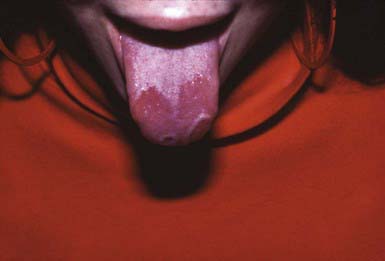
Geographic Tongue (Benign Migratory Glossitis)
Geographic tongue consists of single or multiple sharply demarcated, irregular, smooth red plaques on the dorsum of the tongue caused by transient atrophy of the filiform papillae and the surface epithelium, often with elevated gray margins composed of intervening filiform papillae that are increased in thickness (Fig. 656-4). Symptoms of mild burning or irritation may occasionally be bothersome. Onset is rapid, and the pattern may change over hours to days. Some patients feel that the condition is exacerbated by stress or by hot or spicy foods. The histology of geographic tongue is similar to that of pustular psoriasis. No therapy other than reassurance is necessary.
Acute Necrotizing Ulcerative Gingivitis (Vincent Stomatitis, Fusospirochetal Gingivitis, Trench Mouth)
Noma
Noma is a severe form of fusospirillary gangrenous stomatitis that occurs primarily in malnourished children 2-5 yr of age who have had a preceding illness such as measles, scarlet fever, tuberculosis, malignancy, or immunodeficiency. It manifests as a painful, red, indurated papule on the alveolar margin, followed by ulceration and mutilating gangrenous destruction of tissue in the oronasal region. The process may also involve the scalp, neck, shoulders, perineum, and vulva. Noma neonatorum manifests in the first month of life as gangrenous lesions of the lips, nose, mouth, and anal regions. Affected infants are usually small for gestational age, malnourished, premature, and frequently ill, particularly with Pseudomonas aeruginosa sepsis. Care consists of nutritional support, conservative debridement of necrotic soft tissues, empirical broad-spectrum antibiotics such as penicillin and metronidazole, and, in the case of noma neonatorum, antipseudomonal antibiotics (Chapter 43).
Altenburg A, Zouboulis CC. Current concepts in the treatment of recurrent aphthous stomatitis. Skin Therapy Lett. 2008;13:1-4.
Bischoff EWMA, Uijen A, van der Wel M. Aphthous ulcers. BMJ. 2009;339:345-346.
Gonsalves WC, Chi AC, Neville BW. Common oral lesions: part 1. Superficial mucosal lesions. Am Fam Physician. 2007;75:501-507.
Nico MM, Park JH, Lourenco SV. Mucocoele in pediatric patients. Pediatr Dermatol. 2008;25:308-311.
Piperi E, Omile J, Pambuccian S, et al. Oral hairy leukoplakia in HIV-negative patients: report of 10 cases. Int J Surg Pathol. 2008. epub doi:10.1177/1066896908327865