Disorders of the midtarsal joints
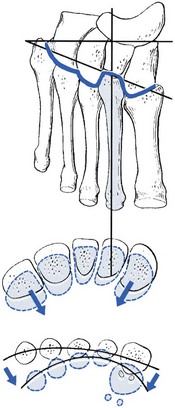
At the distal (Lisfranc’s) joint, considerable rotation round the second metatarsal shaft is possible (Fig. 59.1). Because of the specific structure of the joint line, plantiflexion of the metatarsals will always be accompanied by a movement towards the second metatarsal. Therefore a plantiflexion movement at the midtarsal joint increases the curvature of the anterior arch, whereas dorsiflexion is associated with flattening.
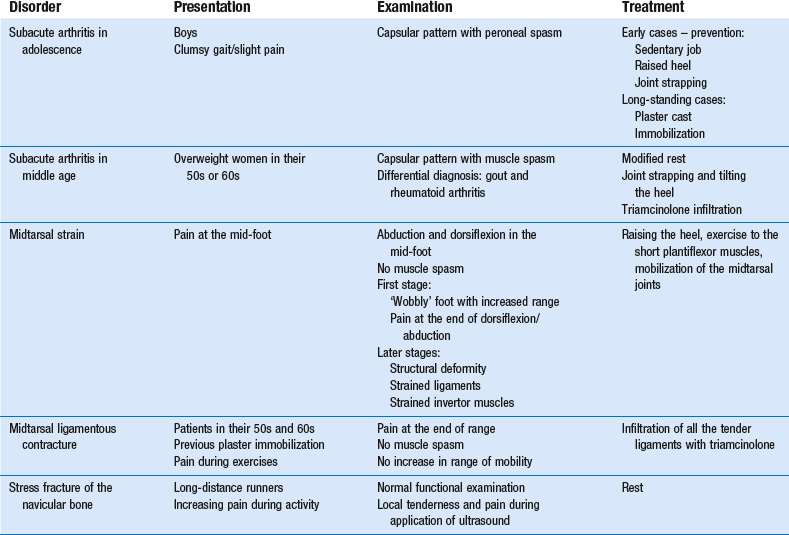
Capsular pattern
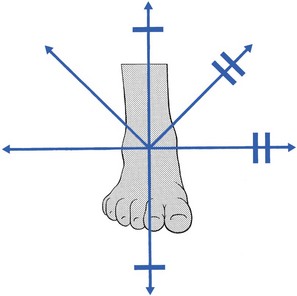
The capsular pattern at the midtarsal joints is increasing limitation of adduction, supination, plantiflexion and dorsiflexion (Fig. 59.2). The mid-foot finally fixes in an abducted and pronated position because of a spasm of the peroneal muscles.
Subacute arthritis in adolescence
Subacute arthritis in middle age
Non-capsular pattern
Midtarsal strain
If an excessive strain is imposed on the midtarsal joints – for example, as the result of a deformity (e.g. plantaris) – the power of the musculature (tibialis posterior and flexor hallucis longus) becomes insufficient to maintain the longitudinal arches during weight bearing.2 After some time, the midtarsal ligaments become stretched, elongate and undergo inflammatory changes, so that pain results. Elongation promotes excessive movements at the midtarsal joints, which cause the plantar arch to flatten during weight bearing. As a result, the forefoot dorsiflexes and abducts, which causes the inner side of the foot to become prominent and further overstretches the calcaneonavicular ligament. In due course, the excessive motion of the joints and their poor alignment leads to inflammation of the capsule and to structural damage of the articular surfaces, which finally results in structural deformity and arthrosis.
Mechanism
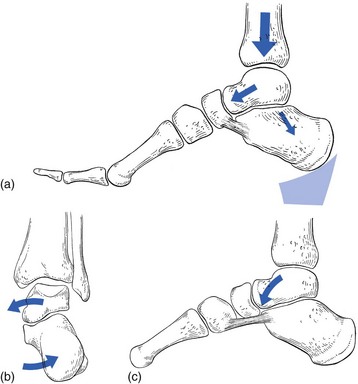
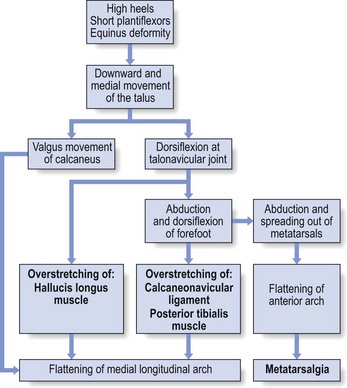
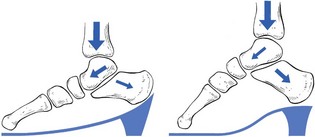
Initially, the body weight bears on the talus via a downward thrust through the tibia. The talus is supported by the calcaneus, on which it lies obliquely. The former therefore has a tendency to glide in a medial and forward direction, especially in patients with an equinus deformity at the ankle or in patients with too short plantiflexor muscles. In women who wear high, oblique heels, the talus also tends to be pushed forwards on the calcaneus (Fig. 59.3a).
The forward and medial gliding of the talus imposes medial and downward pressure on the anteromedial calcaneal border. The medial pressure forces the calcaneus towards valgus, which may be furthered by a shortening of the Achilles tendon (Fig. 59.3b). The downward pressure of the talus evokes dorsiflexion at the talonavicular joint.3 This increases the depression of the longitudinal arch and can be responsible for greater stress on the plantar ligaments and the fascia plantaris (Fig. 59.3c). The downward pressure of the talus and the consequent dorsiflexion at the talonavicular joint will initiate a number of other events, which are the source of more deformity and trouble:
• Because of the obliquity of the joint surfaces, each dorsiflexion in the midtarsal joints is accompanied by some abduction. The downward movement of the talus is thus at the origin of an abduction deformity in the mid-foot. This dorsiflexed and abducted foot overstretches the inner ligaments (calcaneonavicular ligament and capsule of the talonavicular joint).
• Dorsiflexion at the midtarsal joint also causes spreading out and abduction of the metatarsals. Abduction is the result of obliquity of the joint line. Spreading out is caused by the specific cone-shaped form of the bases of the metatarsals, which move their heads away from the centre during extension (see online chapter Applied anatomy of the lower leg, ankle and foot). This flattens the anterior arch and results in a splay foot.
• Valgus of the calcaneus with possible shortening of the Achilles tendon
• Dorsiflexion and abduction of the mid-foot, with flattening of the longitudinal arch and tension in the plantar and medial ligaments
• Flattening and abduction of the forefoot, with spreading of the metatarsal heads and loss of the anterior arch
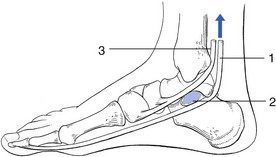
• In due course, there will also be some effect on the tendons: that of the tibialis posterior, the first invertor of the foot, suffers strain and becomes inflamed. The tendon of the flexor hallucis longus, which is not only an invertor, but also, through its position under the sustentaculum tali, has a specific function as a stabilizer of the anterior part of the calcaneus, also becomes strained (Fig. 59.4).
The mechanism of midtarsal strain is summarized in Fig. 59.5.
Clinical examination
As midtarsal strain advances, three clinical grades can be distinguished.
Treatment
Heel raising
The heel must be raised horizontally (Fig. 59.6) so as to allow the forefoot to adopt a more plantigrade position in relation to the talus when weight is borne. A slight medial wedge can be added to correct the valgus position of the heel. Attempts should be made to stretch the triceps muscle if there is shortening.
Exercises for the invertors
Exercises for the invertors should also be given; strengthening them protects the foot against further pronation–abduction. A strong and functional flexor hallucis longus muscle plays a role in ‘propping’ the talus upwards by lifting the sustentaculum tali (see Fig. 59.4). The posterior tibial muscle, the key dynamic support of the medial longitudinal arch of the foot, should also be strengthened.5
Mobilization of the joints
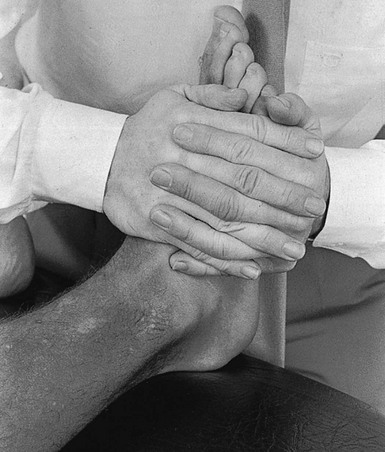
The patient lies in a supine position on a high couch. The manipulator sits facing the patient’s foot. As great strength is required and the manipulator has to work without leverage, a good starting position is vital. The heel of the ipsilateral hand is placed at the dorsum of the first metatarsal bone, and the heel of the contralateral hand is placed at the plantar aspect of the fourth and fifth metatarsal bones. Both hands are clasped about the outer and dorsal aspect of the forefoot. The foot is pressed slightly towards dorsiflexion (Fig. 59.7). Rotation is now imparted to the forefoot by a swinging movement in the shoulders and elbows, which causes the upper hand on the inner side to press towards the manipulator and the outer hand to press away from him. This movement is repeated in a rhythmic manner for a few minutes.
Steroid infiltration
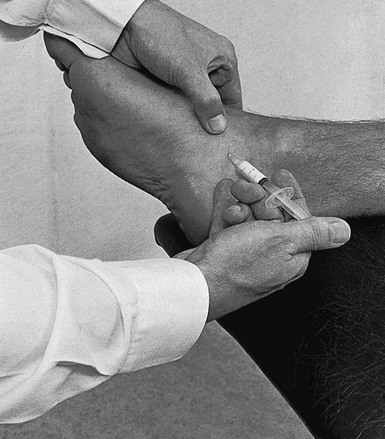
The palpating thumb remains on the tender ligament and the needle is introduced between the thumb and bone (Fig. 59.8). The point of the needle is then aimed towards the calcaneal border of the ligament, where 1 mL is injected. Another 1 mL is then infiltrated at the navicular insertion of the ligament.
Deep friction
If the flexor hallucis longus or the tibialis posterior tendons are at fault, deep friction is indicated (see Ch. 57).
Surgery
If conservative management fails, the painful midtarsal joints are best stabilized by arthrodesis. In the past, triple arthrodesis was used extensively6; nowadays, more limited single-joint fusions are used which allow more preservation of the hindfoot motion, resulting in better function.7–10
Conservative treatment of midtarsal strain is summarized in Box 59.1.
Aseptic necrosis
Osteochondritis dissecans at the navicular bone appears in boys aged between 4 and 12 years and is known as Köhler’s disease I. There is pain and limitation of the midtarsal movements. The diagnosis is made from a radiograph or a bone scan.11
The course of the disease process is benign and self-limiting.12,13 Treatment is symptomatic and consists of weight-bearing plaster casts over 3 months.14 With or without treatment, there is spontaneous reconstitution of the navicular bone and excellent recovery of function after an average duration of 15 months.15,16
Navicular stress fracture
Navicular stress fractures account for about 15% of all stress fractures.17 They typically occur in running and jumping athletes, in whom repetitive cyclic loading results in fatigue failure of the navicular bone, the cornerstone of the medial arch. Biomechanical analysis of navicular motion during stride18 reveals that most of the impingement force is focused at the central third of the navicular bone, which is also an area of relative avascularity.19 This explains why the characteristic fracture is located in the central third of the bone.
On examination, neither swelling nor discoloration is visible. Rising on tiptoe may be painful, as is the passive plantiflexion–dorsiflexion movement at the midtarsal joints. Clinical suspicion is raised when tenderness is elicited over the ‘N spot’, a nickel-sized area at the central region of the proximal dorsal navicular bone.20 Tenderness is strongly associated with navicular stress fractures.21
Early diagnosis can be made by ultrasound, which is a good screening test for stress fractures.22 Computed tomography (CT) is the best tool in the diagnosis of navicular stress fracture. It allows differentiation between stress fracture and stress reaction, and enables accurate fracture definition.23
Non-displaced fractures respond well to 6 weeks of non-weight-bearing cast immobilization. Displacement, comminution and delayed or non-union fractures are indications for surgical open reduction and internal fixation.24,25
Cuboid rotation
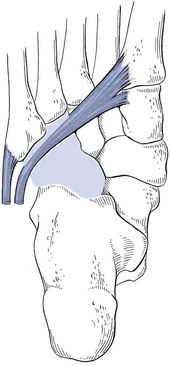
Subluxation of the cuboid bone occurs when a strong pull exerted by the tendon of the peroneus longus muscle causes rotation of the bone26 (Fig. 59.9). The lateral side of the cuboid is tilted upwards and the medial side becomes depressed. The cuboid is locked in this subluxated position and pain results. Newell and Woodle27 found this condition in some 4% of athletes complaining of pain in the midtarsal region. The condition seems to be more common in patients who have pronated feet.
The diagnosis is primarily subjective, and must be made on the basis of the patient’s history and physical findings. The patient, most often a long-distance runner or dancer, complains of lateral mid-foot pain during and after activity. Inspection may reveal a subtle forefoot valgus, a shallow depression on the dorsal surface of the foot and a palpable fullness on the plantar aspect of the cuboid. Clinical examination usually shows end-range pain during midtarsal movements and/or some limitation of dorsiflexion–plantiflexion. In addition, pressing on the plantar surface of the cuboid in a dorsal direction produces pain.28,29
Documentation by radiograph, CT scan or MRI is difficult. Treatment is manipulation (the ‘cuboid whip’).30
The patient stands with the back to the manipulator and holds on to a couch or a chair. The knee is flexed at a right angle. The physician grasps the foot with both hands so that the fingers are placed at the dorsum of the forefoot and the crossed thumbs over the plantar aspect of the cuboid (Fig. 59.10). The manipulation is now performed as a quick upward ‘whiplash’, while the thumbs, at the plantar aspect, apply strong downward pressure. The manipulator’s elbows should be close together and the arms, wrists and hands should be fully relaxed.
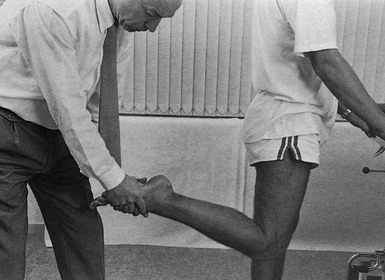
Fig 59.10 Manipulation for cuboid rotation.
Lesions of the cuneiform–first metatarsal joint
The disorders that occur at this joint are:
Osteoarthrosis
This condition usually results from previous osteochondritis (Cyriax1: p. 439). There is a similarity to hallux rigidus, also known to be the result of osteochondritis.33
Treatment
It is important to note that gross osteoarthrosis of the cuneiform–first metatarsal joint may lead to fixation, with considerable plantaris deformation of the first metatarsal (fixation in plantiflexed position). This may, in turn, result in metatarsalgia of the first metatarsophalangeal joint or, more frequently, a lesion of the sesamoid–metatarsal joint. If this occurs, a support must be prescribed to take the weight off the head of the bone (see online chapter Disorders of the forefoot and toes).
Gout
It is not uncommon for gout to attack this joint, even before the metatarsophalangeal joint of the big toe.34 If there is sudden pain, warmth, reddening of the skin, pain at night and extreme tenderness of the joint, gout should be considered.
References
1. Cyriax, JH. Textbook of Orthopaedic Medicine, vol 1, Diagnosis of Soft Tissue Lesions, 8th ed. London: Baillière Tindall; 1982.
2. Wiewiorski, M, Valderrabano, V, Painful flatfoot deformity. Acta Chir Orthop Traumatol Cech. 2011;78(1):20–26. ![]()
3. Astion, DJ, Deland, JT, Otis, JC, Kenneally, S, Motion of the hindfoot after simulated arthrodesis. J Bone Joint Surg. 1997;79A(2):241–246. ![]()
4. Greisberg, J, Hansen, ST, Jr., Sangeorzan, B, Deformity and degeneration in the hindfoot and mid-foot joints of the adult acquired flatfoot. Foot Ankle Int. 2003;24(7):530–534. ![]()
5. Karges, DE, Current concepts for treatment of the painful flatfoot in the elderly. Mo Med. 2005;102(3):236–239. ![]()
6. Schramm, CA, Hein, SC, Cooper, PS, Triple arthrodesis. AORN J. 1996;64(1):31–52. ![]()
7. Donatto, KC, Arthritis and arthrodesis of the hindfoot. Clin Orthop 1998; 349:81–92. ![]()
8. Harper, MC, Talonavicular arthrodesis for the acquired flatfoot in the adult. Clin Orthop 1999; 365:65–68. ![]()
9. Harper, MC, Tisdel, CL, Talonavicular arthrodesis for the painful adult acquired flatfoot. Foot Ankle Int. 1996;17(11):658–661. ![]()
10. Zonno, AJ, Myerson, MS, Surgical correction of mid-foot arthritis with and without deformity. Foot Ankle Clin. 2011;16(1):35–47. ![]()
11. Bui-Mansfield, LT, Lenchik, L, Rogers, LF, et al, Osteochondritis dissecans of the tarsal navicular bone: imaging findings in four patients. J Comput Assist Tomogr. 2000;24(5):744–747. ![]()
12. Borges, JL, Guille, JT, Bowen, JR, Kohler’s bone disease of the tarsal navicular. J Pediatr Orthop. 1995;15(5):596–598. ![]()
13. Devine, KM, Van Demark, RE, Kohler’s osteochondrosis of the tarsal navicular: case report with twenty-eight year follow up. South Dakota. J Med. 1989;42(9):5–6. ![]()
14. Ippolito, E, Ricciardi Pollini, PT, Falez, F, Kohler’s disease of the tarsal navicular: long-term follow-up of 12 cases ’. J Pediatr Orthop. 1984;4(4):416–418. ![]()
15. Williams, GA, Cowell, HR, Kohler’s disease of the tarsal navicular. Clin Orthop 1981; 158:53–58. ![]()
16. Leeson, MC, Weiner, DS, Osteochondrosis of the tarsal cuneiforms. Clin Orthop 1985; 196:260–264. ![]()
17. Bennell, KL, Malcolm, SA, Thomas, SA, et al, The incidence and distribution of stress fractures in competitive track and field athletes. A twelve-month prospective study. Am J Sports Med 1996; 24:211–217. ![]()
18. Van Langelaan, EJ, A kinematical analysis of the tarsal joints. An x-ray photogrammetric study. Acta Orthop Scand Suppl 1983; 204:1–269. ![]()
19. Torg, JS, Pavlov, H, Cooley, LH, et al, Stress fractures of the tarsal navicular. J Bone Joint Surg 1982; 64:700–712. ![]()
20. Brukner, PD, Khan, KM. Clinical sports medicine. Sydney: McGraw-Hill; 2001.
21. Khan, KM, Fuller, PJ, Brukner, PD, et al, Outcome of conservative and surgical management of navicular stress fracture in athletes. Eighty-six cases proven with computerized tomography. Am J Sports Med 1992; 20:657–666. ![]()
22. Moss, A, Mowat, AG, Ultrasonic assessment of stress fractures. BMJ 1983; 286:1479–1480. ![]()
23. Kiss, ZS, Khan, KM, Fuller, PJ, Stress fractures of the tarsal navicular bone: CT findings in 55 cases. Am J Radiol 1993; 160:111–115. ![]()
24. Saxena, A, Fullem, B, Hannaford, D, Results of treatment of 22 navicular stress fractures and a new proposed radiographic classification system. J Foot Ankle Surg 2000; 39:96–103. ![]()
25. Potter, NJ, Brukner, PD, Makdissi, M, et al, Navicular stress fractures: outcomes of surgical and conservative management. Br J Sports Med. 2006;40(8):692–695. ![]()
26. Mooney, M, Maffey-Ward, L, Cuboid plantar and dorsal subluxation: assessment and treatment. JOSPT 1994; 20:220–226. ![]()
27. Newell, SG, Woodle, A. Cuboid syndrome. Phys Sportsmed. 1981; 9(4):71–76.
28. Marshall, P, Hamilton, WG, Cuboid subluxation in ballet dancers. Am J Sports Med. 1992;20(2):169–175. ![]()
29. Adams, E, Madden, C, Cuboid subluxation: a case study and review of the literature. Curr Sports Med Rep. 2009;8(6):300–307. ![]()
30. Jennings, J, Davies, GJ, Treatment of cuboid syndrome secondary to lateral ankle sprains: a case series. J Orthop Sports Phys Ther. 2005;35(7):409–415. ![]()
31. Taplin, GC. Foot technique. J Am Osteopath Assoc. 1928; 27:606–608.
32. Jones, LH, Foot treatment without hand trauma. J Am Osteopath Assoc 1973; 72:481–489. ![]()
33. Huskisson, EC, Hart, FD. Joint Disease: All the Arthropathies, 4th ed. Bristol: John Wright; 1987.
34. Dieppe, PA, Calvent, P. Crystals and Joint Disease. London: Chapman & Hall; 1983.