Disorders of the lower leg
Bone disorders
Children between the ages of 6 and 11 years who complain of diffuse pain in the legs but have a normal clinical examination are very often regarded as suffering from ‘growing pains’. Paediatricians’ estimates of the frequency of this diagnosis vary from 4%1 to 20%2 of all children. During recent decades, several hypotheses have been put forward but none gives a good explanation for the symptoms. As it occurs between the ages of 6 and 12, which is not the period of maximum rate of growth, ‘growing’ cannot be the real reason for the pain. Whatever the origin of the pain, it disappears spontaneously and completely after the age of 12 years.3,4
Lesions of the plantiflexors
Pain
Tennis leg
This is the common term to describe a tear in the triceps. It occurs most often in the medial belly of the gastrocnemius muscle, usually some 5 cm above the musculotendinous junction.5
The disorder was first described by Hood in 1884.6 For decades it has been regarded as a ruptured plantaris tendon,7,8 but careful clinical examination of patients suffering from this disorder shows this to be false.9
Examination reveals pain during resisted plantiflexion but no weakness. In the supine-lying position, dorsiflexion at the ankle is found to be markedly limited when the knee is in the extended position but becomes normal when the knee is flexed. This implicates the gastrocnemius muscle, part of which is in spasm around the tear. The difference in range between a flexed and an extended knee in a disorder of the gastrocnemius muscle is another example of the constant-length phenomenon. Palpation of the calf reveals the tender area in the medial gastrocnemius, with either swelling and haematoma if the lesion is recent, or induration around the tear if it is old. After a severe rupture, it is possible to palpate the gap in the medial gastrocnemius. Ultrasonography is the imaging technique of choice to demonstrate size and grade of the lesion.10,11
Differential diagnosis
Although the diagnosis is obvious, it is as well to bear in mind some other possibilities.
High rupture of the Achilles tendon
Although the similar onset and localization of the pain can cause diagnostic confusion, this condition should hardly be a problem if a proper clinical examination is done. Weak resisted plantiflexion and no spasm during passive dorsiflexion in a ruptured Achilles tendon contrast with the findings in tennis leg.12,13 If there is any doubt, a simple test can be done as follows.14 The patient lies prone, the foot hanging over the edge of the couch. The examiner squeezes the calf muscles. If the Achilles tendon is intact, the foot moves into plantar flexion. When there is total rupture, no movement results.
Deep venous thrombosis in the calf muscles
Differential diagnosis from this condition is very important. Instances have been described of patients with tennis leg receiving anticoagulants, which aggravated their condition.15 The main historical difference is in the onset. In deep venous thrombosis, pain appears after immobilization or after sitting for a couple of hours,16 and not during vigorous contraction of the calf muscles. Clinical examination does not show limited passive dorsiflexion, although passive dorsiflexion and resisted plantiflexion can be painful. The calf muscle and leg are swollen and the foot becomes oedematous because of obstruction to venous return. Palpation of the tender spot shows other differences: in thrombosis the whole calf muscle is painful to the touch and sometimes a painful ‘string’ can be palpated deep within it.17,18
Rupture of a Baker’s cyst
In long-standing rheumatoid arthritis of the knee, chronic distension with fluid can weaken the posterior ligaments and during exertion these can rupture. Sudden pain in the knee, followed by swelling of the leg and oedema of the ankle, strongly suggests venous thrombosis.19 Here, the long-standing rheumatoid arthritis and the absence of injury suggest the diagnosis, which can be confirmed by arthrography.
Posterior compartment syndrome
The patient, usually a young man, reports an ache and swelling in the calf some hours after unaccustomed exercise. Walking is uncomfortable and increases the swelling. Examination shows that rising on tiptoe is not difficult and not really uncomfortable. The calf is diffusely swollen and the skin is red and warm to the touch. Passive dorsiflexion of the foot is severely limited by loss of elasticity of the calf muscles. Palpation reveals uniform tenderness of the whole calf muscle without any localized tender area.20 The symptoms result from muscle ischaemia, produced by increased tissue fluid pressure in the closed fascial compartment. The difference from tennis leg lies in the discrepancy between marked restriction of passive dorsiflexion and almost painless tiptoe rising. Treatment is surgical division of the deep fascia.
Treatment
Different types of treatment have been advocated for tennis leg. Most authorities advise partial or total immobilization for small tears21 and surgical suture for serious ruptures.22,23
In our opinion, surgery for this condition is scarcely ever necessary and partial or total immobilization by plaster cast or strapping is obsolete. When such treatment is instituted, the formation of a chronic adherent scar is promoted, which results in disability lasting several months. The aim of treatment in muscle tears is to allow the torn fibres to heal in such a way that mobile and functional scar tissue is formed. If normal enlargement of the muscle is impaired by adhesions, self-perpetuating inflammation will be the result. Muscle belly lesions (tennis leg is an excellent example) therefore need a different and more functional approach. The aim must be to restore normal movement in the damaged muscle as quickly as possible. This can be achieved with combined treatment: early compression to decrease the amount of haemorrhage; aspiration and infiltration with local anaesthetic as soon as the patient is seen; and deep transverse friction and electrically stimulated or active contractions of the muscle during the next few days.24 During the recovery period, the muscle must be protected by a raised heel pad, which enables the patient to use the unaffected parts of the gastrocnemius without strain on the line of healing.
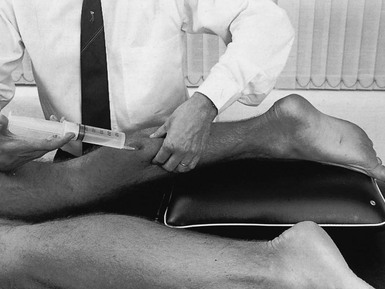
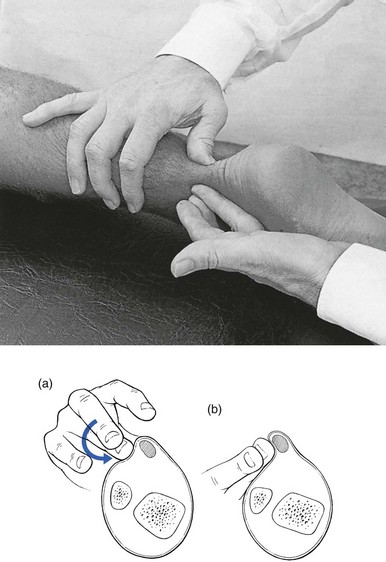
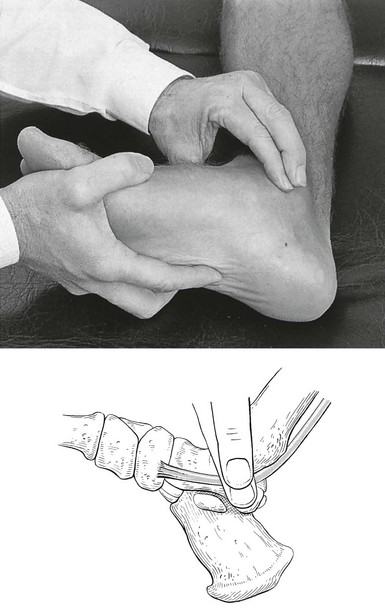
Technique: infiltration
As soon as the patient is seen – whether on the day of the accident or some weeks or months later – local anaesthesia is induced at the site of the partial rupture. The patient lies prone, the knee slightly bent and the foot plantiflexed, to allow maximal relaxation of the muscle. The tender spot is located and gripped between thumb and index finger (Fig. 57.1). If there is any fluctuation, an attempt is made to aspirate the haematoma. Once that has been done, 30–50 mL of procaine 0.5% is injected using the usual infiltration techniques. As the spot is never precisely localized (gentle pressure does not reveal tenderness in the deeper part of the muscle, whereas strong pressure is apt to hurt throughout the belly) and the gastrocnemius muscle is a large structure, up to 50 mL of a 0.5% solution may be required.
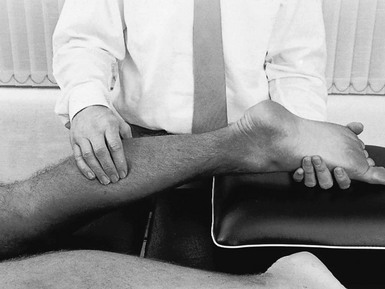
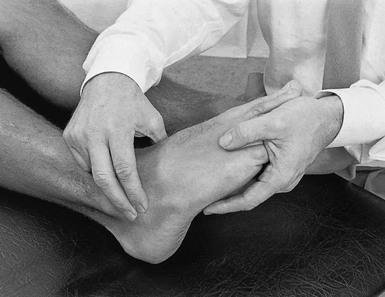
Technique: friction and electrical contractions
The patient lies prone with the foot fully plantiflexed. The therapist sits at the level of the patient’s leg. The fingers are placed at one side of the affected area and the thumb is positioned at the opposite side of the leg so as to apply counterpressure. The other hand may reinforce the palpating one (Fig. 57.2). Transverse friction starts deeply. By drawing the fingers upwards over the affected area, the therapist feels the muscle fibres escape from the grip until only skin and subcutaneous tissue remain. In the second stage, the fingers are slightly relaxed and moved backwards into the previous deep position, where the same movement starts again. The procedure is continued for about 15 minutes. During friction, the fingers do not move in relation to the skin – fingers and skin move as a unit over the muscle fibres.
The diagnosis and treatment of tennis leg is summarized in Box 57.1.
Achilles tendinopathy
The terminology used to describe this painful condition of the Achilles tendon is very confusing and terms such as Achilles tendinitis, tendonitis and tendinopathy have been widely used. In this book we use the term tendinopathy as the general clinical label for the combination of tendon pain, swelling and impaired performance. Peritendinitis and tendinosis are the histopathological entities of the disease.25
Achilles tendon problems are very common among athletes as well as the general population.1,2 Tendinitis of the Achilles tendon is chiefly a runner’s problem.26 Non-sporting people can also suffer from this condition and it then starts after unaccustomed exertion or a long walk in inappropriate shoes. Nevertheless, it most often occurs in long-distance runners, and it comes as no surprise that the increase in the number of people running during the past few decades has been paralleled by an increase in the number of cases of inflamed Achilles tendon.27,28 In a survey of 2002 running injuries seen over a 10-year period at a sports medicine referral clinic, overuse injury to the Achilles tendon was the sixth most common injury.29 The lifetime cumulative incidence of Achilles tendinosis is 5.9% among sedentary people and 50% among elite endurance athletes.30
The site of the lesion lies usually at mid-tendon. Occasionally, the strain occurs level with the upper border of the calcaneus or, very rarely, at the musculotendinous junction. Achilles tendinitis is multifactorial and usually the outcome of a combination of anatomical and biomechanical characteristics, along with poor training technique.31 The most important aetiological factors are short triceps (decreased touchdown angle), poor stretching habits and increased plantar flexion peak torque.32,33 Some authors suggest that there might also be a vascular factor furthering the condition.34,35 This would explain the usual location of the lesion at mid-tendon, which is the junction of its two vascular systems.36,37
During the last decade, fluoroquinolone antibiotics have been implicated in the aetiology of Achilles tendinitis and subsequent tendon rupture.38–41
The history in Achilles tendinitis is quite simple.42 The patient states that the heel aches during or after walking or running (stage I). Sometimes there is pain at the beginning of exertion, improving after a while and reappearing on fatigue (stage II). Alternatively, there is continuous and worsening pain during exercise (stage III). Sometimes the pain does not cease after exertion but continues at rest (stage IV). As a rule, however, pain eases at rest and increases on running or walking. Nocturnal pain is absent.
Because we advocate deep transverse friction as the most effective conservative treatment for this disorder and massage only acts where it is applied, the tendon should be palpated very carefully to discover all the tender areas because there may be more than one. The lesion nearly always lies at the inner or outer aspect, or both, of the tendon. Very often, the anterior surface is affected but almost never the posterior.43 Most of the lesions lie 2–6 cm above the tenoperiosteal junction.44 The morphological and macroscopic changes in the condition are not always the same. Observations during surgery have led to the description of two separate histopathological types:
• Peritendinitis: the inflammatory changes are confined to the peritenon, which is thickened and shows inflammatory changes, with considerable connective tissue proliferation and adhesions between peritendineum and tendon.45,46
• Tendinosis: this is characterized by inflammatory and degenerative changes in the tendon tissue itself.47,48 Sometimes partial ruptures of deeply situated fibres can be seen, with the superficial parts of the tendon remaining intact. Here there is a visible and palpable enlargement at the tendon from the structural changes of chronic fibrosis.49
Imaging methods
Ultrasonography has been used increasingly to examine Achilles tendon injuries. It is a quick, safe and inexpensive method to verify the existence and location of intratendinous lesions but is operator-dependent.50,51 Magnetic resonance imaging (MRI) is useful in visualizing pathological conditions of the tendon but is expensive and time-consuming. It is unwise, however, to rely solely on the results of these imaging techniques. First of all, the normal anatomy of an asymptomatic Achilles tendon may vary, which causes diagnostic misinterpretation.52 Secondly, several studies have reported intratendinous changes in up to 34% of cadaver specimens, in ultrasound and MRI images of patients without symptoms.53–55
Treatment
There are a number of approaches. Initial conservative treatment should be directed towards preventing adhesion formation between tendon and paratenon. Cold packs and stretching comprise most of the treatments proposed in the recent literature and may produce some benefit. Cold therapy is able to control pain and oedema, as well as to reduce regional blood flow and the metabolic demands of the tissue, and thereby helps to prevent further tissue damage at the site of injury. Passive stretching of the Achilles tendon has been advocated as restoring normal ankle joint mobility and decreasing the strain of the Achilles tendon with normal motion.56
Steroid injection
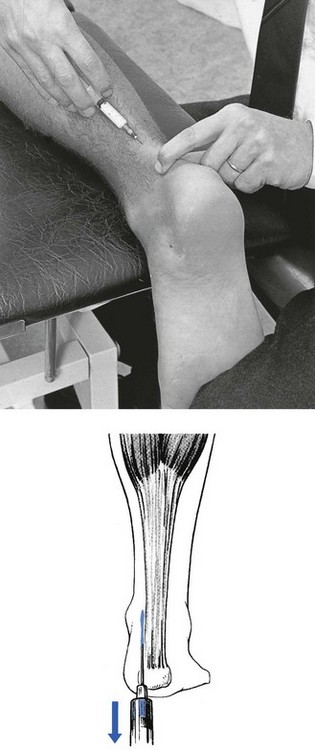
The role of corticosteroid injections in the treatment of Achilles tendinopathy is controversial.57–61 Several reports demonstrate disappointing results and injections have also been blamed for causing spontaneous rupture of the Achilles tendon.62 However, localized paratendinous infiltrations with small doses of triamcinolone (10–20 mg) still have a place in the treatment of Achilles tendinopathy, provided the correct technique is used. The injection is never made into the body of the tendon but along the surface, between tendon and peritendineum. After the injection, the patient should avoid all exercise during the first 10 days, after which a training programme can gradually be resumed. The injection can be repeated once if there is no cure after 2 weeks. If this procedure is followed and the correct technique is used, as set out below, postinfiltration ruptures are not to be feared.63
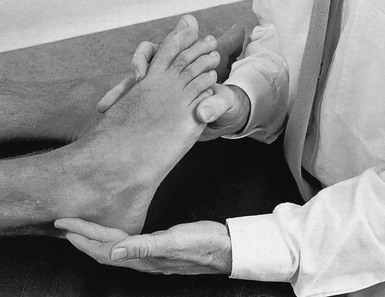
The patient lies prone on the couch. The foot is forced into dorsiflexion over the edge of the couch. This stretches the tendon, which facilitates palpation of the affected area. A 2 mL syringe is filled with 20 mg triamcinolone. A 5 cm needle is fitted and introduced some 3 cm away from the lesion. It is pushed through the skin and moved either upwards or downwards, parallel to the tendon, until the tip reaches the distal edge of the lesion. A small injection is given while the needle is drawn back along the surface of the tendon (Fig. 57.3); the manœuvre is repeated four or five times, each time a little to one side of the previous infiltration line. If the tip of the needle stays superficial to the tendon, no particular resistance to the plunger will be felt during the injection.
Prolotherapy
Recently, promising results have been described in studies of patients with Achilles tendinopathy who were treated with paratendinous injections of a sclerosing agent. On ultrasonography, neovascularization and tendon inhomogeneity decreased significantly as the clinical parameters improved.64–66
Surgery
In simple peritendinitis, the crural fascia and the paratenon are split longitudinally from the musculotendinous junction to the insertion on the calcaneus, and adhesions between the tendon and the sheath are released.67
In cases with focal tendinosis and partial rupture of the tendon, the diseased area of the tendon is excised and the tendon repaired by side-to-side suture of the remaining tendinous fibres.68 Where excision of the degenerated tissue disrupts the continuity of the tendon, the tendon is reconstructed and reinforced with the fascia of the gastrocnemius.69
If there is extensive tendinitis, excessive scar tissue is excised.70 Some authors claim better results if carbon fibres are implanted between the tendinous straps.71
Deep friction to the Achilles tendon
This was introduced more than 40 years ago by Cyriax74 and is, in our opinion, the best conservative treatment for the condition, provided it is given correctly: (a) at the right point, (b) with a good friction technique, (c) 20 minutes per session and (d) at regular intervals (three times a week). During the period of treatment, the patient must take relative rest.
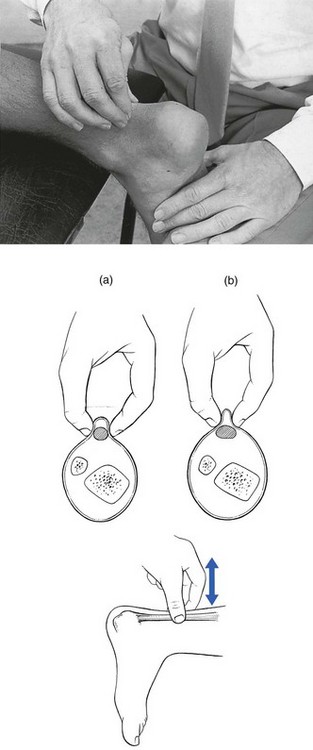
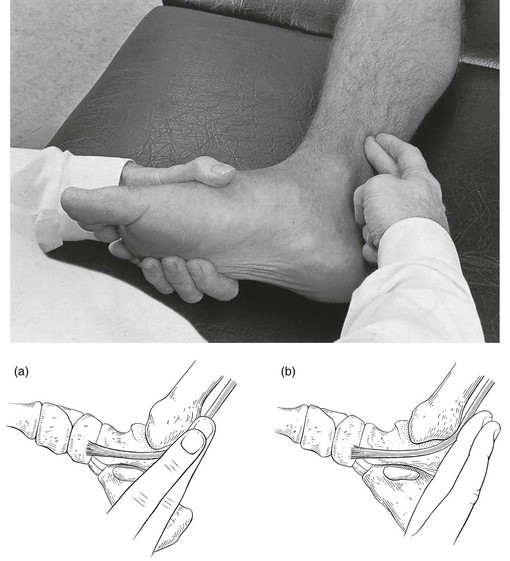
Technique: friction to the medial and lateral edge of the tendon![]()
The patient lies face downwards on a low couch, with the foot projecting just beyond the edge of the couch. The therapist sits at the foot and pushes the sole into dorsiflexion through a slight pressure of the contralateral knee. At the correct point the tendon is grasped between finger and thumb, or two fingers and thumb, depending on the extent of the lesion (‘a’ in Fig. 57.4). Slight pressure under the tendon is exerted and the hand is drawn upwards until the fingers slip towards the posterior aspect of the tendon (‘b’ in Fig. 57.4). In the final stage of this manœuvre, only skin remains between the two grasping fingers. The pressure is now released slightly and the fingers are pushed downwards until they lie at the starting position (‘a’) and the whole procedure can be repeated. The cycle is repeated for about 15 minutes.
Technique: friction to the anterior part of the tendon![]()
This localization should always be sought in addition to other tender spots.
Once again, friction is given in two phases. First, the fingertip is placed deeply under the tendon with the forearm in a slightly pronated position (‘a’ in Fig. 57.5). Pressure is exerted in a dorsal and medial direction; meanwhile, the arm moves in full supination, until the lateral fibres escape under the fingertip (‘b’ in Fig. 57.5). Caution is taken not to move the finger on the skin but rather to move the skin and the fingertip as a whole. Now pressure is slightly released and the fingertips replaced in the former position (‘a’), so that the whole procedure can be repeated. The to-and-fro movements are performed for 15 minutes. The fingers must not be allowed to glide on the skin, to avoid the formation of a blister.
Technique: friction to the tenoperiosteal insertion of the tendon![]()
The tendon is compressed between the therapist’s fingers and the upper surface of the calcaneus. Using both hands, a circle is made round the heel with one index finger, reinforced by the other, at the lesion. Both thumbs cross at the plantar surface. Pressing downwards squeezes the tendon between the fingers and the calcaneus. Deep friction is performed by moving the forearms in opposite directions. The amplitude of the movement must be large enough to reach the whole width of the tendon (Fig. 57.6).
Eccentric training
Recently, there has been increasing interest in the use of eccentric loading in treatment of chronic Achilles tendinopathy. (In an eccentric contraction, the muscle–tendon unit lengthens as a load is applied to it.) In 1986 Stanish et al75 reported that a once-daily, 6-week eccentric loading programme led to complete relief of pain in 44% and a marked improvement in symptoms in a further 43% of patients. More recently, others have confirmed the efficacy of eccentric loading for mid-substance lesions of the Achilles tendon,76,77 and high success rates (at least 60% either good or excellent) have also been reported in prospective randomized trials.78–80 However, the mechanism for the efficacy of eccentric loading remains unknown.81
Prevention
Raised heels, shock-absorbing heels and correction of a valgus deformity are usually prescribed.82 As the triceps is also a slight invertor, a valgus deformity must always be corrected to relieve excessive strain on the tendon.83 Although these measures are certainly beneficial, it is important to remember that they are prescribed for prevention only because they do not lead to substantial and histological changes at the site of adhesions.
Many authors pay a great deal of attention to the preventive value of stretching exercises before running.84,85 Although they may have such value, the worth of stretching techniques alone should not be overestimated when they are used as therapy in actual lesions. Stretching is a good method of prevention but, in our experience, has no therapeutic value.
Achilles tenovaginitis
Rheumatoid arthritis and ankylosing spondylitis
In these conditions, the contrast between the mild symptoms and the marked signs is striking. It is also important to remember that gout can sometimes affect the Achilles tendon. The main complaint is not, as in tendinitis, pain during contraction of the triceps but pain during local pressure, e.g. catching the heel against the edge of the shoe. Examination shows that rising on tiptoe is indeed just uncomfortable rather than painful but the tendon is warm, swollen and very tender to the touch.86,87 Local treatment consists of infiltration with 20 mg of triamcinolone between the sheath and the tendon. The technique is the same as described for Achilles tendinitis.
Calcaneus apophysitis
Apophysitis of the calcaneus (Sever’s disease, Osgood’s disease) occurs in boys between 6 and 12 years of age and is often bilateral. The disorder has been classified among the general osteochondrosis syndromes, such as Legg–Calvé–Perthes disease at the hip or Osgood–Schlatter disease at the tibial tuberosity. The child complains of sharp pain in the heel, occurring during contraction of the triceps. The pain starts suddenly, can last a couple of hours or days, and may disappear and reappear. Rising on tiptoe can be negative but the bone is usually tender to the touch. The radiological appearances are characteristic – ‘slight fragmentation of the apophysis’ – and confirm the diagnosis. Spontaneous recovery occurs in a year or two, often with the development of a slight permanent prominence on the posterior aspect of the calcaneus.88
There is no treatment except relative rest, slightly raising the heel and inserting shock-absorbing heel pads in the shoe.89
Weakness
Weakness of the plantiflexor mechanism is detected by an inability to rise on tiptoe.
Apart from neurological lesions, which are discussed at the end of this chapter, the commonest cause of weakness is a rupture of the Achilles tendon, most frequent in athletes over 30 years of age.90 The tear lies in the ‘critical zone of poor vascularization’, which is 2–6 cm above the calcaneal insertion.91
It is surprising that this simple and easy-to-detect condition very often remains undiagnosed for a time. Between 30 and 41% of Achilles tendon ruptures remain undiagnosed for more than 2 weeks.35,92,93
When the patient lies on the couch, the clinical examination reveals little. There is usually no haematoma or visible thickening. Passive movements are painless. An alert examiner will probably detect an excessive range of dorsiflexion. In the supine, non-weight-bearing position, resisted plantiflexion remains possible because the plantaris, flexor hallucis longus and flexor digitorum muscles still contract. Rising on tiptoe, however, immediately reveals the diagnosis. The squeeze test is also positive: the patient lies prone, with both feet suspended over the edge of the couch; compressing the triceps surae causes plantiflexion of the foot when the tendon is intact but not when it is ruptured.14
Treatment
There is still controversy concerning the best treatment for Achilles tendon ruptures. It appears that a satisfactory outcome may be achieved with either non-operative or operative treatment but surgical repair appears to provide better functional capacity94 with better scores of strength, power and endurance95–97 and lower re-rupture rates. The advantages of the conservative approach are that there are no risks of anaesthesia, infection, skin adhesions and sural nerve injury.98,99 Reports in the literature indicate that in active, young, very demanding individuals, surgical repair should be considered, with non-surgical treatment reserved for elderly or sedentary patients.100–102 However, conservative treatment can also be considered in athletically active patients, as treatment should always be individualized to the concerns and health of the patient.103,104
There is no single, uniformly accepted surgical technique for Achilles tendon repair. Most acute ruptures have been treated successfully with excision of the devitalized tendon tissue and simple end-to-end suture. However, various augmentation procedures, such as reinforcement of the suture with a triceps surae tendon tip-over graft, have been combined with simple suture and have had satisfactory outcomes.105–107 To minimize the complications typically associated with open surgery, percutaneous techniques to repair the ruptured Achilles tendon have been advocated, and the results are reported to be promising, although not without failures and complications.108,109
Several recent studies have reported functional benefits of early postoperative tendon mobilization in well-motivated patients, as treatment results are determined not only by the method of repair but also, and perhaps more importantly, by the early postoperative functional rehabilitation.110,111
Conservative treatment consists of 8 weeks in a plaster cast with the foot in equinus position, followed by the use of a 2.5 cm heel for an additional 1 or 2 months.112,113 The thickened and enlarged scar tissue resulting from conservative treatment can be massaged twice a week for 2–3 months. The fibrous swelling at the point of the rupture never seems to disappear, however, and some residual disability can be permanent.
It can be concluded that the treatment of choice in the athletically active patient is primary surgical repair.114 Conservative treatment is chosen in middle-aged or less active patients.115
Short plantiflexor muscles
Short calf muscles, resulting in equinus deformity, are among the most common complications in children with cerebral palsy.116 Sometimes, shortening of calf muscles is an isolated finding and may easily be overlooked.
Clinical examination
This shows the dorsiflexion range at the ankle joint to be painlessly limited. A gastrocnemius equinus is typically characterized by less than 10° of ankle dorsiflexion with the knee extended.117
Complications
Because the patient cannot bear weight adequately on the heels, mid-tarsal hypermobility and later painful strain will result. Limited dorsiflexion at the ankle can also lead to various compensations in the lower extremity that ostensibly cause secondary problems, including Achilles tendinopathy,118 flat foot, chronic metatarsalgia119 and strain of the plantar fascia.120
Symptoms and complications associated with short plantiflexor muscles are summarized in Box 57.2.
Treatment
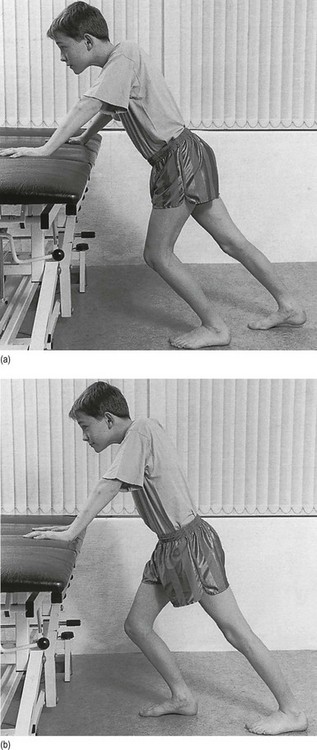
Younger patients
The soleus muscle is stretched in the following way. The child performs knee flexion exercises and tries to keep the heels on the ground (Fig. 57.7a). Once this can be done easily, the patient is encouraged to lean further and further forwards so as to stretch the soleus more.
To stretch the gastrocnemii muscles, the child stands in front of a wall, with feet fully dorsiflexed and knees extended, the heels remaining on the ground. The patient then leans forwards, keeping the knees firmly in full extension (Fig. 57.7b).
Lesions of the dorsiflexors
Pain
Lesions of the muscle bellies respond equally well to local anaesthesia and deep friction (Box 57.3). Three injections, each of 10–30 mL of procaine 0.5%, at weekly intervals usually give good results. Friction is given according to the general principles that it should be deep and transverse, with sufficient sweep on a relaxed muscle, three times a week for 6–10 sessions.
Special conditions
Myosynovitis of the tibialis anterior muscle
The only parallel condition in the body is myosynovitis of the bellies of the abductor pollicis longus and the extensor pollicis muscles in the forearm. The lesion occurs as an overuse phenomenon in skaters, skiers and long-distance runners. It has also been described in army recruits after a long march, who are unaccustomed to wearing heavy boots.123 Resisted dorsiflexion hurts above the front of the ankle. Painless resisted dorsiflexion of the big toe and outer toes points to the tibialis anterior muscle but palpation fails to reveal any tenderness in the anterior tibial tendon itself. If the palpating finger moves upwards to the musculotendinous junction, a painful area is detected close to the bone. If the foot is moved gently up and down, crepitus may be felt.
Technique: deep transverse friction to the tibialis anterior muscle
The therapist sits opposite the patient. With one hand, the foot is brought into full plantiflexion and eversion in order to stretch the muscle. The thumb of the other hand is placed at the medial aspect of the leg and the fingers on the lesion (Fig. 57.8). The thumb is used as a fixed point and the fingers move in a transverse direction over the anterior aspect of the anterior tibial muscle. To allow sufficient sweep, the movement is conducted by an adduction movement of the shoulder.
Tight fascia syndrome of the anterior compartment
This disorder may resemble intermittent claudication but the patient is much younger and physically active. After exertion – for example, kicking a football for about 10 minutes – voluntary dorsiflexion becomes impossible and what seems like a drop foot develops. This is accompanied by vague pain at the front of the leg and sometimes by pins and needles over the dorsum of the foot and the inner four toes. After a short rest, the muscle recovers and pain and weakness disappear.124 When the patient is examined at rest, nothing special is revealed: dorsiflexion is strong and painless, and the arterial pulsations are normal. In long-standing cases, it is sometimes possible to palpate fascial hernias over the front of the leg.125
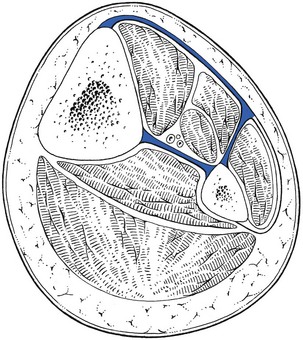
The symptoms result from increased tissue fluid pressure in the closed fascial compartment which is formed by the tibia, the fibula, the interosseous membrane and the anterior fascia (Fig. 57.9). During exercise, muscle volume may expand by 20%, from both increased blood flow and capillary filtration.126,127 If the superficial fascia is not lax enough to accommodate the greater volume, the intramuscular pressure rises to levels that compress the anterior tibial artery. This produces relative muscle ischaemia and therefore temporary paralysis and pain. The swelling may also trap the superficial peroneal nerve at its exit through the fascial foramen at mid-leg and cause paraesthesia in the outer foot.
After some minutes’ rest, blood flow recovers and symptoms resolve. Because the patient is asymptomatic between occurrences and not chronically disabled, some authors prefer the suffix ‘recurrent’ rather than ‘chronic’ to identify anterior compartment syndromes.128 However, if the minute vessels in the belly of the muscle themselves gradually become silted up with cells, the disorder may become irreversible.129
The diagnosis is made on the typical history in combination with a negative clinical examination. However, if the athlete is examined after completing the exercise that reproduces the symptoms, clinical examination will show pain on passive plantiflexion and weak dorsiflexion. The anterior compartment is also tender on palpation.130
The differential diagnoses of an anterior compartment syndrome include shin splint, stress fracture, nerve entrapment syndromes and claudication.131 The gold standard of diagnosing anterior compartment syndrome is the measurement of intracompartmental pressures before and after exertion.132,133 A resting pressure > 15 mm Hg, and 5 minutes post-exercise pressures > 20 mm Hg are diagnostic of compartment syndrome.134–136
Acute and severe anterior compartment syndromes may develop after a tibial fracture137 or a direct blow.138 Within a few hours, pain at the mid-leg becomes intense and is not relieved by immobilization. The overlying skin sometimes becomes shiny and warm. Together with the palpable tenderness, this may give the false impression of cellulitis. Making this error is a disaster because, if the diagnosis is not made at once and the fascia divided immediately, ischaemic necrosis will ensue. Complete paralysis with a permanent drop foot will then result. There are also documented cases of bilateral compartment syndrome with permanent drop foot complicating surgery of long duration in the lithotomy position.139
Treatment
Apart from altering the patient’s activities or training programmes, surgery seems to be the only effective treatment for recurrent compartmental syndromes. The surgical procedure consists of a subcutaneous fasciotomy.140–142
In acute cases, surgical decompression must be performed as soon as possible. As in a strangulated inguinal hernia, the motto is: ‘operate before sunset or sunrise’.143 Sheridan and Matsen144 found that fasciotomy performed within 12 hours of onset of a compartment syndrome resulted in normal function in 68% of cases. However, in those decompressed after 12 hours, only 8% recovered normal function.
Lesions of the invertors
Pain
The main invertor muscles are the anterior and posterior tibialis muscles (Fig. 57.10). The flexor hallucis longus and the triceps are weak invertors as well.
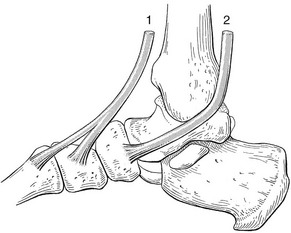
Fig 57.10 Tendons and insertions of the main invertor muscles: 1, tibialis anterior; 2, tibialis posterior.
Posterior tibial tendinitis is usually caused by overuse, which occurs frequently in a valgus deformity at the subtalar joint.145 Resisted inversion of the foot hurts and dorsiflexion does not. Because the tibialis posterior has an additional function in stabilizing the hindfoot during rising on tiptoe, this test may also be painful. Palpation then discloses whether the lesion lies at the insertion on the navicular bone, at the tendon (distal or proximal to or under the medial malleolus), at the muscle belly or at the proximal musculotendinous junction.
In rheumatoid tenosynovitis, 10 mg of triamcinolone is injected between the tendon and its sheath.
Deep friction techniques
Technique: friction to the upper part of tibialis posterior
The therapist sits lateral to the patient’s foot. With the contralateral hand, the foot is fixed in dorsiflexion. As the tendon lies deeply between the posterior aspect of the tibia and the tendon of the flexor digitorum longus, the proper spot can only be reached if the pronation–supination technique is used. The middle finger of the ipsilateral hand, reinforced by the index finger, is thus laid flat on the affected part of the tendon, just behind the edge of the tibia (Fig. 57.11). The ring and little fingers are kept extended. The fingers, the wrist and the forearm are brought into line with the tibia. Friction is imparted with a supination movement, which is continued until the tendon escapes from the finger. Pressure is then released a little and the finger returned to the original position by pronation.
Technique: friction to the lower part of tibialis posterior
The patient’s foot is dorsiflexed and the therapist sits level with the affected foot. The thumb of the contralateral hand is placed at the lateral side of the foot. The tips of one or two fingers are placed on the affected length of the tendon, just beyond it. Friction is now given with an extension movement at the wrist (Fig. 57.12), using the thumb as a fulcrum. The fingers ride over the whole width of the tendon until the latter escapes from the pressure. Using flexion of the wrist, without losing contact with the skin, the fingers are then moved to the original position behind the tendon, and the whole procedure is repeated.
Friction is continued for 20 minutes, twice a week, for 1 or 2 weeks.
Shin splints
Pain at the posterior medial edge of the tibia in athletes and long-distance runners is called ‘shin splints’ or ‘medial tibial stress syndrome’. Few conditions have caused as much controversy. The term has been used to cover a variety of conditions, such as stress fractures,146–148 periostitis and soft tissue inflammation.149 The American Medical Association subcommittee for classification of sports injuries restricts the name shin splints to musculotendinous lesions of the tibialis posterior muscle.150
The disorder appears as an overuse phenomenon in runners and is one of the most common causes of exertional leg pain, accounting for 6–16% of all running injuries.151
The most common complaint is diffuse pain of the lower extremity, along the middle-distal tibia, associated with exertion. In the early course, pain is worse at the beginning of exercise but gradually subsides during training and within minutes of cessation of exercise. As the injury progresses, however, pain presents with less activity and may occur at rest.152
Differential diagnosis must include exertional compartment syndrome and stress fracture. Here, pain is elicited by sharply striking the heel or tapping the anterior tibia, or the bone is tender to direct pressure. During the initial weeks, a stress fracture is not visible on a plain radiograph153 but can be detected with ultrasound.154 In case of doubt, a bone scintigram can be obtained that easily distinguishes an inflammatory shin splint from a stress fracture.155,156
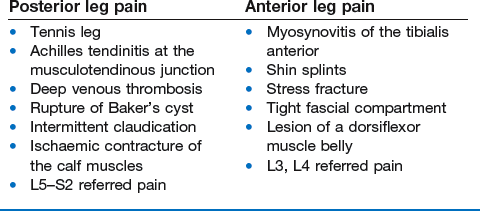
Differential diagnosis between posterior and anterior leg pain is summarized in Box 57.4.
Weakness
Neurological lesions are discussed at the end of this chapter.
Weak resisted inversion is often caused by a rupture of the tibialis posterior tendon (TPT), secondary to a combination of degenerative changes and trauma.157 It is usually located in a critical zone with a low degree of vascularity, posterior to the medial malleolus.158
• Valgus deformity of the heel
• Loss in height of the medial longitudinal arch
• Abduction of the forefoot, which is detected by the ‘too many toes sign’159: more of the lateral toes are seen on the affected side when the patient is inspected from behind.
Rupture of the tibialis posterior tendon thus leads to a progressive, unilateral, acquired flat foot, with increasing valgus of the heel, plantar flexion of the talus and subluxation of the talonavicular joint.157,160
It is difficult to detect weakness of the tibialis posterior during manual testing because the synergistic action of the other invertors of the foot substitutes for the power of the ruptured muscle. Weakness of the tendon is best detected during rising on tiptoe. In a normal foot, this test shows a typical sequence. First the TPT is activated, which inverts the foot and locks the heel and the mid-tarsal joints. Then the triceps muscle pulls on the now-rigid calcaneus, the heel rises and the body weight is imparted to the ball of the foot. With a rupture of the TPT, however, the initial varus movement at the heel is impossible and the patient rises up with the heel in valgus or does not get up on to the ball of the foot at all.161,162
Conservative treatment includes a medial heel wedge and a longitudinal arch support.163
Surgical treatment must be considered when the patient is young and active. A plantaris or extensor tendon graft may be used to bridge the defect. Recently, the transfer of the flexor digitorum longus tendon into the sheath of the tibialis posterior has been used for larger defects.164,165
Lesions of the evertors
Pain
Tendinopathy
If there is pain on resisted eversion of the foot, the peroneal muscles are at fault. Peroneal tendinosis is usually a simple overuse phenomenon in runners and skaters,166,167 although it may also appear as a complication of ankle sprain (see p. 774).168,169
Treatment
Technique: deep friction above and below the malleolus 170
170
The patient lies supine, with the leg medially rotated. The therapist sits at the opposite side. The foot is brought into inversion; this stretches the tendon. Two or three fingertips of the therapist’s ipsilateral hand are now placed on the tendon. The fingers are slightly flexed, thereby pressing the tendon against the fibular shaft. The thumb is placed at the medial side of the lower leg or ankle to provide counterpressure (Fig. 57.13). Friction is given with a to-and-fro movement of the forearm, during which the fingers ride over the tendon. The friction is in two phases: an active phase, during which the tendon is pressed and pulled, and a relaxed phase, during which the fingers are placed in the previous position to restart the movement.
Technique: deep friction level with the malleolus
The therapist sits by the patient’s foot, facing it. The foot is held in inversion and plantar flexion is produced by slight pressure of the ipsilateral hand. The therapist holds the contralateral hand and forearm in line with the leg. The middle finger, reinforced by the index finger, is placed in the sulcus, behind the peroneus tendon (Fig. 57.14). Friction is started with the finger behind the tendon. Pressure is exerted and, with a supination movement of the forearm, the tendon is pressed anteriorly until it escapes from the finger and slips backwards. The now-supinated hand is manœuvred back to the pronated position behind the tendon, where the movement restarts.
Other conditions
‘Snapping ankle’
Sometimes patients complain of a slight pain, together with a snapping feeling at the outer side of the ankle, during certain movements. The reason is a loosening of the peroneal tendons in the groove of the posterior surface of the fibula. They slip forwards over the malleolus when the ankle is dorsiflexed and ‘jump back’ during plantiflexion.171 This ‘snapping ankle’ is usually not painful, just uncomfortable. Sometimes, however, it is the origin of a superimposed tendinitis. Non-surgical treatment should always be instituted first and consists of holding the tendons reduced in their anatomical positions while the superior peroneal retinaculum heals by scarring.172 If considerable discomfort remains, surgery can be advised. Different methods of repair have been described.173,174 Usually, a new retinaculum is constructed behind the lateral malleolus or the calcaneofibular ligament is transposed to the lateral side of the peroneal tendons.175
Disorders causing neurological weakness of the foot
Dorsiflexion, eversion and inversion are tested in the supine-lying position. As described in Chapter 55, it is very important to give strong counterpressure, with the leg in a neutral position. Normally, the extrinsic muscles of the foot are very strong and their pull cannot be overcome by the examiner’s force. Both sides should be compared.
In central or upper motor neurone lesions, the weakness is gross and distributed over different muscles and muscle groups (Table 57.1).
Table 57.1
Innervation of neurological weakness of the foot
| Muscle | Segmental innervation | Peripheral nerve |
| Tibialis anterior | L4 (L5) | Deep peroneal |
| Extensor digitorum longus | L4, L5 | Deep peroneal |
| Extensor hallucis longus | L4, L5 | Deep peroneal |
| Peronei | L5, S1 | Superficial peroneal |
| Tibialis posterior | L4, L5 | Tibial |
| Flexor digitorum longus | L5–S1 | Tibial |
| Flexor hallucis longus | L5–S1 | Tibial |
| Triceps surae | S1, S2 | Tibial |
In lesions of a peripheral nerve, weakness follows the normal afferent distribution of the nerve. Very often, the pain appears silently, without previous pain in the innervated area. As the peripheral nerves in the lower limb behave in the same way as a nerve trunk, paraesthesia will only appear when pressure on the nerve is released and not during the actual period of compression (see release phenomenon in Ch. 2).176,177
References
1. Naish, JM, Appley, J, ‘Growing pains’. A clinical study of nonarthritic limb pain in children. Arch Dis Child 1951; 26:134–140. ![]()
2. Oster, J, Nielsen, A, Growing pains – a clinical investigation of a school population. Acta Paediatr Scand 1972; 61:134–140. ![]()
3. Baxter, MP, Dulberg, C, ‘Growing pains’ in childhood. A proposal for treatment. J Pediatr Orthop 1988; 8:402–406. ![]()
4. Harel, L, Growing pains: myth or reality. Pediatr Endocrinol Rev. 2010;8(2):76–78. ![]()
5. Miller, A, Rupture of the musculotendinous juncture of the medial head of the gastrocnemius. Am J Sports Med 1977; 5:191–193. ![]()
6. Hood, WP. On lawn-tennis leg. Lancet. 1884; i:728–729.
7. Gilcreest, EL. Ruptures and tears of muscles and tendons of the lower extremity. JAMA. 1993; 100:153–160.
8. Cornwell, HE, Allredge, RH. Ruptures and tears of tendons and muscles. Am J Surg. 1937; 35:22–33.
9. Golding, D, Tennis leg. BMJ 1969; 4:243. ![]()
10. Gaulrapp, H, ‘Tennis leg’: ultrasound differential diagnosis and follow-up. Sportverletz Sportschaden. 1999;13(2):53–58. ![]()
11. Bianchi, S, Martinoli, C, Abdelwahab, IF, et al, Sonographic evaluation of tears of the gastrocnemius medial head (‘tennis leg’). J Ultrasound Med. 1998;17(3):157–162. ![]()
12. Werken van der, C, Marti, RK, Rupturen van de Achillespees. Ned Tijdschr Geneeskd 1980; 124:1321–1322. ![]()
13. Visser, JD, Achillespeesruptuur. Ned Tijdschr Geneeskd 1980; 124:1340–1342. ![]()
14. Thompson, TL, Doherty, JH, Spontaneous rupture of tendon of Achilles, a new diagnostic clinical test. J Trauma 1962; 2:126–129. ![]()
15. Gauer, EF, Düring, M, Müller, W, Die proximate Ruptur im Triceps surae, eine typische, aber oft verkannte Verletzung. Chirurgie. 1976;47(4):236–240. ![]()
16. Scurr, JH, Coleridge-Smith, PD, Hasby, JH, Deep venous thrombosis: a continuing problem. BMJ 1988; 297:28. ![]()
17. Lambie, JM, Mahaffy, RG, Barber, DC, et al, Diagnostic accuracy in venous thrombosis. BMJ 1970; ii:142–143. ![]()
18. Kakkar, W, Howe, CT, Flance, C, Clarke, MB, Natural history of postoperative deep vein thrombosis. Lancet 1969; ii:230–232. ![]()
19. Baker WM. Chronic synovial cysts 1887; Report. St Bartholomew’s Hospital, London.
20. Cyriax, JH. Textbook of Orthopaedic Medicine, 8th ed. London: Baillière Tindall; 1982.
21. Colson, JHC, Armour, WJ. Sport Injuries and their Treatment. London: Stanley Paul; 1975.
22. Franke, K. Traumatologie des Sports. Stuttgart: Thieme; 1980.
23. Dürig, M, Schuppiser, JP, Gauer, EF, Muller, W, Spontaneous rupture of the gastrocnemius muscle. Injury 1977; 9:143–145. ![]()
24. Kwak, HS, Lee, KB, Han, YM, Ruptures of the medial head of the gastrocnemius (‘tennis leg’): clinical outcome and compression effect. Clin Imaging. 2006;30(1):48–53. ![]()
25. Khan, KM, Cook, JL, Kannus, P, et al, Time to abandon the ‘tendinitis’ myth [editorial]. BMJ 2002; 324:626–627. ![]()
26. Biedert, R, Beschwerden im Achillessehnenbereich. Ätiologien und therapeutische Äberlegungen. Unfall Chirurg. 1991;94(10):531–537. ![]()
27. Devereaux, MD, Lachmann, SM, Athletes attending a sports injury clinic – a review. Br J Sports Med 1983; 17:137–142. ![]()
28. Kvist, DR, Järvinen, M. Zur Epidemiologie von Sportverletzungen und Fehlbelastungsformen. Patienten-analyse einer Sportmedizinischer Poliklinik. Med Sport. 1980; 20:375–378.
29. Taunton, JE, Ryan, M, Clement, DB, et al, A retrospective case-control analysis of 2002 running injuries. Br J Sport Med 2002; 36:95–101. ![]()
30. Kujala, UM, Sama, S, Kaprio, J, Cumulative incidence of Achilles tendon rupture and tendinopathy in male former elite athletes. Clin J Sport Med 2005; 15:133–135. ![]()
31. McCrory, JL, Martin, DF, Lowery, RB, et al, Etiologic factors associated with Achilles tendinitis in runners. Med Sci Sports Exerc. 1999;31(10):1374–1381. ![]()
32. Scioli, MW, Achilles tendinitis. Orthop Clin North Am. 1994;25(1):177–182. ![]()
33. Reinschmidt, C, Nigg, BM, Influence of heel height on ankle joint moments in running. Med Sci Sports Exerc. 1995;27(3):410–416. ![]()
34. Lemaire, M, Miremad, C, Combelles, F. Tendinite du tendon d’Achille du sportif. Méd Sport. 1981; 55:6.
35. Zuinen, C. Ruptures du tendon d’Achille. Méd Sport. 1980; 54:6.
36. Logengren, C, Lindholm, A, Vascular distribution in the Achilles tendon. Acta Chir Scand 1958; 116:491–495. ![]()
37. Schmidt-Rohlfing, B, Graf, J, Schneider, U, Niethard, FU, The blood supply of the Achilles tendon. Int Orthop. 1992;16(1):29–31. ![]()
38. McGarvey, WC, Singh, D, Trevino, SG, Partial Achilles tendon ruptures associated with fluoroquinolone antibiotics: a case report and literature review. Foot Ankle Int. 1996;17(8):496–498. ![]()
39. van der Linden, PD, van de Lei, J, Nab, HW, et al, Achilles tendinitis associated with fluoroquinolones. Br J Clin Pharmacol. 1999;48(3):433–437. ![]()
40. Lewis, JR, Gums, JG, Dickensheets, DL, Levofloxacin-induced bilateral Achilles tendonitis. Ann Pharmacother. 1999;33(7–8):792–795. ![]()
41. Casparian, JM, Luchi, M, Moffat, RE, Hinthorn, D, Quinolones and tendon ruptures. South Med J. 2000;93(5):488–491. ![]()
42. Schepsis, AA, Jones, H, Haas, AL, Achilles tendon disorders in athletes. Am J Sports Med 2002; 30:287–305. ![]()
43. Ohberg, L, Lorentzon, R, Alfredson, H, Neovascularisation in Achilles tendons with painful tendinosis but not in normal tendons: an ultrasonographic investigation. Knee Surg Sports Traumatol Arthrosc 2001; 9:233–238. ![]()
44. Paavola, M, Kannus, P, Järvinen, T, et al. Current concepts review: Achilles tendinopathy. J Bone Jt Surg. 2002; 84A:2062–2076.
45. Kvist, MH, Lehto, MU, Jozsa, L, et al, Chronic Achilles paratenonitis: an immunohistologic study of fibronectin and fibrinogen. Am J Sports Med 1988; 16:616–623. ![]()
46. Järvinen, M, Jóa, L, Kannus, P, et al, Histopathological findings in chronic tendon disorders. Scand J Med Sci Sports 1997; 7:86–95. ![]()
47. Clement, DB, Taunton, JE, Smart, GW, Achilles tendinitis and peritendinitis. Etiology and treatment. Am J Sports Med 1984; 12:179–184. ![]()
48. Åström, M, Rausing, A, Chronic Achilles tendinopathy. A survey of surgical and histopathologic findings. Clin Orthop 1995; 316:151–164. ![]()
49. Auquier, L, Siaud, JR, Tendinites nodulaires du tendon d’Achille. Rev Rhum 1971; 38:373–381. ![]()
50. Schie, HT, de Vos, RJ, de Jonge, S, et al, Ultrasonographic tissue characterisation of human Achilles tendons: quantification of tendon structure through a novel non-invasive approach. Br J Sports Med 2010; 44:1153–1159. ![]()
51. Paavola, M, Paakkala, T, Kannus, P, Järvinen, M, Ultrasonography in the differential diagnosis of Achilles tendon injuries and related disorders. A comparison between preoperative ultrasonography and surgical findings. Acta Radiol 1998; 39:612–619. ![]()
52. Soila, K, Karjalainen, PT, Aronen, HJ, et al, High resolution MR imaging of the asymptomatic Achilles tendon: new observations. AJR Am J Roentgenol 1999; 173:323–328. ![]()
53. Haims, AH, Schweitzer, ME, Patel, RS, et al, MR imaging of the Achilles tendon: overlap of findings in symptomatic and asymptomatic individuals. Skeletal Radiol 2000; 29:640–645. ![]()
54. Khan, KM, Forster, BB, Robinson, J, et al, Are ultrasound and magnetic resonance imaging of value in assessment of Achilles tendon disorders? A two year prospective study. Br J Sports Med 2003; 37:149–153. ![]()
55. Emerson, C, Morrissey, D, Perry, M, Jalan, R, Ultrasonographically detected changes in Achilles tendons and self reported symptoms in elite gymnasts compared with controls – an observational study. Man Ther 2010; 15:37–42. ![]()
56. Sandmeier, R, Renström, PA, Diagnosis and treatment of chronic tendon disorders in sports. Scand J Med Sci Sports 1997; 7:96–106. ![]()
57. Daniel, U, Skeoch, MD. Spontaneous partial subcutaneous ruptures of the tendo Achilles. Am J Sports Med. 1981; 9(1):135–137.
58. Bedi, S, Ellis, W, Achilles tendon ruptures. Ann Rheum Dis 1970; 29:494. ![]()
59. Visser, JD. Achillespeesruptuur. Ned Tijdschr Geneeskd. 1980; 124(32):1344–1347.
60. Krahl, H, Plaue, R. Sehnenrupturen nach Cortisoninjektionen. Med Sport. 1971; 11:264.
61. Mahler, F, Fritschy, D, Partial and complete ruptures of the Achilles tendon and local corticosteroid injections. Br J Sports Med. 1992;26(1):7–14. ![]()
62. Shrier, I, Matheson, GO, Kohl, HW, Achilles tendonitis: are corticosteroid injections useful or harmful? Clin J Sport Med. 1996;6(4):245–250. ![]()
63. Read, MT, Motto, SG, Tendo Achillis pain: steroids and outcome. Br J Sports Med. 1992;26(1):15–21. ![]()
64. Maxwell, NJ, Ryan, MB, Taunton, JE, et al, Sonographically guided intratendinous injection of hyperosmolar dextrose to treat chronic tendinosis of the Achilles tendon: a pilot study. AJR 2007; 189:947. ![]()
65. Alfredson, H, Öhberg, L, Sclerosing injections to areas of neo-vascularisation reduce pain in chronic Achilles tendinopathy: a double-blind randomised controlled trial. Knee Surg Sports Traumatol Arthrosc 2005; 13:338–344. ![]()
66. Ryan, M, Wong, A, Taunton, J, Favorable outcomes after sonographically guided intratendinous injection of hyperosmolar dextrose for chronic insertional and midportion achilles tendinosis. AJR Am J Roentgenol. 2010;194(4):1047–1053. ![]()
67. Schepsis, AA, Leach, RE, Surgical management of Achilles tendinitis. Am J Sports Med. 1987;15(4):308–315. ![]()
68. Saxena, A, Surgery for chronic Achilles tendon problems. J Foot Ankle Surg. 1995;34(3):294–300. ![]()
69. Schepsis, AA, Wagner, C, Leach, R, Surgical management of Achilles tendon overuse injuries. Am J Sports Med 1994; 5:611–619. ![]()
70. Nelen, G, Martens, M, Burssens, A, Surgical treatment of chronic Achilles tendinitis. Am J Sports Med 1989; 17:754–759. ![]()
71. Jenkins, DHR, Forster, IW, McKibbin, B, Ralis, ZA, Induction of tendon and ligament formation by carbon implantation. J Bone Joint Surg 1977; 59B:53–57. ![]()
72. Leach, RE, Schepsis, AA, Takai, H, Long-term results of surgical management of Achilles tendinitis in runners. Clin Orthop 1992; 282:208–212. ![]()
73. Maffulli, N, Testa, V, Capasso, G, et al, Results of percutaneous longitudinal tenotomy for Achilles tendinopathy in middle- and long-distance runners. Am J Sports Med. 1997;25(6):835–840. ![]()
74. Cyriax, JH. Textbook of Orthopaedic Medicine, vol. II. Treatment by Manipulation, Massage and Injection. London: Baillière Tindall; 1986.
75. Stanish, WD, Rubinovich, RM, Curwin, S, Eccentric exercise in chronic tendinitis. Clin Orthop Relat Res 1986; 208:65–68. ![]()
76. Alfredson, H, Pietilä, T, Jonsson, P, Lorentzon, R, Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med 1998; 26:360–366. ![]()
77. Mafi, N, Lorentzon, R, Alfredson, H, Superior short-term results with eccentric calf muscle training compared to concentric training in a randomized prospective multicenter study on patients with chronic Achilles tendinosis. Knee Surg Sports Traumatol Arthrosc 2001; 9:42–47. ![]()
78. Silbernagel, KG, Thomeé, R, Thomeé, P, Karlsson, J, Eccentric overload training for patients with chronic Achilles tendon pain – a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports 2001; 11:197–206. ![]()
79. Sayana, MK, Maffulli, N, Eccentric calf muscle training in non-athletic patients with Achilles tendinopathy. J Sci Med Sport 2007; 10:52–58. ![]()
80. Rompe, JD, Nate, B, Fuira, JP, Maffulli, N, Eccentric loading, shock-wave treatment, or a wait-and-see policy for tendinopathy of the main body of the tendo Achilles: a randomized control trial. Am J Sports Med 2007; 35:374–383. ![]()
81. Rees, JD, Lichtwark, GA, Wolman, RL, Wilson, AM, The mechanism for efficacy of eccentric loading in Achilles tendon injury; an in vivo study in humans. Rheumatology (Oxford). 2008;47(10):1493–1497. ![]()
82. Subotnick, SI. Orthotic foot control and the overuse syndrome. Physician Sportsmed. 1975; 3(1):75–79.
83. James, SL, Bates, BT, Ostering, LR, Injuries to runners. Am J Sports Med. 1978;6(2):40–50. ![]()
84. Möller, MHC, Ekstrand, J, Oeberg, BE, Gillquist, J, Duration of stretching effect on range of motion in lower extremities. Arch Phys Med Rehabil 1985; 65:171–173. ![]()
85. Wiktorsson-Möller, M, Oeberg, B, Ekstrand, J, Gillquist, J, Effects of warming up, massage and stretching on range of motion and muscle strength in the lower extremity. Am J Sports Med 1983; 11:249–252. ![]()
86. Gerster, JC, Vischer, TL, Bennanin, A, Fallet, GH, The painful heel. Ann Rheum Dis 1977; 36:343–349. ![]()
87. Rask, MR, Achilles tendon disease owing to rheumatoid disease. JAMA. 1978;239(5):435–436. ![]()
88. Rodman, GP, McEwen, C, Wallace, SL. Primer on rheumatic diseases. JAMA. 1976; 224(suppl5):67–68.
89. Taunton, J, McKenzie, D, Clement, D, The role of biomechanics in the epidemiology of injuries. Sports Med 1988; 6:107–120. ![]()
90. Jozsa, L, The role of recreational sport activity in Achilles tendon rupture. Am J Sports Med 1989; 3:338–343. ![]()
91. Shields, CL, Kerlan, RK, Jobe, FW, et al, The Cybex II evaluation of surgically repaired Achilles tendon rupture. Am J Sports Med. 1978;6(6):369–372. ![]()
92. Kennedy, R, Inglis, J, Malcolm, L. Late reconstruction of the Achilles tendon. J Bone Joint Surg. 1979; 61A(6):653–658.
93. Rodineau, J. La Rupture du tendon d’Achille. Pratique Médicale. 1982.
94. Majewski, M, Rickert, M, Steinbruck, K, Achilles tendon rupture. A prospective study assessing various treatment possibilities. Orthopade. 2000;29(7):670–676. ![]()
95. Inglis, AE, Scott, WN, Sculco, TP, Patterson, AH, Ruptures of the tendo Achillis: an objective assessment of surgical and non-surgical treatment. J Bone Joint Surg 1976; 58A:990. ![]()
96. Jacobs, D, Martens, M, Van Audekercke, R, Comparison of conservative and operative treatment of Achilles tendon rupture. Am J Sports Med 1978; 6:107. ![]()
97. Percy, EC, Connochie, LB, The surgical treatment of ruptured Achilles tendon. Am J Sports Med 1978; 6:132. ![]()
98. Stein, SR, Leukens, CA, Closed treatment of Achilles tendon ruptures. Orthop Clin North Am 1976; 7:241. ![]()
99. Fruensgaard, S, Helmig, P, Riis, J, Stovring, JO, Conservative treatment for acute rupture of the Achilles tendon. Int Orthop. 1992;16(1):29–31. ![]()
100. Nistor, L, Surgical and non-surgical treatment of Achilles tendon rupture. J Bone Joint Surg 1981; 63A:394. ![]()
101. Carden, DJ, Rupture of the calcaneal tendon: the early and the late management. J Bone Joint Surg 1987; 69B:416–420. ![]()
102. Popovic, N, Lemaire, R, Diagnosis and treatment of acute ruptures of the Achilles tendon. Current concepts review. Acta Orthop Belg. 1999;65(4):458–471. ![]()
103. Lo, IK, Kirkley, A, Nonweiler, B, Kumbhare, DA, Operative versus nonoperative treatment of acute Achilles tendon ruptures: a quantitative review. Clin J Sport Med. 1997;7(3):207–211. ![]()
104. Gorschewsky, O, Vogel, U, Schweizer, A, van Laar, B, Percutaneous tenodesis of the Achilles tendon. A new surgical method for the treatment of acute Achilles tendon rupture through percutaneous tenodesis. Injury. 1999;30(5):315–321. ![]()
105. Ralston, EL, Schmidt, ER, Repair of the ruptured Achilles tendon. J Trauma. 1971;11(1):15–21. ![]()
106. Winter, E, Weise, K, Weller, S, Ambacher, T, Surgical repair of Achilles tendon rupture. Comparison of surgical with conservative treatment. Arch Orthop Trauma Surg. 1998;117(6–7):364–374. ![]()
107. Zell, RA, Santoro, VM, Augmented repair of acute Achilles tendon ruptures. Foot Ankle Int. 2000;21(6):469–474. ![]()
108. Cretnik, A, Kosanovic, M, Smrkolj, V, Percutaneous suturing of the ruptured Achilles tendon under local anesthesia. J Foot Ankle Surg. 2004;43(2):72–81. ![]()
109. Mertl, P, Jarde, O, Van, FT, et al, Percutaneous tenorrhaphy for Achilles tendon rupture. Study of 29 cases. Rev Chir Orthop Reparatrice Appar Mot. 1999;85(3):277–285. ![]()
110. Buchgraber, A, Passler, HH, Percutaneous repair of Achilles tendon rupture. Immobilization versus functional postoperative treatment. Clin Orthop 1997; 341:113–122. ![]()
111. Bring, DK, Kreicbergs, A, Renstrom, PA, Ackermann, PW, Physical activity modulates nerve plasticity and stimulates repair after Achilles tendon rupture. J Orthop Res. 2007;25(2):164–172. ![]()
112. Lea, RB, Smith, L, Non-surgical treatment of tendo Achilles rupture. J Bone Joint Surg 1972; 54A:1394. ![]()
113. Angermann, P, Hovgaard, D, Chronic Achilles tendinopathy in athletic individuals: results of nonsurgical treatment. Foot Ankle Int. 1999;20(5):304–306. ![]()
114. Singer, K, Jones, D. Soft tissue conditions of the ankle and foot. In: Nicholas J, Hershman E, eds. The Lower Extremity and Spine in Sports Medicine. St Louis: Mosby; 1986:418–425.
115. Fruensgaard, S, Helmig, P, Riis, J, Stovring, JO, Conservative treatment for acute rupture of the Achilles tendon. Int Orthop. 1992;16(11):33–35. ![]()
116. Fontenrose, A, Miller, J, Hallum, A, Physicians’ and physical therapists’ evaluation of cerebral-palsied children for Achilles tendon lengthening. Dev Child Neurol 1984; 26:208–214. ![]()
117. McGlamry, ED, Banks, AS. McGlamry’s Comprehensive Textbook of Foot and Ankle Surgery, 3. Philadelphia: Lippincott Williams & Wilkins; 2001.
118. Lamm, BM, Paley, D, Herzenberg, JE, Gastrocnemius soleus recession: a simpler, more limited approach. J Am Podiatr Med Assoc 2005; 95:18–25. ![]()
119. Hill, R, Ankle equinus: prevalence and linkage to common foot pathology. J Am Podiatr Med Assoc 1995; 85:295–300. ![]()
120. Heim, M, Blankstein, A, Congenital short Achilles tendon. Orthop Rev. 1992;21(1):105–107. ![]()
121. Trevino, S, Gibbs, M, Panchbhavi, V, Evaluation of results of endoscopic gastrocnemius recession. Foot Ankle Int 2005; 26:359–364. ![]()
122. Saxena, A, Widtfeldt, A, Endoscopic gastrocnemius recession: preliminary report on 18 cases. J Foot Ankle Surg 2004; 43:302–306. ![]()
123. O’Donoghue, DH. Treatment of Injuries to Athletes, 3rd ed. Philadelphia: Saunders; 1976.
124. Shah, S, Miller, B, Kuhn, J, Chronic exertional compartment syndrome. Am J Orthop. 2004;33(7):335–341. ![]()
125. Veith, RG, Matsen, FA, Newell, SG. Recurrent anterior compartmental syndromes. Physician Sportsmed. 8(11), 1980.
126. Arai, M, Endoh, H, Blood flow through human skeletal muscle, during and after contraction. Tohoku J Exp Med 1974; 114:379–384. ![]()
127. Schissel, DJ, Godwin, J, Effort-related chronic compartment syndrome of the lower extremity. Mil Med. 1999;164(11):830–832. ![]()
128. Reneman, RS. The Anterior and Lateral Compartment Syndrome of the Leg. Mouton: The Hague; 1968.
129. Harman, W, Significance of local vascular phenomena in ischaemic necrosis in skeletal muscle. Am J Path 1948; 24:625. ![]()
130. Humphries, D. Exertional compartment syndromes. Medscape Gen Med. 1999; 3:1–7.
131. Bong, M, Polatsch, D, Jazrawi, L, et al, Chronic exertional compartment syndrome: diagnosis and management. Hosp Joint Dis 2005; 62:77–84. ![]()
132. Mubarak, SJ, Hargens, AR, Owen, CA, et al, The wick catheter technique for measurement of intra-muscular pressure. A new research and clinical tool. J Bone Joint Surg 1976; 58A:1016–1020. ![]()
133. Pedowitz, RA, Hargens, AR, Mubarak, SJ, Hershuni, DH, Modified criteria for the objective diagnosis of chronic compartment syndromes of the leg. Am J Sports Med 1990; 18:35–40. ![]()
134. McQueen, M, Acute compartment syndrome. Acta Chir Belg. 1998;98(4):166–170. ![]()
135. Verleisdonk, EJ, van den Helder, CJ, Hoogendoorn, HA, van der Werken, C, Good results of fasciotomy in chronic compartment syndrome of the lower leg. Ned Tijdschr Geneeskd. 1996;140(50):2513–2517. ![]()
136. Simon, R, Sherman, S, Koenigsknecht, S. Compartment syndrome. Emergency orthopedics: the extremities. New York: McGraw Hill; 2007.
137. Wiggins, H, The anterior tibial compartment syndrome. A complication of the Hauser procedure. Clin Orthop 1975; 113:90–94. ![]()
138. Leach, RE, Corbett, M, Anterior tibial compartment syndrome in soccer players. Am J Sports Med. 1979;7(4). ![]()
139. Duflo, F, Allaouchiche, B, Mathon, L, Chassard, D, Bilateral anterior tibial compartment syndrome from prolonged surgery in the lithotomy position. Ann Fr Anesth Reanim. 1999;18(7):779–782. ![]()
140. Blackman, PG, A review of chronic exertional compartment syndrome in the lower leg. Med Sci Sports Exerc. 2000;32(3 suppl):S4–S10. ![]()
141. Schepsis, AA, Gill, SS, Foster, TA, Fasciotomy for exertional anterior compartment syndrome: is lateral compartment release necessary? Am J Sports Med. 1999;27(4):430–435. ![]()
142. Kitajima, I, Tachibana, S, Hirota, Y, et al, One-portal technique of endoscopic fasciotomy: chronic compartment syndrome of the lower leg. Arthroscopy. 2001;17(8):1. ![]()
143. Swierstra, JCC, Klasen, HJ. Het tibialis anteriorsyndroom. Geneeskd Sport. 1970; 2(3):45–46.
144. Sheridan, GW, Matsen, FA, Fasciotomy in the treatment of the acute compartmental syndrome. J Bone Joint Surg 1976; 58A:112–115. ![]()
145. Conti, SF, Posterior tibial tendon problems in athletes. Orthop Clin North Am. 1994;25(1):109–121. ![]()
146. Devereaux, MD, Parr, GR, Lachman, SM, et al, The diagnosis of stress fractures in athletes. JAMA 1984; 252:531–533. ![]()
147. Batt, ME, Ugalde, V, Anderson, MW, Shelton, DK, A prospective controlled study of diagnostic imaging for acute shin splints. Med Sci Sports Exerc. 1998;30(11):1564–1571. ![]()
148. Anderson, MW, Ugalde, V, Batt, M, Gacayan, J, Shin splints: MR appearance in a preliminary study. Radiology. 1997;204(1):177–180. ![]()
149. Jackson, D. Shinsplints: an update. Phys Sports Med. 1978; 6:51–61.
150. American Medical Association. Standard Nomenclature of Athletic Injuries. Chicago: American Medical Association; 1976.
151. Bronfort, G, Haas, M, Evans, R, et al, Effectiveness of manual therapies: the UK evidence report. Chiropr Osteopat 2010; 18:3. ![]()
152. Kortebein, P, Kaufman, K, Basford, J, Stuart, M, Medial tibial stress syndrome. Med Sci Sports Exerc. 2000;32(3 suppl):S27–S33. ![]()
153. Prather, JC, Nuzynowitzi, ML, Snody, AJ, et al. Scintigraphic findings in stress fractures. J Bone Joint Surg. 1977; 59A:896.
154. Gilaldi, M. Comparison between radiography, bone scan and ultrasound in the diagnosis of stress fractures. Milit Med. 1984; 149:459–461.
155. Holder, LE, Radionuclide bone-imaging in the evaluation of bone pain. J Bone Joint Surg 1982; 64A:1391–1396. ![]()
156. Young, A, McAllister, D, Evaluation and treatment of tibial stress fractures. Clin Sports Med. 2006;25(1):117–128. ![]()
157. Mann, RA, Thompson, F, Rupture of the posterior tibial tendon, causing flat foot. J Bone Joint Surg 1985; 67A:556–561. ![]()
158. Frey, CC, Shereff, MJ, Tendon injuries about the ankle in athletes. Clin Sports Med 1988; 7:103–118. ![]()
159. Johnson, KA, Tibialis posterior tendon rupture. Clin Orthop Rel Res 1983; 117:140–147. ![]()
160. Funk, DA, Cass, JR, Johnson, KA, Acquired adult flat foot secondary to posterior tibial tendon pathology. J Bone Joint Surg 1986; 68A:95–102. ![]()
161. Ness, ME, Long, J, Marks, R, Harris, G, Foot and ankle kinematics in patients with posterior tibial tendon dysfunction. Gait Posture. 2008;27(2):331–339. ![]()
162. Tome, J, Nawoczenski, DA, Flemister, A, Houck, J, Comparison of foot kinematics between subjects with posterior tibialis tendon dysfunction and healthy controls. J Orthop Sports Phys Ther. 2006;36(9):635–644. ![]()
163. Kulig, K, Reischl, SF, Pomrantz, AB, et al, Nonsurgical management of posterior tibial tendon dysfunction with orthoses and resistive exercise: a randomized controlled trial. Phys Ther. 2009;89(1):26–37. ![]()
164. Hansen, ST, Clark, W, Tendon transfer to augment the weakened tibialis posterior mechanism. JAMA 1988; 78:309–402. ![]()
165. Mendicino, SS, Quinn, M, Tibialis posterior dysfunction: an overview with a surgical case report using a flexor tendon transfer. J Foot Surg 1989; 28:154–157. ![]()
166. Sammarco, GJ, Peroneal tendon injuries. Orthop Clin North Am. 1994;25(1):135–145. ![]()
167. Jackson, MA, Gudas, CJ, Peroneus longus tendinitis: a possible biomechanical etiology. J Foot Surg. 1982;21(4):344–348. ![]()
168. Anderson, E, Stenosing peroneal tenosynovitis symptomatically simulating ankle instability. Am J Sports Med 1987; 157:258–260. ![]()
169. Sammarco, GJ, DiRaimondo, CV, Chronic peroneus brevis tendon lesions. Foot Ankle. 1989;9(4):163–170. ![]()
170. Bisschop, P, Deconinck, R, Ombregt, L, Van de Velde, T. Workbook for the Cyriax Course in Orthopaedic Medicine. De Haan: Belgian Scientific Society of Orthopaedic Medicine; 1986.
171. McLennon, JG, Treatment of acute and chronic luxations of the peroneal tendons. Am J Sports Med 1980; 8:422–436. ![]()
172. Stover, CN, Bryan, DR, Traumatic dislocation of the peroneal tendons. Am J Surg 1962; 103:180–186. ![]()
173. Martens, MA, Noyez, JF, Mulier, JC, Recurrent dislocation of the peroneal tendons. Results of rerouting the tendons under the calcaneofibular ligament. Am J Sports Med. 1986;14(2):148–150. ![]()
174. Das De, S, Balasubramaniam, P, A repair operation for recurrent dislocation of peroneal tendons. J Bone Joint Surg. 1985;67B(4):585–587. ![]()
175. Ferran, NA, Maffulli, N, Oliva, F, Management of recurrent subluxation of the peroneal tendons. Foot Ankle Clin. 2006;11(3):465–474. ![]()
176. Guarantors of Brain. Aids to the Examination of the Peripheral Nervous System. London: Baillière Tindall; 1986.
177. Brügger, A. Die Erkrankungen des Bewegungsapparates und seines Nervensystems. Stuttgart: Gustav Fisher; 1980.