Disorders of the inert structures
Ligaments
Introduction
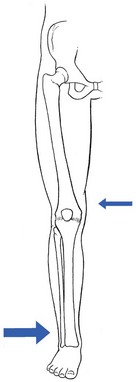
Ligamentous lesions at the knee are quite common. The joint is relatively uncovered by muscles, which makes it vulnerable to direct injury. Furthermore, the indirect forces acting on the knee have a large leverage, whereas the active and passive stabilizers of the joint have only a small leverage (Fig. 53.1) and thus give very inadequate protection.
We firmly believe that immobilization is never a good method. If there is a serious grade III lesion (see below) in a young athlete and instability is feared, the patient should be sent for surgery. If, for one reason or another, the patient is not treated surgically, early mobilization, deep transverse friction and functional treatment should be used. This treatment regime gives the needed physiological stimulus for quick and proper healing of the lesion and prevents the formation of adhesions, so often the cause of persistent trouble.1
Classification
Ligamentous injuries can also be classified according to which structure has been damaged. The commonest injuries are at the medial collateral and the anterior cruciate ligaments. Sometimes these occur together and in combination with a torn medial meniscus – the ‘unhappy triad’, or the triad of O’Donoghue2,3 – or in combination with a tear of the lateral meniscus.4 Lesions at the lateral collateral ligament and the posterior cruciate ligament are rare. In our experience, tears at the medial coronary ligament are very common; however, these are often misdiagnosed as medial collateral tears or meniscus lesions.
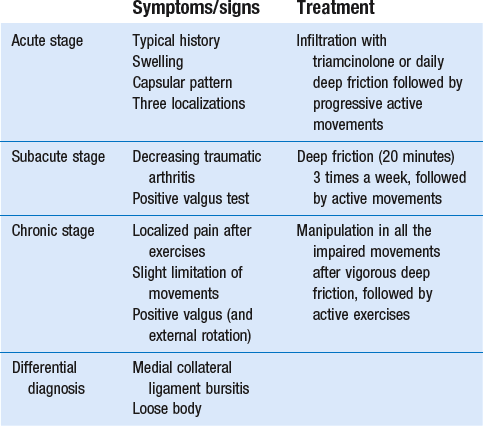
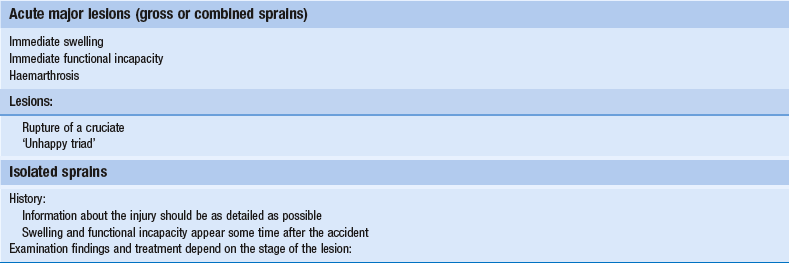
This temporal division is important in choice of treatment (Table 53.1).
Table 53.1
Classification of ligamentous injuries according to severity, structure and time
| Severity | Structure | Time |
| Grade I: slight overstretching | Isolated sprain | Acute: less than 2 weeks |
| Grade II: partial tear | Combined sprains | Subacute: between 2 and 6 weeks |
| Grade III: complete tear | In combination with meniscal tears | Chronic: more than 6 weeks |
Diagnosis
Even in the era of arthroscopy, a clinical approach to ligamentous lesions continues to be vital.
In the acute stage, information obtained from the history and clinical examination enables the examiner to make the distinction between serious and mild lesions. If symptoms and signs warrant, the patient is then referred for further assessment by arthroscopy.5
History
It is vital to obtain a very detailed history of the mechanism that has led to the injury, as summarized in Box 53.1, especially in acute sprains of the knee.
• The injury: at the moment of injury, what was the position of the knee, what forces acted where on the knee and in which directions were they applied?
• The initial symptoms: what was the immediate result of the trauma? Where was the initial pain? Was there immediate swelling? Was there immediate functional incapacity caused by locking or instability or could the patient continue activities? Did pain, swelling and functional disability appear only after a certain lapse of time?
• The evolution: what was the evolution of pain, swelling and disability after the first few days?
• Treatment received: what sort of treatment did the patient receive and what was the result?
In long-standing cases, the current symptoms should be ascertained:
Examination
The functional examination described in Chapter 50 is carried out.
In acute cases, the ligamentous tests will sometimes be overshadowed by the capsular pattern of the traumatic arthritis, which makes it very difficult to estimate the degree of damage. In subacute and chronic cases, the capsular signs have largely subsided and the tests of ligamentous integrity become more informative. Sometimes, laxity is found during the routine examination, in which case instability tests are then carried out (see online chapter Disorders of the inert structures: ligamentous instability). Sometimes, it is not so much instability but rather pain and limitation of a non-capsular type that are detected; these indicate the formation of adhesions around the healed tissue.
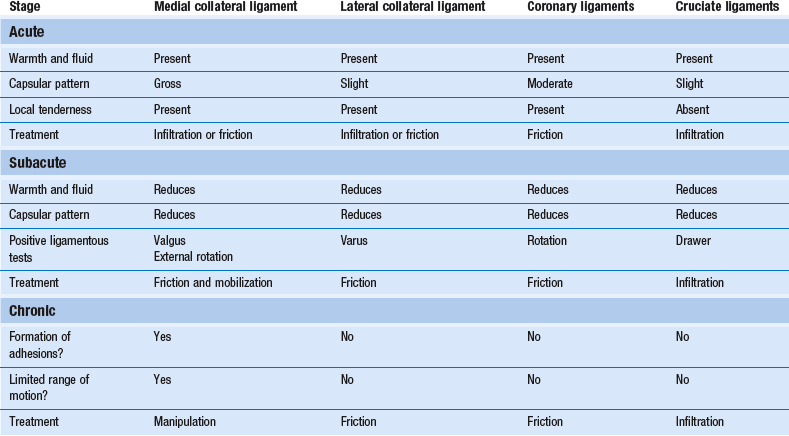
Acute ligamentous lesions
In acute ligamentous lesions at the knee, the history will be what first indicates severity. A few hours after a serious sprain, the knee will start to hurt considerably and develop a distinct capsular pattern, protected by muscle spasm that makes it almost impossible to perform ligamentous tests. In order to distinguish between a serious injury and a less important lesion, a number of elements gained from the history may be of value (Table 53.2).
Table 53.2
Acute ligamentous lesions: contrasting histories of serious and less serious lesions
| Serious lesions | Less serious lesions | |
| Impairment of function | Immediate inability to continue the sport or activity | Most initial pain disappears and sports and activities can be continued after a short time |
| Swelling | Immediate or developing during the first hour, indicating haemarthrosis5 | Appears a few hours after the accident, with functional incapacity and generalized pain |
| Feeling of instability? | Yes | No |
| Aspiration | Blood may be present | Clear fluid is obtained |
| Possible diagnoses | Triad of O’Donoghue? Isolated rupture of a cruciate ligament? |
Isolated sprain of a collateral, coronary or cruciate ligament |
Chronic ligamentous lesions
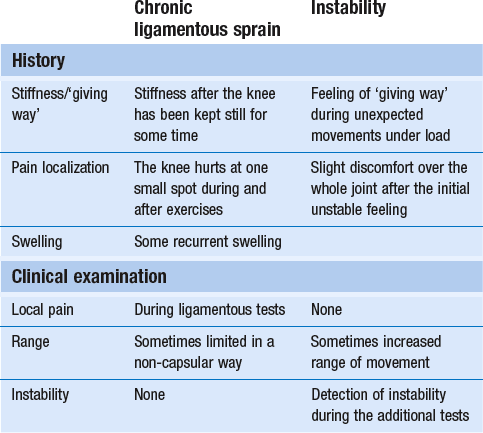
Because the treatment is quite different, it is vital to differentiate between instability as the result of a total ligamentous rupture and chronic ligamentous adhesions leading to a ‘self-perpetuating inflammation’. Once again, history and clinical examination are the first approach to differentiate between these conditions and, in instability, to estimate its degree (Table 53.3).
Instability is characterized by a sensation of ‘giving way’ during unexpected movements under load. There may be accompanying pain and discomfort, sometimes lasting for a day or two. Additional instability tests will usually detect the type and degree of ligamentous insufficiency (see online chapter Disorders of the inert structures: ligamentous instability).
Treatment: the principle of early mobilization
Experimental studies over the past few decades have demonstrated that regeneration of injured connective tissue is significantly better with the application of continuous passive motion. Under functional load, the collagen fibres are oriented in a longitudinal direction and the mechanical properties are optimized.6 Therefore, functional conservative treatment is advised for all coronary ligament sprains and all isolated grade I, II or III sprains of the medial collateral ligament7 and posterior cruciate ligament and isolated grade I or II lesions of the anterior cruciate ligament.8 However, in combined lesions and in anterior cruciate ligament tears with a positive pivot shift phenomenon, surgery is the treatment of choice.9
Mobilization not only is the best promoter of ligamentous repair but also prevents ligamentous adhesions within or around the healing structure. Another advantage of early mobilization is the positive effect on muscle strength10 and proprioceptive reflexes,11 which ensures the active stability of the joint.
This conservative and functional approach to recent and isolated tears was first advocated by Cyriax12 and has recently received much support. Several studies have demonstrated that the non-operative management of an isolated medial collateral ligament injury, especially of grade I and II, is as good as, if not better than, a primary surgical approach.13–18 The conservative treatment of grade III sprains of the medial collateral ligaments also gives results that are equally as good as the surgical approach but with significantly quicker rehabilitation.19–21 Jones et al22 treated 24 high-school football players with an isolated grade III injury of the medial collateral ligament. They administered mobilization, using a regime of muscle strengthening and agility exercises. Knee stability was achieved in 22 cases, with an average recovery time of 29 days. The players returned to competitive sport after a mean of 34 days. Similar results were obtained in a long-term study of 21 grade III medial collateral ligament tears.23 The overall conclusion was that non-surgical treatment of a complete tear of the medial collateral ligament was extremely successful, provided there was no associated structural damage to the anterior cruciate ligament.
• Relieve the inflammation and pain as soon as possible so the patient can mobilize the knee. This can be achieved by local infiltration of a small amount of triamcinolone.
• As advised by Cyriax, mobilize the ligament over the bone by deep transverse friction instead of moving the bone under the ligament as in ordinary mobilizations. The relative movement will be the same, as is the mechanical stimulus to the regenerating fibrils.
Isolated sprains
Medial collateral ligament
The medial collateral ligament prevents valgus deviation of the knee and, through its posterior fibres, checks external rotation of the tibia.24 An understanding of this is of importance in the interpretation of clinical tests in a torn medial collateral ligament.25
Diagnosis
The medial collateral ligament is the most commonly injured ligamentous structure of the knee. The classic mechanism of injury is a forced valgus movement on a partly flexed and externally rotated knee,26 which typically occurs when a soccer or American football player receives a kick or blow at the outer side of the weight-bearing knee.27 The patient experiences a crack and feels sudden pain at the inner aspect of the knee. Most of the pain disappears fairly quickly and the sportsman or woman can probably return to the game or walk off the pitch. At first, the knee is not swollen and there is only slight disability. The real incapacity, with increasing swelling and pain, starts after a few hours. By the next day, the patient can hardly stand and can only hobble with assistance.
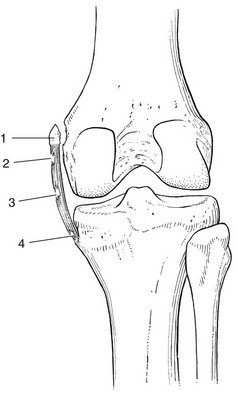
The tear can be proximal, be related to the mid-portion of the ligament or be situated at the distal, tibial portion (Fig. 53.2). Mid-portion tears are the most common, but also the most disruptive, because they also involve the deeply situated meniscotibial and meniscofemoral portions of the ligament.28 In a proximal tear, it is wise to perform radiography to exclude avulsion of a bony fragment, which is an indication for surgical repair.29,30
• There has been good healing, with a strong non-adherent ligament.
• The ligament is permanently lengthened, resulting in an unstable knee.
• The ligament is adherent, leaving the patient with recurrent and localized disability.
Stieda–Pellegrini disease
Sometimes calcification of the medial collateral ligament develops after an apparently ordinary sprain of the inner side of the knee. Suspicion arises when increasing limitation of flexion, together with a hard end-feel, is found 4–6 weeks after the accident. Radiography shows ossification along the inner side of the medial femoral condyle.31
Conservative treatment is ineffective but good results have been reported with surgical treatment.32 Spontaneous recovery takes 6 months to 1 year.33
Treatment
All grade I and grade II sprains (partial tears), as well as isolated grade III sprains (complete tears) of the medial collateral ligament should be treated conservatively. Surgery is indicated only in combined lesions of medial collateral ligament and meniscus and/or anterior cruciate ligament.34
The technique chosen depends on the stage of the lesion, as summarized in Box 53.2. If the patient is seen during the first 24 hours after the accident, local infiltration with triamcinolone can be considered. Deep transverse friction in combination with early mobilization can be applied during the first 6 weeks following the accident. If the patient is seen after more than 6 weeks, the lesion must be considered as chronic and manipulation is given.
Acute stage
Infiltration and cold compression
During the next 24 hours, the patient remains in bed with an ice bag on the affected area. From the second day on, flexion is strongly encouraged, as is extension without weight bearing. During the first week, however, no attempt should be made to straighten the knee completely on walking; the medial collateral ligament is taut in extension and too much stretching at the point of injury would cause harm. On account of the anti-inflammatory effect of the triamcinolone, pain and swelling abate very quickly and normal gait is restored after 1–2 weeks. Walking and modest movement of the knee should be encouraged because they provide the best stimulus to normal healing and prevent the formation of adhesions. The patient can usually return to sports after 6 weeks.35 By that time, movements are of full range and ligamentous tests negative. It is wise to recommend a protective knee brace during the first few weeks of sporting activity, especially if the patient returns to contact sports.
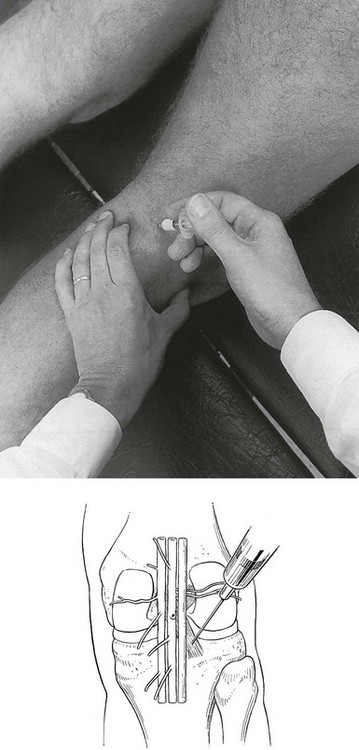
Technique: infiltration
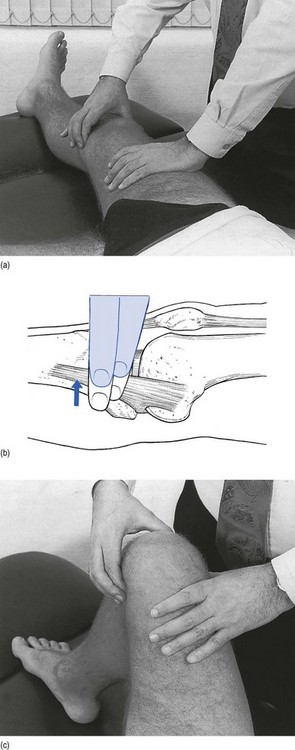
The patient lies supine, with a pillow under the knee. The physician, standing at the inner side of the knee, outlines the correct area. A fine needle is fitted to the syringe, filled with a mixture of 1 mL of lidocaine 2% and 20 mg of triamcinolone. The needle is thrust in almost horizontally (Fig. 53.3) and the whole tender area is infiltrated by a series of small droplets.
Friction
Friction serves a double purpose: it prevents any fibrils from binding the ligament to bone and applies a positive stimulus to the healing connective tissue. As, in the acute stage, adhesions will not yet have formed, just 2 minutes of deep friction are required in both flexion and extension, though the preparatory phase of gentle massage, followed by slight superficial friction (which renders the ligament anaesthetized), may take up to 20 minutes. The patient is given this deep friction every day during the first week, after which the subacute stage is entered. If the massage is given adequately, the range of flexion increases dramatically during the first few days. The patient should be encouraged to walk and to move actively, although straightening the last 20° or flexing the last 60° must be avoided during the first week because these movements put too much longitudinal strain on the ligament.36 The joint can be protected with a partial mobile brace, the coronal straps of which prevent excessive valgus movement.37
Technique: deep friction
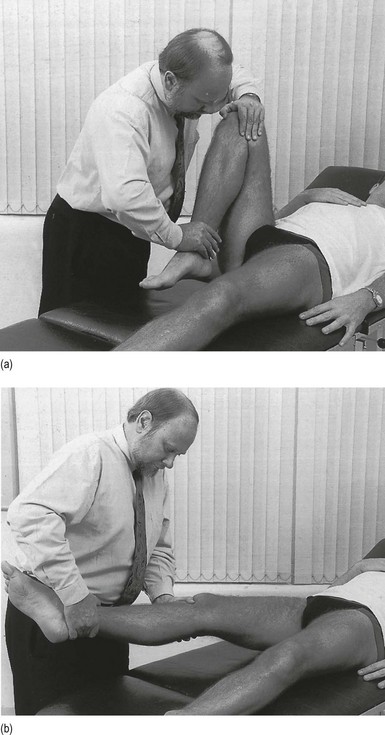
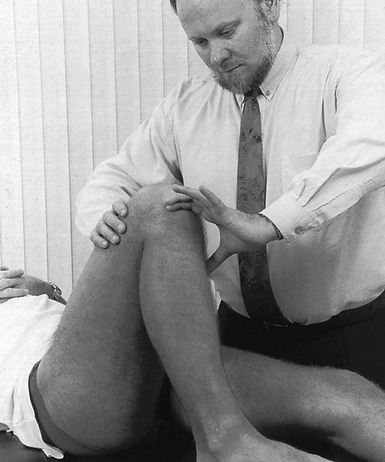
The patient lies supine on the couch and the exact point is identified. Friction is first given in as much extension (![]() ) as possible, then in as much flexion (
) as possible, then in as much flexion (![]() ) as possible. The therapist places the index finger at the exact point, which is most often the central part of the ligament at the joint line. The index finger is reinforced by the middle finger, and the thumb is placed at the outer side of the joint so that it can be used as a fulcrum (Fig. 53.4). Friction is imparted by an extension movement at the wrist, which draws the index finger anteriorly over the ligament. Releasing the grip and flexion of the wrist moves the index finger back to the starting position.
) as possible. The therapist places the index finger at the exact point, which is most often the central part of the ligament at the joint line. The index finger is reinforced by the middle finger, and the thumb is placed at the outer side of the joint so that it can be used as a fulcrum (Fig. 53.4). Friction is imparted by an extension movement at the wrist, which draws the index finger anteriorly over the ligament. Releasing the grip and flexion of the wrist moves the index finger back to the starting position.
Subacute stage
In the subacute stage, massage is given more thoroughly and for longer, applying the same technique as described for the acute stage (see Fig. 53.4). By moving the ligament across the bone, the normal movement of bone over ligament is mimicked. Immediately after the massage, gentle movements in flexion, extension and external rotation are carried out by the therapist (passive movement). In order to prevent atrophy of the thigh muscles, a programme of resisted exercises should also be followed. Treatment three times a week for two weeks usually suffices for full recovery. Return to competitive sports is allowed only when running ability has returned to normal. This may take up to 6 weeks.38
Chronic stage
When the patient is first seen in the chronic stage, adhesions have already formed between the ligament and bone – a situation that would never have been reached if the patient had received proper treatment from the start, but which is often encountered when the knee has been immobilized. The principle of treatment is to restore a full range of movement by rupturing the abnormal adhesions. In order to do so, vigorous deep friction to the affected part of the ligament is applied for 20 minutes: 10 minutes in as much flexion as possible and 10 minutes in as much extension as possible (see Fig. 53.4). This massage anaesthetizes the affected tissue. Manipulation in all the impaired directions is now performed. It is important for the manipulations to be within normal physiological limits; attempting to overstretch the medial collateral ligament has no part in restoration of range at the knee joint, as it would create instability.
Manipulation techniques
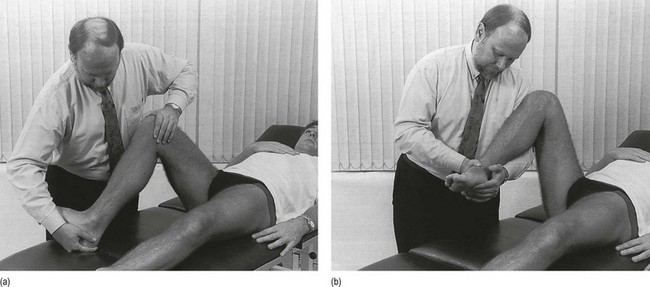
Manipulation in flexion
The patient lies supine or adopts a half-lying position on the couch. The hip is bent and the knee flexed as far as it will go. The therapist presses the ipsilateral hand just above the ankle. The other hand is placed on the knee (Fig. 53.5a), with the fingers on the ligament to feel the ‘tearing’ during the manipulation. The slack is taken up at the end of flexion and the tibia is forced vigorously backwards to the end of range. A snap is heard, which demonstrates the tearing of the adhesions.
Manipulation in extension
The patient lies supine on the couch, the knee extended as far as possible. The therapist stands to the side, level with the knee. The ipsilateral hand supports the heel and the other hand encircles the knee, just below the patella (Fig. 53.5b). The knee is slightly flexed and suddenly moved into full extension with a strong, quick jerk. A tiny snap is heard, which indicates that the adhesion has broken.
Manipulation in lateral (external) rotation
The patient adopts the half-lying position, with the hip flexed and the knee at 90°. The therapist stands level with the patient. The ipsilateral hand is clasped behind the heel, which rests on the couch. The foot is dorsiflexed, the inner side against the therapist’s forearm. The contralateral hand is used to stabilize the knee and the femur (Fig. 53.6a). Lateral rotation is now easily performed by using the foot as a lever. The slack is taken up at the end of range and the manipulation performed by a quick adduction movement of the shoulder.
Manipulation in medial (internal) rotation
It is unusual for an adhesion of the medial collateral ligament to cause pain on medial rotation. If it does, this technique is used. The patient adopts a half-lying position, with the hip and knee well flexed. The therapist stands at the affected side, level with the thigh, and encircles the heel with both hands. The contralateral hand clasps the inner side of the foot, while the arm passes behind the leg and supports it (Fig. 53.6b).
Lateral collateral ligament
Treatment
Technique: deep friction
The patient lies supine, the knee in extension. The therapist sits on the opposite side. The index finger, reinforced by the middle finger, covers the affected part of the ligament. The thumb is placed at the inner side of the knee, to be used as a fulcrum (Fig. 53.7). Via alternate flexion and extension of the wrist, the forefinger will be moved to and fro over the ligament, while the thumb is kept still. In a recent injury, when there is a lot of local tenderness, a gradual start to the friction is necessary – preparing the area for the 2 minutes of thorough friction which is required. In chronic cases, 20 minutes’ friction may be necessary, three times a week, for about 2 weeks.
Coronary ligaments
Cyriax39 was the first to draw attention to sprains of the coronary ligaments, which are very common but mostly go undiagnosed because the localization of the pain and nature of the onset resemble a meniscus lesion or a sprain of the medial collateral ligament. Recently, magnetic resonance imaging (MRI) examination40,41 and arthroscopy42 have confirmed the existence of coronary ligament lesions. The treatment is simple but effective and the injury is usually cured after 1 or 2 weeks’ deep friction or after one infiltration. Without treatment, the lesion recovers spontaneously in about 3 months, although in some cases it can persist indefinitely.
Differential diagnosis, history and examination
The differential diagnosis from a meniscal lesion is extremely important and once again relies almost entirely on history and clinical examination. In our opinion, it is unwise to refer a patient for arthroscopy before a lesion of the coronary ligament has been excluded. Meniscal lesions are so common that certainly not all cause symptoms.43,44 Although arthroscopy detects meniscus tears with almost 100% accuracy, it does not necessarily follow that the detected tears are the cause of the patient’s symptoms.45 The differential diagnosis between a meniscus lesion and a coronary ligament sprain is thus made on information gained from the history and clinical examination.
Treatment
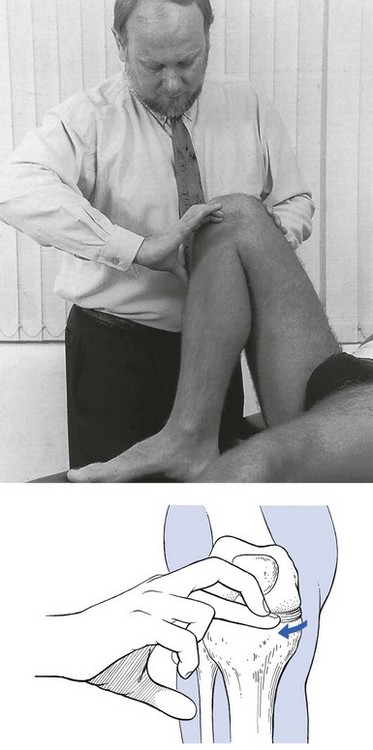
Technique: friction to the medial coronary ligament
The thumb is placed at the lateral side of the knee, where it is used as a fulcrum. The therapist ensures a vertical downward pressure of the index finger by placing the thumb as distally as possible on the leg. Massage is now given by drawing the fingertip horizontally along the condyle, around the fixed thumb (Fig. 53.8). As usual, there is an active phase of sweeping the index finger anteriorly and a relaxing phase when the finger is moved backwards to the previous position. In order to give sufficient excursion to the fingertip, the therapist should not sit or stand too close to the patient, so that the entire arm, elbow and wrist can be moved during the massage.
Technique: friction to the lateral coronary ligament
The technique is the same as described for the medial coronary ligament but the therapist stands on the opposite side of the damaged knee. The well-bent knee is now brought into inward rotation. Friction is performed by the contralateral hand. Once again, the fingertip of the index finger is placed horizontally on the affected ligament. The thumb now lies downwards on the inner side of the knee and acts as a fulcrum (Fig. 53.9). Friction is given by a movement of the whole arm, drawing the index finger along the tibial condyle.
Technique: infiltration of the medial (lateral) coronary ligament
The knee is well bent and brought into lateral (medial) rotation. The tibial condyle is identified and the site of the lesion ascertained. A small, thin needle is fitted to a 1 mL syringe, filled with 10 mg of triamcinolone and inserted from above until it hits bone. A series of small droplets are injected all over the tender area (Fig. 53.10).
Anterior cruciate ligament
An isolated tear of the anterior cruciate ligament may be caused by a hyperextension strain combined with medial rotation.46 Alternatively, the ligament may tear when the knee is loaded in valgus position, with the femur internally rotated and the pivot shifted to the lateral femorotibial compartment.47 Both situations occur frequently in soccer, basketball and volleyball, when an athlete decelerates, pivots/turns quickly or lands heavily from a jump.48 Combined lesions of the anterior cruciate and medial collateral ligaments, together with a torn meniscus, occur in contact sports (e.g. rugby, American football and judo).49,50 It has also been demonstrated that chronic anterior cruciate deficiencies can result from longitudinal meniscal tears.51,52
Diagnosis
Immediate swelling after the injury indicates haemarthrosis, which suggests a complete rupture of the ligament.53–55 In moderate sprain, only mild traumatic arthritis may result. Blood is a strong irritant to capsule and cartilage,56 and should be removed at once. If the patient is an athlete competing in a high-performance sport, arthroscopic assessment of the integrity of the anterior cruciate ligament must always follow the detection of a traumatic haemarthrosis. Alternatively, the patient is referred for MRI examination because this technique has become the imaging method of choice to evaluate the integrity of the anterior cruciate ligament.57
Sometimes a sprain leads to permanent lengthening, resulting in serious instability. The problem of instability is discussed later but it is as well to remember that lengthening of the anterior cruciate ligament, or even complete rupture, does not always lead to permanent functional instability.58–60 For its anterior stability, the knee depends not only on the anterior cruciate ligament but also on the capsular ligaments, the integrity of the menisci and good proprioceptive reflexes from the quadriceps and hamstring muscles.61 Messner and Maletius re-examined 22 patients with minor knee instability caused by partial rupture of the anterior cruciate ligament after a mean of 12 years and found excellent knee function that showed no differences from that of a control group.62
Treatment
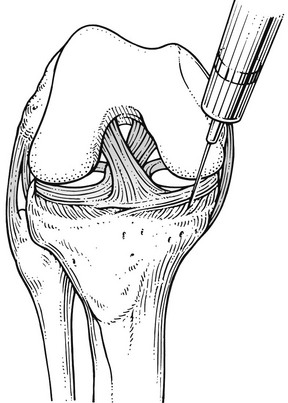
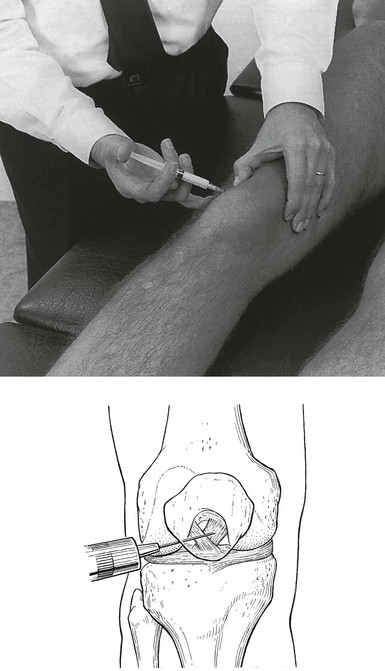
Technique: infiltration of the anterior end of the anterior cruciate ligament
The patient lies on the couch, with the knee bent at a right angle. The border of the medial tibial condyle is identified, together with the medial side of the patella and the infrapatellar tendon. A point is chosen just medial to the inferior edge of the patella, about 3 cm above the tibial rim. A 5 cm long needle is introduced here, in a backward and medial direction, aiming at the spine of the tibia (Fig. 53.11). The needle must cross dense tissue before it touches bone. If bone is hit immediately, this indicates that the needle does not lie within the ligament. If the correct position is reached, an area 1 cm2 is infiltrated with 20 mg of triamcinolone, by means of a series of small withdrawals and reinsertions. It is important to note that the infiltration must be made only at the ligamentoperiosteal junction, which is when the tip of the needle hits bone.
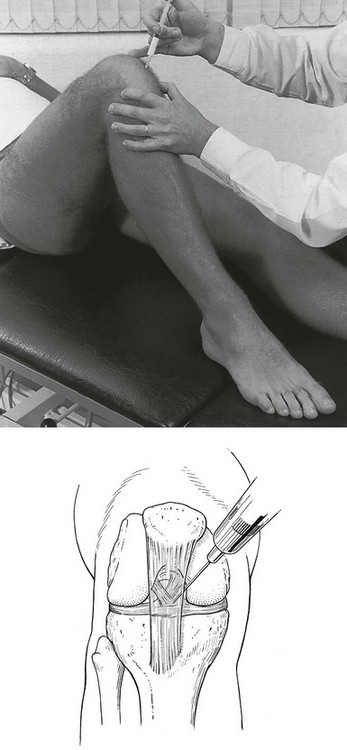
Technique: infiltration of the posterior end of the anterior cruciate ligament
The patient lies prone, with the knee extended. The medial and lateral femoral condyles form the landmarks. The free thumb is placed on the lateral condyle. The femoral attachment of the anterior cruciate ligament lies at the medial surface of the lateral condyle. It cannot be reached by a downward thrust and the needle must be brought in from a medial aspect, using an almost horizontal insertion. A 6 cm long needle is inserted at the apex of the medial condyle and moved at an angle of 30° to the horizontal in the direction of the lateral condyle. This approach ensures that the needle passes well posterior to the popliteal vessels (Fig. 53.12). The needle has to penetrate a tough ligamentous structure before it touches bone. The infiltration is given via a series of small droplets at different spots of the tenoperiosteal junction.
Posterior cruciate ligament
A severe lesion of the posterior cruciate ligament is always serious because the ligament creates the axis about which the knee rotates.63
Furthermore, most patients with posterior cruciate ligament injuries have combined ligamentous and/or chondral knee damage.64 Therefore, complete rupture of the ligament will often lead to considerable instability and limited function of the knee.65
A mild, isolated sprain at the tibial or femoral insertion, however, does not lead to gross instability.66 Nevertheless, it can induce persistent problems due to the formation of painful, self-perpetuating inflammation.
In this section we deal with mild sprains only. Complete and/or combined ruptures of the posterior cruciate ligament are discussed in the online chapter Disorders of the inert structures: ligamentous instability. A severe lesion should always be suspected if haemarthrosis is present. Escape of blood through a rupture of the posterior capsule may mask this sign.
Diagnosis
Motor vehicle accidents are the most common cause of injury, but sports-related trauma (football, skiing) has increased in recent years. The usual mechanism of injury in motor vehicle accidents is a ‘dashboard’ injury: during a car crash the femur is forced forwards on the immobilized tibia.67 Sports-related injuries result from severe hyperextension of the knee or from hyperflexion with the foot typically plantarflexed. The latter mechanism is the most common cause of isolated posterior cruciate ligament injuries.68
During the first few days after the accident, examination shows traumatic arthritis, with a warm and swollen knee containing clear fluid. Tests for the collateral ligaments are negative but internal rotation can be painful at the end of range. The posterior drawer test demonstrates pain rather than laxity. Shearing the tibia laterally on the femur is also painful, as is resisted flexion with the knee in a 90° flexed position. As a rule, the lesion lies at the tibial border. Sometimes a small bony chip may be avulsed and is visible on a plain radiograph.69
During the last few decades, MRI has proven to be very accurate in the diagnosis of posterior cruciate ligament lesions and in demonstrating associated injury.70–72
Treatment
Treatment of posterior cruciate ligament lesions depends on their severity, the existence of concomitant lesions and the presence and degree of laxity.73,74 Isolated, partial posterior cruciate ligament injuries (grades I and II) are best treated non-operatively, while complete injuries (grade III) may require operative treatment based on clinical features. All combined ligamentous injuries usually respond best to surgical management. In recent years, several studies have demonstrated that knees with an isolated injury to the posterior cruciate ligament, without concomitant articular damage, may be successfully managed conservatively and that the majority of athletes with isolated posterior cruciate ligament injuries who maintain muscle strength return to sports without any functional disability.75–78
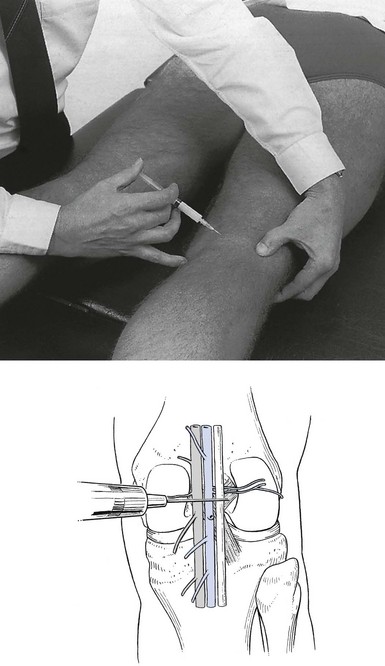
Technique: infiltration of the posterior end of the posterior cruciate ligament
The patient lies prone, with the knee extended. The landmarks here are the lateral femoral condyle – which is easily identified – the popliteal artery and the posterior margin of the tibia. The latter cannot be palpated directly and must be marked by palpation of the joint line at the anterolateral side. The level of the posterior edge of the tibia can then be estimated. The posterior end of the posterior cruciate ligament is at the mid-point of the tibia, extending somewhat to the lateral side. A 5 cm long needle is inserted at the apex of the lateral femoral condyle, about 2 cm above the estimated level of the tibial surface and directed inferiorly and medially, at about 60° to the horizontal. The palpating index finger is placed on the popliteal artery and the joint line. The lateral approach, together with palpation of the artery, avoids the popliteal vessels. The tip of the needle is advanced until the characteristic feel of a ligament is encountered before bone is felt (Fig. 53.13). If the needle passes without obstruction and hits cartilage, this indicates that it has passed into the knee joint. This is too far proximal and the tip should be moved in a more oblique direction until it penetrates ligament and then touches bone. This is the exact area sought, just below the articular edge of the tibia. Infiltration of 20 mg of triamcinolone should be given here by means of a series of small insertions and withdrawals along the mediolateral borders.
Technique: infiltration of the anterior end of the posterior cruciate ligament
The patient lies supine, with the knee extended. The medial and lateral femoral condyles are identified. The anterior end of the ligament lies at the lateral surface of the medial condyle and is covered by the patella, so that direct access from above is not possible. The physician has to move the patella as far as possible medially and upwards by tilting the outer edge with the thumb. A 5 cm long needle is now inserted just under the inferolateral edge of the patella, and pushed up in the direction of the medial condyle, until it hits bone (Fig. 53.14). It is then moved little by little, until ligamentous resistance is felt. A series of small droplets are injected when the needle is felt to touch bone after piercing the ligament.
Ligamentous lesions of the knee are summarized in Table 53.5.
References
1. Hardy, MA, The biology of scar formation. Phys Ther 1989; 69:1014–1023. ![]()
2. O’Donoghue, DH, Surgical treatment of fresh injuries to the major ligaments of the knee. J Bone Joint Surg 1950; 32A:721–738. ![]()
3. O’Donoghue, DH, Treatment of acute ligamentous injuries of the knee. Orthop Clin North Am 1973; 4:617. ![]()
4. Shelbourne, KD, Nitz, PA, The O’Donoghue triad revisited. Combined knee injuries involving anterior cruciate and medial collateral ligament tears. Am J Sports Med. 1991;19(5):474–477. ![]()
5. Bomberg, BC, McGinty, JB, Acute hemarthrosis of the knee: indications for diagnostic arthroscopy. Arthroscopy. 1990;6(3):221–225. ![]()
6. Lynch, SA, Renstrom, PA, Treatment of acute lateral ankle ligament rupture in the athlete. Conservative versus surgical treatment. Sports Med. 1999;27(1):61–71. ![]()
7. Reider, B, Sathy, MR, Talkington, J, et al, Treatment of isolated medial collateral ligament injuries in athletes with early functional rehabilitation. A five-year follow-up study. Am J Sports Med. 1994;22(4):470–477. ![]()
8. Buss, DD, Min, R, Skyhar, M, et al, Nonoperative treatment of acute anterior cruciate ligament injuries in a selected group of patients. Am J Sports Med. 1995;23(2):160–165. ![]()
9. Jarvinen, M, Kannus, P, Johnson, RJ, How to treat knee ligament injuries? Ann Chir Gynaecol. 1991;80(2):134–140. ![]()
10. Cooper, RR, Alterations during immobilization and regeneration of skeletal muscles in cats. J Bone Joint Surg 1972; 54A:919–951. ![]()
11. Jaervinen, M. Healing of a crush injury in rat striated muscle. With special reference to treatment by early mobilization or immobilization. University of Turku, Turku, Finland: Academic Dissertation; 1976.
12. Cyriax, JH. Textbook of Orthopaedic Medicine, vol 1, Diagnosis of Soft Tissue Lesions, 8th ed. London: Baillière Tindall; 1982.
13. Ellsasser, JC, Reynolds, FC, Omohundro, JR, The non-operative treatment of collateral ligament injuries of the knee in professional football players. J Bone Joint Surg 1974; 56A:1185. ![]()
14. Godshall, RW, Hansen, CA. The classification, treatment and follow-up evaluation of medial collateral ligament injuries of the knee. J Bone Joint Surg. 1974; 56A:1316.
15. Balkfors, B, The course of knee ligament injuries. Acta Orthop Scand. 1982;168(Suppl.):42. ![]()
16. Derscheld, GL, Garrick, JG, Medial collateral ligament injuries in football: non-operative management of grade I and II sprains. Am J Sports Med 1981; 9:365. ![]()
17. Holden, DI, Eggert, AW, Butler, JE, The non-operative treatment of grade I and II medial collateral ligament injuries to the knee. Am J Sports Med 1983; 11:340. ![]()
18. Ritter, MA, McCarroll, J, Wilson, FD, Carlson, SR. Ambulatory care of medial collateral ligament tears. Phys Sports Med. 1983; 11:47.
19. Fetto, JF, Marshall, JL, Medial collateral ligament injuries to the knee: a rationale for treatment. Clin Orthop 1978; 132:206. ![]()
20. Hastings, DE, The non-operative management of collateral ligament injuries of the knee joint. Clin Orthop 1980; 147:22. ![]()
21. Indelicato, PA, Non-operative treatment of complete tears of the medial collateral ligament of the knee. J Bone Joint Surg 1983; 65A:323. ![]()
22. Jones, RE, Bradford Henley, M, Francis, P, Non-operative management of isolated grade III collateral ligament injury in high school football players. Clin Orthop Rel Res 1986; 213:137–140. ![]()
23. Indelicato, P, Hermansdorfer, J, Huegel, M, Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop 1990; 256:174–177. ![]()
24. Mathieu, P, Wybier, M, Busson, J, Morvan, G, The medial collateral ligament of the knee. Ann Radiol (Paris). 1997;40(3):176–181. ![]()
25. Liu, F, Yue, B, Gadikota, HR, et al, Morphology of the medial collateral ligament of the knee. J Orthop Surg Res 2010; . ![]()
26. Hull, ML, Berns, GS, Verma, H, Patterson, HA, Strain in the medial collateral ligament of the human knee under single and combined loads. J Biomech. 1996;29(2):199–206. ![]()
27. Reider, B, Medial collateral ligament injuries in athletes. Sports Med. 1996;21(2):147–156. ![]()
28. Wijdicks, CA, Griffith, CJ, Johansen, S, et al, Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am. 2010;92(5):1266–1280. ![]()
29. Palmer, I. On the injuries to the ligaments of the knee joint. A clinical study. Acta Chir Scand. 81(Suppl. 53), 1938.
30. Schweitzer, ME, Tran, D, Deely, DM, Hume, EL, Medial collateral ligament injuries: evaluation of multiple signs, prevalence and location of associated bone bruises, and assessment with MR imaging. Radiology. 1995;194(3):825–829. ![]()
31. Altschuler, EL, Bryce, TN, Images in clinical medicine. Pellegrini–Stieda syndrome. N Engl J Med. 2006;354(1):e1. ![]()
32. Theivendran, K, Lever, CJ, Hart, WJ, Good result after surgical treatment of Pellegrini–Stieda syndrome. Knee Surg Sports Traumatol Arthrosc. 2009;17(10):1231–1233. ![]()
33. Tucker, WE. Post-traumatic para-articular ossification of the medial collateral ligament of the knee. Br J Sports Med. 1969; 4:212.
34. Chen, L, Kim, PD, Ahmad, CS, Levine, WN, Medial collateral ligament injuries of the knee: current treatment concepts. Curr Rev Musculoskelet Med. 2008;1(2):108–113. ![]()
35. Frank, G, Woo, SL-Y, Amiel, D, et al, Medial collateral ligament healing. A multidisciplinary assessment in rabbits. Am J Sports Med 1983; 11:379. ![]()
36. Burri, C, Helbing, G, Spier, W. Rehabilitation of knee ligament injuries. In: The Knee. New York: Springer; 1978.
37. Steadman, J, Rehabilitation of first and second degree sprains of the medial collateral ligament. Am J Sports Med. 1979;7(5):485–493. ![]()
38. Montgomery, J, Steadman, J, Rehabilitation of the injured knee. Clin Sports Med 1985; 4:333. ![]()
39. Cyriax, JH. Rheumatism of Soft-tissue Injuries. London: Hamilton; 1947.
40. De Maeseneer, M, Lenchik, L, Starok, M, et al, 1998. Normal and abnormal medial meniscocapsular structures: MR imaging and sonography in cadavers. Am J Roentgenol. 1995;171(4):969–976. ![]()
41. George, J, Saw, KY, Ramlan, AA, et al, Radiological classification of meniscocapsular tears of the anterolateral portion of the lateral meniscus of the knee. Australas Radiol. 2000;44(1):19–22. ![]()
42. Lougher, L, Southgate, CR, Holt, MD, Coronary ligament rupture as a cause of medial knee pain. Arthroscopy. 2003;19(10):E19–E20. ![]()
43. Noble, J, Lesions of the menisci: autopsy incidence in adults less than fifty-five years old. J Bone Joint Surg 1977; 59A:480–483. ![]()
44. Noble, J, Hamblen, DL, The pathology of the degenerated meniscus. J Bone Joint Surg 1975; 57B:180–186. ![]()
45. Goodfellow, J, He who hesitates is saved. J Bone Joint Surg 1980; 62B:1–2. ![]()
46. Kanamori, A, Woo, SL, Ma, CB, et al, The forces in the anterior cruciate ligament and knee kinematics during a simulated pivot shift test: a human cadaveric study using robotic technology. Arthroscopy. 2000;16(6):633–639. ![]()
47. Ebstrup, JF, Bojse-Moller, F, Anterior cruciate ligament injury in indoor ball games. Scand J Med Sci Sports. 2000;10(2):114–116. ![]()
48. Griffen, L, Agel, J, Albohm, MJ, et al, Noncontact ACL injuries: risk factors and prevention strategies. J Am Acad Orthop Surg 2000; 8:141–150. ![]()
49. Delfico, AJ, Garrett, WE, Jr., Mechanisms of injury of the anterior cruciate ligament in soccer players. Clin Sports Med. 1998;17(4):779–785. ![]()
50. Peterson, TR. Knee injuries due to blocking: a continuous problem. Phys Sportsmed. 1975; 3(1):440–447.
51. Paterson, FWN, Trickey, EL, Meniscectomy for tears of the meniscus combined with rupture of the anterior cruciate ligament: a follow-up study. J Bone Joint Surg 1983; 65B:388–390. ![]()
52. Bray, RC, Dandy, DJ, Meniscal lesions and chronic anterior cruciate ligament deficiency. J Bone Joint Surg 1989; 71B:128–130. ![]()
53. Goudernak, T, Der posttraumatische Hämarthros des Kniegelenkes-Arthroskopische Abklärung der Ursachen. Unfall Chirurg 1982; 8:159–169. ![]()
54. Noyes, FR, Bassett, RW, Grood, ES, Butler, DL, Arthroscopy in acute traumatic haemarthrosis of the knee. J Bone Joint Surg 1980; 62A:687. ![]()
55. Passler, J, Fellinger, M, Seggl, W, Der posttraumatische Hämarthros des Kniegelenkes – eine Indikation zur Arthroskopie. Akt Traumatol 1989; 19:135–138. ![]()
56. Hoaglund, FF. Experimental haemarthrosis. J Bone Joint Surgery. 1967; 49A:1.
57. Vahey, TN, Meyer, SF, Shelbourne, KD, Klootwyk, TE, MR imaging of anterior cruciate ligament injuries. Magn Reson Imaging Clin North Am. 1994;2(3):365–380. ![]()
58. Sandberg, R, Balkfors, B, Partial rupture of the anterior cruciate ligament – natural course. Clin Orthop Rel Res 1987; 220:176–178. ![]()
59. Clancy, WG, Ray, JM, Zoltan, DJ, Acute tears of the anterior cruciate ligament. Surgical versus conservative treatment. J Bone Joint Surg 1988; 70A:1483–1488. ![]()
60. Buss, DD, Min, R, Skyhar, M, et al, Nonoperative treatment of acute anterior cruciate ligament injuries in a selected group of patients. Am J Sports Med. 1995;23(2):160–165. ![]()
61. Fitzgerald, GK, Axe, MJ, Snyder-Mackler, L, Proposed practice guidelines for nonoperative anterior cruciate ligament rehabilitation of physically active individuals. J Orthop Sports Phys Ther. 2000;30(4):194–203. ![]()
62. Messner, K, Maletius, W, Eighteen- to twenty-five-year follow-up after acute partial anterior cruciate ligament rupture. Am J Sports Med. 1999;27(4):455–459. ![]()
63. Matsumoto, H, Seedhom, BB, Suda, Y, et al, Axis location of tibial rotation and its change with flexion angle. Clin Orthop 2000; 371:178–182. ![]()
64. Janousek, AT, Jones, DG, Clatworthy, M, et al, Posterior cruciate ligament injuries of the knee joint. Sports Med. 1999;28(6):429–441. ![]()
65. Keller, PM, Shelbourne, KD, McCarroll, JR, Rettig, AC, Non-operatively treated isolated posterior cruciate ligament injuries. Am J Sports Med 1993; 3:143–153. ![]()
66. Colvin, AC, Meislin, RJ, Posterior cruciate ligament injuries in the athlete: diagnosis and treatment. Bull NYU Hosp Jt Dis. 2009;67(1):45–51. ![]()
67. Johnson, CJ, Bach, BR. Current concepts review. Posterior cruciate ligament. Am J Knee Surg. 1990; 3:143–153.
68. Hochstein, P, Schmickal, T, Grutzner, PA, Wentzensen, A, Diagnosis and incidence of the rupture of the posterior cruciate ligament. Unfallchirurg. 1999;102(10):753–762. ![]()
69. Covey, DC, Sapega, AA, Current concepts review. Injuries of the posterior cruciate ligament. J Bone Joint Surg 1993; 75A:1376–1386. ![]()
70. Sonin, AH, Fitzgerald, SW, Friedman, H, et al, Posterior cruciate ligament injury: MR imaging diagnosis and patterns of injury. Radiology. 1994;190(2):455–458. ![]()
71. Shelbourne, KD, Jennings, RW, Vahey, TN, Magnetic resonance imaging of posterior cruciate ligament injuries: assessment of healing. Am J Knee Surg. 1999;12(4):209–213. ![]()
72. Munshi, M, Davidson, M, MacDonald, PB, et al, The efficacy of magnetic resonance imaging in acute knee injuries. Clin J Sport Med. 2000;10(1):34–39. ![]()
73. Cosgarea, AJ, Jay, PR, Posterior cruciate ligament injuries: evaluation and management. J Am Acad Orthop Surg. 2001;9(5):297–307. ![]()
74. Duri, ZA, Aichroth, PM, Zorrilla, P, The posterior cruciate ligament: a review. Am J Knee Surg. 1997;10(3):149–164. ![]()
75. Shino, K, Horibe, S, Nakata, K, et al, Conservative treatment of isolated injuries to the posterior cruciate ligament in athletes. J Bone Joint Surg. 1995;77B(6):895–900. ![]()
76. Parolie, JM, Bergfeld, JA, Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med. 1986;14(1):35–38. ![]()
77. Shelbourne, KD, Davis, TJ, Patel, DV, The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1999;27(3):276–283. ![]()
78. Fontbote, CA, Sell, TC, Laudner, KG, et al, Neuromuscular and biomechanical adaptations of patients with isolated deficiency of the posterior cruciate ligament. Am J Sports Med 2005; 33:982–989. ![]()