Disorders of the contractile structures
Extensor mechanism
Quadriceps strains and contusions
Patients who suffer an acute quadriceps strain will usually know right away. They are typically involved in sports requiring kicking, jumping, or initiating a sudden change in direction while running. Frequently, a sharp pain is felt, associated with a loss in function of the quadriceps. Sometimes pain will not fully develop during the athlete’s activity while the thigh is warm; consequently, the extent of the injury is underestimated. Stiffness, disability and pain then set in some time afterwards, e.g. late at night, and the following morning the patient can walk only with a limp.1
Clinical examination shows a normal hip and knee, although passive knee flexion is painful or both painful and limited, depending on the size of the rupture. Resisted extension of the knee is painful and slightly weak. As a rule, the lesion is in the rectus femoris, usually at mid-thigh level.2 The affected muscle belly is hard and tender over a large area. Sometimes a haematoma can be palpated. In serious lesions, a space can be detected by palpation. This is particularly the case in major ruptures just above the suprapatellar tendon, which occur mainly in patients over 40 years of age.3 In such cases, there is not only pain but also weakness during resisted extension, and the patient is unable to straighten the knee actively over the last 30°.
Ultrasonography is an excellent imaging modality for visualizing the quadriceps muscles; it has the ability to image the muscles dynamically and assess for bleeding and haematoma.4
Development of myositis ossificans as a complication of a thigh contusion is not uncommon in adolescents and young adults.5 It occurs in 9% of quadriceps contusions and seems to be associated with five risk factors (knee motion less than 120°, injury occurring during American football, previous quadriceps injury, delay in treatment of more than 3 days and ipsilateral knee effusion).6 Early diagnosis is important and is usually made with the help of sonography.7,8 There is no proper treatment but the lesion undergoes spontaneous cure within 2 years.9 Therapy with deep transverse massage is contraindicated.
Treatment
Initial haemorrhage may be reduced by elastic strapping and an ice bag over the lesion. In the case of a contusion, holding the knee in 120° of flexion for 24 hours following a quadriceps contusion also appears to shorten the time needed for the patient to return to unrestricted full athletic activities.10
Technique: deep friction to the quadriceps muscle
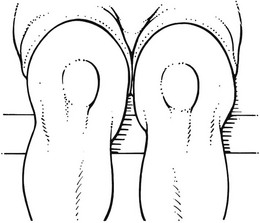
The patient sits with the knees outstretched. Flexion at the hips, together with maximal extension of the knees, induces complete relaxation of the quadriceps. The physiotherapist stands at the patient’s side. The correct level is sought. The fingers of one hand are placed deep to the affected fibres. The other hand can reinforce the palpating one. The thumbs are placed laterally to be used as a fulcrum. By flexion of the fingers, during an upward-drawing movement, the physiotherapist drives all the fibres between fingers and femur (Fig. 54.1).
After the friction, active isometric contractions are done over 5–10 minutes. Again, this is carried out in a fully relaxed position, so that the contraction cannot exert tension on the healing tissue (see Ch. 5).
Tendinous lesions about the patella
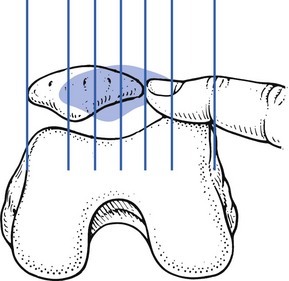
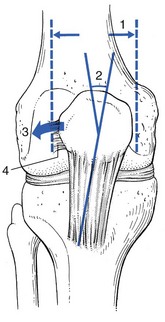
The quadriceps tendon has a superficial and a deep layer. The superficial layer runs without interruption from the quadriceps muscle, over the patella to the tibial tuberosity. The deep layer inserts all around the patellar border, effectively making the patella a sesamoid bone in the tendon. Tendinous lesions therefore occur not only at the inferior aspect of the bone but also at the superior, medial and lateral borders. Tendinosis about the patella is a typical overuse phenomenon in sports characterized by high demands on leg extensor speed and power, such as volleyball, basketball, soccer and athletics. It was first described by Sinding-Larsen in 192111 and Johansson in 1924.12 Kulund13 and Ferretti14 also reported cases of tendinosis at the upper border of the patella. Cyriax15 describes three possible sites: the upper border (suprapatellar tendinosis), the apex – the classic ‘jumper’s knee’ (infrapatellar tendinosis) and at either side of the patella (tendinosis of the quadriceps expansion) (Fig. 54.2). The lesion was uncommon until the mid-1960s, when the syndrome of jumper’s knee became more and more frequent because of increased training and higher performance goals for athletes.16,17 During the last few decades, these lesions have reached epidemic proportions18; in sports medicine centres, patellar tendinopathy is one of the leading reasons for consultation and often contributes to the decision to give up an athletic career.19

Fig 54.2 Localizations of quadriceps tendinitis (with permission from Cyriax15: p. 408): 1, suprapatellar; 2, expansion; 3, infrapatellar.
The history is obvious: during or after exertion, there is localized pain at the front of the knee. In mild examples, there is probably only a little pain after activity, whereas in a severe case pain forces the athlete to stop, and pain at rest can also supervene. The patient also states that walking upstairs or standing up from sitting is painful. The lesion can be classified by its symptoms into four stages (Table 54.1).13,20,21
Table 54.1
Staging of quadriceps tendinitis21
| Stage | Symptoms |
| I | Pain after activity |
| II | Pain at onset, disappearing during activity and reappearing after it |
| III | Continuous pain, inability to perform |
| IV | Weakness due to rupture |
Palpation identifies the site. To make the deeper layers of the tendon accessible for the palpating finger, the patella must be tilted as much as possible (see pp. 716 and 717).
Conventional radiographic techniques are of no use in the diagnosis of quadriceps tendinitis. Ultrasonography, however, seems to have some value in staging the disorder.22–24
On magnetic resonance imaging (MRI), swelling of the tendon and changes in the intrasubstance signal may be present.25 However, the sensitivity and specificity of MRI is 75% and 29%, respectively. In younger patients with relatively mild symptoms, MRI does not show significant changes and in older, active patients changes may be present in asymptomatic knees.26,27
Treatment
Classically, conservative treatment for patellar tendinopathy consists of rest, ice, taping and anti-inflammatory drugs. Other modalities, such as electrotherapy, ultrasound, laser therapy and extracorporeal shock wave therapy, have also been used.28 If these measures are insufficient or fail to relieve the symptoms, surgery is usually advised.29 The patellar tendon is incised and the hyaline inflammatory tissue (usually the middle portion of the patellar ligament) is removed.30,31 However, the benefits of open tenotomy can be questioned on the basis of the results, which show a success rate that varies between 58%14 and 78%.32 Sporting success is seen in about 50% of tenotomy patients, with a median time to return to pre-injury level of activity of 10 months.33
Eccentric training as a treatment option for tendinopathy has gained credit in recent decades. The technique was first presented by Curwin and Stanish in 1984, with encouraging results.34 The programme is based on eccentric drop squats, which are performed with some level of discomfort. During the programme, the athlete should be removed from sports activity. When training becomes pain-free, load is increased by first increasing the speed of the eccentric phase and then adding weight.35,36
Our advice is to treat all peripatellar lesions with either a local infiltration of triamcinolone or a series of deep transverse friction.37 At the upper border and the apex, infiltration with triamcinolone can be used safely and with very good results, providing the injection is done exactly at the right spot, using a weak solution (10 mg/mL) and according to the general principles of infiltration. Deep transverse friction is preferred if the lesion is too extended for infiltration. If a small spot remains resistant to treatment, it can subsequently be infiltrated.
Because relative rest is always the first measure in tendinous lesions, the patient should not return to athletics until complete remission of the lesion has been achieved. After successful treatment, and in order to prevent recurrence, it is important to detect the possible causes of the tendinitis (inappropriate or faulty training programme or structural factors) and to correct these.38
In recalcitrant cases, one or two infiltrations with sclerosing solution to the tenoperiosteal border can be tried.39
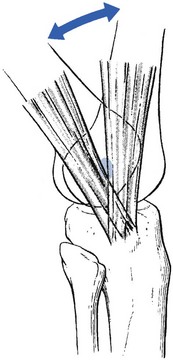
Technique: deep friction to the suprapatellar tendon
The patella must be tilted in such a way that the affected spot can be reached. This can be achieved by pressing the lower pole of the patella posteriorly with the web of the thumb or with thumb and index finger, which steadies the bone and forces the upper border upwards and forwards. With the middle finger of the other hand, the tender area can now be sought more easily. It is important to move the finger as far as possible under the inclined patella in order to catch the tendinous fibres of insertion deep under the bone. Deep friction is performed by pressing the tendon between the middle finger and the superior aspect of the patella (Fig. 54.3). The index finger is used to reinforce the middle finger. The thumb is placed as far distally as possible on the leg and used as a fulcrum. The friction consists of a to-and-fro movement of the whole forearm and hand, in a transverse direction over the tendinous fibres.
Technique: infiltration to the suprapatellar tendon
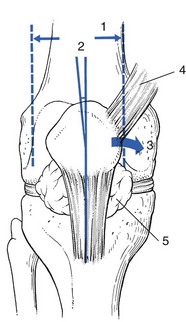
The patient sits with the knee outstretched and the hip flexed, so that the quadriceps is fully relaxed. The patella is fixed as described earlier. The upper edge of the patella is marked and the tender area identified. Usually it lies at the medial edge of the upper border, less frequently at the lateral edge of the upper border, and as a rule it is no larger than 1 or 2 cm. A spot is chosen about 1.5–2.0 cm above the centre of the affected area. A 3 cm needle fitted to a 2 mL syringe is introduced at this spot and moved in the direction of the patella (Fig. 54.4). The more the patella is tilted, the better the needle can reach the affected area. Small injections are given only when the tip of the needle is felt to pierce tendinous structure and touch bone. Considerable resistance is felt during the injection. Caution is taken to infiltrate the whole tender area by the usual technique of fanwise insertions and withdrawals.
Technique: deep friction to the quadriceps expansion
Once again, the patient sits with the knees outstretched and the quadriceps muscle fully relaxed. The therapist sits level with the patient’s knees. With the thumb of one hand, the patella is pushed distally and over towards the affected side. This allows the edge of the patella to project outwards. The little finger of the other hand is extended as far as possible. The ring finger, reinforced by the middle finger, is placed under the patellar edge in such a way that it presses upwards, squeezing the tendinous fibres against the posterior aspect of the patella. Caution is observed so as to bring the hand into full supination, which means that the operating finger is horizontal, with pressure being applied against the back of the projecting edge of the patella. A vertical finger just presses against the femur and no friction on the tenoperiosteal junction results. Hand and forearm are held in line with the tibia, and friction is produced by a horizontal movement along the patellar edge (Fig. 54.5).
Twenty minutes’ friction, three times a week for 2–3 weeks, nearly always results in cure.
Technique: deep friction to the infrapatellar tendon
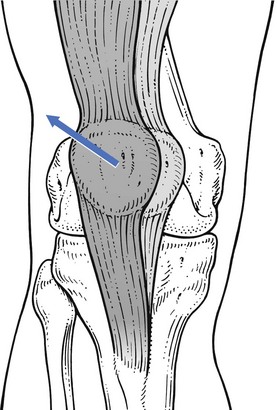
Infrapatellar tendinitis is by far the most common tendinitis at the patella. The lesion lies over an area of 1–2 cm at the inferior pole of the patella. In order to make this area more accessible, pressure is exerted at the upper part of the patella, in the following manner. The physiotherapist stands level with the extended knee. One hand is placed just above the patella, so that the web of the thumb can exert downward pressure. This stabilizes the patella and tilts the apex upwards, so that the tender area can be sought with great accuracy. Friction is given with the middle finger of the other hand, reinforced by the index finger. The thumb is placed as far proximally as possible on the thigh. Pressure is exerted upwards, so that the lesion becomes squeezed between finger and bone (Fig. 54.6). Sometimes a large osteophyte can be palpated at the apex; if so, it is important to investigate to establish which side of the osteophyte the tenderness is located. Friction is given by alternate adduction and abduction movements at the shoulder, which draw the finger strongly along the inferior border of the patella.
Technique: infiltration of the infrapatellar tendon
Once the exact location is identified and the borders marked on the skin, a point is chosen 1.5–2 cm inferior to the midpoint of the affected area. A thin 3 cm needle is fitted with a syringe, containing 2 mL of triamcinolone. With the patella remaining tilted, the needle is inserted at the identified point and moved upwards, through the infrapatellar tendon, until it hits bone (Fig. 54.7). It is important to reach the posterior aspect of the patellar apex because most lesions lie deeply at the tenoperiosteal junction. The infiltration is now given using a series of small droplets along the inferior border. Considerable pressure has to be exerted on the syringe to push the drug in. Care is taken to inject only when the tip of the needle is felt to hit bone.
Return to sport must be gradual, and a training programme that does not impose too much strain on the quadriceps during the first few weeks is advised. An underlying biomechanical factor as the basis for a possible recurrence should be sought.40,41,38
Treatment of quadriceps tendinitis is summarized in Figure 54.8.

Fig 54.8 Treatment of quadriceps tendinitis.
Rupture of the quadriceps tendon
Rupture of the suprapatellar quadriceps tendon is an uncommon injury. Most of the patients are elderly, and sometimes there is diagnostic confusion with other causes of inability to use the legs, such as a mild stroke.41 The mechanism of injury usually involves forced hyperflexion or rapid extension from a weight-bearing position.42 Pain, swelling, a palpable gap and inability to straighten the leg against resistance are the cardinal features. Treatment is operative repair.
Lesions of the infrapatellar tendon
A patellar tendon rupture may be caused by acute or chronic excessive traction force.43 The tendon is then pulled from the lower pole of the patella.44 Degenerative rheumatic disease may also give rise to rupture of the infrapatellar tendon.45,46
Lesions of the insertion at the tibial tuberosity
Apophysitis
Osteochondrosis of the tibial tuberosity, or Osgood–Schlatter disease, occurs in boys between 10 and 15 years of age.48
The typical symptoms are local pain during sports or when walking upstairs. Local tenderness makes kneeling impossible.49 Clinical examination reveals local ache during resisted extension of the knee. Palpation shows an enlarged, tender and warm tuberosity.
Radiography confirms the diagnosis and is important in differentiating the condition from more serious disorders such as osteomyelitis, arteriovenous malformations and osteosarcoma.50
Patellar fracture
Most patellar fractures are stellate fractures, occurring after a fall or a direct blow (dashboard injuries). In the last decade, an increasing number of patellar fractures in association with total knee replacement have been described.51,52
In young patients, an uncomplicated fracture heals quickly but early osteoarthrosis has to be expected.53 When accurate reduction and stable fixation cannot be achieved, partial or total patellectomy must be considered and seems to produce satisfactory results.54,55
Transverse fractures are uncommon, except in an elderly person with an osteoporotic patella. After the trauma, the patient can walk with pain; because the capsule enclosing the patella is not ruptured, displacement is avoided and therefore the disability is minor.56
Patellofemoral disorders
Introduction
Patellofemoral pain is a common condition. About 25% of the population will, at some stage in their lives, suffer from patellofemoral symptoms.57 There is no clear consensus in the literature concerning the terminology, aetiology and treatment for pain in the anterior part of the knee. The term ‘anterior knee pain’ is suggested to encompass all pain-related problems. By excluding anterior knee pain caused by intra-articular disorders, peripatellar tendinitis or bursitis, plica syndromes, Osgood–Schlatter disease and other rarely occurring conditions, it is suggested that those remaining patients with a clinical presentation of anterior knee pain could be diagnosed as having patellofemoral pain syndrome (PFPS).58 The term chondromalacia patellae, although once used as an all-inclusive term for anterior knee pain, is now only accepted to describe pathological lesions of the patellar articular cartilage found at arthroscopy or arthrotomy. A diagnosis of ‘chondromalacia patellae’ for anterior knee pain is made far too often.59,60 Stougard detected cartilaginous lesions at the posterior aspect of the patella in almost every knee joint at autopsy61 and Paar and Riehl observed damage to the patellar cartilage in almost every operated knee.62
The cause of patellofemoral pain is unknown.63 Currently, there are two theories to explain its origin: the mechanical and the neural theory.64
Mechanical theory
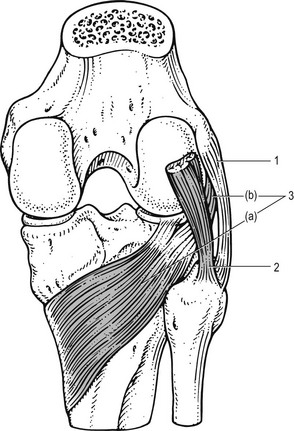
Most authors stress the importance of the congruency between the articular surfaces of the femur and the patella.65–67 During the last decade, a great deal of emphasis was given to the idea of imbalance of the soft tissues surrounding the patella as the prime cause of patellar ‘maltracking’. The soft tissue balance is particularly critical in the first 20° of knee flexion, where the position of the patella in relation to the femur is determined by the interaction of the medial and the lateral soft tissue structures; after this 20° of motion, the patella engages the femur and the bony architecture becomes more important for the position of the patella relative to the femur.68 Any imbalance in the soft tissue structures in the first 20° of flexion will mean that the patella does not encounter the trochlea optimally, which may lead to undue stress on various tissues around the joint and thus to pain. The imbalance may be the consequence of multiple biomechanical defaults. Weakness of the vastus medialis obliquus is thought to be the single most important factor causing momentary patellar subluxation.69 Also, the passive stabilizing structures are usually more extensive and stronger on the lateral than on the medial side. Active stabilization is provided by the quadriceps muscle – on the lateral side the vastus lateralis and on the medial side the vastus medialis. The fibres of the vastus medialis are divided functionally into two compartments: the vastus medialis longus and the vastus medialis obliquus (VMO). The latter does not play a role in active extension of the knee but keeps the patella centred in the trochlea of the femur throughout knee extension.70
The VMO is the only active stabilizer of the patella (Fig. 54.9); therefore the timing and the amount of activity in the VMO is critical to patellofemoral function and it is hypothesized that small changes in its activity may have considerable effects on the patellar position.71 Electromyography (EMG) studies have revealed that, in patients with patellofemoral pain, the VMO contracts at a significantly slower rate than the vastus lateralis, whereas in normal subjects the reflex response time of both muscles is equal.72–74 A recent MRI study examined VMO size in patients with patellofemoral problems and found atrophy in all of them. Although it is not clear whether this atrophy is a result or a cause of PFPS, there is obviously a strong relationship between the two.75

Fig 54.9 Active medial stabilization is provided by the vastus medialis obliquus (VMO): 1, VMO; 2, patella.
Other biomechanical factors that may contribute to the development of patellofemoral pain are tightness in the lateral structures, increased Q angle (see p. 722) and faulty foot mechanisms.76–78 In a retrospective study on 282 male and female students enrolled in physical education classes, Witvrouw et al found a significant correlation between four parameters and the development of patellofemoral pain: a shortened quadriceps muscle, an altered VMO muscle reflex response time, a decreased explosive strength and a hypermobile patella.79
Neural theory
The normal articular cartilage is aneural, so defects in the surface are not thought to produce pain. It has therefore been suggested that irritation of the subchondral bone produces the pain.80 Schneider et al could reproduce the typical pain sensation by raising intrapatellar pressure in about 40% of patients suffering from persistent patellofemoral pain. This subgroup was treated with a new method of intraosseous drilling and decompression. Of the patients so treated, 90% experienced pain relief more than 3 years postoperatively, which may indicate osseous hypertension as a cause of the pain.81
Some authors have sought the origin of the pain in soft tissue structures around the knee. Nociceptive nerve fibres and neural markers (S-100 protein, neurofilament protein, substance P and neural growth factor) have been demonstrated in the medial and lateral retinacula and in the infrapatellar fat pad.82,83
Clinical examination
It is important to stress the fact that most anterior knee pain is not caused by patellofemoral disorders but stems from infra-, supra- or peripatellar tendinitis, or a coronary ligament lesion. A basic functional examination should therefore always be performed first (see Box 54.1). However, if specific symptoms warrant, and the basic functional examination is totally negative, attention must be directed towards any peculiarities found during inspection of the patella and surrounding tissues.
Inspection on standing
Alignment of the lower extremity is evaluated first by observing the patient standing. Excessive varus or valgus of the extremities and internal femoral rotation are often associated with an extensor mechanism malalignment. Hyperextendable knees may also contribute to the development of anterior knee pain. McConnell points out that shock absorption throughout the lower leg then comes from internal rotation of the femur, rather than from knee flexion.84
Inspection on sitting
Some of the most important observations are made with the patient in the sitting position, with the legs bent to 90°. The position of the patella is assessed by viewing the knee from the lateral and the frontal aspects. In a lateral view (Fig. 54.10), the patella should be situated on the distal end of the femur, with the proximal patellar pole level with the anterior femur and the anterior surface of the patella in line with the tibial shaft. In ‘patella alta’, the upper border of the patella sits more on the anterior surface of the femur and ‘faces towards the ceiling’. Viewed from anterior, a normally positioned patella faces straight ahead (Fig. 54.11); ‘outfacing’ and ‘infacing’ patellae are easily recognized in this position.
Inspection in the supine position
The knee is in almost full extension (a small cushion is placed in the popliteal fossa) and the quadriceps is fully relaxed. The position of the patella in relation to the femur is observed. In the obese knee it may be necessary to palpate the patellar borders with one hand and the femoral condyles with the other. Four components affect the patella statically and dynamically: lateral glide, mediolateral tilt, anteroposterior tilt and rotation. An optimal patellar position is one where the patella is parallel to the femur in the frontal and the sagittal planes and midway between the two condyles of the femur when the knee is flexed to 20°.84
Q angle
Next the Q angle is measured. This is the angle at the centre of the patella between two imaginary lines, from the anterior superior iliac spine and from the tibial tuberosity to the geometric centre of the patella. A Q angle of up to 10° is normal in the male and up to 15° in the female (Fig. 54.12).85
Passive movements of the patella
Patellar mobility is best assessed on a knee flexed to ± 20° (the knee resting on a cushion or on the thigh of the examiner), with the quadriceps completely relaxed. The examiner’s thumbs are placed on the medial border of the patella and the index fingers on the lateral border as attempts are first made to push the patella laterally and then medially. Quantitating the degree of mobility can be done by dividing the width of the patella into four longitudinal quadrants (Fig. 54.13). In normal subjects, the patella cannot be displaced more than three quadrants laterally and should allow a medial shift over at least one quadrant. When the patella is moved in a medial direction, it should initially remain parallel to the femur and not tilt during the first quadrant of the movement.
Inspection during active movement
Close observation of the patella in relation to the femur is then continued during active contraction of the quadriceps. The patella should be pulled directly superiorly, or superiorly and slightly laterally. Excessive lateral displacement represents lateral overpull by the quadriceps and has been referred to as the ‘lateral pull sign’ (Fig. 54.14).86
Clinical examination of the patellofemoral articulation is summarized in Box 54.1.
Clinical manifestations
From a clinical perspective, patellofemoral problems in the skeletally mature patient fall into three broad categories: patellofemoral instability (subluxation or dislocation), patellofemoral pain with malalignment but no episodes of instability, and patellofemoral pain without malalignment.87
Recurrent dislocation and subluxation of the patella
More often, there is a subluxation of the kneecap. The patient does not report the dramatic features described above but merely a ‘catching’ of the knee, followed by medial pain. The latter is caused by tearing of the medial capsular structures and should be differentiated from lesions of the medial meniscus.88
Clinical examination often reveals an enlarged fat pad and patella alta. There is deficiency or atrophy of the VMO. Some authors find a significantly decreased Q angle.89 Lateral patellar mobility is increased (more than three-quarters of the width of the patella) and apprehension can often be provoked during glide mobilization of the patella (Fig. 54.15).
Treatment
In acute or recurrent dislocation, surgical intervention is advised but only after puberty, when the epiphysis has closed. Good subjective results are to be expected in about 80% of patients.90
In recurrent subluxation, the decision to operate should not be taken lightly because it has been demonstrated that long-term results continue to show an incidence of persistent instability and late patellofemoral arthrosis.91–93 Arthroscopic release only gives a satisfactory result in 40% of cases.94 Treatment of patellofemoral instability should therefore be conservative, surgical interventions being reserved for patients who do not respond adequately. Conservative treatment consists of intensive functional vastus medialis rehabilitation, together with the use of a brace (see treatment of PFPS, p. 1143).
Patellofemoral pain syndrome without subluxation
The source of pain in ‘patellofemoral pain syndrome’ cannot be adequately explained. The hypothesis is that patients with PFPS have lateral displacement of the patella within the femoral trochlea.95 This lateral ‘malalignment’ may result from a number of factors, including malalignment of the lower extremity and/or the patella, tight lateral soft tissue structures and muscular imbalance of the lower extremity. All may lead to areas of increased stress on the patellofemoral joint and pain.96
Most patients with knee pain attributed to PFPS are young women. The common symptom is of a dull and vague aching behind the kneecap during and after physical activity, especially during body-weight loading of the lower extremities (walking up- or downstairs and squatting). The knee is usually also sore in a sitting position and a few patients have nocturnal pain too.97
Routine clinical examination reveals nothing. There is a full and painless range of movement, with normal end-feels. Resisted extension is strong and painless. Inspection may reveal some typical abnormalities. Excessive varus or valgus position of the lower extremities is often associated with a malalignment of the patella. The position of the patellae is first assessed in the sitting position. Laterally tilted patellae (Fig. 54.16) appear to be ‘looking’ up and over the examiner’s shoulders towards the ceiling, the so-called ‘grasshopper eyes’ kneecap.
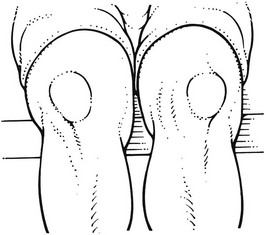
Fig 54.16 Laterally tilted patellae.
Excessive lateral movement of the patella during active contraction of the quadriceps (the ‘lateral pull sign’) or during active extension of the knee in a sitting position indicates predominance of lateral forces. They are common findings in PFPS (Fig. 54.17).
The classic radiological examination techniques to visualize the patellofemoral articulation are the Merchant98 and Laurin99 views, whereby the joint surfaces are visualized with the knee flexed to 45° and 30° respectively. MRI has also been found to be an accurate and reproducible method of measurement of the patellar tilt angle.100,101
Arthroscopy is of little value in the diagnosis of PFPS. The incidence of damaged cartilage in asymptomatic patients is so high that arthroscopy on its own cannot determine whether the symptoms should be attributed to chondromalacia. Hertel detected lesions of the articular surface of the patella in about 50% of routine arthroscopies.102 Paar and Schneider found clear damage to the cartilage in 67% of the joints in which they undertook arthroscopies.103 These two series establish that arthroscopic lesions occur far more frequently than do clinical manifestations, and that overestimation of disease is a hazard if diagnosis is based totally on the result of arthroscopy.
Treatment
In a number of patients, the condition seems to be self-limiting, as demonstrated by Sandow and Goodfellow, who reported spontaneous cure in more than 20% of anterior knee syndromes. Of 54 girls suffering from PFPS, only 9 were permanently unable to participate in sports after a follow-up period of 4 years.104
Many different treatment protocols for PFPS have been described in the literature. It is clear that, if abnormal tracking of the patella is believed to be the reason for the pain, the initial treatment must be to try to restore normal alignment. An optimal patellar position is achieved by stretching the tight lateral structures and by changing the activation pattern of the VMO.68
Stretching is performed passively by the therapist. However, the most effective stretch to the shortened retinacular tissue is obtained by sustained low load, using tape, which facilitates a permanent elongation of the tissue.105–107
Specific training of the vastus medialis includes timing and intensity of the VMO relative to the vastus lateralis (VL). Ideally, the VMO should come in slightly earlier than the VL.73 This is mainly achieved during weight-bearing activities. It has been proposed that training causes changes within the nervous system that allow an individual to coordinate the activities of muscle groups better.108 Biofeedback machines are extremely useful to facilitate this process.109 Adding some hip adduction in training will also cause an increase in VMO activity relative to VL.110
If symptoms persist despite a conservative treatment programme, surgery may be indicated. An arthroscopic approach, with shaving of the affected area111 and/or lateral release of the lateral retinaculum, is recommended.112,113 Before deciding to operate, however, it is important to remember that the long-term results are not as good as might be hoped.114,115
Patellofemoral arthrosis
This can occur after a flake fracture of the articular surface of the patella.116 It is not clear whether chondromalacia patellae precedes osteoarthritic changes because the anatomical location of the two conditions differs. Chondromalacia is most often found near the median ridge, whereas osteoarthrosis first appears on the very medial side of the patella.13 Erosion of the cartilage at the medial edge may start before the age of 20 and has been shown to be present in three-quarters of individuals by the age of 30.
As in other localizations of osteoarthrosis, radiographic signs do not always equate with symptoms. Sometimes the patient is aware only of grating or cracking when walking upstairs. Alternatively, the symptoms may be very similar to those in chondromalacia: anterior pain when walking upstairs, squatting or sitting with bent knees.117 Palpation during squatting reveals pain, together with ‘crackling’ and ‘popping’ sensations.
Treatment depends on the severity of the symptoms. Intra-articular injections with hyaluronan has proven to be an effective treatment modality for patellofemoral arthrosis, with beneficial effects on pain, function and patient global assessment.118,119 In intractable cases, patellofemoral arthroplasty can be advised.120
Strained iliotibial band
The iliotibial band, a thick extension of the fascia lata, inserts at the tibial tubercle of Gerdy. The band lies anterior to the flexion–extension axis of the knee in extension and posterior in flexion. The tensor fasciae latae, acting through the band, is thus a weak external rotator and extensor of the knee. Iliotibial band friction syndrome is an overuse injury usually seen in military personnel, cyclists and long-distance runners.121 With an incidence of between 1.6 and 12%, it is the most common running injury of the lateral knee in long-distance runners.122,123
The presumed pathogenesis is that during activities involving repetitive knee flexion (such as running), the iliotibial band repetitively shifts forwards and backwards over the lateral femoral epicondyle, causing friction and thus inflammation of the iliotibial band (Fig. 54.18). Friction thus occurs at, or slightly below, 30° of flexion.124 This can produce either irritation and subsequent inflammatory reactions within the iliotibial tract itself, or formation of a painful bursa between the band and the epicondyle.125,126
While running, athletes notice increasing pain at the outer side of the knee, which forces them to stop. The pain is more intense when the foot comes in contact with the ground when running downhill or during deceleration.127 In severe instances, the pain may be so sharp that walking with a normal gait becomes impossible.
Examination reveals no abnormality of the joint but some discomfort is experienced when extension and lateral rotation are carried out against resistance. Sometimes a painful arc is found when the band slips over the lateral epicondyle at 30° of flexion. When the routine examination is negative, a simple confirmatory test may be done. In 90° of flexion, pressure is applied at the iliotibial band over the lateral epicondyle; as the knee is gradually extended, the epicondylar area becomes painful at about 30° of flexion.128 MRI may be useful in confirming the diagnosis.129–131
Flexor mechanism
Hamstring strains
The hamstrings have a double function. They not only extend the thigh and flex the knee (concentric function), but also antagonize the quadriceps during knee extension in running (eccentric function). It is probable that a sudden change from stabilizing activity to an active function is the main reason for a hamstring strain.133–135
Lesions of the hamstrings are frequently seen in athletes, and rugby, American football and soccer players.136–138 Classically, a strain occurs as a sprinter leaves the starting blocks or during a slide in soccer. The athlete feels a snap, immediately followed by pain and functional loss. In lesions of the muscle belly, straight leg raising is limited by pain because of muscle spasm. Prone-lying resisted knee flexion is painful. Resisted external or internal rotation can then distinguish between a biceps lesion or a lesion in the medial hamstrings. The short head of the biceps seems to be the most frequently strained.139,140 Sometimes there is a haematoma and the tender area is swollen.141
Treatment
An elastic wrap and an ice bag should be applied immediately after the incident.
Technique: deep friction to the hamstrings
The technique is very similar to the one used in quadriceps lesions but here the patient lies prone, with the hip extended and the knee passively flexed to 90°. This position produces complete relaxation of the muscle belly. The therapist sits or stands level with the patient’s limb. The fingers of one hand, perhaps reinforced by the other hand, are placed deep to the affected part of the belly. The thumbs are positioned laterally on the femur and used as a fulcrum. An extension movement at the wrists moves the flexed fingers upwards and pulls on the fibres, which are felt to slip under the fingers (Fig. 54.19). The effect of deep friction can be increased somewhat by a rotational movement around the thumbs at the end of this movement. As this treatment is extremely tiring, three periods of 5 minutes’ friction over a total of 20 minutes is as much as is practicable.
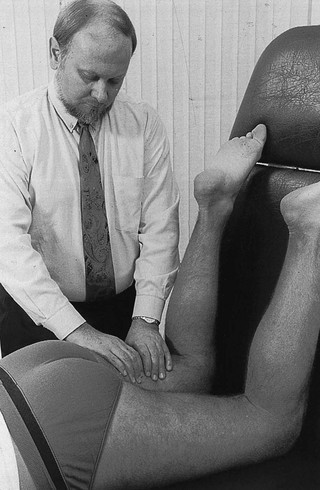
Fig 54.19 Deep friction to the hamstrings.
After friction, electric or active isometric contractions should be given for about 10 minutes. The purpose is to expand the muscle transversely as much as possible, without strain on the healing fibres. This prevents intramuscular adhesions, often responsible for recurrent or chronic strains of the hamstrings.142 The possibility of recurrence is considerable if the patient goes back to athletics too soon.143 Therefore treatment should continue with massage and electric contractions for a week after clinical cure is established. Return to sport should be progressive, and special care should be taken to ‘warm up’ adequately.
Prophylaxis should also include progressive strengthening exercises and stretching before and after activity.144
Biceps tendinitis
This usually occurs as an overuse lesion in athletes. Pain develops at the outer side of the knee. Functional examination is entirely negative, except that resisted flexion hurts at the outer side. Resisted external rotation is also painful. Tenderness is found at the biceps tendon, usually at the tenoperiosteal insertion at the head of the fibula.145,146
Technique: friction to the biceps tendon
The patient lies prone with the knee fully outstretched. The physiotherapist stands at the opposite side, level with the knee. The head of the fibula is easily identified. The index finger is placed on the tendon at the level of the lesion. Counterpressure is exerted with the thumb placed at the medial side of the knee (Fig. 54.20). Massage is now given using small, alternating extension and flexion movements at the wrist, while the thumb is kept still.

Fig 54.20 Massage of the biceps tendon.
Twenty minutes, three times a week for 3–6 weeks, may be required.
Lesions of the upper tibiofibular joint
Dislocations or fractures may occur after violent twists or direct blows, as when a rider’s knee is caught between a tree and the horse, for example.147 It is clear that the examiner must be especially alert for these injuries because they can lead to peroneal nerve palsy.
A sprain of the upper tibiofibular ligament can develop after trauma to the ankle joint or as the result of repetitive strains.148
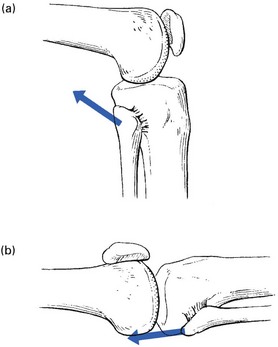
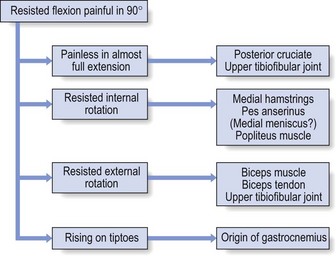
The findings on clinical examination are the same as in biceps tendinitis. Because contraction of the biceps pulls the fibula backwards on the tibia, resisted flexion and resisted external rotation hurt at the outer side of the knee (Fig. 54.21a). However, when the biceps tendon is examined for tenderness, none is found. Resisted flexion in almost full extension is also painless, because the fibular head is now pulling upwards instead of backwards and stress is no longer imposed on the tibiofibular ligaments (Fig. 54.21b). Also, passive backwards movement of the fibular head elicits pain and the anterior tibiofibular ligament is tender to the touch.
Strained popliteus muscle
Should resisted flexion and internal rotation hurt at the lateral or posterolateral aspect of the knee, the popliteus tendon or muscle is suspected (Fig. 54.22).
The popliteus tendon originates from the lateral femoral condyle. It passes deeply to the lateral collateral ligament, which it separates from the lateral meniscus.149 The tendon also attaches partly to the lateral meniscus.150,151 The muscle belly inserts with a broad and short tendon at the posterior aspect of the tibia, in the popliteal fossa. Although the muscle is a flexor and internal rotator of the leg, its main function is to prevent a sliding forwards of the lateral femoral condyle on the fixed tibia during the stance phase in walking or running, especially in running downhill or descending stairs.152–154 This makes the popliteus an important active stabilizer of the lateral and posterolateral aspect of the knee joint and explains the frequency of popliteal lesions in long-distance runners and downhill skiers. The prevention of forward sliding is also a function of the posterior cruciate ligament (passive stabilizer), and a strained popliteus muscle can closely simulate a ligamentous strain of the posterior cruciate. Only a careful functional examination differentiates the two lesions.155
Localization of the pain and palpation for tenderness further reveal that the lesion lies at the tendon or in the muscle belly.156,157
Treatment
Tendinous lesions respond very well to one or two infiltrations with 10 mg of triamcinolone.
Technique: infiltration of the popliteus tendon
The patient lies supine, with the knee flexed to 90°. The tendon is identified by careful palpation of the lateral condyle. At the most prominent aspect, two small bony projections can be palpated, with a groove running vertically downwards between them. In this groove, the origin of the popliteus tendon can easily be palpated and followed until it disappears under the lateral collateral ligament. If the origin is tender, 1 mL of triamcinolone should be infiltrated with the usual technique: the needle is brought in through capsule and ligament until it reaches bone (Fig. 54.23). A series of droplets is then injected at different areas, but only when the tip of the needle is felt to touch bone.
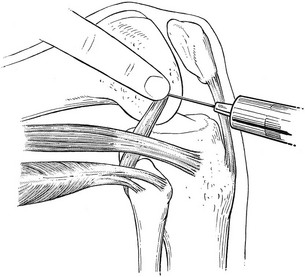
Fig 54.23 Infiltration of the popliteus tendon.
Technique: deep friction to the popliteus muscle
The patient adopts a prone position, with the knee slightly bent. The physiotherapist stands lateral to the patient’s leg. One thumb, reinforced by the other, is placed on the affected spot, parallel to the muscular fibres (Fig. 54.24). Deep transverse friction is now given, by a supination movement of both arms, which makes the thumbs roll transversely over the muscle fibres. The direction of the movement is cranial and medial.

Fig 54.24 Deep friction to the popliteus muscle.
References
1. Ryan, AJ. Quadriceps strain, rupture and charley horse. Med J Sports. 1969; 1:106–111.
2. Hughes, C, Hasselman, CT, Best, TM, et al, Incomplete, intrasubstance strain injuries of the rectus femoris muscle. Am J Sports Med 1995; 23:500–506. ![]()
3. Funk, FJ, Jr. Injuries of the extensor mechanism of the knee. Athletic Training. 1975; 10:141–145.
4. La, S, Fessell, DP, Femino, JE, et al, Sonography of partial thickness quadriceps tendon tears with surgical correlation. J Ultrasound Med 2003; 22:1323–1329. ![]()
5. Young, JL, Laskowski, ER, Rock, MG, Thigh injuries in athletes. Mayo Clin Proc. 1993;68(11):1099–1106. ![]()
6. Ryan, JB, Wheeler, JH, Hopkinson, WJ, et al, Quadriceps contusions. West Point update. Am J Sports Med. 1991;19(3):299–304. ![]()
7. Peck, RJ, Metreweli, C, Early myositis ossificans: a new echographic sign. Clin Radiol. 1988;139(6):586–588. ![]()
8. Mellerowicz, H, Stelling, E, Kefenbaum, A, Diagnostic ultrasound in the athlete’s locomotor system. Br J Sports Med. 1990;24(1):31–39. ![]()
9. Sumiyoshi, K, Tsuneyoshi, M, Enjoji, M, Myositis ossificans. A clinicopathologic study of 21 cases. Acta Pathol Jpn. 1985;35(5):1109–1122. ![]()
10. Aronen, JG, Garrick, JG, Chronister, RD, McDevitt, ER, Quadriceps contusions: clinical results of immediate immobilization in 120 degrees of knee flexion. Clin J Sport Med. 2006;16(5):383–387. ![]()
11. Sinding-Larsen, CMF, Kristiana, MD. A hitherto unknown affection of the patella in children. Acta Radiol. 1921; 1:171–173.
12. Johansson, S. Eine bisher anscheinend unbekannte Erkrankung der Patella. Z Orthop Chirurg. 1924; 43:82–87.
13. Kulund, DN. The Injured Athlete, 2nd ed. Philadelphia: Lippincott; 1988.
14. Ferretti, A, Puddu, G, Marianni, PP, Neri, M, The natural history of jumper’s knee. Patellar or quadriceps tendinitis. Int Orthop 1985; 8:239–242. ![]()
15. Cyriax, JH. Textbook of Orthopaedic Medicine, vol I, Diagnosis of Soft Tissue Lesions, 8th ed. London: Harcourt Brace & Co Ltd, Elsevier Health Science Books; 1982.
16. Schneider, PG. Das Patellaspitzensyndrom. Dtsch Z Sportsmedizin. 1981; 2:27–35.
17. Colosimo, AJ, Bassett, FH, Jumper’s knee. Diagnosis and treatment. Orthop Rev. 1990;19(2):139–149. ![]()
18. Lian, OB, Engebretsen, L, Bahr, R, Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med 2005; 33:561–567. ![]()
19. Kettunen, JA, Kvist, M, Alanen, E, Kujala, UM, Long-term prognosis for jumper’s knee in male athletes. A prospective follow-up study. Am J Sports Med 2002; 30:689–692. ![]()
20. Roels, J, Martens, M, Mulier, JC, Burssens, A, Patellar tendinitis (jumper’s knee). Am J Sports Med 1978; 6:362–368. ![]()
21. Blazina, ME, Kerlan, RK, Jobe, FW, et al, Jumper’s knee. Orthop Clin North Am 1973; 4:665–678. ![]()
22. Fornage, B. L’Ultrasonographie du tendon rotulien. J Echogr Med Ultrasonore. 1983; 4:145–149.
23. Fritschy, D, de Gautard, R, Jumper’s knee and ultrasonography. Am J Sports Med. 1988;16(6):636–640. ![]()
24. King, JB, Percy, DJ, Mourad, K, Kumar, SJ, Lesions of the patellar ligament. J Bone Joint Surg 1990; 72B:46–48. ![]()
25. Johnson, DP, Wakeley, CJ, Watt, I, Magnetic resonance imaging of patellar tendonitis. J Bone Joint Surg. 1996;78B(3):452–457. ![]()
26. Shalaby, M, Almekinders, LC, Patellar tendinitis: the significance of magnetic resonance imaging findings. Am J Sports Med. 1999;27(3):345–349. ![]()
27. Major, NM, Helms, CA, MR imaging of the knee: findings in asymptomatic collegiate basketball players. AJR Am J Roentgenol. 2002;179(3):641–644. ![]()
28. Peers, KH, Lysens, RJ, Patellar tendinopathy in athletes: current diagnostic and therapeutic recommendations. Sports Med 2005; 35:71–387. ![]()
29. Popp, JE, Yu, JS, Kaeding, CC, Recalcitrant patellar tendinitis. Magnetic resonance imaging, histologic evaluation, and surgical treatment. Am J Sports Med 1997; 25:218–222. ![]()
30. Krahl, H, ‘Jumper’s Knee’ – Athiologie, Differentialdiagnose und Therapeutische Möglichkeiten. Orthopäde 1980; 9:197. ![]()
31. Pierets, K, Verdonk, R, De Muynck, M, Lagast, J, Jumper’s knee: postoperative assessment. A retrospective clinical study. Knee Surg Sports Traumatol Arthrosc. 1999;7(4):239–242. ![]()
32. Van der, Ent, Baere, GAJ. Jumper’s knee. In: Jaarcongres van de Nederlandse Orthopaedische Vereniging. Leiden: De Medicus; 1985:145–165.
33. Coleman, BD, Khan, KM, Kiss, ZS, et al, Open and arthroscopic patellar tenotomy for chronic patellar tendinopathy. A retrospective outcome study. Victorian Institute of Sport Tendon Study Group. Am J Sports Med. 2000;28(2):183–190. ![]()
34. Curwin, S, Stanish, WD. Tendinitis: its etiology and treatment. Lexington, MA: Collamore Press; 1984.
35. Jonsson, P, Alfredson, H, Superior results with eccentric compared to concentric quadriceps training in patients with jumper’s knee: a prospective randomised study. Br J Sports Med 2005; 39:847–850. ![]()
36. Purdam, CR, Jonsson, P, Alfredson, H, et al, A pilot study of the eccentric decline squat in the management of painful chronic patellar tendinopathy. Br J Sports Med 2004; 38:395–397. ![]()
37. Houbben, R. La Tendinite du tendon rotulien chez le sportif par le massage transversal profond. Belgium: Mémoires de fin d’étude, Ecole Provinciale Supérieure de Kinésthérapie, Fléron; 1989.
38. Peers, KH, Lysens, RJ, Patellar tendinopathy in athletes: current diagnostic and therapeutic recommendations. Sports Med. 2005;35(1):71–87. ![]()
39. Hoksrud, A, Ohberg, L, Alfredson, H, Bahr, R, Ultrasound-guided sclerosis of neovessels in painful chronic patellar tendinopathy: a randomized controlled trial. Am J Sports Med 2006; 34:1738–1746. ![]()
40. Petracic, B, Petracic, A, Insertionstendinopathie des Kniegelenkes bei Radsportlern in Abhängigkeit von der Körperposition sowie Schuhpedalenverbindung. Sportverletz Sportschaden. 1992;6(1):29–31. ![]()
41. McEachern, AG, Plewes, JL, Bilateral simultaneous rupture of the quadriceps tendon. J Bone Joint Surg 1984; 66B:250–252. ![]()
42. Levine, RJ, Patellar tendon rupture. The importance of timely recognition and repair. Postgrad Med. 1996;100(2):241–242. ![]()
43. Rosenberg, JM, Whitaker, JH, Bilateral infrapatellar tendon rupture in a patient with jumper’s knee. Am J Sports Med. 1991;19(1):94–95. ![]()
44. Zernicke, RF, Garhammer, J, Jobe, FW, Human patellar tendon rupture: a kinetic analysis. J Bone Joint Surg 1977; 59A:179–183. ![]()
45. Julius, A, Rupture of the quadriceps tendon. Neth J Surg 1984; 36:134–136. ![]()
46. Loehr, JR, Welsh, RP, Spontaneous rupture of quadriceps tendon and patellar ligament during treatment for chronic renal failure. Can Med Assoc 1983; 129:254–256. ![]()
47. Kelly, DW, Carter, VS, Joke, FW, Kerlan, RK, Patellar and quadriceps tendon ruptures – Jumper’s knee. Am J Sports Med 1984; 12:375. ![]()
48. Osgood, RB. Lesions of the tibial tubercle occurring during adolescence. Boston Med Surg J. 1903; 148:114–117.
49. Mital, M. Osgood–Schlatter’s disease: the painful puzzler. Phys Sportsmed. 1977; 5(6):60–73.
50. D’Ambrosia, RD, MacDonald, GL, Pitfalls in the diagnosis of Osgood–Schlatter disease. Clin Orthop 1975; 110:206–209. ![]()
51. Bourne, RB, Fractures of the patella after total knee replacement. Orthop Clin North Am. 1999;30(2):287–291. ![]()
52. Harwin, SF, Patellofemoral complications in symmetrical total knee arthroplasty. J Arthroplasty. 1998;13(7):753–762. ![]()
53. Larson, RL, Singer, KM. Patellar disorders. Clin Sports Med. 4(2), 1985.
54. Jakobsen, J, Christiansen, KS, Rasmussen, OS, Patellectomy, a 20 year follow-up. Acta Orthop Scand 1985; 56:430–432. ![]()
55. Freuler, F, Brunner, CH, Rüter, A, Spätresultate bei operierten Patellafrakturen. Hefte Unfallheilkunde 1975; 120:68–75. ![]()
56. Klassen, JF, Trousdale, RT, Treatment of delayed and nonunion of the patella. J Orthop Trauma. 1997;11(3):188–194. ![]()
57. Fulkerson, J, Hungerford, D. Disorders of the Patellofemoral Joint, 2nd ed. Baltimore: Williams & Wilkins; 1990.
58. Thomee, R, Augustsson, J, Karlsson, J, Patellofemoral pain syndrome: a review of current issues. Sports Med. 1999;28(4):245–262. ![]()
59. Abernethy, PJ, Is chondropathy a separate clinical entity? J Bone Joint Surg 1978; 60B:205–212. ![]()
60. Radin, EL. Anterior knee pain – the need for a specific diagnosis. Stop calling it chondromalacia!. Orthop Rev. 1985; 14:128.
61. Stougard, J, Chondromalacia of the patellae: incidence, macroscopical and radiographic findings at autopsy. Acta Orthop Scand 1975; 46:809. ![]()
62. Paar, O, Riehl, KO. Chondropathia patellae und trauma. Munch Med Wochenschr. 1982; 124(41):888.
63. Collado, H, Fredericson, M, Patellofemoral pain syndrome. Clin Sports Med. 2010;29(3):379–398. ![]()
64. Sanchis-Alfonso, V, Rosello-Sastre, E, Martinez-Sanjuan, V, Pathogenesis of anterior knee pain syndrome and functional patellofemoral instability in the active young. Am J Knee Surg. 1999;12(1):29–40. ![]()
65. Insall, J, Current concepts review – patellar pain. J Bone Joint Surg 1982; 64A:147–151. ![]()
66. McNally, EG, Ostlere, SJ, Pal, C, et al, Assessment of patellar maltracking using combined static and dynamic MRI. Eur Radiol. 2000;10(7):1051–1055. ![]()
67. Reider, B, The anterior aspect of the knee joint. J Bone Joint Surg. 1981;63A(3):351. ![]()
68. McConnell, J, Management of patellofemoral problems. Manual Therapy 1996; 1:60–66. ![]()
69. Sakai, N, Luo, ZP, Rand, JA, An, KN, The influence of weakness in the vastus medialis oblique muscle on the patellofemoral joint: an in vitro biomechanical study. Clin Biomech. 2000;15(5):335–339. ![]()
70. Lieb, F, Perry, J, Quadriceps function. J Bone Joint Surg. 1968;50A(8):1535–1548. ![]()
71. Powers, CM, Patellar kinematics, part I: the influence of vastus muscle activity in subjects with and without patellofemoral pain. Phys Ther. 2000;80(10):956–964. ![]()
72. Mariano, P, Caruso, J, An electromyographic investigation of subluxation of the patella. J Bone Joint Surg 1979; 61:169–171. ![]()
73. Voigt, M, Weider, D, Comparative reflex response times of the vastus medialis and the vastus lateralis in normal subjects and subjects with extensor mechanism dysfunction. Am J Sports Med 1991; 10:131–137. ![]()
74. Van Tiggelen, D, Cowan, S, Coorevits, P, et al, Delayed vastus medialis obliquus to vastus lateralis onset timing contributes to the development of patellofemoral pain in previously healthy men: a prospective study. Am J Sports Med. 2009;37(6):1099–1105. ![]()
75. Pattyn, E, Verdonk, P, Steyaert, A, et al, Vastus medialis obliquus atrophy: does it exist in patellofemoral pain syndrome? Am J Sports Med. 2011;39(7):1450–1455. ![]()
76. Luo, ZP, Sakai, N, Rand, JA, An, KN, Tensile stress of the lateral patellofemoral ligament during knee motion. Am J Knee Surg. 1997;10(3):139–144. ![]()
77. Huberti, HH, Hayes, WC, Patellofemoral contact pressure. J Bone Joint Surg 1984; 66A:715–724. ![]()
78. Ficat, P, Ficat, C, Bailleux, A, Syndrome d’hyperextension externe de la rotule. Rev Chirurg Orthop 1975; 61:39–59. ![]()
79. Witvrouw, E, Lysens, R, Bellemans, J, et al, Intrinsic risk factors for the development of anterior knee pain in an athletic population. A two-year prospective study. Am J Sports Med. 2000;28(4):480–489. ![]()
80. Insall, J, ‘Chondromalacia patellae’: patellar malalignment syndrome. Orthop Clin North Am 1979; 10:117–127. ![]()
81. Schneider, U, Breusch, SJ, Thomsen, M, et al, A new concept in the treatment of anterior knee pain: patellar hypertension syndrome. Orthopedics. 2000;23(6):581–586. ![]()
82. Witonski, D, Wagrowska-Danielewicz, M, Distribution of substance-P nerve fibers in the knee joint in patients with anterior knee pain syndrome. A preliminary report. Knee Surg Sports Traumatol Arthrosc. 1999;7(3):177–183. ![]()
83. Sanchis-Alfonso, V, Rosello-Sastre, E, Immunohistochemical analysis for neural markers of the lateral retinaculum in patients with isolated symptomatic patellofemoral malalignment. A neuroanatomic basis for anterior knee pain in the active young patient. Am J Sports Med. 2000;28(5):725–731. ![]()
84. McConnell, J. The management of chondromalacia patellae. A long term solution. Aust J Physiother. 1986; 2:215–233.
85. Carson, W, James, S, Larson, L, et al, Patellofemoral disorders. Physical and radiographic evaluation. Part I: physical examination. Clin Orthop 1984; 185:165–177. ![]()
86. Kolowich, PA, Paulos, LE, Rosenberg, TD, Fansworth, S, Lateral release of the patella: indications and contraindications. Am J Sports Med 1990; 18:359–365. ![]()
87. Holmes, SW, Jr., Clancy, WG, Jr., Clinical classification of patellofemoral pain and dysfunction. J Orthop Sports Phys Ther. 1998;28(5):299–306. ![]()
88. Hughston, JC, Subluxation of the patella. J Bone Joint Surg 1968; 50A:1003–1026. ![]()
89. Reider, B, Marshall, J, Warren, R, Clinical characteristics of patellar disorders in young athletes. Am J Sports Med. 1981;9(4):270–274. ![]()
90. Vainionpaä, S, Laasonen, E, Silvenoinne, T, et al, Acute dislocation of the patella: a prospective review of operative treatment. J Bone Joint Surg 1990; 77B:366–369. ![]()
91. De Cesare, WF, Late results of the Hauser procedure for recurrent dislocation of the patella. Clin Orthop 1979; 140:137–143. ![]()
92. Crossby, E, Insall, JW, Recurrent dislocation of the patella. A study of its pathology and treatment in 106 knees. J Bone Joint Surg 1976; 58A:9–13. ![]()
93. Nikku, R, Nietosvaara, Y, Kallio, PE, et al, Operative versus closed treatment of primary dislocation of the patella. Similar 2-year results in 125 randomized patients. Acta Orthop Scand. 1997;68(5):419–423. ![]()
94. Dandy, DJ, Griffiths, D, Lateral release for recurrent dislocations of the patella. J Bone Joint Surg 1989; 71B:121–125. ![]()
95. Merchant, AC, Classification of patellofemoral disorders. Arthroscopy 1988; 4:235–240. ![]()
96. Ahmed, AM, Burke, DL, Hyder, A, Force analysis of the patellar mechanism. J Orthop Res 1987; 5:69–85. ![]()
97. Paar, O, Bernett, P, Huyer, C, Experiences with patellar chondropathy: etiology, diagnosis and therapy. Int J Sports Med 1986; 6:803–813. ![]()
98. Merchant, AC, Mercer, RL, Jacobsen, RH, Cool, CR, Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg 1974; 56A:1391–1396. ![]()
99. Laurin, CA, Dussault, R, Levesque, HP, The tangential X-ray investigations of the patellofemoral joint. Clin Orthop 1979; 144:16–26. ![]()
100. McNally, EG, Ostlere, SJ, Pal, C, et al, Assessment of patellar maltracking using combined static and dynamic MRI. Eur Radiol. 2000;10(7):1051–1055. ![]()
101. Pookarnjanamorakot, C, Jaovisidha, S, Apiyasawat, P, The patellar tilt angle: correlation of MRI evaluation with anterior knee pain. J Med Assoc Thai. 1998;81(12):958–963. ![]()
102. Hertel, E. Die artroskopische Diagnostik der Chondropathia Patella. Orthop Praxis. 1980; 6:522.
103. Paar, O, Schneider, B, Vergleichende klinische und arthroscopische Untersuchung des Kniegelenkes bei Chondromalacia patellae. Akt Traumatol 1989; 19:142–146. ![]()
104. Sandow, MJ, Goodfellow, JW, The natural history of anterior knee pain syndrome in adolescents. J Bone Joint Surg. 1985;67(1):36–38. ![]()
105. Somes, S, Worrell, TW, Corey, BCD. Effects of patellar taping on patellar position in the open and closed kinetic chain: a preliminary study. J Sports Rehab. 1997; 6:299–308.
106. Derasari, A, Brindle, TJ, Alter, KE, Sheehan, FT, McConnell taping shifts the patella inferiorly in patients with patellofemoral pain: a dynamic magnetic resonance imaging study. Phys Ther. 2010;90(3):411–419. ![]()
107. Lan, TY, Lin, WP, Jiang, CC, Chiang, H, Immediate effect and predictors of effectiveness of taping for patellofemoral pain syndrome: a prospective cohort study. Am J Sports Med. 2010;38(8):1626–1630. ![]()
108. Sale, D, Influence of exercise and training on motor unit activation. Exerc Sports Sci Rev 1987; 5:95–151. ![]()
109. Ingersoll, C, Knight, K, Patellar location changes following EMG biofeedback for progressive resistive exercises. Med Sci Sports Exerc. 1991;23(10):1122–1127. ![]()
110. Hodges, P, Richardson, CA, An investigation into the effectiveness of hip adduction in the optimization of the vastus medialis oblique contraction. Scand J Rehabil Med 1993; 25:57–62. ![]()
111. Ogilvie-Harris, DJ, Jackson, RW, The arthroscopic treatment of chondromalacia patellae. J Bone Joint Surg 1984; 668:660–665. ![]()
112. O’Neill, DB, Open lateral retinacular lengthening compared with arthroscopic release. A prospective, randomized outcome study. J Bone Joint Surg. 1997;79A(12):1759–1769. ![]()
113. Pidoriano, AJ, Fulkerson, JP, Arthroscopy of the patellofemoral joint. Clin Sports Med. 1997;16(1):17–28. ![]()
114. Biedert, R, Friederich, N, Femoropatellar pain syndrome: which operation is still sensible? Ther Umsch. 1996;53(10):775. ![]()
115. Federico, DJ, Reider, B, Results of isolated patellar debridement for patellofemoral pain in patients with normal patellar alignment. Am J Sports Med. 1997;25(5):663–669. ![]()
116. Bandi, W. Die retropatellaren Kniegelenkschäden. Bern: Huber; 1982.
117. Munzinger, U, Bubs, L, Buchmann, R, Das femoropatelläre Schmerzsyndrom. Orthopäde 1985; 14:247. ![]()
118. Clarke, S, Lock, V, Duddy, J, et al, Intra-articular hylan G-F 20 (Synvisc) in the management of patellofemoral osteoarthritis of the knee (POAK). Knee. 2005;12(1):57–62. ![]()
119. Bellamy, N, Campbell, J, Robinson, V, et al, Viscosupplementation for the treatment of osteoarthritis of the knee. Cochrane Database Syst Rev 2005; 2. ![]()
120. Lonner, JH, Patellofemoral arthroplasty. J Am Acad Orthop Surg. 2007;15(8):495–506. ![]()
121. Kirk, KL, Kuklo, T, Klemme, W, Iliotibial band friction syndrome. Orthopedics. 2000;23(11):1209–1214. ![]()
122. Taunton, J, Ryan, M, Clement, D, et al, A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36(2):95–101. ![]()
123. Jones, SL, Bates, BT, Osternig, LR, Injuries to runners. Am J Sports Med. 1978;6(2):40–50. ![]()
124. Orchard, JW, Fricker, PA, Abud, AT, Mason, BR, Biomechanics of iliotibial band friction syndrome in runners. Am J Sports Med. 1996;24(3):375–379. ![]()
125. Renne, JW, The iliotibial band friction syndrome. J Bone Joint Surg 1975; 57A:1110–1111. ![]()
126. Ekman, EF, Pope, T, Martin, DF, Curl, WW, Magnetic resonance imaging of iliotibial band syndrome. Am J Sports Med. 1994;22(6):851–854. ![]()
127. Noble, HB, Hajek, HR, Porter, M. Diagnosis and treatment of iliotibial band tightness in runners. Phys Sports Med. 1982; 10(4):67–74.
128. Noble, CA, Iliotibial band friction syndrome in runners. Am J Sports Med. 1980;8(4):232–234. ![]()
129. Murphy, BJ, Hechtman, KS, Uribe, JW, et al, Iliotibial band friction syndrome: MR imaging findings. Radiology. 1992;185(2):569–571. ![]()
130. Muhle, C, Ahn, JM, Yeh, L, et al, Iliotibial band friction syndrome: MR imaging findings in 16 patients and MR arthrographic study of six cadaveric knees. Radiology. 1999;212(1):103–110. ![]()
131. Nishimura, G, Yamato, M, Tamai, K, et al, MR findings in iliotibial band syndrome. Skeletal Radiol. 1997;26(9):533–537. ![]()
132. Orava, S, Iliotibial tract friction syndromes in athletes. Br J Sports Med 1978; 12:69–73. ![]()
133. Cooper, DL, Fair, J. Trainer’s corner. Hamstring strains. Phys Sportsmed. 1978; 6(8):104.
134. Mann, RA. Biomechanics in running. In: Mack R, ed. American Academy of Orthopedic Surgeons’ Symposium on the Foot and Leg in Running Sports. St Louis: Mosby; 1982:1–9.
135. Stanton, P, Purdam, C, Hamstring injuries in sprinting – the role of eccentric exercise. J Orthop Sports Phys Ther. 1989;10(9):343–349. ![]()
136. Lysholm, J, Wiklander, J, Injuries in runners. Am J Sports Med 1987; 15:168–171. ![]()
137. McMaster, W, Walter, M. Injuries in soccer. Am J Sports Med. 1986; 6(1):293–299.
138. Askling, C, Tengvar, M, Saartok, T, Thorstensson, A, Sports related hamstring strains – two cases with different etiologies and injury sites. Scand J Med Sci Sports. 2000;10(5):304–307. ![]()
139. Burkett, LN, Investigation into hamstring strains: the case of the hybrid muscle. Am J Sports Med 1975; 3:5. ![]()
140. Garrett, WE, Rich, FR, Nikolaous, PK, Volger, JB, Computed tomography of hamstring strains. Med Sci Sports Exer. 1989;21(5):506–514. ![]()
141. Clanton, TO, Coupe, KJ, Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6(4):237–248. ![]()
142. Nikolaous, PK, Macdonald, BL, Glisson, PR, et al, Biomechanical and histological evaluation of muscle after controlled strain injury. Am J Sports Med. 1987;15(1):9–14. ![]()
143. Agre, JC, Hamstring injuries. Proposed aetiological factors, prevention, and treatment. Sports Med. 1985;2(1):21–33. ![]()
144. Worell, TW, Perrin, DH, Hamstring muscle injury: the influence of strength, flexibility, warm-up and fatigue. J Orthop Sports Phys Ther. 1992;16(1):12–18. ![]()
145. David, A, Buchholz, J, Muhr, G, Tear of the biceps femoris tendon. Arch Orthop Trauma Surg. 1994;113(6):351–352. ![]()
146. Lokiec, F, Velkes, S, Schindler, A, Pritsch, M, The snapping biceps femoris syndrome. Clin Orthop 1992; 283:205–206. ![]()
147. Ogden, JA, Subluxation and dislocation of the proximal tibiofibular joint. J Bone Joint Surg 1974; 56A:145–154. ![]()
148. Forster, BB, Lee, JS, Kelly, S, et al, Proximal tibiofibular joint: an often-forgotten cause of lateral knee pain. AJR Am J Roentgenol. 2007;188(4):W359–W366. ![]()
149. Harley, JD, An anatomic arthrographic study of the relationships of the lateral meniscus and the popliteus tendon. Am J Roentgenol 1977; 128:181. ![]()
150. Jones, CD, Keene, GC, Christie, AD, The popliteus as a retractor of the lateral meniscus of the knee. Arthroscopy. 1995;11(3):270–274. ![]()
151. Olson, WR, Rechkemmer, L, Popliteus tendinitis. J Am Podiatr Med Assoc. 1993;83(9):537–540. ![]()
152. Barnett, C, Richardson, AT, The postural function of the popliteus muscle. Ann Phys Med 1953; 17:179. ![]()
153. Peterson, L, Pitman, MI, Gold, J, The active pivot shift: the role of the popliteus muscle. Am J Sports Med 1984; 12:313. ![]()
154. Mann, RA, Hagy, JL, The popliteus muscle. J Bone Joint Surg 1977; 59A:924–927. ![]()
155. Stainier, P. Le Muscle poplité. Cyriax Info. 1991; 3(1):5–7.
156. Mayfield, GW, Popliteus tendon tenosynovitis. Am J Sports Med 1977; 5:31. ![]()
157. Hughston, JC, Jackson, KE, Chronic posterolateral rotatory instability of the knee. J Bone Joint Surg 1985; 67A:351. ![]()