Chapter 618 Disorders of the Conjunctiva
Conjunctivitis
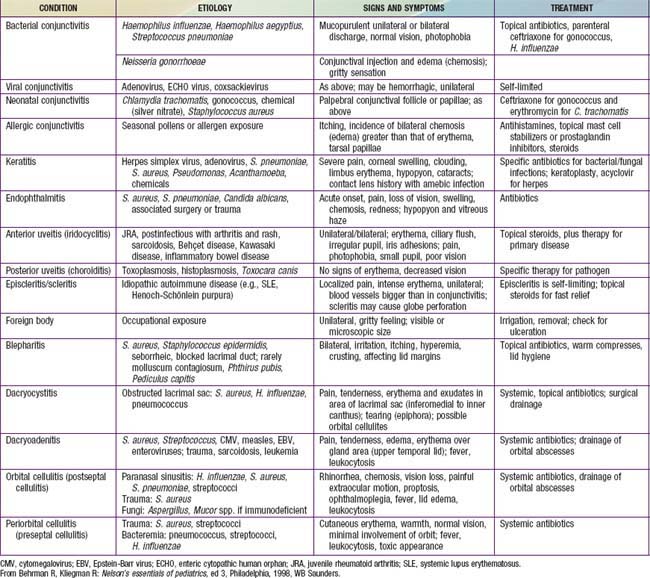
The conjunctiva reacts to a wide range of bacterial and viral agents, allergens, irritants, toxins, and systemic diseases. Conjunctivitis is common in childhood and may be infectious or noninfectious. The differential diagnosis of a red-appearing eye includes conjunctival as well as other ocular sites (Table 618-1).
Vernal Conjunctivitis
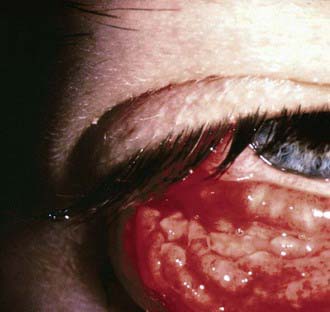
This usually begins in the prepubertal years and may recur for many years. Atopy appears to have a role in its origin, but the pathogenesis is uncertain. Extreme itching and tearing are the usual complaints. Large, flattened, cobblestone-like papillary lesions of the palpebral conjunctivae are characteristic (Fig. 618-1). A stringy exudate and a milky conjunctival pseudomembrane are frequently present. Small elevated lesions of the bulbar conjunctiva adjacent to the limbus (limbal form) may be found. Smear of the conjunctival exudate reveals many eosinophils. Topical corticosteroid therapy and cold compresses afford some relief. Topical mast cell stabilizers or prostaglandin inhibitors are useful when long-term control is needed. The long-term use of corticosteroids should be avoided.
Parinaud Oculoglandular Syndrome
This represents a form of cat-scratch disease and is caused by Bartonella henselae, which is transmitted from cat to cat by fleas (Chapter 201). Kittens are more likely than adult cats to be infected. Humans can become infected when they are scratched by a cat. In addition, bacteria may pass from a cat’s saliva to its fur during grooming. The bacteria can then be deposited on the conjunctiva after rubbing one’s eyes after handling the cat. Lymphadenopathy and conjunctivitis are hallmarks of the disease. Conjunctival granulomas may develop (Fig. 618-2). The course is generally self-limited, but antibiotics may be used in some cases.
Atik B, Thanh TTK, Luong VQ, et al. Impact of annual targeted treatment of infectious trachoma and susceptibility to reinfection. JAMA. 2006;296:1488-1497.
Bremond-Gignac D, Mariani-Kurkdjian P, Beresniak A, et al. Efficacy and safety of azithromycin 1.5% eye drops for purulent bacterial conjunctivitis in pediatric patients. Pediatr Infect Dis J. 2010;29:222-226.
Centers for Disease Control and Prevention. Acute hemorrhagic conjunctivitis outbreaks caused by coxsackievirus A24v—Uganda and Southern Sudan, 2010. MMWR Morb Mortal Wkly Rep. 2010;59:1024.
Centers for Disease Control and Prevention. Outbreak of bacterial conjunctivitis at a college—New Hampshire, January-March, 2002. MMWR Morb Mortal Wkly Rep. 2002;51:205-208.
Centers for Disease Control and Prevention. Acute hemorrhagic conjunctivitis outbreak caused by coxsackievirus A24—Puerto Rico, 2003. MMWR Morb Mortal Wkly Rep. 2004;53:632.
Chang DC, Grant GB, O’Donnell K, et al. Multistate outbreak of fusarium keratitis associated with use of a contact lens solution. JAMA. 2006;296:953-963.
Everitt HA, Little PS, Smith PWF. A randomised controlled trial of management strategies for acute infective conjunctivitis in general practice. BMJ. 2006;333:321-324.
House JI, Ayele B, Porco TC, et al. Assessment of herd protection against trachoma due to repeated mass antibiotic distributions: a cluster-randomised trial. Lancet. 2009;373:1111-1118.
The Medical Letter. Ophthalmic besifloxacin (Besivance). Med Lett. 2009;51:101-102.
The Medical Letter. Ophthalmic azithromycin (Azasite). Med Lett. 2008;50:1279-1280.
Meltzer JA, Kunkov S, Crain EF. Identifying children at low risk for bacterial conjunctivitis. Arch Pediatr Adolesc Med. 2010;164:263-267.
O’Hara MA. Ophthalmia neonatorum. Pediatr Clin North Am. 1993;40:715.
Porco TC, Gebre T, Ayele B, et al. Effect of mass distribution of azithromycin for trachoma control on overall mortality in Ethiopian children. JAMA. 2009;302:962-968.
Rietveld RP, ter Riet G, Bindels PJE, et al. Predicting bacterial cause in infectious conjunctivitis: cohort study on informativeness of combinations of signs and symptoms. Br Med J. 2004;329:206-208.
Rose PW, Hamden A, Brueggemann AB, et al. Chloramphenicol treatment for acute infective conjunctivitis in children in primary care: a randomized double-blind placebo-controlled trial. Lancet. 2005;366:37-42.
Shiuey Y, Ambati BK, Adamis AP, et al. A randomized, double-masked trial of topical ketorolac versus artificial tears for treatment of viral conjunctivitis. Ophthalmology. 2000;107:1512-1517.
Weiss A, Brinser JH, Nazar-Stewart V. Acute conjunctivitis in childhood. J Pediatr. 1993;122:10-14.