Chapter 64 Diseases of the Thoracic Cage and Respiratory Muscles
Respiratory Muscle Pump
The respiratory system is made up of two main components: the respiratory muscle pump, which facilitates airflow, thereby enabling ventilation, and the lungs, which support pulmonary gas exchange (see Chapter 6 for more detailed explanations and for respiratory muscle testing). The respiratory muscle pump itself is made up of the inspiratory muscles, the diaphragm and extradiaphragmatic accessory muscles, and the expiratory muscles, principally the abdominal wall muscles. Inspiration is an active process in which contraction of the diaphragm forces the abdominal contents in an anterocaudal direction to allow the volume of the chest cavity to increase. This expansion, in turn, generates a negative subatmospheric pressure to form a pressure gradient that drives air into the lungs. At rest, expiration is a passive process with the elastic properties of the chest wall and lungs providing the recoil forces that allow the lung volume to return to the functional residual capacity. During exercise and forced expiratory maneuvers (e.g., coughing), however, contraction of the abdominal muscles occurs, pushing the diaphragm upward in the absence of flow limitation.
Clinical Consequences of Respiratory Muscle Pump Imbalance
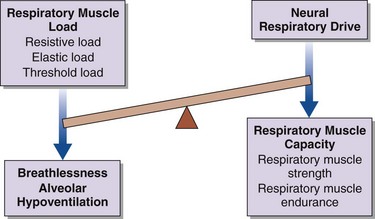
Breathlessness, alveolar hypoventilation and hypercapnic respiratory failure result from an imbalance between the respiratory muscle load, capacity, and neural respiratory drive (Figure 64-1). By using this model the physician can develop a simple clinical tool to assess the breathless patient and the patient in chronic respiratory failure. More commonly, in patients with restrictive lung disease, the reduction in capacity occurs as a consequence of intrinsic muscle weakness. On occasion, however, capacity may be relatively preserved, but in the context of a significant respiratory muscle load or poor orientation of the inspiratory muscles (e.g., kyphoscoliosis), this may limit the pressure-generating capacity, so that dyspnea and alveolar hypoventilation can develop subsequently. In critically ill patients, the respiratory muscle weakness may be transient and reversible, such as occurs in respiratory acidosis, hypokalemia, and hypophosphatemia (Box 64-1).
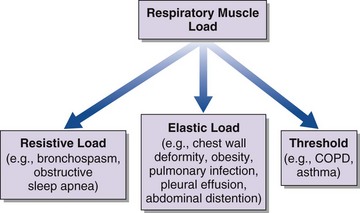
An increase in respiratory muscle load occurs in patients with increased airway resistance, chest wall deformity, or obesity. Any of these conditions will accelerate the onset of dyspnea and alveolar hypoventilation in patients with respiratory muscle weakness (Figure 64-2).
Assessment of the Respiratory Muscle Pump
Clinical Features
As always, a detailed history will facilitate making a correct diagnosis (Table 64-1). Of particular importance is the rate of onset of symptoms. Acute respiratory muscle weakness tends to progress rapidly, culminating in a medical emergency requiring intubation and mechanical ventilation. Some causes of acute respiratory muscle weakness, such as an acute myasthenic crisis or Guillain-Barré disease, may be reversible, and it is important to facilitate invasive respiratory support in the acute setting until a diagnosis can be made and appropriate therapies initiated. In chronic respiratory failure, the onset may not be clear, but clues to the course of events can be gained from the history. Often patients will describe dyspnea on exertion, but if peripheral muscle weakness precedes respiratory muscle weakness, the consequent loss of significant locomotor function will not permit exertion of sufficient degree to produce dyspnea. Classic features of diaphragm weakness are not always present in patients with generalized neuromuscular disease but may include dyspnea on lying supine, on bending forward, or on immersion in water above the midchest level. If respiratory weakness is severe, patients also may describe symptoms of nocturnal hypoventilation, such as extensive daytime somnolence, reduced concentration, and morning headaches that typically resolve within 30 minutes of waking. Specifically, in the pediatric and adolescent populations, clinicians should be alerted to more subtle clinical features such as failing school performance, recurrent episodes of chest sepsis, reduction in appetite, and weight loss.
Table 64-1 Important Clinical Features in Diseases of the Thoracic Cage and Respiratory Muscles
| Disorder | Clinical Manifestations |
|---|---|
| Sleep-disordered breathing | Morning headache, daytime sleepiness, disrupted sleep pattern, impaired intellectual function, generalized fatigue, loss of appetite and weight |
| Respiratory muscle weakness | Orthopnea, breathlessness on immersion in water, breathlessness on leaning forward, breathlessness on exertion, poor cough, poor chest expansion, paradoxical abdominal motion during inspiration (inward motion of the anterior abdominal wall due to diaphragm weakness), abdominal muscle recruitment in expiration |
| Bulbar dysfunction | Low volume voice, difficulty swallowing, drooling, difficulty clearing secretions, poor cough, staccato/slurred speech, coughing on swallowing |
Pulmonary Function Tests
The pattern of respiratory muscle weakness must be considered in interpreting results of pulmonary function tests in patients with chest wall disease and respiratory muscle weakness. Although total lung capacity (TLC) and VC are reduced in patients with predominantly inspiratory muscle weakness and combined inspiratory and expiratory muscle weakness, the pattern of weakness influences functional residual capacity (FRC), residual volume (RV), overall gas transfer (DLCO), and gas transfer corrected for alveolar volume (Table 64-2).
Table 64-2 Pulmonary Function Tests for Patients with Predominantly Inspiratory Muscle Weakness and Combined Inspiratory/Expiratory Muscle Weakness
| Inspiratory Muscle Weakness | Combined Inspiratory/Expiratory Muscle Weakness |
|---|---|
| Reduced VC | Reduced VC |
| Fall in supine VC >20% | N/A |
| FEV1/FVC ratio >80% | FEV1/FVC ratio >80% |
| Reduced TLC | Reduced TLC |
| Normal RV | Increased RV |
| Reduced FRC | Increased FRC |
| Reduced TLCO | Reduced TLCO |
| “Supranormal” KCO | Reduced KCO |
FEV1, forced expiratory volume in 1 second FRC, functional residual capacity; FVC, forced vital capacity; KCO, gas transfer coefficient corrected for alveolar volume; N/A, not available; RV, residual volume; TLC, total lung capacity; TLCO, overall gas transfer; VC, vital capacity.
Tests of Respiratory Muscle Function
Because respiratory muscle contraction generates tension, the consequent pressure change that occurs can serve as an in vivo measure for the quantification of respiratory muscle strength. In addition, recent developments have expanded the current understanding of the mechanical actions and interactions of the respiratory muscles. A greater emphasis has been placed on assessing and quantifying respiratory muscle strength and pulmonary mechanics in a variety of patient groups, including children, adolescents, and adults (see Chapter 6 for a more detailed discussion).
Sniff Inspiratory Pressure
The rapid inspiratory effort of a sniff maneuver (see Chapter 6) is accompanied by momentary equilibration of intrathoracic and upper airway pressures. This equilibration occurs above a pressure of 10 to 12 cm H2O, so employing sniff nasal pressure (Pnsn) allows noninvasive measurement of inspiratory muscle strength. Pnsn is a particularly useful additional investigation in patients with a low or equivocal PImax to confirm or exclude the presence of inspiratory muscle weakness.
Maximum Transdiaphragmatic Pressure Measurements
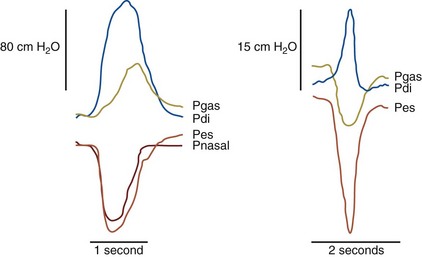
The previously described tests provide data only on global respiratory muscle function, rather than on diaphragm function itself. To specifically assess diaphragm function, transdiaphragmatic pressure (Pdi) is measured by placement of a pressure-monitoring catheter in both the esophagus and stomach, to provide measurement of the esophageal and gastric pressures (Figure 64-3).
Although transdiaphragmatic pressure during a maximal static maneuver (Pdimax) has been reported, this maneuver gives a wide normal range in naive (i.e., previously untested) subjects. An alternative is to obtain maximal sniff transdiaphragmatic pressure (Pdisn), which has gained recognition in clinical practice not only because it is a familiar maneuver but because it measures both Pessn and Pdisn, providing data on global inspiratory muscle and diaphragm strength (Figure 64-4).
Twitch Transdiaphragmatic Pressure
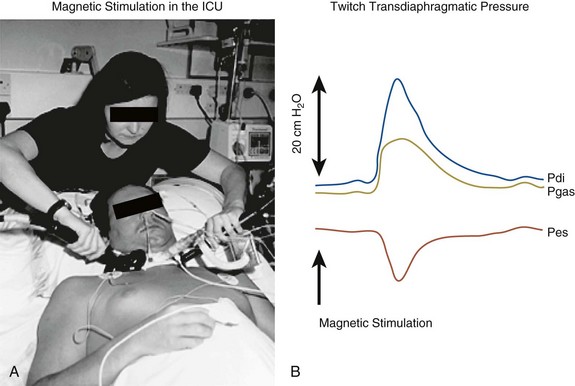
Clinical magnetic stimulation to allow bilateral stimulation of the roots supplying the phrenic nerves was first reported in 1989. Subsequent work has demonstrated its clinical usefulness, and this technique provides a nonvolitional assessment of diaphragm strength in a number of patient groups, including children and adolescents, as well as critically ill patients in intensive care in whom motivation and cooperation to perform maximal volitional maneuvers are difficult to achieve. In addition to improved tolerability, magnetic stimulation has advantages over electrical stimulation in that it is easier to stimulate the phrenic nerves and reduces the technical difficulties involved in isolation of the nerve (Figure 64-5). Further details can be found in the recommended reading section.
Sleep Studies
Overnight oximetry and capnometry constitute an essential part of the assessment for the early detection of nocturnal hypoventilation. These are recommended investigations in patients with neuromuscular and chest wall disease who report symptoms of sleep-disordered breathing (see Table 64-1). Although some investigators advocate the use of polysomnography, including an electroencephalogram, to confirm and quantify arousals during respiratory events, this study is not necessary in the routine clinical management of these patients. Nocturnal hypoventilation can be managed simply with overnight titration of ventilatory support to a defined level of hypercapnia, irrespective of the sleep stage of the patient.
Respiratory Presentations of Neurologic and Chest Wall Disease
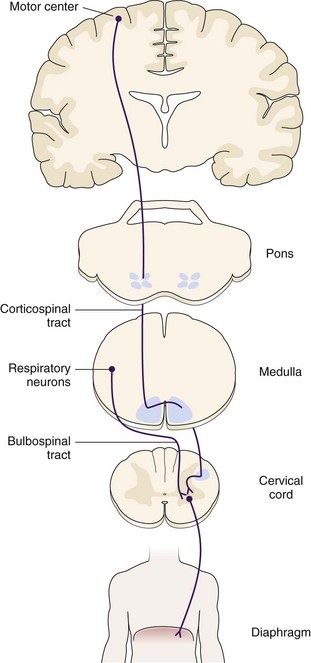
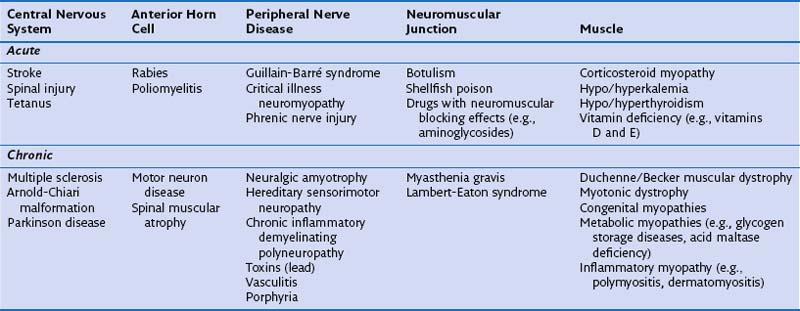
The remainder of this chapter describes specific neurologic/neuromuscular disorders and chest wall diseases, as well as obesity, recognized to be associated with restrictive lung disease. These conditions are divided into acute and chronic presentations (Table 64-3), and the neuromuscular conditions are discussed in the context of the disease and grouped according to their impact on the relevant portion of the anatomic pathway from the central cortex to the peripheral muscle (Figure 64-6).
Table 64-3 Acute and Chronic Presentations of Neuromuscular Disorders From Central Cortex to Peripheral Muscle
Acute Disorders Affecting the Central Nervous System
Stroke
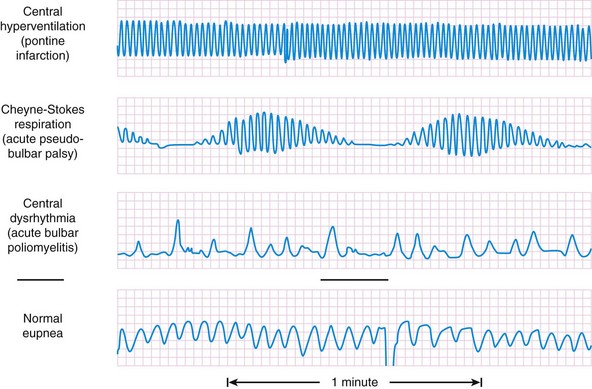
Certain classic breathing patterns (Figure 64-7) are considered to reflect aspects of central nervous system pathology, though these are relatively rare in mainstream respiratory clinical practice. These include (1) central neurogenic hyperventilation resulting from a pontine lesion with hyperventilation present throughout both sleep and wakefulness; (2) cluster breathing caused by a mid–brain stem lesion, with periods of hyperventilation alternating with distinct periods of apnea; (3) apneustic breathing as a consequence of damage to the caudal pons with prolonged pauses after each inspiratory breath resulting in hypoventilation; and (4) ataxic breathing observed in patients with cortical lesions of the medulla, which is characterized by an erratic breathing pattern, which differs from the other breathing patterns in having no clear-cut cyclic nature.
Chronic Disorders Affecting the Central Nervous System
Parkinson Disease
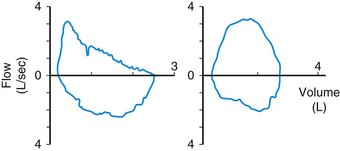
Patients with Parkinson disease commonly exhibit involuntary movements affecting the upper airways. A saw-tooth flutter wave often is present on the flow-volume loop trace (Figure 64-8); this aberration results from repetitive adduction of the vocal cords, occurring at the same frequency as a tremor of 4 to 8 Hz. It can cause significant difficulties if tracheal intubation is required. Obstructive sleep apnea is observed more frequently in patients with Parkinson disease, although patients also may experience sleep fragmentation because of pain or dystonias. Finally, the related condition of multisystem atrophy is characterized by features of Parkinson disease and autonomic failure. It has been associated with irregular breathing patterns and life-threatening upper airway obstruction related to glottis and vocal cord dysfunction narrowing during sleep.
Chronic Disorders Affecting the Anterior Horn Cells
Motor Neuron Disease
Motor neuron disease (MND), also known as amyotrophic lateral sclerosis (ALS), has a European annual incidence of approximately 2 to 3 cases per 100,000 population. Only 1% to 3% of MND cases manifest with respiratory muscle weakness and acute respiratory failure. It is uncommon for patients to describe the classical signs of respiratory muscle weakness (see Table 64-1) as a presenting complaint, but respiratory physicians should consider this diagnosis in patients with coexisting muscle wasting and weakness. A more common presentation is one of exertional and positional dyspnea, ineffective cough, and low speech volume in a patient who has already received the diagnosis. Bulbar features, notably aspiration, are common in advanced disease. When muscle weakness is severe, the patient may report disrupted sleep and excessive fatigue, morning headaches and confusion. Physical findings may include tachypnea at rest, inability to complete full sentences, use of accessory muscles, and abdominal inspiratory paradox.
Chronic Disorders Affecting the Peripheral Nerves
Chronic Muscle Disorders
Duchenne Muscular Dystrophy
Respiratory support also will include secretion clearance, specifically during any episode of pneumonia, with the introduction of a mechanical insufflation-exsufflation device to enhance cough function and secretion management (see earlier under “Cough Peak Flow”). As bulbar function declines, in addition to a reduction in effective cough, patients will be at increased risk for aspiration, and these swallowing problems reduce nutritional intake, resulting in weight loss. Early gastrostomy feeding tube insertion, accomplished with endoscopic or radiologic guidance, is recommended, although evidence supporting this practice is limited. It is possible, with appropriate expertise, to do such procedures with sedation using noninvasive ventilation alone in patients with established respiratory failure.
Thoracic Disorders
Chest wall deformities, such as kyphosis, scoliosis, and kyphoscoliosis, and obesity hypoventilation syndrome are described in detail in Chapters 63 and 62, respectively. Obesity itself also has clinical consequences for pulmonary function, and an overview of this issue is presented next, with specific emphasis on pulmonary function tests, pulmonary mechanics, hypercapnic ventilatory response, and respiratory muscle strength.
American Thoracic Society/European Respiratory Society. ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166:518–624.
Bassetti CL, Gugger M. Sleep disordered breathing in neurologic diseases. Swiss Med Wkly. 2002;132:109–115.
Hart N. Respiratory failure. Clin Med. 2008;36:242–245.
Hart N, Polkey MI. Investigation of respiratory muscle function. Clin Pulm Med. 2001;8:180–187.
Laghi F, Tobin MJ. Disorders of the respiratory muscles. Am J Respir Crit Care Med. 2003;168:10–48.
Luo YM, Moxham J, Polkey MI. Diaphragm electromyelography using an oesophageal catheter: current concepts. Clin Sci (Lond). 2008;115:233–244.
Murphy P, Polkey MI, Hart N. Diagnostic tests in the assessment of patients for home mechanical ventilation. In: Elliott MW, Nava S, Schönhofer B. Principles and practices of non-invasive ventilation and weaning. London: Hodder Arnold; 2010:151–166.
Mustfa N, Moxham J. Respiratory muscle assessment in motor neurone disease. Q J Med. 2001;94:497–502.
Polkey MI, Lyall RA, Davidson AC, et al. Ethical and clinical issues in the use of home non-invasive mechanical ventilation for the palliation of breathlessness in motor neurone disease. Thorax. 1999;54:367–371.
Polkey MI, Lyall RA, Moxham J, Leigh PN. Respiratory aspects of neurological disease. J Neurol Neurosurg Psychiatry. 1999;66:5–15.
Polkey MI, Moxham J. Clinical aspects of respiratory muscle dysfunction in the critically ill. Chest. 2001;119:926–939.
Tobin M. Principles and practices of mechanical ventilation, ed 2. New York: McGraw-Hill; 2006.