Chapter 10 Discontinuation of Mechanical Ventilation
2 When should patients receiving mechanical ventilation be assessed for ventilator discontinuation?
3 How, exactly, should this assessment be done?
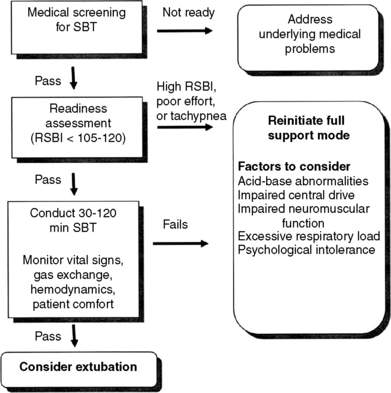
As of yet, no systematic weaning protocol has been agreed on. However, most protocols have a stepwise assessment that varies in the details. The above criteria should be assessed daily as a wean screen. For the patients who pass the daily wean screen, there is first an initial brief trial or readiness assessment during which patients are closely observed for 1 to 5 minutes while receiving minimal or no support (continuous positive airway pressure [CPAP] ≤ 5 cm H2O, T-piece trial, 5 to 7 cm H2O pressure support from the ventilator, or automatic tube compensation) to assess their ability to undergo a formal spontaneous breathing trial (SBT). If the patient does well during the readiness assessment, an SBT is performed for between 30 and 120 minutes. During this time patients are closely monitored for signs of respiratory insufficiency, hemodynamic deterioration, problems with gas exchange, or patient discomfort. Full ventilatory support is promptly reinitiated if problems develop. Successfully completing an SBT is highly predictive of successful ventilator discontinuation. These steps are illustrated in Figure 10-1.
4 What is the rapid shallow breathing index (RSBI)? What does it predict?
5 To which mode should the ventilator be set during the SBT?
8 What do you do with patients who have failure during the SBT?
 Return the patient to a full ventilatory support mode (e.g., assist/control).
Return the patient to a full ventilatory support mode (e.g., assist/control).
 Perform a comprehensive review of potential contributing factors to the failure.
Perform a comprehensive review of potential contributing factors to the failure.
To sustain spontaneous ventilation successfully, patients must have an intact respiratory center drive and adequate neuromuscular function and not have excessive loads on the respiratory muscles. Box 10-1 provides one method of systematically reviewing possible causes of failure during an SBT. Patients often have more than one cause for failure to wean, and correction of these factors may require multiple interventions. In general, it is recommended to wait 24 hours before attempting another SBT.
1. The patient has an increasing PaCO2 without increases in respiratory effort or rate.
2. The patient has tachypnea, tachycardia, or distress.
 Diaphragmatic paresis or paralysis due to phrenic nerve injury resulting from cold cardioplegia or thoracic or neck surgery
Diaphragmatic paresis or paralysis due to phrenic nerve injury resulting from cold cardioplegia or thoracic or neck surgery Air trapping and increased threshold load due to positive residual pressures (particularly in patients with COPD)
Air trapping and increased threshold load due to positive residual pressures (particularly in patients with COPD) Decreased respiratory system compliance (e.g., pulmonary edema, fibrosis, pneumonia, abdominal distention, thoracic cage abnormalities, pleural effusions)
Decreased respiratory system compliance (e.g., pulmonary edema, fibrosis, pneumonia, abdominal distention, thoracic cage abnormalities, pleural effusions)COPD, Chronic obstructive pulmonary disease.
10 What about using noninvasive ventilation (NIV) for patients who have respiratory failure after extubation?
12 Should these patients be managed with different modes of ventilation?
Patients who are ventilator dependent after 14 to 21 days despite improvement in disease state may require different management strategies. Multidisciplinary rehabilitation with focus on ventilatory support, nutrition, physical therapy, and psychosocial support are all important aspects. Gradual reduction in ventilatory support may be used in PMV patients. Many clinicians wean patients to approximately 50% of their maximal support levels without using SBTs. Once at the 50% level, daily SBTs are started. Ventilatory support should be withdrawn gradually during the day, with progressively longer SBTs, allowing rest and sleep on full support modes at night. Once the patient tolerates spontaneous ventilation throughout the day, withdrawal of nocturnal ventilation may proceed relatively quickly. The success rate of ventilator discontinuation is only 50% to 60%. As in acutely ill patients, a therapist-driven protocol approach to weaning appears to improve outcomes in comparison with clinical judgment alone. Clinicians should continue efforts to identify and correct physiologic reasons for the patient’s inability to resume spontaneous ventilation (see Box 10-1).
13 Why is there such an emphasis on protocols?
Key Points Discontinuation of mechanical ventilation
1. Daily systematic assessments of patients receiving mechanical ventilation for the ability to breathe spontaneously are important in achieving timely discontinuation of ventilator support and reducing complications related to artificial airways and mechanical ventilation.
2. A respiratory therapist–driven or nurse-driven protocol for this daily assessment can safely reduce the duration of mechanical ventilation and performs better than standard physician assessments.
3. Sedation and analgesia should be minimized or interrupted on a daily basis.
4. Before removing the artificial airway, patients should be able to protect their airway, should demonstrate good cough effort, and should not have copious secretions.
5. Systematic attention to medical conditions that impair spontaneous breathing, such as left ventricular dysfunction, muscle fatigue, and metabolic abnormalities, should be part of this daily assessment. This can guide the medical care for those patients in whom a spontaneous breathing trial fails or who require prolonged ventilatory support.
1 Blackwood B., Alderdice F., Burns K.E., et al. Protocolized versus non-protocolized weaning for reducing the duration of mechanical ventilation in critically ill adult patients. Cochrane Database Syst Rev. 5, 2010. CD006904, 2010
2 Burns K.E., Adhikari N.K., Keenan S.P., et al. Noninvasive positive pressure ventilation as a weaning strategy for intubated adults with respiratory failure. Cochrane Database Syst Rev. 8, 2010. CD004127, 2010
3 El-Khatib M.F., Bou-Khalil P. Clinical review: liberation from mechanical ventilation. Crit Care. 2008;12:221.
4 Ely E., Meade M., Haponik E., et al. Mechanical ventilator weaning protocols driven by nonphysician health-care professionals: evidence-based clinical practice guidelines. Chest. 2001;120(6 Suppl):454S–463S.
5 Epstein S.K., Ciubotaru R.L., Wong J.B. Effect of failed extubation on the outcome of mechanical ventilation. Chest. 1997;112:186–192.
6 Esteban A., Anzueto A., Frutos F., et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287:345–355.
7 Jackson D.L., Proudfoot C.W., Cann K.F., et al. A systematic review of the impact of sedation practice in the ICU on resource use, costs and patient safety. Crit Care. 2010;14:R59. Available online at http://ccforum.com/content/14/2/R59. Accessed February 4, 2012
8 Kress J., Pohlman A., O’Connor M., et al. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med. 2000;342:1471–1477.
9 Krishan J., Moore D., Robeson C., et al. A prospective, controlled trial of a protocol-based strategy to discontinue mechanical ventilation. Am J Respir Crit Care Med. 2004;169:673–678.
10 MacIntyre N. Discontinuing mechanical ventilatory support. Chest. 2007;132:1049–1056.
11 MacIntyre N., Epstein S., Carson S., et al. Management of patients requiring prolonged mechanical ventilation: report of a NAMDRC consensus conference. Chest. 2005;128:3937–3954.
12 MacIntyre N.R., Cook D.J., Ely E.W., et al. Evidence based guidelines for weaning and discontinuing mechanical ventilation: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest. 2001;120(6 Suppl):375S–395S.
13 Patel K.N., Ganatra K.D., Bates J.H., et al. Variation in the rapid shallow breathing index associated with common measurement techniques and conditions. Respir Care. 2009;54:1462–1466.
14 Tobin M. Advances in mechanical ventilation. N Engl J Med. 2001;344:1986–1996.
15 Yang K.L., Tobin M.J. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med. 1991;324:1445–1450.