Chapter 34 Disaster Preparedness, Cardiopulmonary Resuscitation, and Airway Management
V. Hospital Incident Command System
VI. Operating Room Preparation
VII. Anesthetic and Resuscitation Techniques
VIII. Planning and Preparation
IX. Basic Life Support and Cardiopulmonary Resuscitation Guidelines
X. Initial Airway Management During Cardiopulmonary Resuscitation
XI. Advanced Airway Management During Cardiopulmonary Resuscitation
XII. Alternative Methods of Oxygen Delivery During Cardiopulmonary Resuscitation
XIII. Challenges of Airway Management During Cardiopulmonary Resuscitation
I Introduction
Disasters happen. They happen frequently, but they are not uniformly distributed in time and geography. Any particular place tends to experience them infrequently. Although there are many definitions of disaster, the most common medical definition of a disaster is an “event that results in casualties that overwhelm the health care system in which the event occurs.”1 Typically, disasters degrade the fundamental infrastructure necessary for a viable economy and civil society. This disruption magnifies the impact of the event by widening the gap between needed and available resources (Fig. 34-1).
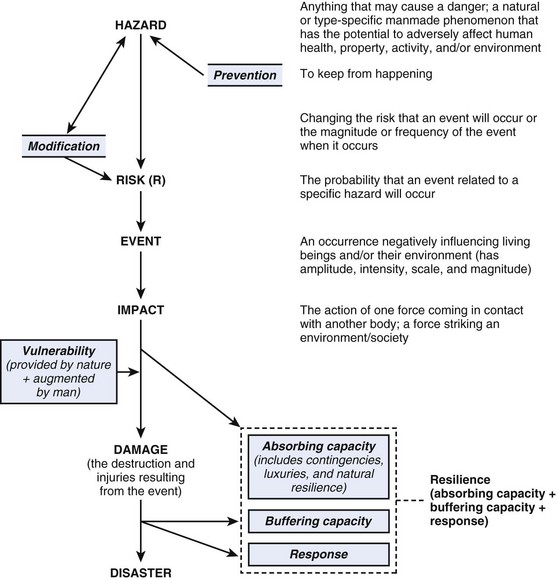
Figure 34-1 Standardized definitions of terms used to communicate by the various disciplines involved in disasters.
(Modified from Task Force for Quality Control of Disaster Medicine (TFQCDM)/World Association for Disaster and Emergency Medicine (WADEM): Health disaster management: guidelines for evaluation and research in the Utstein style, vol 1. Available at http://www.wadem.org/guidelines/chapter_3.pdf [accessed March 2012].)
II Disaster Triage
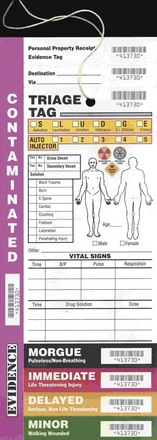
Triage is the act of sorting casualties. It implies that numbers of casualties exceed available medical resources. During routine circumstances in modern hospitals, the sickest patients receive the highest priority. During mass casualty events, patients are sorted into several levels based on the ability to help the greatest number while conserving scarce resources. Several systems are in use, and all are based loosely on military systems but have not been scientifically validated.2 Patients who require intense resources with little likelihood of salvage are called expectant. They are expected to die and are given comfort measures only. Those with severe but treatable conditions are marked as immediate. Wounded who can wait are referred to as delayed or minimal (Fig. 34-2). Because triage depends on resources, repeat triage should occur when there is a change in patient status, available care, and transfer to another facility.
III Surge Capacity
The concept of surge capacity is important beyond the emergency department. As the number of arriving patients peaks, the ability to expand services and number of beds is critical. Although temporarily increased capacity can result from cancellation or delay of routine patient load, there ultimately must be an expansion of overall facility capacity or introduction of new facilities into the system.3 This can be done by adding portable facilities, recruiting administrative space within the institution, or using municipal buildings (e.g., schools) for treatment space. Unless providers and supplies can be augmented from outside the disaster zone, creative allocation of resources is the only option. The Agency for Healthcare Research and Quality (AHRQ) has developed an online, disaster-specific hospital surge model that can be used for planning.4
IV Altered Standards of Care
In large-scale disasters, an altered standard of care must be implemented. Chronic diseases such as diabetes, hypertension, and hypothyroidism become uncontrolled as the medication supply is depleted. Life-threatening conditions such as coronary ischemia and dialysis-dependent renal failure can no longer be treated adequately. Scarce resources are more appropriately directed to others. Loss of sanitation and hygiene increase the frequency of wound infection, respiratory diseases and gastrointestinal diseases. Acute shortages of antibiotics can become a major limitation, and determination of the standard of care can be set regionally (e.g., in pandemic influenza) or done on an ad hoc basis.5
V Hospital Incident Command System
All U.S. hospitals are required by The Joint Commission (TJC), formerly the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), and by governmental policies to have disaster plans prepared and tested twice per year. The most accepted standard for hospital disaster response is the Hospital Incident Response System (HICS) (http://www.hicscenter.org/index.php [accessed March 2012]). HICS consists of a command and control framework headed by the incident commander and prioritized task lists for each designated subordinate. Modeled on military combat systems and perfected by the California Fire Service, HICS is a time-tested system.
VI Operating Room Preparation
On notification of a disaster situation, the local institution’s operating room disaster standard operating procedure should be used.6 HICS does not delineate how a surgical service should organize the operating room. The HICS model should be used with a single chief of the operating room, preferably a senior anesthesiologist who is in communication with the emergency department, intensive care units, postanesthesia care unit, the chief of perioperative nursing, and the hospital’s surgical chief.
VII Anesthetic and Resuscitation Techniques
A Emergency Airway Management and Ventilation
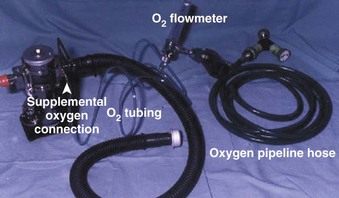
Tracheal intubation, except when performed blindly, requires a light source and a laryngoscope. Typically, the intubated patient requires controlled ventilation. Use of a surgical airway is rarely indicated, but it remains an option in selected cases. The expenditure of effort and resources for such a patient may not be consistent with the most good for the greatest number, but care should not be denied to a salvageable casualty when time and resources are available. Advanced techniques are only as good as their availability and the skill of the practitioner. Several types of portable ventilators can be used during a respiratory disease pandemic if normal infrastructure (i.e., electrical power and compressed gas) is available. Figure 34-3 shows a portable ventilator.
B Anesthetic Techniques
Choice of anesthetic technique depends on the resources available and the skill of the practitioner. Total intravenous anesthesia (TIVA) with local anesthetic infiltration has been the default option when resources are constrained. Needed quantities of parenteral agents such as ketamine, narcotics, benzodiazepines, propofol, and barbiturates are compact, easy to transport, and easy to store. Judicious infiltration of local anesthetics can provide acceptable conditions for short procedures when used alone. Baker and colleagues7 described three levels of military anesthesia care on the battlefield: sevoflurane inhalation using standard anesthesia machines at the highest level, drawover vaporizers at the intermediate level, and TIVA at the lowest level. Regional anesthesia, particularly nerve blocks placed with a nerve stimulator or ultrasound if available, has enjoyed popularity in war zones and during the 2010 Haiti earthquake.8
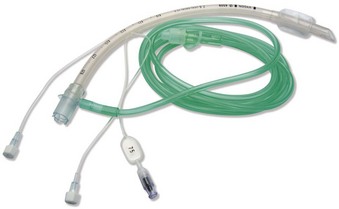
The Omeda Universal Portable Anesthesia Complete (U-PAC) drawover anesthesia system (GE Healthcare, Fairfield, CT) has been deployed with the U.S. military. Drawover features include durability, compactness, portability, low capital investment, low operating expense, and no requirement for compressed gas or electricity.9 Components of a drawover system include a vaporizer powered by patient respiration or a self-inflating bag with a one-way valve (Fig. 34-4).
VIII Planning and Preparation
The key to successful management during a disaster is good preparation and planning, which starts with a realistic understanding of the situation. When preparing to meet the needs of a distant event, the response should be tailored to the acute and endemic disease spectrum, climate, degree of infrastructure impairment, and cultural particulars of the affected area. An area with inadequate transportation; total loss of power, water, and sanitation; and tenuous security after a major earthquake has significantly different needs from an area experiencing pandemic influenza (Fig. 34-5). Logistics are always the major limiting factor. Resupply may be uncertain or nonexistent. Local manufacture of substitutes (e.g., boiled linen for sterile dressings) may be the only option. Compressed gas and intravenous fluids are heavy, bulky, and in short supply. Lack of refrigeration limits use of certain pharmaceuticals. Modern sterilization methods may not be available, requiring improvisation. Boiling metal instruments for 15 to 30 minutes renders a high degree of asepsis. After thorough cleaning with soap or detergent, soaking heat-intolerant equipment in common household bleach (i.e., sodium hypochlorite solution) is an excellent means of sterilization, but it tends to degrade many materials after repeated application.
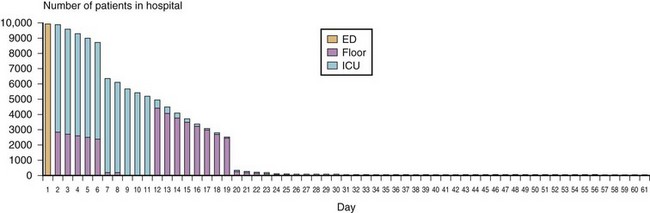
(From U.S. Department of Health and Human Services: Hospital surge model. Available at http://www.hospitalsurgemodel.org [accessed March 2012].)
A The U.S. National Disaster System
The National Incident Management System (NIMS) provides a systematic,10 proactive approach to guide all levels of governmental departments and agencies, nongovernmental organizations, and the private sector to work seamlessly to prevent, protect against, respond to, recover from, and mitigate the effects of incidents, regardless of cause, size, location, or complexity, to reduce the loss of life and property and harm to the environment. NIMS works hand in hand with the National Response Framework (NRF).11 NIMS provides the template for the management of incidents, and the NRF provides the structure and mechanisms for national-level policy for incident management.
The National Disaster Medical System (NDMS) is a nationwide partnership designed to deliver quality medical care to the victims of and the responders to a domestic disaster.12 NDMS provides state-of-the-art medical care under any conditions at the disaster site, in transit from the impacted area, and in participating definitive care facilities.
F Anticipating Surprise
Expect the unexpected. Failure to predict surprise can result in panic, paralysis, and a sense of defeat. Developing a psychology to anticipate unexpected occurrences and then training for such contingencies creates an atmosphere of resilience. Attitude is probably the most important characteristic that determines outcome. In retrospect, most surprises can be seen as having indicators that were overlooked or recognized but rejected as unbelievable. Typically, they are high-impact, low-probability events.13
G Decontamination, Personal Protective Equipment, and Isolation for Chemical, Biologic, and Radiologic Events
It is important to distinguish between decontamination and isolation. Infectious patients cannot be decontaminated because the infection is internal. Patients with external chemical and radiologic contamination should be decontaminated to minimize the patient’s exposure to the agent and the exposure of the treating staff. Removal of clothing and washing with copious amounts of water (with or without soap) constitute the best universal decontamination strategy. This can be accomplished for mass casualties through a formal decontamination system or by any improvised method that accomplishes the goal. Employing a method for assessing the effectiveness of decontamination (e.g., testing patients after decontamination with a Geiger counter, chemical meter, or using a surrogate tracer) can increase confidence in the system, but studies have consistently shown several orders of magnitude of contamination reduction using only clothing removal and shower. The main exception to this rule is a gross level of contamination by persistent chemicals used by the military, such as thickened nerve agents and some vesicants. These scenarios are more likely to occur in large-scale chemical warfare, which is unlikely to occur because most armies have eliminated their inventories. First responders at the hospital level typically wear level C PPE, whereas first responders at a site of high agent concentration often wear level A or B PPE.14
Use of PPE imposes a burden on the caregiver. Besides the psychological impact and heat stress, there are measurable impediments to vision, hearing, communications, and manual dexterity. Suyama and colleagues found that for a non–PPE-wearing operator,15 needle-to-skin time favored intravenous placement over intraosseous but that an intraosseous approach provided faster vascular access when wearing PPE. The affect of PPE on airway management seems less clear. Although Greenland and coworkers found that PPE affected bronchoscopy but not intubation,16 Castle and colleagues found that chemical-biologic-radiologic-nuclear (CBRN) PPE significantly impaired intubation but not laryngeal mask airway placement while kneeling,17 sitting, or lying on the floor.
IX Basic Life Support and Cardiopulmonary Resuscitation Guidelines
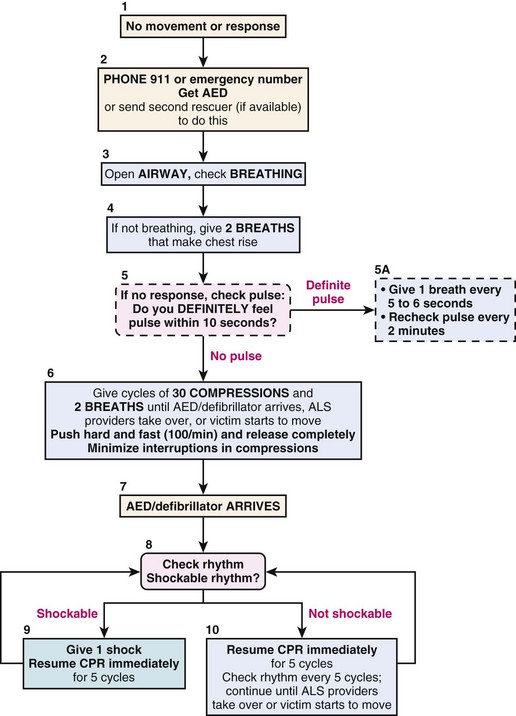
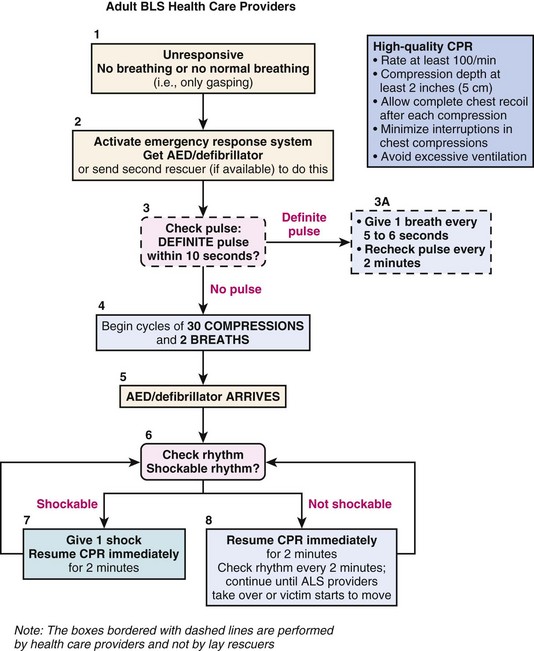
The 2005 American Heart Association (AHA) guidelines for basic life support (BLS) and cardiopulmonary resuscitation (CPR) recommended the sequence of airway, breathing, and circulation (A-B-C).18 The first steps in the 2005 BLS were opening the airway, checking for breathing, and providing two rescue breaths if adequate breathing is not detected. The third step was to initiate chest compressions (Fig. 34-6). To check for breathing, lay rescuers and health care providers were advised to “look, listen, and feel.” Health care providers were then advised to check for a pulse after delivery of the initial rescue breaths to a nonresponsive, nonbreathing individual.
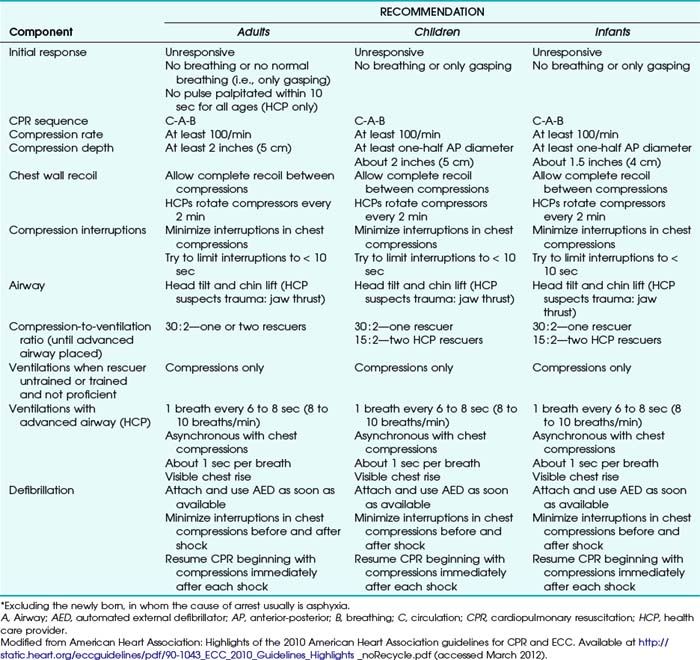
Updated BLS and CPR guidelines were released by the AHA in 2010.19–21 Table 34-1 summarizes these guidelines. The recommended sequence was changed to circulation, airway, and breathing (C-A-B). In conditions of low blood flow (e.g., cardiac arrest), oxygen delivery to the brain and heart is limited primarily by blood flow instead of arterial oxygen content.22 Using cardiac-only resuscitation and minimizing delays or interruptions in chest compressions can improve survival.23 Evidence does not show any difference in survival rates between chest compressions delivered alone and chest compressions combined with positive-pressure ventilation.23–25 The AHA currently recommends that chest compressions be initiated before rescue breaths or advanced airway placement. Rescue breaths are provided after the first cycle of chest compressions (Fig. 34-7). “Look, listen, and feel” has been removed from the 2010 algorithm.
Although the optimal oxygen concentration to be delivered during CPR has not been defined, current AHA guidelines recommend initial delivery of 100% oxygen during resuscitation. After return of spontaneous circulation, the 2010 guidelines recommend titration of oxygen administration to maintain an oxygen saturation level of 94% or greater to avoid hyperoxia when appropriate monitoring is available. Box 34-1 summarizes the changes pertaining to airway management during CPR that were introduced in the 2010 AHA guidelines.
Box 34-1 2010 Advanced Cardiac Life Support Guidelines
Changes in Airway Management
1. The basic life support sequence has changed from A-B-C to C-A-B for adults, children, and infants. Initiate chest compressions before ventilations.
2. Use of cricoid pressure during ventilations is not recommended.
3. Instruction to “look, listen, and feel for breathing” has been removed from the algorithm.
4. Excessive ventilation should be avoided.
5. Continuous quantitative capnography is recommended to confirm endotracheal tube placement.
6. Oxygen concentration is weaned after return of spontaneous circulation to maintain oxygen saturation at 94% or greater.
X Initial Airway Management during Cardiopulmonary Resuscitation
XI Advanced Airway Management during Cardiopulmonary Resuscitation
Endotracheal intubation during CPR should be performed by trained health care providers, and interruptions of chest compressions should be minimized. Endotracheal intubation through direct laryngoscopy may be more difficult if performed during chest compressions. Prolonged attempts at tracheal intubation should be avoided, especially if chest compressions are halted during attempts. Placement of an endotracheal tube or other advanced airway device has not been associated with any improvement in return of spontaneous circulation. Endotracheal intubation attempts by inexperienced providers may result in complications such as failed intubation or esophageal intubation.26
After endotracheal tube placement, ventilations are delivered without interruption of chest compressions at a rate of one breath every 6 to 8 seconds. Certain resuscitation medications (Box 34-2) can be delivered through the endotracheal tube. Secretions can be removed from the airway through the endotracheal tube, and the endotracheal tube cuff may provide a barrier against aspiration.
Box 34-2 Resuscitation Medications That Can Be Delivered Through an Endotracheal Tube
Administer two to three times the intravenous dosage, followed by 10 mL of normal saline:
A Confirmation of Endotracheal Tube Placement During Cardiopulmonary Resuscitation
The 2005 CPR guidelines recommended the use of exhaled carbon dioxide (CO2) detectors or esophageal detectors for confirmation of endotracheal tube placement in addition to clinical assessment by auscultation and direct visualization. Exhaled CO2 detectors may produce a false-negative result due to decreased blood flow and CO2 delivery to the lungs, pulmonary embolus, pulmonary edema, or severe airway obstruction.27 False-positive readings have been detected when the stomach contains large amounts of carbonated liquids.28
Thoracic impedance measurement may aid in detection of esophageal intubation, but evidence is insufficient to recommend its use for confirmation of endotracheal tube placement. Thoracic impedance is significantly higher during inspiration than during expiration, and changes in impedance, which can be measured by defibrillation pads, occur only if the endotracheal tube is correctly placed.29
B Use of Cricoid Pressure During Cardiopulmonary Resuscitation
The 2005 CPR guidelines recommended the use of cricoid pressure by a third rescuer if the victim is deeply unconscious. Evidence suggests that applying cricoid pressure may impede ventilation and interfere with the placement of advanced airway devices or intubation.30,31 The 2010 guidelines recommend against the routine use of cricoid pressure as part of airway management during CPR.
C Supraglottic Airway Devices
The 2005 and 2010 AHA CPR guidelines support the use of a supraglottic airway device as an alternative to endotracheal intubation. Box 34-3 lists the supraglottic devices that have been studied for use in cardiac arrest and acknowledged by the AHA. Because intubation through a supraglottic airway does not require glottic visualization, placement may be faster than endotracheal intubation, and it may result in shorter no-flow times (i.e., period when chest compressions are halted for other interventions).32,33 Supraglottic airway placement should be considered as an option if endotracheal intubation fails. Ventilations are delivered through a supraglottic airway device in the same ratio as through an endotracheal tube (i.e., one breath every 6 to 8 seconds without interruption of chest compressions).
If available, newer supraglottic airway devices that provide a conduit for intubation can be considered. Preliminary evidence supports their use in the prehospital environment, especially if difficulty with intubation is encountered.34,35
D Role of Advanced Airway Devices
Advanced airway management techniques such as fiberoptic intubation and video laryngoscopy have not been widely studied as intubation techniques for airway management during CPR. Preliminary evidence suggests that video laryngoscopy may be an acceptable alternative to conventional laryngoscopy, especially for difficult intubations.36,37 Advanced airway devices may not be easily accessible in the prehospital environment. Inadequate light conditions and the lack of electricity may limit the usefulness of video laryngoscopy outside the hospital setting.
XII Alternative Methods of Oxygen Delivery during Cardiopulmonary Resuscitation
A Oxylator
The Oxylator (CPR Medical Devices, Ontario, Canada) is a fixed-flow automatic resuscitation management system with an adjustable pressure limit. Several models exist, including the Oxylator EMX, which is recommended for prehospital use (Fig. 34-8). The Oxylator delivers oxygen flow at 30 L/min until an adjustable maximum pressure (up to 45 cm H2O) is reached, at which point passive exhalation occurs to an airway pressure of 2 to 4 cm H2O. The device allows manual (rescuer initiated) and automatic inhalation modes. The Oxylator works with medical oxygen or hospital air supply, tank, or compressor; it does not require electricity; and it can be connected to a face mask, supraglottic airway, or endotracheal tube.

Figure 34-8 The Oxylator EMX is a positive-pressure resuscitation and inhalation system.
(Courtesy of Lifesaving Systems, Inc., Roswell, GA.)
Potential advantages of the Oxylator over bag-mask ventilation include consistent ventilation and oxygenation to a set pressure; possible avoidance of hyperventilation, excessive ventilation, or gastric insufflation; and early detection of airway obstruction.38 Use of the Oxylator in the automatic mode can free the CPR provider to focus on other resuscitation tasks. The Oxylator may be useful in austere environments in which access to the patient’s head and airway may be limited.
B ResQPOD
The ResQPOD (Advanced Circulatory Systems, Roseville, MN), designated an AHA class 2A recommendation for patients in cardiac arrest, is an impedance threshold device. By regulating thoracic pressure during ventilation, the device increases blood flow to the heart and brain, increases systolic blood pressure, and increases the success rate of defibrillation. By preventing excess air from entering the thorax during ventilation, the device increases thoracic negative pressure and increases blood flow to the heart. It is placed proximal to a face mask, supraglottic airway, or endotracheal tube and connects to the source of ventilation (Fig. 34-9). The ResQPOD also contains timing-assist lights to guide proper ventilation rates and prevent hyperventilation. Use of this device during CPR has improved survival rates.39
C Passive Oxygen Insufflation
Oxygen can be delivered passively through an oropharyngeal airway, face mask, supraglottic airway, or modified endotracheal tube (Boussignac endotracheal tube, Vygon Corporation, Montgomeryville, PA). The Boussignac tube contains capillaries through which oxygen is delivered by continuous insufflation, generating a constant positive alveolar pressure. The proximal end of the tube remains open to allow exhalation (Fig. 34-10). The changes in intrathoracic pressure that occur during chest compressions trigger passive inhalation and active exhalation, allowing adequate gas exchange.
Passive oxygen delivery does not require the use of a rescuer to deliver ventilations, minimizes interruptions in chest compressions, and may reduce the risk of barotrauma caused by excessive ventilation. Evidence shows passive oxygen delivery to be as effective as bag-mask ventilation or mechanical ventilation through an endotracheal tube.40,41 Passive oxygen delivery is described as an alternative but not a replacement for ventilation during CPR in the 2010 AHA guidelines.
XIII Challenges of Airway Management during Cardiopulmonary Resuscitation
B Cervical Spine Injury
Cervical spine injury has been diagnosed in 2% to 5% of patients after traumatic injury.42 If the anterior and posterior columns of the cervical spine are injured, the injury is considered unstable.43 Most trauma patients are placed in a cervical collar until cervical injury is ruled out; some of these patients may require CPR and emergent airway management before a radiologic examination can be obtained. Significant head injury is associated with traumatic cervical spine injury; patients with a Glasgow Coma Scale score of 8 or less often require emergent airway management.44
No one method of intubation has been proved to be safest, and rapid-sequence intubation by direct laryngoscopy is the most commonly reported technique. Evidence shows that some degree of cervical spine motion occurs with all methods of intubation,45,46 but data are lacking about whether the small amount of movement that occurs during airway management is clinically significant. A higher incidence of cervical spine limitation and difficult intubation may exist among elderly patients.47 Box 34-4 describes recommendations for airway management in the patient with a suspected or known cervical spine injury.
Box 34-4
Airway Management Recommendations for Patients with Suspected Cervical Spine Injury
Rapid-sequence intubation is most often recommended.
Manual in-line stabilization of the cervical spine minimizes movement during intubation.
No safe amount of cervical spine movement has been defined.
A selection of laryngoscope blades and sizes should be available.
Modified from Ollerton JE, Parr MJA, Harrison K, et al: Potential cervical spine injury and difficult airway management for emergency intubation of trauma adults in the emergency department—a systematic review. Emerg Med J 23:3–11, 2006.
XIV Controversies
A Role of Hyperventilation
Evidence suggests that hyperventilation may decrease overall survival and should be avoided.48 Excessive ventilation should also be avoided because of the risk of gastric insufflation, regurgitation, or aspiration. Hyperventilation increases intrathoracic pressure and results in reduced coronary perfusion pressures.49
XVI Clinical Pearls
• Disaster management should start with a bottom-to-top approach, followed by a multiple-scale approach.
• Communication, preservation of infrastructure, and mitigation techniques are essential during a disaster response.
• The 2010 AHA CPR guidelines recommend beginning chest compressions before initial airway management (i.e., circulation, airway, and breathing).
• Hyperventilation during CPR should be avoided, and it may reduce overall survival.
• Limited access to the patient may make airway management and resuscitation during disasters more challenging.
All references can be found online at expertconsult.com.
19 Berg RA, Hemphill R, Abella BS, et al. Part 5: Adult basic life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(Suppl 3):S685–S705.
20 Neumar RW, Otto CW, Link MS, et al. Part 8: Adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(Suppl 3):S729–S767.
23 SOS-KANTO study group. Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): An observational study. Lancet. 2007;369:920–926.
43 Crosby ET. Airway management in adults after cervical spine trauma. Anesthesiology. 2006;104:1293–1318.
1 Sundnes KO, Birnbaum ML. Health disaster management: Guidelines for evaluation and research in the Utstein style. Prehosp Disaster Med. 2003;17(Suppl 3):33.
2 Jenkins JL, McCarthy ML, Sauer LM, et al. Mass-casualty triage: Time for an evidence-based approach. Prehosp Disaster Med. 2008;23:3–8.
3 Kaji AH, Koenig KL, Lewis RJ. Current hospital disaster preparedness. JAMA. 2007;298:2188–2190.
4 Agency for Healthcare Research and Quality (AHRQ). Hospital surge model. Available at http://archive.ahrq.gov/prep/hospsurgemodel/ (accessed March 2012)
5 Agency for Healthcare Research and Quality (AHRQ). Altered standards of care in mass casualty events, bioterrorism and other public health emergencies. Available at http://archive.ahrq.gov/research/altstand/ (accessed March 2012)
6 McIsaac J, Antoine J, Barach P, et al. Emergency preparedness. In Manual for anesthesia department organization and management. Available at: http://www.asahq.org/For-Members/Clinical-Information/~/media/For%20Members/COTEP/MADOM-Edited-by-McIsaac-6.ashx. (accessed March 2012)
7 Baker BC, Buckenmaier C, Narine N, et al. Battlefield anesthesia: Advances in patient care and pain management. Anesthesiol Clin. 2007;25:131–145.
8 Buckenmaier CC, 3rd., Brandon-Edwards H, Borden D, Jr., Wright J. Treating pain on the battlefield: A warrior’s perspective. Curr Pain Headache Rep. 2010;14:1–7.
9 Gegel BT. A field-expedient Omeda Universal Portable Anesthesia Complete draw-over vaporizer setup. AANA J. 2008;76:185–187.
10 Federal Emergency Management Agency (FEMA). National Incident Management System. Available at http://www.fema.gov/emergency/nims (accessed March 2012)
11 Federal Emergency Management Agency (FEMA). National Response Framework. Available at http://www.fema.gov/emergency/nrf (accessed March 2012)
12 U.S. Department of Health and Human Services, Public Health Emergency. National Disaster Medical System. Available at http://www.phe.gov/Preparedness/support/medicalassistance/Pages/default.aspx#ndms (accessed March 2012)
13 Barnett DJ, Levine R, Thompson CB, et al. Gauging U.S. emergency medical services workers’ willingness to respond to pandemic influenza using a threat- and efficacy-based assessment framework. PLoS One. 2010;5:e9856.
14 Occupational Safety and Health Administration (OSHA). Best practices for hospital-based first receivers of victims from mass casualty incidents involving the release of hazardous substances. Available at http://www.osha.gov/dts/osta/bestpractices/html/hospital_firstreceivers.html (March 2012)
15 Suyama J, Knutsen CC, Northington WE, et al. IO versus IV access while wearing personal protective equipment in a hazmat scenario. Prehosp Emerg Care. 2007;11:467–472.
16 Greenland KB, Tsui D, Goodyear P, Irwin MG. Personal protection equipment for biological hazards: Does it affect tracheal intubation performance? Resuscitation. 2007;74:119–126.
17 Castle N, Owen R, Hann M, et al. Impact of chemical, biological, radiation, and nuclear personal protective equipment on the performance of low- and high-dexterity airway and vascular access skills. Resuscitation. 2009;80:1290–1295.
18 Emergency Cardiovascular Care (ECC) Committee, Subcommittees, and Task Forces of the American Heart Association. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112(Suppl):IV1–IV203.
19 Berg RA, Hemphill R, Abella BS, et al. Part 5: Adult basic life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(Suppl 3):S685–S705.
20 Neumar RW, Otto CW, Link MS, et al. Part 8: Adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(Suppl 3):S729–S767.
21 Morrison LJ, Deakin CD, Morley PT, et al. Part 8: Advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with treatment recommendations. Circulation. 2010;122(Suppl 2):S345–S421.
22 Chandra NC, Gruben KG, Tsitlik JE, et al. Observations of ventilation during resuscitation in a canine model. Circulation. 1994;90:3070–3075.
23 SOS-KANTO study group. Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): An observational study. Lancet. 2007;369:920–926.
24 Tang W, Weil MH, Sun S, et al. Cardiopulmonary resuscitation by precordial compression but without mechanical ventilation. Am J Respir Crit Care Med. 1994;150:1709–1713.
25 Noc M, Weil MH, Tang W, et al. Mechanical ventilation may not be essential for initial cardiopulmonary resuscitation. Chest. 1995;108:821–827.
26 Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37:32–37.
27 Ornato JP, Shipley JB, Racht EM, et al. Multicenter study of a portable, hand-size, colorimetric end-tidal carbon dioxide detection device. Ann Emerg Med. 1992;21:518–523.
28 Sum Ping ST, Mehta MP, Symreng T. Accuracy of the FEF CO2 detector in the assessment of endotracheal tube placement. Anesth Analg. 1992;74:415–419.
29 Pytte P, Olasveengen TM, Steen PA, et al. Misplaced and dislodged endotracheal tubes may be detected by the defibrillator during cardiopulmonary resuscitation. Acta Anaesthesiol Scand. 2007;51:770–772.
30 Asai T, Goy RW, Liu EH. Cricoid pressure prevents placement of the laryngeal tube and laryngeal tube suction II. Br J Anaesth. 2007;99:282–285.
31 Hocking G, Roberts FL, Thew ME. Airway obstruction with cricoid pressure and lateral tilt. Anaesthesia. 2001;56:825–828.
32 Abo BN, Hostler D, Wang HE. Does the type of out-of-hospital airway interfere with other cardiopulmonary resuscitation tasks? Resuscitation. 2007;72:234–239.
33 Wiese CH, Bartels U, Bergmann A, et al. Using a laryngeal tube during cardiac arrest reduces “no flow time” in a manikin study: A comparison between laryngeal tube and endotracheal tube. Wien Klin Wochenschr. 2008;120:217–223.
34 Tentiller E, Heydenreich C, Cros AM, et al. Use of the intubating laryngeal mask airway in emergency pre-hospital difficult intubation. Resuscitation. 2008;77:30–34.
35 Timmerman A, Russo SG, Rosenblatt WH, et al. Intubating laryngeal mask airway for difficult out-of-hospital airway management: A prospective evaluation. Br J Anaesth. 2007;99:286–291.
36 Kim YM, Kang HG, Kim JH, et al. Direct versus video laryngoscopic intubation by novice prehospital intubators with and without chest compressions: A pilot manikin study. Prehosp Emerg Care. 2011;15:98–103.
37 Wong E, Ng YY. The difficult airway in the emergency department. Int J Emerg Med. 2008;1:107–111.
38 Noordergraaf GJ, van Dunn PJ, Kramer BP, et al. Airway management by first responders when using a bag-valve device and two oxygen-driven resuscitators in 104 patients. Eur J Anaesthesiol. 2004;21:361–366.
39 Aufderheide TP, Pirrallo RG, Provo TA, Lurie KG. Clinical evaluation of an inspiratory threshold device during standard cardiopulmonary resuscitation in patients with out-of-hospital cardiac arrest. Crit Care Med. 2005;33:734–740.
40 Bertrand C, Hemery F, Carli P, et al. Constant flow insufflation of oxygen as the sole mode of ventilation during out-of-hospital cardiac arrest. Intensive Care Med. 2006;32:843–851.
41 Bobrow BJ, Ewy GA, Clark L, et al. Passive oxygen insufflation is superior to bag-mask-ventilation for witnessed ventricular fibrillation out-of-hospital cardiac arrest. Ann Emerg Med. 2009;54:656–662.
42 Ollerton JE, Parr MJA, Harrison K, et al. Potential cervical spine injury and difficult airway management for emergency intubation of trauma adults in the emergency department: A systemic review. Emerg Med J. 2006;23:3–11.
43 Crosby ET. Airway management in adults after cervical spine trauma. Anesthesiology. 2006;104:1293–1318.
44 Pimentel L, Diegelmann L. Evaluation and management of acute cervical spine trauma. Emerg Med Clin North Am. 2010;28:719–738.
45 LeGrand SA, Hindman BJ, Dexter F, et al. Craniocervical motion during direct laryngoscopy and orotracheal intubation with the Macintosh and Miller blades: An in vivo cinefluoroscopic study. Anesthesiology. 2007;107:884–891.
46 Lennarson PJ, Smith D, Todd MM, et al. Segmental cervical spine motion during orotracheal intubation of the intact and injured spine with and without external stabilization. J Neurosurg. 2000;92(Suppl):201–206.
47 Mashour GA, Stallmer ML, Kheterpal S, et al. Predictors of difficult intubation in patients with cervical spine limitations. J Neurosurg Anesthesiol. 2008;20:110–115.
48 Aufderheide TP, Lurie KG. Death by hyperventilation: A common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med. 2004;82(Suppl):S345–S351.
49 Aufderheide TP, Sigurdsson G, Pirrallo RG, et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109:1960–1965.