CHAPTER 56 Difficult breast augmentations
Tuberous breast deformity
Anatomy
Physical evaluation
Technical steps
The procedure to correct the tuberous breast includes the following options:
• Periareolar mastopexy in most cases.
• Soft tissue parenchymal manipulation to reshape the existing breast tissue.
• Breast augmentation, frequently asymmetric.
• Manipulation and lowering of the inframammary fold.
• Scoring the lower breast skin flap in the lower pole of the breast.
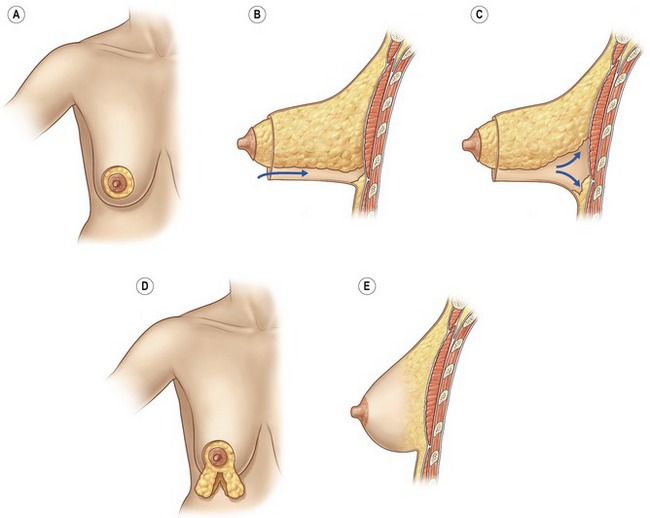
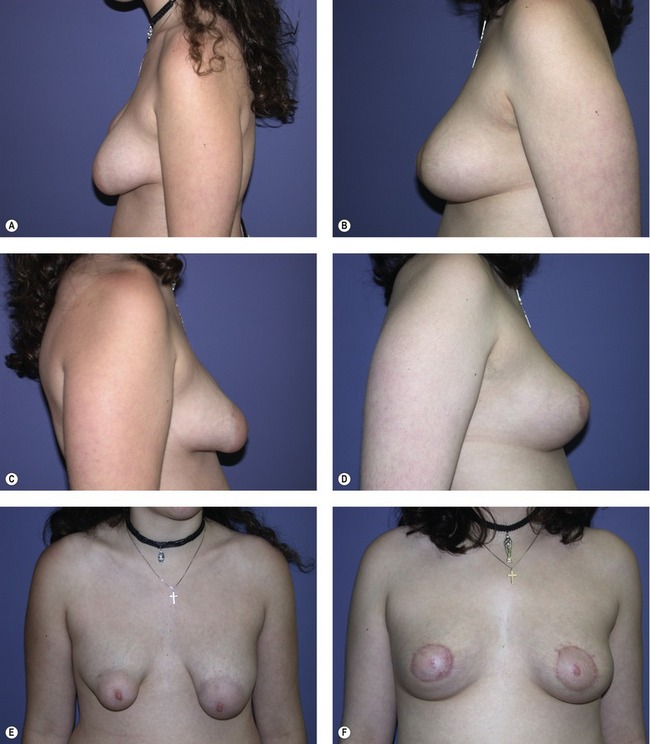
Periareolar mastopexy is almost always a part of any procedure to treat tuberous breasts. After the periareolar skin resection, a lower breast skin flap is elevated. The breast is completely mobilized to the chest wall and then the dissection is continued superiorly until the entire lower breast is mobilized and delivered through the incision. The breast is usually split at the 6 o’clock position and medial and lateral flaps are created. The fibrous ring is divided. Additional cuts are made in the ring if needed. The flaps are sutured together to make a round more normal lower pole of the breast (Fig. 56.1). If the skin of the lower pole of the breast is felt to be deficient, a tissue expander may be inserted. If need for a tissue expander is though to be a possibility, it should be discussed with the patient prior to surgery. In most cases, a tissue expander is not required and the breast is augmented. Usually a subpectoral or dual-plane pocket is created, a sizer is placed, and the appropriate implant is selected. The areola is closed with a permanent purse-string suture (Fig. 56.2).
Anterior thoracic hypoplasia
Anatomy and physical evaluation
It is important to make sure that any chest wall asymmetries are noted when evaluating a patient for breast augmentation. It is a good idea to take a series of basic chest measurements when examining a breast augmentation patient. These include:
Poland’s syndrome
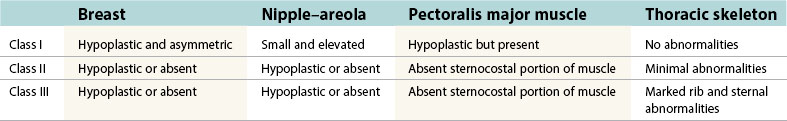
Poland’s syndrome was classified by Hartrampf (Table 56.1). Class 2 and 3 patients are reconstructed with breast reconstruction techniques which are beyond the scope of this chapter. Class 1 patients are reconstructed with techniques that are similar to those used with anterior thoracic hypoplasia. In class 1 patients the pectoralis muscle is hypoplastic and frequently does not need to be separately reconstructed. Since many patients with Poland’s syndrome present in their teenage years, prior to complete breast growth, the first stage of the reconstruction often involves placement of a tissue expander or an adjustable implant. When growth is complete, the implant or tissue expander is replaced with a permanent implant and the unaffected side is modified to match the affected side as best as possible (Fig. 56.3).
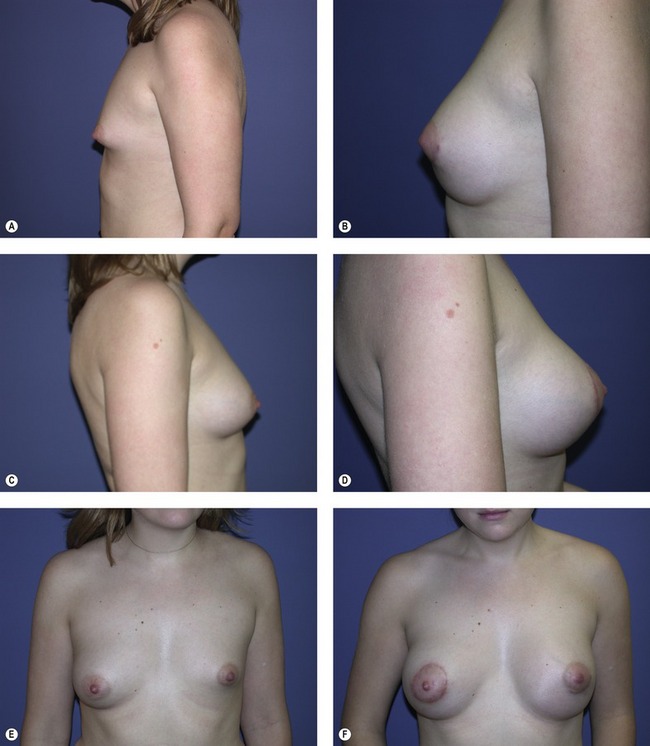
Fig. 56.3 A–F, 20-year-old patient with left Poland’s syndrome treated with left breast augmentation alone.
Pearls & pitfalls
Pearls
• More extreme deformities have to be dealt with in specific ways to attain a good result from breast augmentation.
• The tuberous breast may show lower medial breast deficiency; deficiency in the entire lower pole of the breast; deficiency in the entire breast.
• Chest wall deformities may involve the ribs, sternum and muscles as well as the breast and other soft tissues.
• It is important to make sure that any chest wall asymmetries are noted when evaluating a patient for breast augmentation.
• Poland’s syndrome always has involvement of the pectoralis major muscle.
Pitfalls
• The most common complication associated with tuberous breast surgery is either not recognizing the deformity or underestimating the deformity and only placing a breast implant.
• In many cases, there is no way to correct the high-riding nipple–areola complex. This needs to be explained to the patient preoperatively.
• Patients with tuberous breasts, Poland’s syndrome and anterior thoracic hypoplasia need to be cautioned that as they go through the different stages of life (pregnancy, breast feeding, aging), the affected and unaffected breasts will change in different ways. This frequently results in the need for revisional surgery. The patient should be carefully advised of this prior to any surgical procedure.
Summary of steps
Tuberous breast deformity
Grolleau JL, Lanfrey E, Lavigne B. Breast base anomalies: Treatment strategy for tuberous breasts, minor deformities, and asymmetry. Plast Reconstr Surg. 1999;104:2040–2048.
Hodgkinson DJ. The management of Anterior chest wall deformity in patients presenting for breast augmentation. Plast Reconstr Surg. 2002;109:1714–1723.
Mandrekas AD, Zambacos GJ, Anastasopoulos A, et al. Aesthetic reconstruction of the tuberous breast deformity. Plast Reconstr Surg. 2003;112:1099–1108.
Rees TD, Aston SJ. The tuberous breast. Clin Plast Surg. 1976;3:339–347.
Rohrich RJ, Hartley W, Brown S. Incidence of breast and chest wall asymmetry in breast augmentation: A retrospective analysis of 100 patients. Plast Reconstr Surg. 2003;111:1513–1519.
Sadove AM, van Aalst JA. Congenital and acquired pediatric breast anomalies: A review of 20 years experience. Plast Reconstr Surg. 2005;115:1039–1050.
Spear SL, Pelletiere CV, Lee E. Anterior thoracic hypoplasia: A separate entity from Poland’s syndrome. Plast Reconstr Surg. 2004;13:69–77.