Chapter 6 Diagnosis of Anterior Cruciate Ligament Tear
Partial Tears
This chapter deals primarily with complete ACL tears. Traditionally, partial tears have been found to produce a smaller degree of anteroposterior (AP) laxity than complete tears on Lachman or instrumented Lachman testing, as described later. Until the present time, the only alternatives have been nonoperative treatment or complete reconstruction, which would necessitate ablation of the remaining ligament. Given these alternatives, nonsurgical treatment has been the usual alternative if less than 50% of the ligament was torn.1 With more awareness of ACL double-bundle anatomy, single-bundle repairs that preserve the remaining ligament have been developed.2 These repairs have been used in some cases of single-bundle partial ACL tear. Lachman testing and arthrometer testing in these cases appear to show 2- to 3-mm asymmetry in anteromedial (AM) bundle tears and 1- to 2-mm asymmetry in posterolateral (PL) bundle tears.3 Arthroscopy is required for definite anatomical diagnosis. The pivot shift is of much greater value in the anesthetized versus the awake patient. Diagnostic criteria as well as surgical indications and techniques in these cases continue to evolve.
History
Acute
The history and mechanism of ACL tear are familiar to all orthopaedists.4–10 The history most commonly entails twisting, landing, or a valgus blow to the knee. However, almost any history of knee trauma can be associated with ACL tear. These atypical histories may represent unusual mechanisms or inaccurate remembrances by the patient. The important point is never to eliminate ACL tear from the differential diagnosis based on the history. Classically, swelling is marked within a few hours. However, some ACL tears never produce more than minimal swelling, even acutely. Patients often hear or feel a “pop,” but many do not. Similarly, patients may have felt the knee “go out of place,” or felt their “leg go one way and the body another” but often they have not felt these sensations. Pain may be severe and persisting or may be mild and transient.
Physical Exam
Pivot Shift
The pivot shift is a specific but very insensitive test for ACL tear in the nonanesthetized patient.11,12 It is also subject to great interobserver error. Because the pivot shift is often quite painful when positive, has low sensitivity, and usually adds nothing beyond the Lachman test, I (C. Prodromos) use it only rarely for the diagnosis of ACL tear in the office. I do use it routinely in the 1- and 2-year follow-up exams, where its negativity confirms that ACL reconstruction has been successful.
Lachman Test
The Lachman test,13 the anterior drawer test in approximately 20 degrees of flexion, is the most reliable exam test for ACL tear11 but is far more reliable in the chronic case, when secondary restraints have stretched and there is less hamstring spasm, than in the acute case. After 21 years of sports medicine practice, I still find the Lachman inconclusive with some frequency in the acute setting, particular in regards to the differential between partial and complete tear, because of persisting hamstring spasm. The firmness of the endpoint may be particularly hard to evaluate. The examiner may or may not be successful in relaxing the hamstrings. Palpating them posteriorly and simultaneously while asking the patient to relax them is often effective. It is important that the patient is in the supine, not sitting, position, and he or she should be instructed to relax the entire body to help relax the knee. The Lachman test should be considered definitive only if it is clearly negative with a firm endpoint. It is important that the examiner be able to differentiate between a negative Lachman test and a false negative caused by this hamstring spasm to avoid missing a torn ACL.
Anterior Cruciate Ligament Versus Posterior Cruciate Ligament Tear
A posterior cruciate ligament (PCL) tear produces increased AP laxity and can mimic an ACL tear. Classically there will be increased AP laxity, but with a firm anterior endpoint, with a PCL tear. However, this can also be seen with a healed partial ACL tear. If there is a question of ACL versus PCL tear, then MRI or the quadriceps active test14 should be used to differentiate the two. In addition, it is wise to always arthroscopically inspect the knee before any graft harvesting takes place to make certain that the ACL is in fact completely torn.
Locking
“Pseudolocking” may be seen classically with partial tears.15,16 However, a knee with a 20-degree or so persisting flexion contracture (i.e., pseudolocking) can occasionally be seen with isolated complete ACL tear from hamstring spasm alone. True locking is seen with ACL tear in combination with displaced bucket-handle meniscal tears. In these cases the “locking” is actually reflex hamstring spasm in response to extension in the presence of the displaced meniscal tear. Thus, the Lachman test is always difficult to perform and frequently false negative because of the hamstring spasm.17
Hemarthrosis
The presence of a large hemarthrosis is much more highly associated with ACL tear in adults18–21 than in children.22 Patellar dislocation and fracture are other leading causes of hemarthrosis. The former can usually be accurately diagnosed by physical exam, the latter by radiography. Arthrocentesis is usually not indicated. Its only diagnostic value is in determining whether a large effusion is a hemarthrosis. In most of these cases, an MRI will be ordered, which will provide much more information and spare the patient the pain of the arthrocentesis. If the effusion is sufficiently tense, hemarthrosis may be indicated for pain relief. If MRI is unavailable and the exam is equivocal, then arthrocentesis may be useful. A 16-gauge needle is preferable, but an 18-gauge needle may be used.
Patellofemoral Injury
Although concomitant ACL tear and patellar dislocation or injury is unusual, it does occur.23 The presence of physical exam signs of acute patellar instability should not cause the examiner to fail to test for ACL instability.
KT-1000 or Other Instrumented Lachman Test
The KT-100024–29 (Figs. 6-1 and 6-2) maximum manual examination is a highly accurate method for definitive diagnosis of ACL tear that is heavily relied on in our clinic. When it indicates a complete ACL tear, we generally do not order an MRI scan. A side-to-side difference of more than 4 mm, particularly with an absolute value of 10 or more, is nearly 100% specific for complete ACL tear30 if the examiner is experienced in its use. The more difficult differential may be between complete and partial ACL tear. We have found partial ACL tears to usually have a laxity of 2 or 3 mm. When it is greater, a complete tear has almost always existed. Others have found a slightly larger range.31 Larger differences, up to 4 and perhaps 5 mm, can be seen after ACL reconstruction without graft discontinuity. It is important to point out that the maximum manual test is more reliable than other methods. A 20-lb pull in particular will understate the amount of laxity. The 30-lb pull will as well, but to a lesser extent.32 Other arthrometers are in use, particularly in Europe, with reportedly good results.33 We have no experience with them.
As described earlier, PCL tears can mimic ACL tears. The “quadriceps active test”14 performed with the KT-1000 has been shown to reliably differentiate the two.
Examination Under Anesthesia
The examination under anesthesia (EUA) dramatically increases the sensitivity of the pivot shift test.12 The accuracy of the KT-1000 is also improved. We may perform both just prior to arthroscopy when the diagnosis is in doubt. The differential in question is usually between a partial and complete ACL tear. EUA may appear to be unnecessary because arthroscopic examination can seemingly determine whether a complete tear exists. However, with partial tears the EUA is a valuable supplement to the arthroscopic findings in determining whether reconstruction is needed. The difference between a partially torn but substantially intact ACL that would do well with conservative treatment versus a completely torn ACL that has scarred in with fibrofatty tissue and is essentially functionless is not always obvious arthroscopically. In these circumstances the EUA is very helpful in helping to determine proper treatment.
Radiographs
Radiographs are typically negative; however, certain radiographic signs may be present. These include the lateral tibial rim or “segond” fracture and posterior lateral tibial plateau fracture or lateral femoral condyle impaction fracture.34 Tibial spine peaking is common in chronic tears but is a nonspecific sign. Tibial eminence fracture is seen occasionally in the skeletally immature and rarely in the skeletally mature (Figs. 6-3 and 6-4). Radiographic signs of a hemarthrosis are usually present.
Magnetic Resonance Imaging
Sensitivity rates of 80% to 81% for arthroscopically proven complete ACL tears have been reported using MRI.30,35 Others have reported accuracy rates of more than 90%36,37 and sensitivity and specificity over 95%.38 However, Tsai et al found only a 67% specificity rate for complete tear.39 The MRI was very sensitive for detecting some ACL injury, but it was much less specific for differentiating the complete from the partial tear. This is an important distinction because the former is usually a surgical lesion, whereas the latter is usually not.
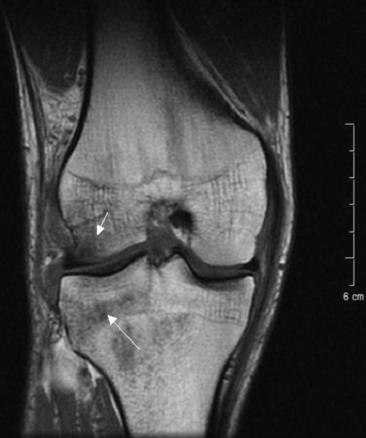
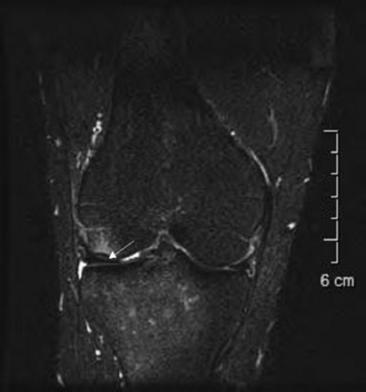
The normal ACL is both distinctly seen and appears taut (Fig. 6-5). The torn ACL is indistinct and appears lax (Fig. 6-6). Bone bruises (Fig. 6-7) in the lateral compartment are seen in roughly half of acute ACL tears.40,41 Their absence should thus not be relied on to rule out ACL tear. A fracture of the posterior lip of the tibia is another characteristic finding (Fig. 6-8). Transchondral fracture with intact articular cartilage is sometimes also seen (Fig. 6-9).
High-field MRI machines generally produce better accuracy for ACL tears than low-field MRI machines and should be obtained where possible. If the only available high-field MRI machine is closed-field and the patient is claustrophobic, oral diazepam may be given. This will enable many such claustrophobic patients to undergo a closed test, especially if they understand that the improved quality of the images is worth their trouble. Finally, the skill of the radiologist is extremely important. The same study can be interpreted as positive or negative depending on the radiologist’s experience. A skilled radiologist can be of great help to the orthopaedist in interpreting difficult cases. False-positive MRIs are less common but also occur. One study found MRI to add no diagnostic accuracy beyond history, physical exam, and radiographs (but not KT-1000) for all ACL tears.42 We believe this is greater clinical diagnostic accuracy than most orthopaedists, including the author, would achieve.
Conclusions
1 Noyes FR, Mooar LA, Moorman CTIII, et al. Partial tears of the anterior cruciate ligament: progression to complete ligament deficiency. J Bone Joint Surg Br. 1989;71:825-833.
2 Prodromos CC, Fu F, Howell S, et al. Controversies in soft tissue anterior cruciate ligament reconstruction. Presented at the symposium of the 2006 of the American Academy of Orthopaedic Surgeons. Controversies in Soft Tissues ACL Reconstruction, Chicago. March, 2006.
3 Fu FH. Personal communication. August, 2006.
4 Berns GS, Hull ML, Patterson HA. Strain in the anteriormedial bundle of the anterior cruciate ligament under combined loading. J Orthop Res. 1992;10:167-176.
5 Boden BP, Dean GS, Geagin JA, et al. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573-578.
6 DeMorat G, Weinhold P, Blackburn T, et al. Aggressive quadriceps loading can induce non-contact anterior cruciate ligament injury. Am J Sports Med. 2004;32:477-483.
7 Fleming BC, Renstrom PA, Beynnon BD, et al. The effect of weightbearing and external loading on anterior cruciate ligament strain. J Biomech. 2001;34:163-170.
8 Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33:492-505.
9 Markolf KL, Burchfield DM, Sharpiro MM, et al. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13:930-935.
10 Mazzocca AD, Nissen CW, Geary M, et al. Valgus medial collateral ligament rupture causes concomitant loading and damage of the anterior cruciate ligament. J Knee Surg. 2003;16:148-151.
11 Benjaminse A, Gokeler A, van der Schans CP. Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther. 2006;36:267-288.
12 Donaldson WFIII, Warren RF, Wickiewicz T. A comparison of acute anterior cruciate ligament examinations. Initial versus examination under anesthesia. Am J Sports Med. 1985;13:5-10.
13 Ostrowski JA. Accuracy of 3 diagnostic tests for anterior cruciate ligament tears. J Athl Train. 2006;41:120-121.
14 Daniel DM, Stone ML, Barnett P, et al. Use of the quadriceps active test to diagnose posterior cruciate ligament disruption and measure posterior laxity of the knee. J Bone Joint Surg Am. 1988;70:386-391.
15 Chun CH, Lee BC, Yang JH. Extension block secondary to partial anterior cruciate ligament tear on the femoral attachment of the posterolateral bundle. Arthroscopy. 2002;18:227-231.
16 Finsterbush A, Frankl U, Mann G. Fat pad adhesion to partially torn anterior cruciate ligament: a cause of knee locking. Am J Sports Med. 1989;17:92-95.
17 Kong KC, Hamlet MR, Peckham T, et al. Displaced bucket handle tears of the medial meniscus masking anterior cruciate deficiency. Arch Orthop Trauma Surg. 1994;114:51-52.
18 Sarimo J, Rantanen J, Heikkila J, et al. Acute traumatic hemarthrosis of the knee. Is routine arthroscopic examination necessary? A study of 320 consecutive patients. Scand J Surgery. 2002;91:361-364.
19 Adalberth T, Roos H, Lauren M, et al. Magnetic resonance imaging, scintigraphy, and arthroscopic evaluation of traumatic hemarthrosis of the knee. Am J Sports Med. 1997;25:231-237.
20 Lundberg M, Odensten M, Thuomas KA, et al. The diagnostic validity of magnetic resonance imaging in acute knee injuries with hemarthrosis. A single-blinded evaluation in 69 patients using high-field MRI before arthroscopy. Int J Sports Med. 1996;17:218-222.
21 Maffulli N, Binfield PM, King JB, et al. Acute hemarthrosis of the knee in athletes. A prospective study of 106 cases. J Bone Joint Surg Br. 1993;75:945-949.
22 Matelic TM, Aronsson DD, Boyd DWJr, et al. Acute hemarthrosis of the knee in children. Am J Sports Med. 1995;23:668-671.
23 Chiang AS, Shin SS, Jazrawi LM, et al. Simultaneous ruptures of the anterior cruciate ligament and patellar tendon: a case report. Bull Hosp Joint Dis. 2005;62:134-136.
24 Rangger C, Daniel DM, Stone ML, et al. Diagnosis of an ACL disruption with KT-1000 arthrometer measurements. Knee Surg Sports Traumatol Arthrosc. 1993;1:60-66.
25 Boyer P, Dijan P, Christel P, et al. Reliability of the KT-1000 arthrometer (Medmetric) for measuring anterior knee laxity: comparison with Telos in 147 knees. Rev Chir Orthop Reparatrice Appar Mot. 2004;90:757-764.
26 Bonnaire F, Berwarth H, Munst P, et al. Can the results of cruciate ligament operations be arthrometrically evaluated? A comparison of subjective assessment, Lysholm score, clinical stability classification and measuring stability with the KT 1000 after complex knee injuries. Unfallchirurgie. 1995;21:83-91.
27 Anderson AF, Snyder RB, Federspiel CF, et al. Instrumented evaluation of knee laxity: a comparison of five arthrometers. Am J Sports Med. 1992;20:135-140.
28 Bach BRJr, Warren RF, Flynn WM, et al. Arthrometric evaluation of knees that have a torn anterior cruciate ligament. J Bone Joint Surg Am. 1990;72A:1299-1306.
29 Liu SH, Osti L, Henry M, et al. The diagnosis of acute complete tears of the anterior cruciate ligament. Comparison of MRI, arthrometry and clinical examination. J Bone Joint Surg Br. 1995;77B:586-588.
30 Prodromos CC, Han YS, Keller BL, et al. Stability of hamstring anterior cruciate ligament reconstruction at two- to eight-year follow-up. Arthroscopy. 2005;21:138-146.
31 Gonzalez-Couto E, Klages N, Strubin M. Synergistic and promoter-selective activation of transcription by recruitment of transcription factors TFIID and TFIIB. Proc Natl Acad Sci USA. 1997;94:8036-8041.
32 Strand T, Solheim E. Clinical tests versus KT-1000 instrumented laxity test in acute anterior cruciate ligament tears. Int J Sports Med. 1995;16:51-53.
33 Anderson AF, Snyder RB, Federspiel CF, et al. Instrumented evaluation of knee laxity: a comparison of five arthrometers. Am J Sports Med. 1992;20:135-140.
34 Stallenberg B, Gevenois PA, Sintzoff SAJr, et al. Fracture of the posterior aspect of the lateral tibial plateau: radiographic sign of anterior cruciate ligament tear. Radiology. 1993;187:821-825.
35 Varanda P, Amado P, Monteiro A, et al. Diagnosis of complete anterior cruciate ligament rupture: comparison of clinical examination, MRI and arthrometry. Presented at the 2006 meeting of the European Society of Sports Traumatology, Knee Surgery, and Arthroscopy, Innsbruck, Australia. May, 2006.
36 Vellet AD, Lee DH, Munk PL, et al. Anterior cruciate ligament tear: prospective evaluation of diagnostic accuracy of middle-and high-field strength MR imaging at 1.5 and 0.5 T. Radiology. 1995;197:826-830.
37 Vaz CE, Camargo OP, Santana PJ, et al. Accuracy of magnetic resonance in identifying traumatic intraarticular knee lesions. Clinics. 2005;60:445-450.
38 Craig JC, Go L, Blechinger J, et al. Three-tesla imaging of the knee: initial experience. Skeletal Radiol. 2005;34:453-461.
39 Tsai KJ, Chiang H, Jiang CC. Magnetic resonance imaging of anterior cruciate ligament rupture. BMC Musculoskelet Disord. 2004;8:21.
40 Dimond PM, Fadale PD, Hulstyn MJ, et al. A comparison of MRI findings in patients with acute and chronic ACL tears. Am J Knee Surg. 1998;11:153-159.
41 Tung GA, Davis LM, Wiggins ME, et al. Tears of the anterior cruciate ligament: primary and secondary signs at MR imaging. Radiology. 1993;188:661-667.
42 Kocabey Y, Tetik O, Isbell WM, et al. The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. Arthroscopy. 2004;21:696-700.