CHAPTER 47 Diagnosis and Treatment of Ulnar Collateral Ligament Injuries in Athletes
INTRODUCTION
Injury to the elbow medial ulnar collateral ligament (MUCL) from valgus forces was first recognized in a javelin thrower in 1946.32 The injury has since become well recognized in baseball pitchers and other overhead throwing athletes. Frank W. Jobe developed the original MUCL reconstruction and described the technique with initial results in 1986.17 The technique transected and reflected the flexor-pronator mass, transposed the ulnar nerve to a submuscular position, and created humeral tunnels that penetrated the posterior humeral cortex. Excellent exposure was achieved at the expense of morbidity to the flexor-pronator mass and handling the ulnar nerve. Since that initial report, modifications in the surgical technique have been made to ease technical demands and decrease soft tissue morbidity. A muscle-splitting approach has been developed to safely avoid detachment of the flexor-pronator mass with or without subcutaneous transposition of the ulnar nerve.29,30 Modifications in bone tunnel creation have also been made that direct the tunnels anterior on the humeral epicondyle to avoid risk of ulnar nerve injury while still allowing figure-of-eight graft passage and configuration.30 Further changes in bone tunnel configuration have reduced the total number of tunnels and facilitate easier graft tensioning.1,27 Results with these modified techniques have proven effective in returning high-level athletes back to throwing. In addition to advancements in surgical technique, advancements have been made in the pathophysiology and diagnosis of MUCL injuries. This chapter describes MUCL pathophysiology, patient evaluation, and surgical indications, and describes three popular surgical techniques.
PATHOPHYSIOLOGY
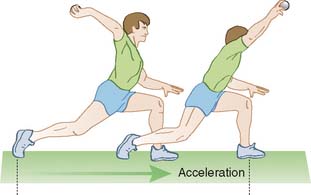
The anterior bundle of the MUCL is the strongest component and the primary restraint and stabilizer to valgus stress.5,16,22,25 The AOL is functionally composed of anterior and posterior bands that provide a reciprocal function in resisting valgus stress through the range of flexion-extension motion.20,25 Valgus stress is generated at the elbow during throwing maneuvers in baseball, softball, football, tennis serving, and volleyball spiking. The calculated valgus torque during the acceleration phase of throwing is 64 N-m,14,33 and more than 60 N-m with the tennis serve.11,13 These estimated forces exceed the known ultimate tensile strength of cadaveric MUCL specimens (33 N-m).38 Thus the MUCL is at risk for injury from these repetitive forces. A cadaver model has demonstrated that the flexor carpi ulnaris is the primary dynamic contributor to valgus stability and the flexor digitorum superficialis is a secondary stabilizer.24 Thus, the muscular dynamic stability to the medial elbow is essential and must be included in rehabilitation programs and morbidity from surgical techniques must be minimized.
DIAGNOSIS
HISTORY
Patients with MUCL injuries complain of medial elbow pain during the acceleration phase of throwing (Fig. 47-1). Chronic injuries present gradually and often with pain occurring only when throwing greater than 50% to 75% of maximal effort. Acute injuries may present suddenly with a pop, sharp pain, and inability to continue throwing. Patients may be affected with valgus extension overload syndrome associated with MUCL insufficiency. Occasionally, the presenting symptoms of VEO overshadow the symptoms of MUCL insufficiency, especially in the setting of chronic slowly progressive ligament attenuation. In these cases, the symptoms of sharp posteromedial elbow pain in both the acceleration (flexion) and more so in deceleration (extension) phases of throwing are also associated with limited extension and mechanical catching resulting from impinging osteophytes, chondromalacia, and loose bodies.
PHYSICAL
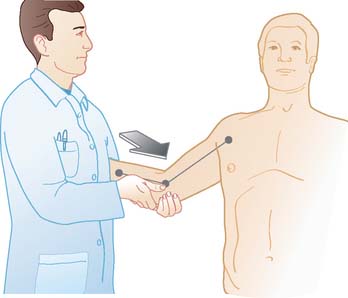
Physical examination features indicating MUCL injury include point tenderness directly over the MUCL or toward its insertion sites. Valgus instability is tested with the patients’ elbow flexed between 20 and 30 degrees to unlock the olecranon from its fossa as valgus stress is applied (Fig. 47-2). The milking maneuver is performed by either the patient or the examiner pulling on the patient’s thumb to create valgus stress with the patients’ forearm supinated and elbow flexed beyond 90 degrees. The moving valgus stress test is performed by applying valgus torque while the elbow is then flexed and extended and is considered positive if the medial elbow pain is reproduced at the MUCL and is maximum between 70 and 120 degrees (Fig. 47-3). The moving valgus stress test is highly sensitive and specific.
IMAGING
Anteroposterior, lateral, and axillary views of the elbow are assessed for joint space narrowing, osteophytes, and loose bodies. Valgus stress radiographs may be used to measure medial joint line opening, and an opening greater than 3 mm has been considered diagnostic of valgus instability.6,17,30 However, mild increased valgus elbow laxity has been observed in uninjured, asymptomatic dominant elbows of professional baseball pitchers when compared with their nondominant elbow.10 Computed tomography and magnetic resonance imaging (MRI) may further define loose bodies and osteophytes. Conventional MRI is capable of identifying thickening within the ligament from chronic injury or more obvious full-thickness tears. MR arthrography enhanced with intra-articular gadolinium improves the diagnosis of partial undersurface tears.7,15,21 Therefore the preferred imaging technique is MR enhanced with intra-articular gadolinium contrast, high-field closed magnet, and narrow slice images. Figure 47-4 demonstrates a full thickness tear of the MUCL from its attachment to the medial humeral epicondyle.

FIGURE 47-4 Magnetic resonance imaging scan with arrow indicating ulnar collateral ligament tear.
(From Ahmad, C. S.: Elbow injuries and the throwing athlete. In Galatz, L. M. [ed.]: Orthopaedic Knowledge Update: Shoulder and Elbow 3. Rosemont, IL, American Academy of Orthopaedic Surgeons, 2007, with permission.)
Dynamic ultrasonography has recently been studied as a means to evaluate the MUCL and is capable of detecting increased laxity with valgus stress.28 Advantages of ultrasound is that it is noninvasive, inexpensive, and dynamic. A disadvantage lies in dependence on operator experience.
TREATMENT
INDICATIONS AND CONTRAINDICATIONS
Treatment decisions require consideration of the patient’s athletic demands and the degree of MUCL injury. Nonoperative treatment includes a 6-week period of rest from throwing and flexor-pronator strengthening.24 If the patient becomes asymptomatic and the physical examination normalizes, then return to throwing with optimizing throwing mechanics is started. Rettig and colleagures26 demonstrated a 42% return to same level of play with an average return at 24.5 weeks with nonoperative treatment. No history or physical examination features are predictive for athletes who will respond to nonoperative treatment. Local steroid injections should be avoided because it may risk further injury to the MUCL.
SURICAL TECHNIQUES
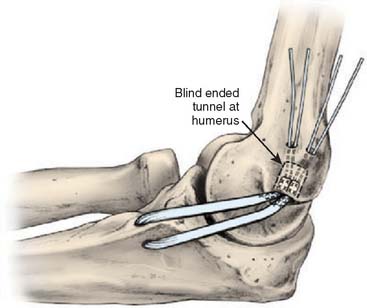
Several surgical techniques have evolved, and each has advantages and disadvantages. The modified Jobe technique has been considered the gold standard and has a reported success rate as high as 93% in returning throwing athletes back to competition (Fig. 47-5). This technique is technically demanding, however, in regard to number of tunnels, exact placement and connecting of tunnels, graft passing, and graft fixation. The docking technique has the advantages of reducing the complex ity of tunnel creation, passing and tensioning, and fixation. A potential disadvantage is that the graft is reduced from a triple strand used in the Jobe technique to a double-strand graft. However, a modification of the technique now allows doubling the graft on itself to form a quadruple limb graft. Finally, the hybrid interference screw technique has the advantage of further reducing the number and complexity of tunnel creation. With a single tunnel required on the ulna, there is less manipulating and risk of injury to the ulnar nerve. Furthermore, this technique allows independent tensioning of the anterior and posterior bands of the anterior bundle of the UCL, which is not accomplished with the other described techniques. A disadvantage is potential inflammatory reaction to the bioabsorbable screws.
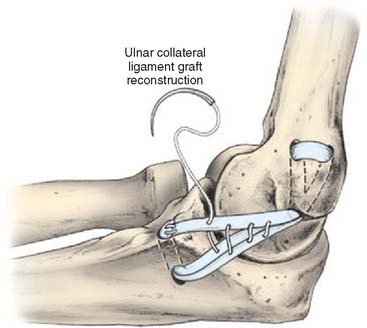
FIGURE 47-5 Classic Jobe UCL reconstruction.
(Redrawn from Safran, M., Ahmad, C. S., and ElAttrache, N. S.: Ulnar collateral ligament of the elbow. Arthroscopy 21:1381, 2005, with permission.)
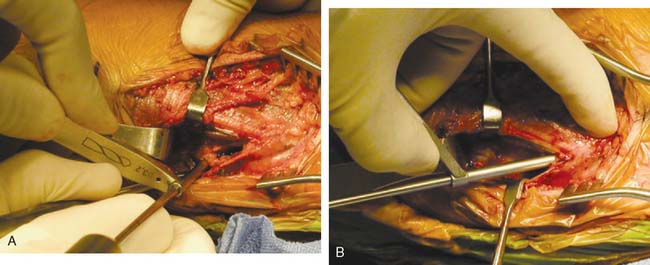
Jobe Technique
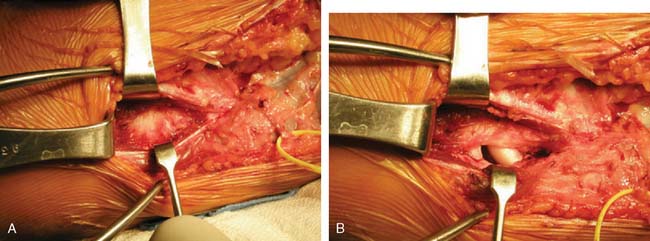
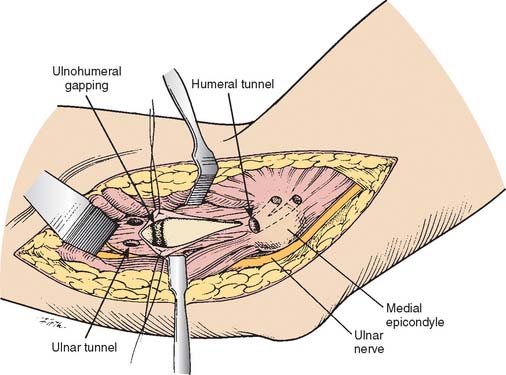
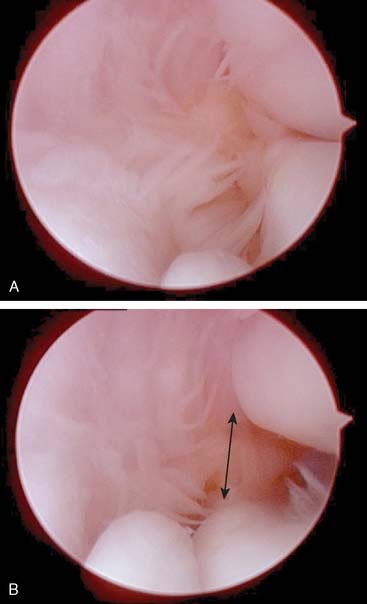
The patient is positioned supine with a pneumatic tourniquet on the upper arm. A skin incision centered over the medial epicondyle is extended 5 cm both proximally and distally. Dissection is carried down to the muscle fascia, and sensory branches of the medial antebrachial cutaneous nerve are consistently identified just anterior and distal to the medial epicondyle. These branches are protected to avoid painful neuroma. A muscle-splitting approach is created by incising the raphe of the flexor carpi ulnaris. A periosteal elevator is used to separate the flexor muscle mass from the MUCL. The ligament is inspected and palpated as valgus stress is applied (Fig. 47-6A). A longitudinal split is made in the ligament and valgus stress applied with the elbow at 30 degrees flexion will reveal opening of the ulnohumeral articulation if the MUCL is insufficient (Fig. 47-6B). Tunnels are then created for graft placement (Fig. 47-7). Converging 3.2-mm drill holes are made in the ulna anterior and posterior to the sublime tubercle with a minimum 5 mm bridge (Fig. 47-8A). The drill holes are connected with an angled curette.
A 4.5 mm drill hole is made at the site of the anatomic origin of the anterior bundle of MUCL on the medial epicondyle that does not penetrate the posterior cortex (Fig. 47-8B). The fascia over the anterior aspect of the epicondyle is split to expose the broad flat surface of the anterosuperior epicondyle. A 3.2-mm drill hole is placed just anterior to the epicondylar attachment of the medial intermuscular septum and directed to communicate with the 4.5-mm drill hole in the epicondyle. A second 3.2-mm drill hole, which is made in the anterosuperior surface of the epicondyle approximately 1 cm from the previous 3.2-mm hole, illustrates the completed humeral bone tunnels.
The palmaris longus from the ipsilateral arm is harvested through a series of small transverse incisions beginning at the distal flexor crease of the wrist. Additional skin incisions are made at 7.5 and 15 cm from the wrist, exposing the entire length of the tendon. Alternatively, the palmaris longus may be harvested with a tendon stripper and a single incision in the flexor crease of the wrist. A number 2 nonabsorbable suture is placed at each end of the graft. The graft is passed through the proximal ulna bone tunnel and medial epicondyle in a figure-of-eight configuration (see Fig. 47-5). With the elbow placed with varus stress, 60 degrees of elbow flexion, and the forearm in supination, tension is applied to the graft. The ulnar side of the graft is sutured to the remnants of the ulnar collateral ligament adjacent to the sublime tubercle. The proximal limb of the graft is sutured to the medial intermuscular septum outside the drill hole on the superior surface of the epicondyle. The elbow is then brought through a ROM to verify isometry of the ligament reconstruction. Simple sutures are placed in the crossing limbs of the graft, which places additional tension on the graft and enhances fixation. The native ligament is then repaired over the graft with the placement of simple sutures. The muscle fascia is repaired, and the skin is closed.
Docking Technique
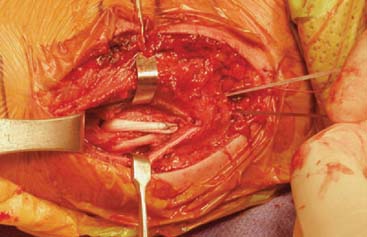
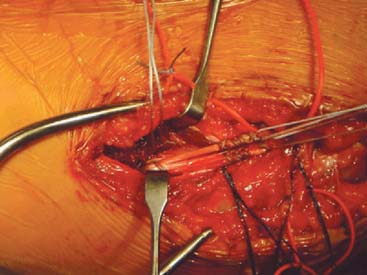
The docking technique is a modification of the Jobe technique that simplifies graft passage, tensioning, and fixation (Fig. 47-9). The docking technique modification uses the muscle-splitting approach with tunnel creation on the ulna similar to the Jobe technique (see Fig. 47-6A and B). The humeral tunnel position is located in the anterior half of the medial epicondyle at the anatomic insertion of the native MUCL similar to the Jobe technique. This tunnel is created to a depth of 15 mm using a 4-mm burr or drill. The upper border of the epicondyle is exposed. Two small exit tunnels separated by 5 mm to 1 cm are created to allow suture passage from the primary humeral tunnel (Fig. 47-10). Suture loops are then placed from the primary humeral tunnel through the exit tunnels to facilitate graft passing. With the elbow in forearm supination and mild varus stress, the horizontal incision in the native MUCL is repaired with a 2.0 absorbable suture.
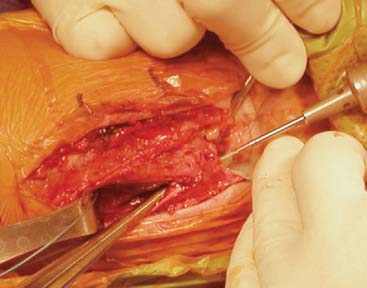
FIGURE 47-10 Exit holes created on superior aspect of epicondyle.
(From Ahmad, C. S., and ElAttrache, N. S.: Elbow valgus instability in the throwing athlete. J. Am. Acad. Orthop. Surg. 14:693, 2006, with permission. © 2006 American Academy of Orthopaedic Surgeons.)
The graft is then passed through the ulnar tunnel from anterior to posterior. The posterior limb of the graft is passed into the humeral tunnel. The final length of the anterior limb of the graft is determined by placing it adjacent to the humeral tunnel and visually estimating the length of the graft that would allow the graft to be tensioned within the humeral tunnel. A No. 1 braided nonabsorbable suture is placed in a Krackow fashion. The excess graft is excised and the graft limb is passed into the humeral tunnel with the sutures exiting the small tunnels. Final graft tensioning is performed by placing the elbow through a full range of motion with varus stress placed on the elbow (Fig. 47-11). The sutures are then tied over the bony bridge on the humeral epicondyle with the elbow in 60 degrees of flexion, supination, and varus stress applied.
Hybrid Interference Screw Fixation Technique
A new technique of MUCL reconstruction has been evaluated in the laboratory that reconstructs the central isometric fibers of the native ligament and achieves ulnar-sided fixation in a single bone tunnel with an interference screw and humeral fixation using the docking technique (Fig. 47-12). This technique is less technically demanding because the required number of drill holes necessary is reduced. Less dissection through a muscle-splitting approach is afforded because only a single central tunnel is required rather than two tunnels with an intervening bony bridge on the ulna. With a single tunnel, the posterior ulnar tunnel, which is in closest proximity to the ulnar nerve, is avoided. Finally, graft passage is less difficult with an interference screw in a single tunnel.
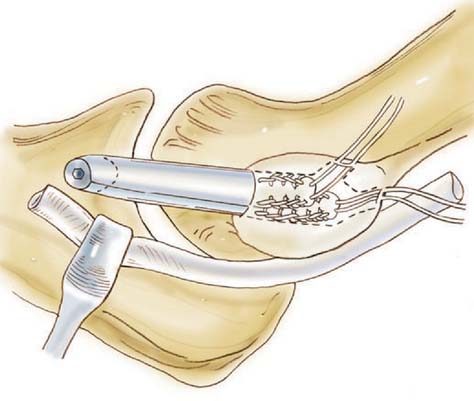
FIGURE 47-12 Interference screw fixation technique.
(Redrawn from Conway, J. E.: The DANE TJ procedure for elbow medial ulnar collateral ligament insufficiency. Tech. Shoulder Elbow Surg. 7:36, 2006, with permission.)
After exposing the MUCL through the muscle-splitting approach as described for the previous techniques (see Fig. 47-6A and B), the central isometric fiber attachments on the ulna and humeral epicondyle are identified to direct tunnel placement. At the insertion on the sublime tubercle of the ulna, approximately 4.5 mm distal to the joint surface, a 5-mm diameter tunnel is drilled and directed 45 degrees distally to the long axis of the ulna for a depth of 20 mm (Fig. 47-13). The size of the tunnel diameter may be increased for larger graft diameters. The drill is advanced with guidance of the drill sleeve that protects the soft tissue and ulnar nerve. Maintenance of a 2-mm bone bridge from the edge of the tunnel to the joint avoids possible fracture of the tunnel into the ulnohumeral joint.

FIGURE 47-13 Ulnar tunnel created at sublime tubercle.
(From Ahmad, C. S., and ElAttrache, N. S.: Elbow valgus instability in the throwing athlete. J. Am. Acad. Orthop. Surg. 14:693, 2006, with permission. © 2006 American Academy of Orthopaedic Surgeons.)
The humeral tunnels are created as described for the docking procedure, as shown in Figure 47-10. The two limbs of the graft are then prepared as described for the docking procedure with the modification that both limbs must be accurately cut to length (Fig. 47-14). The anterior graft limb sutures are then marked with ink for later identification. One suture from the anterior graft limb and posterior graft limb are then passed through the anterior humeral tunnel using a free needle or suture passing wire. The two remaining sutures from each graft limb are passed through the posterior tunnel. The graft is delivered into the humeral tunnel, and the elbow is flexed and extended with tension on the sutures to eliminate any creep. The elbow is positioned at 80 degrees of flexion, varus stress applied, and the posterior limb sutures tied. Then with the elbow positioned at 30 degrees of flexion and varus stress applied, the anterior limb sutures are tied.
SURGICAL CONSIDERATIONS
Graft Choices
The presence or absence of the palmaris longus tendon should be assessed before the procedure. When this tendon is available, it is the tissue of choice for reconstruction for many surgeons; however, absence of the palmaris longus occurs approximately 6% to 25% in the general population.31 When absent, the gracillus, plantaris, Achilles tendon, and toe extensor tendons are alternative options. Our preference is the ipsilateral gracillus when the palmaris is not available because of predictable size and ease of harvest.
Ulnar Nerve
Symptoms of ulnar nerve irritation are present in more than 40% of paitents with UCL insufficiency.6 Inflammation involving UCL traction, friction, and compression can secondarily affect the ulnar nerve as it crossed the elbow. Sources of injury to the ulnar nerve have been divided into three basic groups: compression, friction, and traction. Compression neuropathy can develop secondary to space-occupying lesions such as bony spurs, scar tissue, thickening of the arcuate ligament, calcifications of the MCL, or hypertrophy to the medial head of the triceps. The path of the ulnar nerve about the elbow places it at risk for compression at several anatomic sites including the arcade of Struthers, the medial intermuscular septum, the cubitul tunnel itself, the fascial origin of the flexor digitorum superficialis, and the confluence of the two heads of the FCU. Friction neuropathy results from subluxation of the ulnar nerve over the medial epicondyle. Traction that causes neuritis results from medial elbow instability and repetitive valgus stress to the elbow. Before surgery, the ulnar nerve should be palpated in elbow flexion and extension to assess possible anterior subluxation. Symptoms related to ulnar nerve irritation should be ascertained such as numbness in the fourth and fifth digits. We reserve ulnar nerve transposition in patients with ulnar neuritis that involves compromised motor function or ulnar neuritis combined with ulnar nerve subluxation.
Arthroscopy
Arthroscopic evaluation of the elbow joint before MUCL reconstruction has been advocated by some.4,27 Arthroscopic assessment of valgus stability may be performed by placing valgus stress to the elbow while positioned at 90 degrees of flexion and the forearm maximally pronated. Normal elbows demonstrate a maximum of 1 to 2 mm of opening, whereas elbows with MUCL insufficiency demonstrate greater than 2 to 3 mm of opening (Fig. 47-15). Although ulnohumeral opening may be appreciated, a cadaveric study demonstrated that the anterior bundle of the MUCL cannot be directly visualized arthroscopically. Arthroscopy does facilitate diagnostic examination of the anterior and posterior compartments, and associated procedures may be performed when necessary such as removal of loose bodies and marginal osteophytes, anterior capsular release, and anterior, posterior, or lateral débridement.12
Valgus Extension Overload
Throwing may also result in posterior elbow pain because the olecranon is repeatedly and forcefully driven into the olecranon fossa. Knowledge of the relationship between the posterior compartment contributions to elbow stability from bony articulations and the soft tissue MUCL is an important concept in the pathophysiology of valgus instability. Andrews et al3 reported that in a series of professional baseball players who underwent olecranon débridement, 25% developed valgus instability and eventually required MUCL reconstruction. This observation suggests that both the olecranon and the MUCL contribute to valgus stability. A recent biomechanical study demonstrated that sequential partial resection of the posteromedial aspect of the olecranon resulted in stepwise increases in elbow valgus angulation.19 Kamineni et al18 also confirmed in a cadaver model that strain in the AOL is increased with increasing posteromedial olecranon resection beyond 3 mm. These studies suggest that aggressive olecranon resection put the MUCL at risk for injury. A different concept suggests that subtle valgus instability may lead posteromedial osteophyte formation.2 MUCL injury simulated in a cadaver model results in contact alterations in the posterior compartment that leads to osteophyte formation. This suggests that patients with posteromedial impinge ment pain should be critically evaluated for suspected MUCL pathology.
POSTOPERATIVE REHABILITATION
PEARLS
Several aspects of MUCL reconstruction enhance success. The location of the inferior humeral tunnel is extremely important to ensure an isometric graft. Limited dissection of the flexor pronator mass is essential to optimize dynamic stability to the elbow. Less handling of the ulnar nerve has been attributed to improved outcome.30 For all reconstruction techniques described, we prefer to repair the native ligament underneath the reconstruction to keep the new graft extrasynovial. The synovial environment may have inflammatory mediators that delay healing and also cause tunnel expansion if access is gained to the drilled tunnels.
RESULTS
MUCL reconstruction is technically demanding with regard to limiting muscular dissection and avoiding ulnar nerve injury. Furthermore, achieving graft isometry, adequate graft tension, and secure graft fixation remain challenging while optimizing graft healing biology. Reports of clinical outcome for MUCL reconstruction have been variable, with 68% to 93% having good to excellent results. In a recent study using a muscle-splitting approach without ulnar nerve transposition, 93% of patients who had no previous elbow surgery had excellent results at 2-year follow-up.30 Prognostic factors were related to associated pathology and history of previous surgery such as olecranon resection. Modifications in surgical technique consisting of minimizing dissection of the flexor-pronator mass and handling of the ulnar nerve have been attributed to improved outcome. Less dissection of the muscle mass seems to reduce morbidity to the muscles that dynamically stabilize the medial aspect of the elbow.
Azar et al4 reported on 78 throwing athletes who underwent MUCL reconstruction with submuscular ulnar nerve transposition. Fifty-nine patients were available for follow-up at 12 to 72 months. Of those patients, 81% returned to the same or higher level of competition. One patient had ulnar nerve symptoms that eventually resolved 10 months after surgery.4 Rohrbough et al27 reported on 36 patients who underwent the docking technique of MUCL reconstruction. At an average follow-up of 3.3 years, 92% returned to or exceeded their previous level of competition for at least 1 year. A review 100 consecutive overhead-throwing athletes who underwent the docking reconstruction technique with a mean follow-up of 36 months found that 90% were able to compete at the same or a higher level for more than 12 months.9 Another modification of the docking technique using a 4-strand palmaris longus graft for reconstruction has been reported in 25 elite professional and collegiate baseball players with a minimum 2-year follow-up.23 Ninety-two percent were able to return to their preinjury level of competition.
The technique of interference screw fixation has been biomechanically evaluated in cadavers, and graft fixation strength was 95% that of control intact MUCLs under valgus load.1 Reconstruction of the MUCL also restored valgus stability to within less than one degree of the intact elbow for all flexion angles.1
Clinical results for the hybrid technique with ulnar screw fixation and humeral docking fixation have been encouraging.8 During a 3-year period, 22 athletes were treated with this technique and evaluated at a minimum of 2 years postoperatively. Nineteen of twenty-two patients had excellent results. There were two fair and one poor result. The poor result was in a revision case. The two other revision UCL reconstructions had excellent outcomes. Additionally, when used in two cases of sublime tubercle avulsions, the results were excellent. Postoperative complications occurred in four patients: two patients developed ulnar neuritis, and two patients required second surgeries for lysis of adhesions. Three of these four patients went on to have excellent outcomes.
1 Ahmad C.S., Lee T.Q., ElAttrache N.S. Biomechanical evaluation of a new ulnar collateral ligament reconstruction technique with interference screw fixation. Am. J. Sports Med. 2003;31:332.
2 Ahmad C.S., Park M.C., ElAttrache N.S. Elbow medial ulnar collateral ligament insufficiency alters posteromedial olecranon contact. Am. J. Sports Med. 2004;32:1607.
3 Andrews J.R., Timmerman L.A. Outcome of elbow surgery in professional baseball players. Am. J. Sports Med. 1995;23:407.
4 Azar F.M., Andrews J.R., Wilk K.E., Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am. J. Sports Med. 2000;28:16.
5 Callaway G.H., Field L.D., Deng X.H., Torzilli P.A., O’Brien S.J., Altchek D.W., Warren R.F. Biomechanical evaluation of the medial collateral ligament of the elbow. J. Bone Joint Surg. Am. 1997;79:1223.
6 Conway J.E., Jobe F.W., Glousman R.E., Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J. Bone Joint Surg. Am. 1992;74:67.
7 Cotton A., Jacobson J., Brossmann J., Pedowitz R., Haghighi P., Trudell D., Resnick D. Collateral ligaments of the elbow: conventional MR imaging and MR arthrography with coronal oblique plane and elbow flexion. Radiology. 1997;204:806.
8 Dines, J. S., ElAttrache, N. S., Conway, W., Ahmad, C. S., and Conway, J. E.: Clinical Outcomes of the Dane TJ Technique to Address Medial Ulnar Collateral Ligament Insufficiency of the Elbow. American Orthopaedic Society for Sports Medicine Annual Meeting; 2007 July 15, 2007; Calgary, Canada; 2007.
9 Dodson C.C., Thomas A., Dines J.S., Nho S.J., Williams R.J.3rd, Altchek D.W. Medial ulnar collateral ligament reconstruction of the elbow in throwing athletes. Am. J. Sports Med. 2006;34:1926.
10 Ellenbecker T.S., Mattalino A.J., Elam E.A., Caplinger R.A. Medial elbow joint laxity in professional baseball pitchers. A bilateral comparison using stress radiography. Am. J. Sports Med. 1998;26:420.
11 Elliott B., Fleisig G., Nicholls R., Escamilia R. Technique effects on upper limb loading in the tennis serve. J. Sci. Med. Sport. 2003;6:76.
12 Field L.D., Callaway G.H., O’Brien S.J., Altchek D.W. Arthroscopic assessment of the medial collateral ligament complex of the elbow. Am. J. Sports Med. 1995;23:396.
13 Fleisig G., Nicholls R., Elliott B., Escamilla R. Kinematics used by world class tennis players to produce high-velocity serves. Sports Biomech. 2003;2:51.
14 Fleisig G.S., Andrews J.R., Dillman C.J., Escamilla R.F. Kinetics of baseball pitching with implications about injury mechanisms. Am. J. Sports Med. 1995;23:233.
15 Hill N.B.Jr, Bucchieri J.S., Shon F., Miller T.T., Rosenwasser M.P. Magnetic resonance imaging of injury to the medial collateral ligament of the elbow: a cadaver model. J. Shoulder Elbow Surg.. 2000;9:418.
16 Hotchkiss R.N., Weiland A.J. Valgus stability of the elbow. J. Orthop. Res. 1987;5:372.
17 Jobe F.W., Stark H., Lombardo S.J. Reconstruction of the ulnar collateral ligament in athletes. J. Bone Joint Surg. Am. 1986;68:1158.
18 Kamineni S., ElAttrache N.S., O’Driscoll S.W., Ahmad C.S., Hirohara H., Neale P.G., An K.N., Morrey B.F. Medial collateral ligament strain with partial posteromedial olecranon resection. A biomechanical study. J. Bone Joint Surg. Am. 2004;86-A:2424.
19 Kamineni S., Hirahara H., Pomianowski S., Neale P.G., O’Driscoll S.W., ElAttrache N., An K.N., Morrey B.F. Partial posteromedial olecranon resection: a kinematic study. J. Bone Joint Surg. Am. 2003;85-A:1005.
20 Morrey B.F., An K.N. Articular and ligamentous contributions to the stability of the elbow joint. Am. J. Sports Med. 1983;11:315.
21 Munshi M., Pretterklieber M.L., Chung C.B., Haghighi P., Cho J.H., Trudell D.J., Resnick D. Anterior bundle of ulnar collateral ligament: evaluation of anatomic relationships by using MR imaging, MR arthrography, and gross anatomic and histologic analysis. Radiology. 2004;231:797.
22 O’Driscoll S.W., Jaloszynski R., Morrey B.F., An K.N. Origin of the medial ulnar collateral ligament. J. Hand Surg. [Am.]. 1992;17:164.
23 Paletta G.A.Jr, Wright R.W. The modified docking procedure for elbow ulnar collateral ligament reconstruction: 2-year follow-up in elite throwers. Am. J. Sports Med. 2006;34:1594.
24 Park M.C., Ahmad C.S. Dynamic contributions of the flexor-pronator mass to elbow valgus stability. J. Bone Joint Surg. Am. 2004;86-A:2268.
25 Regan W.D., Korinek S.L., Morrey B.F., An K.N. Biomechanical study of ligaments around the elbow joint. Clin. Orthop. 1991;271:170.
26 Rettig A.C., Sherrill C., Snead D.S., Mendler J.C., Mieling P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am. J. Sports Med. 2001;29:15.
27 Rohrbough J.T., Altchek D.W., Hyman J., Williams R.J.3rd, Botts J.D. Medial collateral ligament reconstruction of the elbow using the docking technique. Am. J. Sports Med. 2002;30:541.
28 Sasaki J., Takahara M., Ogino T., Kashiwa H., Ishigaki D., Kanauchi Y. Ultrasonographic assessment of the ulnar collateral ligament and medial elbow laxity in college baseball players. J. Bone Joint Surg. Am. 2002;84-A:525.
29 Smith G.R., Altchek D.W., Pagnani M.J., Keeley J.R. A muscle-splitting approach to the ulnar collateral ligament of the elbow. Neuroanatomy and operative technique. Am. J. Sports Med. 1996;24:575.
30 Thompson W.H., Jobe F.W., Yocum L.A., Pink M.M. Ulnar collateral ligament reconstruction in athletes: Muscle-splitting approach without transposition of the ulnar nerve. J. Shoulder Elbow Surg. 2001;10:152.
31 Vanderhooft E. The frequency of and relationship between the palmaris longus and plantaris tendons. Am. J. Orthop. 1996;25:38.
32 Waris W. Elbow injuries in javelin throwers. Acta Chir. Scand. 1946;93:563.
33 Werner S.L., Fleisig G.S., Dillman C.J., Andrews J.R. Biomechanics of the elbow during baseball pitching. J. Orthop. Sports Phys. Ther. 1993;17:274.