81
Dermal Hypertrophies
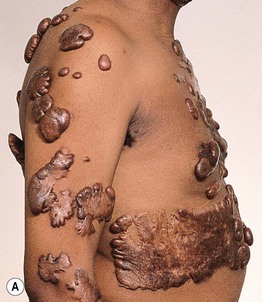
Hypertrophic Scar
• Firm, initially pink to purple in color then becomes skin-colored to hypopigmented, occasionally hyperpigmented; papule or plaque limited to an excision site or wound (Figs. 81.1 and 81.2).

Fig. 81.1 Hypertrophic scar at the site of an excision of an atypical melanocytic nevus. The deltoid region is a common location for hypertrophic scars. Courtesy, Jean L. Bolognia, MD.

Fig. 81.2 Multiple hypertrophic scars due to acne vulgaris. The posterior trunk is a common location for hypertrophic scars. Courtesy, Julie V. Schaffer, MD.
• Most commonly seen on the trunk/shoulders.
• With treatment, can reduce pruritus and height but not width of scar.
Keloid
• More common in patients with darkly pigmented skin who have a familial predisposition.
• Rarely associated with syndromes (e.g. Rubinstein–Taybi or Goeminne syndromes).
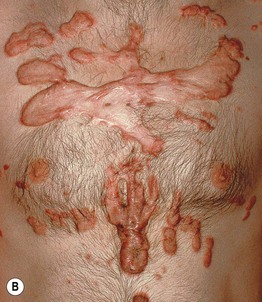
• Raised, often skin-colored firm plaque(s) that, in contrast to hypertrophic scars, extend beyond the wound margin (Fig. 81.3; Table 81.1); color may vary as in hypertrophic scars.

Fig. 81.3 Keloid of the flexor arm in an African-American man. Note the extension of the keloid into the normal surrounding skin in a claw-like manner and the central involution. Courtesy, Claude Burton, MD.
• Follow trauma from surgical procedures (including ear piercing) and inflammatory disorders, especially acne (see Fig. 81.2), but can occur spontaneously (Fig. 81.4).
Dupuytren’s Contracture
• Fibromatosis of the fascia of the ventral aspect of the digit and the palm.
• May gradually progress to flexion contractures (Fig. 81.5).

Fig. 81.5 Dupuytren’s contracture. There is greater involvement of the fifth finger than the fourth finger. Fibrotic cords can be felt and are accentuated by extension of the digits. Eventually, flexion contractures develop. Courtesy, Jean L. Bolognia, MD.
• Associated with other fibromatoses (e.g. plantar, penile), alcoholism, and diabetes mellitus.
• Surgical correction usually helpful; injection of collagenase also sometimes effective.
Cutis Verticis Gyrata
• Hypertrophy and linear folding of the scalp only (Fig. 81.6).

Fig. 81.6 Cutis verticis gyrata. Cerebriform folding of the skin of the scalp. Erythema in the posterior grooves is related to a previous superinfection.
• Primary form may be associated with systemic findings (neurologic, ophthalmologic).
• Secondary form associated with acromegaly, myxedema, and Turner syndrome.
• Differential diagnosis includes several disorders, including pachydermoperiostitis (involves the face and acral sites as well as the scalp), dissecting cellulitis (scalp is boggy and painful), and plexiform neurofibroma.
Hyaline Fibromatosis Syndrome (Juvenile Hyaline Fibromatosis and Infantile Systemic Hyalinosis)
• Autosomal recessive spectrum of disorders due to ANTXR2 mutations.
• Presents during infancy or early childhood with papulonodules on the ears, hands, and periorificial areas (Fig. 81.7), in addition to gingival hypertrophy and flexion contractures.
• Severe form (infantile systemic hyalinosis) has internal organ involvement.
For further information see Ch. 98. From Dermatology, Third Edition.