http://evolve.elsevier.com/McCuistion/pharmacology
Drugs that are central nervous system (CNS) depressants cause varying degrees of depression (reduction in functional activity) within the CNS. The degree of depression depends primarily on the drug and the amount of drug taken. The broad classification of CNS depressants includes sedative-hypnotics, general anesthetics, analgesics, opioid and nonopioid analgesics, anticonvulsants, antipsychotics, and antidepressants. The last five groups of depressant drugs are presented in separate chapters. Sedative-hypnotics and general anesthetics are discussed in this chapter.
Types and Stages of Sleep
Sleep disorders such as insomnia, the inability to fall asleep or remain asleep, occur in 10% to 30% of Americans. Insomnia occurs more frequently in women, and the incidence increases with age.
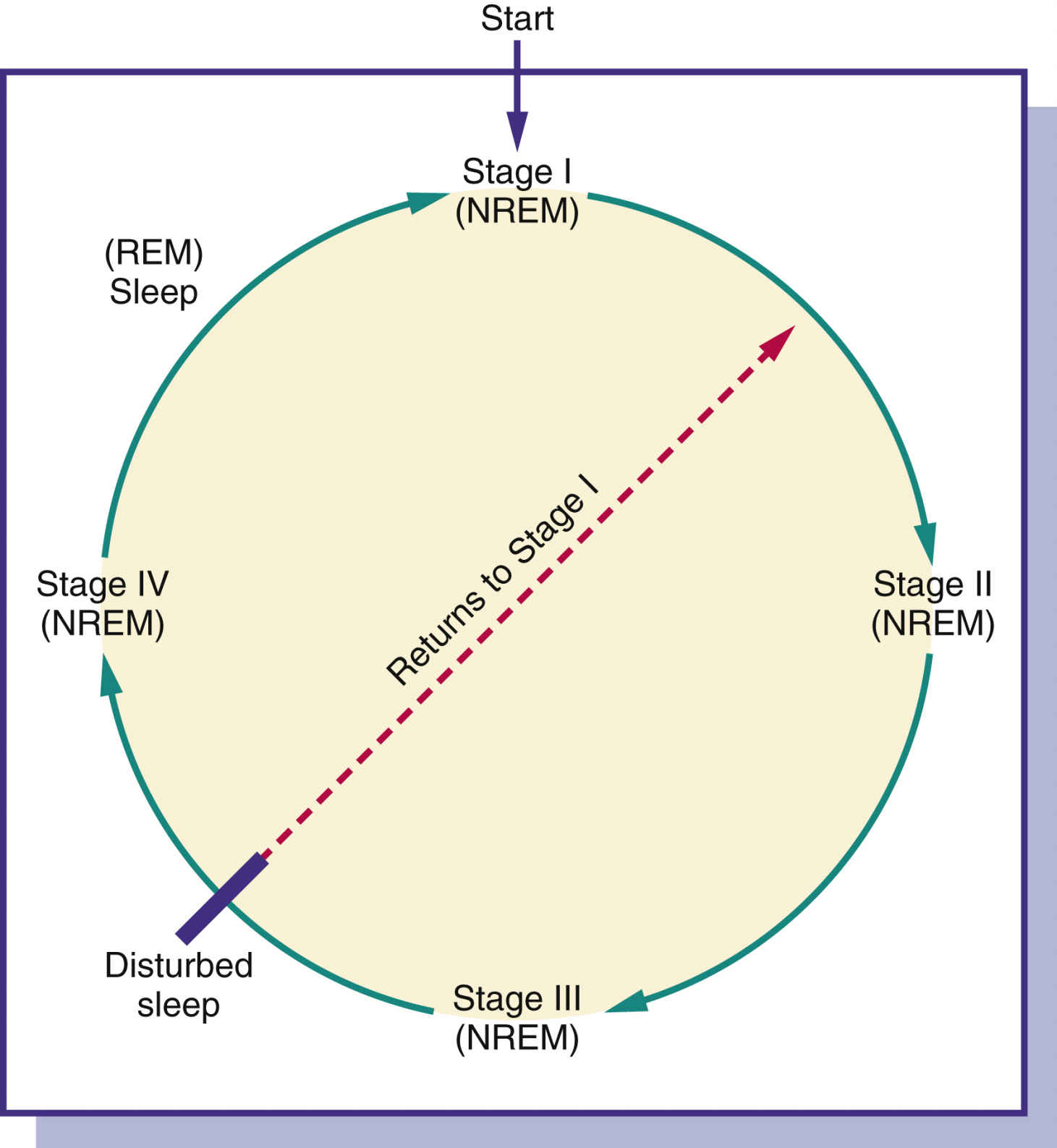
People spend approximately one third of their lives, or as much as 25 years, sleeping. Normal sleep is composed of two definite phases: rapid eye movement (REM) and nonrapid eye movement (NREM) sleep. Both REM and NREM sleep occur cyclically at about 90-minute intervals during sleep (Fig. 18.1). The four succeedingly deeper stages of NREM sleep end with an episode of REM sleep, and the cycle begins again. If sleep is interrupted, the cycle begins again with stage 1 of NREM sleep. Individuals perform better during their waking hours if they experience all types and stages of sleep.
During REM sleep, individuals experience most of their recallable dreams. Children have few REM sleep periods and have longer periods of stage 3 and 4 NREM sleep. Older adults experience a decrease in stage 3 and 4 NREM sleep and have frequent waking periods.
It is difficult to rouse a person during REM sleep, and the period of REM sleep episodes becomes longer during the sleep process. Frequently, if a person is roused from REM sleep, a vivid, bizarre dream may be recalled. If these dreams are unpleasant, they may be called nightmares. Sleepwalking or nightmares that occur in children take place during NREM sleep.
Nonpharmacologic Methods
Before using sedative-hypnotics or over-the-counter (OTC) sleep aids, various nonpharmacologic methods should be used to promote sleep. Once the nurse discovers why the patient cannot sleep, the following ways to promote sleep may be suggested:
1. Arise at a specific hour in the morning.
2. Take few or no daytime naps.
3. Avoid drinks that contain caffeine and alcohol 6 hours before bedtime. Also avoid smoking nicotine products for 6 hours before bedtime.
4. Avoid heavy meals or strenuous exercise before bedtime.
5. Take a warm bath, listen to quiet music, or perform other soothing activities before bedtime.
6. Decrease exposure to loud noises.
7. Avoid drinking copious amounts of fluids before sleep.
8. Drink warm milk before bedtime.
Sedative-Hypnotics
Sedative-hypnotics are commonly ordered for treatment of sleep disorders. The mildest form of CNS depression is sedation, which diminishes physical and mental responses at lower dosages of certain CNS depressants but does not affect consciousness. Sedatives are used mostly during the daytime. Increasing the drug dose can produce a hypnotic effect—not hypnosis but a form of “natural” sleep. Sedative-hypnotic drugs are sometimes the same drug; however, certain drugs are used more often for their hypnotic effect. With very high doses of sedative-hypnotic drugs, anesthesia may be achieved.
Sedatives were first prescribed to reduce tension and anxiety. Barbiturates were initially used for their antianxiety effect until the early 1960s, when benzodiazepines were introduced. Because of the many side effects of barbiturates and their potential for physical and mental dependency, they are now less frequently prescribed.
The Centers for Disease Control and Prevention cite that approximately 70 million Americans have chronic sleep problems and suffer from sleep deprivation. The cost is billions of dollars in lost productivity, and millions of dollars are spent each year on OTC sleep aids. The primary ingredient in OTC sleep aids is an antihistamine such as diphenhydramine.
Hypnotics may be short or intermediate acting. Short-acting hypnotics are useful in achieving sleep because they allow the patient to awaken early in the morning without experiencing lingering side effects. Intermediate-acting hypnotics are useful for sustaining sleep; however, after using one, the patient may experience residual drowsiness, or hangover, in the morning. This may be undesirable if the patient is active and requires mental alertness. The ideal hypnotic promotes natural sleep without disrupting normal patterns of sleep and produces no hangover or undesirable effect. Table 18.1 lists the common side effects and adverse reactions associated with sedative-hypnotic use and abuse.
Hypnotic drug therapy should usually be short term to prevent drug dependence and tolerance. Interrupting hypnotic therapy can decrease drug tolerance, but abruptly discontinuing a high dose of hypnotic taken over a long period can cause withdrawal symptoms. In such cases, the dose should be tapered to avoid withdrawal symptoms. As a general rule, the lowest dose should be taken to achieve sleep. Patients with severe respiratory disorders should avoid hypnotics, which could cause an increase in respiratory depression. Usually, hypnotics are contraindicated during pregnancy. Ramelteon is the only major sedative-hypnotic approved for long-term use. This drug may be used for treating chronic insomnia.
TABLE 18.1
Common Side Effects and Adverse Reactions of Sedative-Hypnotics
| Side Effects and Adverse Reactions | Explanation of the Effects |
| Hangover | A hangover is residual drowsiness resulting in impaired reaction time. The intermediate- and long-acting hypnotics are frequently the cause of drug hangover. The liver biotransforms these drugs into active metabolites that persist in the body, causing drowsiness. |
| REM rebound | REM rebound, which results in vivid dreams and nightmares, frequently occurs after taking a hypnotic for a prolonged period then abruptly stopping. However, it may occur after taking only one hypnotic dose. |
| Dependence | Dependence is the result of chronic hypnotic use. Physical and psychological dependence can result. Physical dependence results in the appearance of specific withdrawal symptoms when a drug is discontinued after prolonged use. The severity of withdrawal symptoms depends on the drug and dosage. Symptoms may include muscular twitching and tremors, dizziness, orthostatic hypotension, delusions, hallucinations, delirium, and seizures. Withdrawal symptoms start within 24 hours and can last for several days. |
| Tolerance | Tolerance results when there is a need to increase the dosage over time to obtain the desired effect. It is mostly caused by an increase in drug metabolism by liver enzymes. The barbiturate drug category can cause tolerance after prolonged use. Tolerance is reversible when the drug is discontinued. |
| Excessive depression | Long-term use of a hypnotic may result in CNS depression, which is characterized by lethargy, sleepiness, lack of concentration, confusion, and psychological depression. |
| Respiratory depression | High doses of sedative-hypnotics can suppress the respiratory center in the medulla. |
| Hypersensitivity | Skin rashes and urticaria can result when taking barbiturates. Such reactions are rare. |
The category of sedative-hypnotics includes barbiturates, benzodiazepines, and nonbenzodiazepines, among others. Each category is discussed separately. Prototype drug charts are included for benzodiazepines and nonbenzodiazepines.
Barbiturates
Barbiturates were introduced as a sedative in the early 1900s. They are classified as long, intermediate, short, and ultrashort acting.
• The long-acting group includes phenobarbital and mephobarbital, which are used to control seizures in epilepsy.
• The intermediate-acting barbiturates, such as butabarbital, are useful as sleep sustainers for maintaining long periods of sleep. Because these drugs take approximately 1 hour for the onset of sleep, they are not prescribed for those who have trouble getting to sleep. Vital signs should be closely monitored in persons who take intermediate-acting barbiturates.
• The short-acting barbiturate secobarbital may be used for procedure sedation. Vital signs should be closely monitored in persons who take short-acting barbiturates.
Barbiturates should be restricted to short-term use (2 weeks or less) because of their numerous side effects, including tolerance to the drug. In the United States, barbiturates are classified under the Controlled Substances Act as Schedule II for short-acting, Schedule III for intermediate-acting, and Schedule IV for long-acting hypnotics. In Canada, barbiturates are classified as Schedule G. Barbiturates are listed in Table 18.2.
Pharmacokinetics
Pentobarbital has been available for nearly half a century and was the hypnotic of choice until the introduction of benzodiazepines in the 1960s. It has a slow absorption rate and is moderately protein bound. The long half-life is mainly because of the formation of active metabolites resulting from liver metabolism.
Pharmacodynamics
Pentobarbital and secobarbital are used primarily for short-term treatment of insomnia. Other uses include control of seizures, preoperative anxiety, and sedation induction. They have a rapid onset with a short duration of action and are considered short-acting barbiturates. The onset of action of pentobarbital is slower when administered intramuscularly (IM) than when administered orally (PO).
Many drug interactions are associated with barbiturates. Alcohol, narcotics, and other sedative-hypnotics used in combination with barbiturates may further depress the CNS. Pentobarbital increases hepatic enzyme action, causing an increased metabolism and decreased effect of drugs such as oral anticoagulants, glucocorticoids, tricyclic antidepressants, and quinidine. Pentobarbital may cause hepatotoxicity if taken with large doses of acetaminophen.
 Benzodiazepines
Benzodiazepines
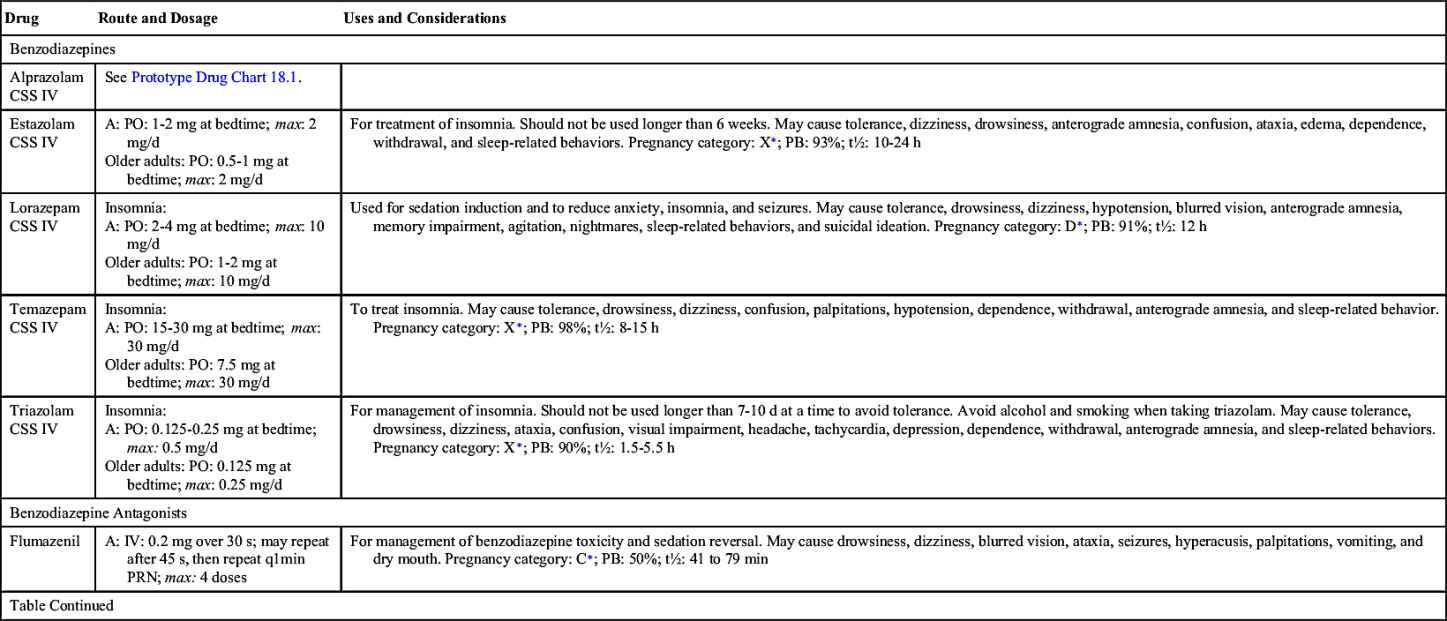
Selected benzodiazepines, minor tranquilizers and anxiolytics, were introduced with chlordiazepoxide in the 1960s as antianxiety agents. This drug group is ordered as sedative-hypnotics for inducing sleep. Several benzodiazepines marketed as hypnotics include flurazepam, alprazolam (Prototype Drug Chart 18.1), temazepam, triazolam, estazolam, and quazepam (Table 18.3). Increased anxiety might be the cause of insomnia for some patients, so lorazepam and diazepam can be used to alleviate the anxiety. These drugs are classified as Schedule IV according to the Controlled Substances Act. The benzodiazepines increase the action of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA) to the GABA receptors. Neuron excitability is reduced.
 Cultural Considerations
Cultural Considerations• Use an interpreter as needed, and involve extended family in health teaching and support.
• Provide written instruction or videos in the patient’s preferred language.
Evaluation
• Assess the effectiveness of benzodiazepines.
• Evaluate respiratory status to ensure that respiratory depression has not occurred.
Benzodiazepines (except for temazepam) can suppress stage 4 of NREM sleep, which may result in vivid dreams or nightmares and can delay REM sleep. Benzodiazepines are effective for sleep disorders for several weeks longer than other sedative-hypnotics; to prevent REM rebound, however, they should not be used for longer than 3 to 4 weeks.
Triazolam is a short-acting hypnotic with a half-life of 2 to 5 hours. It does not produce any active metabolites. Adverse effects of anterograde amnesia or memory impairment occur more frequently with triazolam than with other benzodiazepines, and the risk increases with higher doses and with concurrent alcohol or opioid ingestion. Currently, it is seldom prescribed and should not be taken longer than 7 to 10 days.
One adverse effect closely associated with benzodiazepines is anterograde amnesia, an impaired ability to recall events that occur after dosing. Associated with anterograde amnesia are sleep-related behaviors, such as preparing and eating meals, sleep driving, engaging in sex, or making phone calls during sleep without any memory of the event. Alcohol and CNS depressants increase the risk of sleep-related behaviors.
Small doses of benzodiazepines are recommended for patients with renal or hepatic dysfunction. For benzodiazepine overdose, the benzodiazepine antagonist flumazenil may be prescribed. Benzodiazepines prescribed as antianxiety drugs are discussed in Chapter 22.
Pharmacokinetics
Benzodiazepines are well absorbed through the gastrointestinal (GI) mucosa. They are rapidly metabolized in the liver to active metabolites. Benzodiazepines have an intermediate half-life of usually 8 to 24 hours. These drugs are highly protein bound, and more free drug is available when benzodiazepines are taken with other highly protein-bound drugs, which increases the risk for adverse effects.
Pharmacodynamics
Benzodiazepines are used to treat insomnia by inducing and sustaining sleep. They have a rapid onset of action and intermediate- to long-acting effects. The normal recommended dose of a benzodiazepine may be too much for the older adult, so half the dose is recommended initially to prevent overdosing.
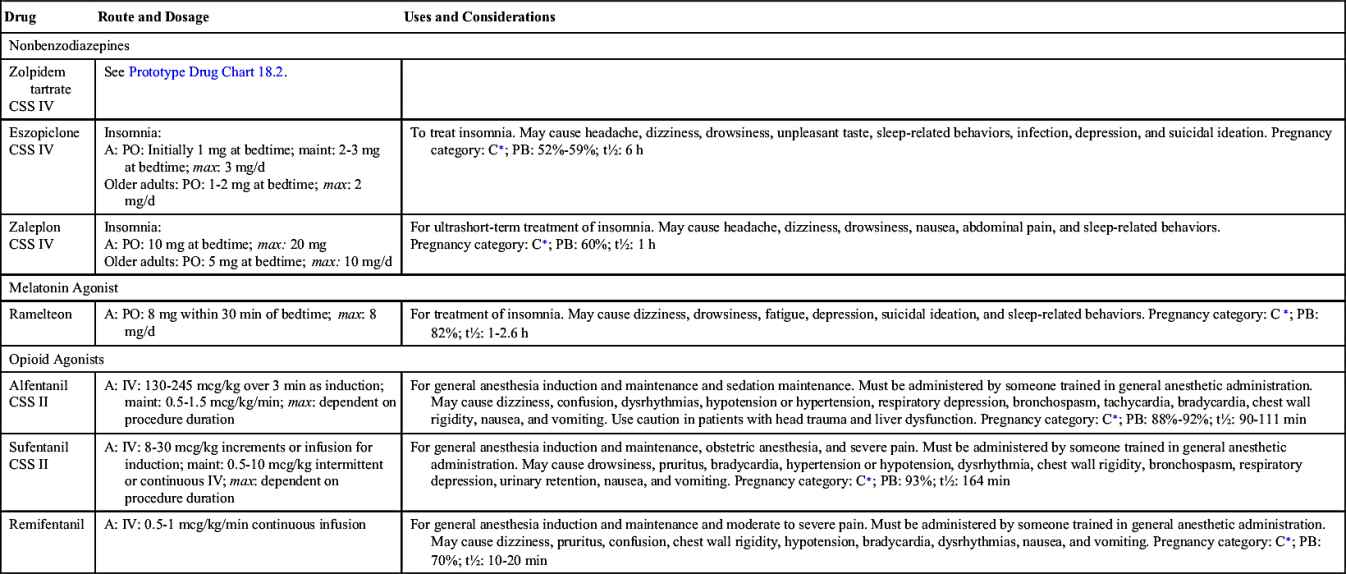
Nonbenzodiazepines
Zolpidem is a nonbenzodiazepine that differs in chemical structure from benzodiazepines. It is used for short-term treatment (<10 days) of insomnia. Its duration of action is 6 to 8 hours with a short half-life of 1.4 to 6.73 hours. Zolpidem is metabolized in the liver to three inactive metabolites and is excreted in bile, urine, and feces. When zolpidem is prescribed for older adults, the dose should be decreased. Table 18.3 lists the benzodiazepines and nonbenzodiazepines used as sedative-hypnotics and their dosages, uses, and considerations including common side effects and a few serious adverse effects. Zolpidem is described in Prototype Drug Chart 18.2.
Melatonin Agonists
Ramelteon is in the newest category of sedative-hypnotics called melatonin agonists. Ramelteon is the first hypnotic approved by the U.S. Food and Drug Administration (FDA) that is not classified as a controlled substance. This drug acts by selectively targeting melatonin receptors to regulate circadian rhythms in the treatment of insomnia. Ramelteon has not been shown to decrease REM sleep. This new drug has a half-life of 1 to 2.6 hours. Adverse effects of ramelteon include drowsiness, dizziness, fatigue, headache, nausea, and suicidal ideation.
Sedatives and Hypnotics for Older Adults
Identifying the cause of insomnia in an older adult should be the first diagnostic consideration, and nonpharmacologic methods should be used before sleep medications are prescribed. Because of physiologic changes in older adults, the use of hypnotics can cause a variety of side effects.
Barbiturates increase CNS depression and confusion in older adults and should not be taken for sleep. The short- to intermediate-acting benzodiazepines—such as estazolam, temazepam, and triazolam—are considered to be safer than barbiturates. Long-acting hypnotic benzodiazepines such as flurazepam, quazepam, and diazepam should be avoided. In many cases, older adults should be instructed to take the prescribed benzodiazepine no more than four times a week to avoid side effects and drug dependency. They can choose selected nights to take the hypnotic.
The main sleep problem experienced by older adults is frequent nighttime awakening. Reports have shown that older women experience more troublesome sleep patterns than men. Sleep disturbance may be caused by discomfort or pain. Occasionally a nonsteroidal antiinflammatory drug (NSAID) such as ibuprofen may alleviate the discomfort that prevents sleep.
 Cultural Considerations
Cultural Considerations• Ask patients about methods family members have used to promote sleep.
• Suggest nonpharmacologic alternatives that may be effective in inducing sleep.
Evaluation
• Evaluate effectiveness of sedative-hypnotics in promoting sleep.
• Determine whether side effects such as hangover occur after several days of taking a sedative-hypnotic. Another hypnotic may be prescribed if side effects persist.
 Anesthetics
Anesthetics
Anesthetics are classified as general and local. General anesthetics depress the CNS, alleviate pain, and cause a loss of consciousness. The first anesthetic, nitrous oxide (“laughing gas”), was used for surgery in the early 1800s. It is still an effective anesthetic and is frequently used in dental procedures and surgery.
Pathophysiology
Several theories exist regarding how inhalation anesthetics cause CNS depression and a loss of consciousness. The differing theories suggest the following about inhalation anesthetics:
1. The lipid structure of cell membranes is altered, resulting in impaired physiologic functions.
2. The inhibitory neurotransmitter GABA is activated to the GABA receptor that pushes chloride ions into the neurons. This greatly decreases the fire action potentials of the neurons.
3. The ascending reticular activating system is altered, and the neurons cease to transmit information (stimuli) to the brain.
Balanced Anesthesia
Balanced anesthesia is a combination of drugs frequently used in general anesthesia. Balanced anesthesia may include the following:
1. A hypnotic given the night before
2. Premedication with an opioid analgesic or benzodiazepine (e.g., midazolam) plus an anticholinergic (e.g., atropine) given about 1 hour before surgery to decrease secretions
3. A short-acting nonbarbiturate such as propofol
4. An inhaled gas, often a combination of an inhalation anesthetic, nitrous oxide, and oxygen
5. A muscle relaxant given as needed
Balanced anesthesia minimizes cardiovascular problems, decreases the amount of general anesthetic needed, reduces possible postanesthesia nausea and vomiting, minimizes the disturbance of organ function, and decreases pain. Because the patient does not receive large doses of general anesthetics, fewer adverse reactions occur; and recovery is enhanced by allowing quicker mobility.
Stages of General Anesthesia
General anesthesia proceeds through four stages (Table 18.4). The surgical procedure is usually performed during the third stage. If an anesthetic agent is given immediately before inhalation anesthesia, the third stage can occur without the early stages of anesthesia being observed. However, if the drug is given slowly, all stages of anesthesia are usually observed.
Assessment Before Surgery
The patient’s response to anesthesia may differ according to variables related to the health status of the individual. These variables include age (young and older adults), a current health disorder (e.g. cardiovascular, pulmonary, renal, liver), pregnancy, history of heavy smoking, and frequent use of alcohol and drugs. These problems must be identified before surgery because the type and amount of anesthetic required may need to be adjusted.
Inhalation Anesthetics
During the third stage of anesthesia, inhalation anesthetics—that is, gas or volatile liquids administered as gas—are used to deliver general anesthesia. Certain gases, notably nitrous oxide, are absorbed quickly, have a rapid action, and are eliminated rapidly. Cyclopropane was a popular inhalation anesthetic from 1930 to 1960, but because of its highly flammable state as ether, it is no longer used. In the late 1950s, halothane was introduced as a nonflammable alternative. Other inhalation drugs used as anesthetics include enflurane, isoflurane, desflurane, and sevoflurane.
Inhalation anesthetics typically provide smooth induction. Upon discontinuing administration of halothane, isoflurane, and enflurane, recovery of consciousness usually occurs in approximately 1 hour. Recovery from desflurane and sevoflurane is within minutes. Inhalation anesthetics are usually combined with a nonbarbiturate, such as propofol; a strong analgesic, such as morphine; and a muscle relaxant, such as pancuronium, for surgical procedures.
Adverse effects from inhalation anesthetics include respiratory depression, hypotension, dysrhythmias, and hepatic dysfunction. In patients at risk, these drugs may trigger malignant hyperthermia. The newer drugs primarily cause less nausea and vomiting than the older anesthetics.
Intravenous Anesthetics
Intravenous (IV) anesthetics may be used for general anesthesia or for the induction stage of anesthesia. For outpatient surgery of short duration, an IV anesthetic might be the preferred form of anesthesia. Propofol, droperidol, etomidate, and ketamine hydrochloride are commonly used to provide a total intravenous anesthetic (TIVA). IV anesthetics have a rapid onset and short duration of action. Table 18.5 describes the inhalation and IV anesthetics used for general anesthesia.
Midazolam and propofol are commonly administered for the induction and maintenance of anesthesia or for conscious sedation for minor surgery or procedures like intubation and mechanical ventilation. Patients are sedated and relaxed but, depending upon the dose, they are responsive to commands.
TABLE 18.4
| Stage | Name | Description |
| 1 | Analgesia | Begins with consciousness and ends with loss of consciousness; speech is difficult, sensations of smell and pain are lost, dreams and auditory and visual hallucinations may occur; this stage may be called the induction stage. |
| 2 | Excitement or delirium | Produces a loss of consciousness caused by depression of the cerebral cortex; confusion, excitement, or delirium occur, and induction time is short. |
| 3 | Surgical | Surgical procedure is performed during this stage. There are four phases: surgery is usually performed in phase 2 and upper phase 3. As anesthesia deepens, respirations become shallower, and the respiratory rate is increased. |
| 4 | Medullary paralysis | Toxic stage of anesthesia in which respirations are lost, and circulatory collapse occurs; ventilatory assistance is necessary. |
Adverse effects from IV anesthetics include respiratory and cardiovascular depression. Propofol supports microbial growth and may increase the risk for bacterial infection. Discarding opened vials within 6 hours is a necessary precaution in the prevention of sepsis.
Topical Anesthetics
Use of topical anesthetic agents is limited to mucous membranes, broken or unbroken skin surfaces, and burns. Topical anesthetics come in different forms: solutions, liquid sprays, ointments, creams, gels, and powders. Topical anesthetics decrease the sensitivity of nerve endings in the affected area.
Local Anesthetics
Local anesthetics block pain at the site where the drug is administered by preventing conduction of nerve impulses. Local anesthetics are useful in dental procedures, suturing skin lacerations, short-term (minor) surgery at a localized area, blocking nerve impulses (nerve block) below the insertion of a spinal anesthetic, and diagnostic procedures such as lumbar puncture and thoracentesis. Local anesthetics may also be used to perform regional blocks—such as brachial plexus, axillary, femoral, or sciatic blocks—to provide analgesia for surgery of the upper or lower extremities.
Most local anesthetics are divided into two groups, the esters and the amides, according to their basic structures. The amides have a very low incidence of allergic reaction.
The first local anesthetic used was cocaine hydrochloride in the late 1800s. Procaine hydrochloride, a synthetic of cocaine, was discovered in the early 1900s. Lidocaine hydrochloride was developed in the mid-1950s to replace procaine except in dental procedures. Lidocaine has a rapid onset and a long duration of action, is more stable in solution, and causes fewer hypersensitivity reactions than procaine. Since the introduction of lidocaine, many local anesthetics have been marketed. Table 18.6 describes the various types of local anesthetics according to short-, moderate-, and long-acting effects.
Orthopedic joint surgeries, mastectomy, cesarean delivery, hysterectomy, hernia repair, and cholecystectomy frequently use the postoperative pain control provided by an anesthetic pump. For example, the patient who has a bilateral hernia repair has a catheter inserted into the deep fascia of the lower abdomen. A continuous flow of bupivacaine, a local anesthetic, is delivered via a Y-connector to both sides. By controlling pain with this delivery method, the patient is allowed increased mobility; reduced opioid use, which reduces associated drowsiness and nausea; and a reduced hospital stay.
Spinal Anesthesia
Spinal anesthesia requires that a local anesthetic be injected into the subarachnoid space below the first lumbar space (L1) in adults and the third lumbar space (L3) in children. If the local anesthetic is given or spreads too high in the spinal column, the respiratory muscles could be affected, and respiratory distress or respiratory failure could result. A postdural-puncture headache might result following spinal anesthesia (a “spinal”), possibly because of a decrease in cerebrospinal fluid pressure caused by a leak of fluid at the needle insertion point. Encouraging the patient to remain flat following surgery with spinal anesthesia and to take increased fluids usually decreases the likelihood of leaking spinal fluid. Postdural-puncture headaches occur most frequently in females and in younger patients, and obstetric patients have the highest incidence. Hypotension also can result following spinal anesthesia due to the ensuing sympathetic blockade and predisposing factors that include sensory block location, history of hypertension, and chronic alcohol intake.
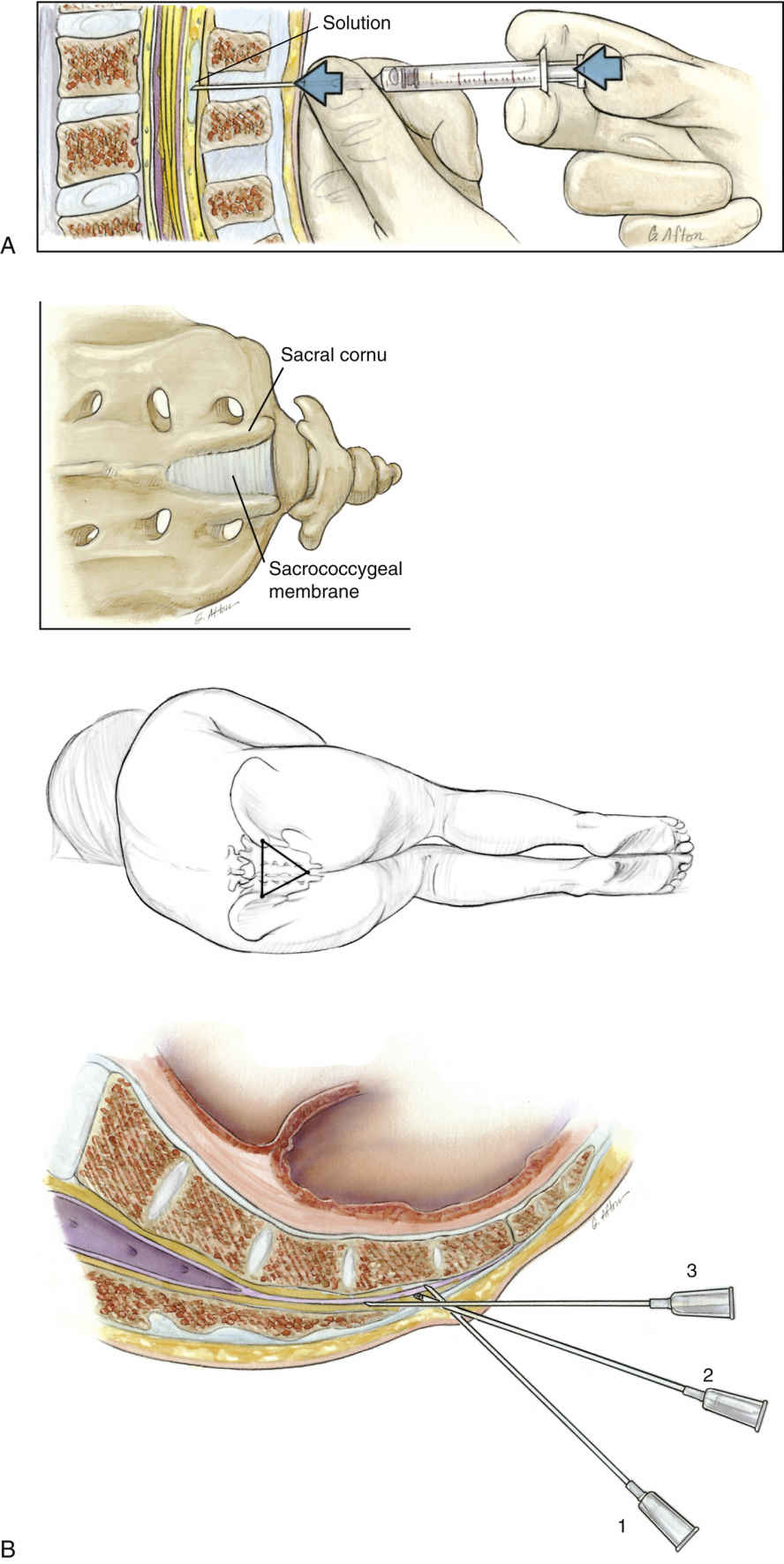
Various sites of the spinal column can be used for a nerve block with a local anesthetic (Fig. 18.2). A spinal block results from the penetration of the anesthetic into the subarachnoid space, which is the space between the pia mater membrane and the arachnoid membrane. An epidural block is the placement of the local anesthetic in the epidural space just posterior to the spinal cord or the dura mater. The epidural space is located between the posterior longitudinal ligament on the anterior side and the ligamentum flavum posteriorly. A caudal block is an epidural block placed by administering a local anesthetic through the sacral hiatus. A saddle block is given at the lower end of the spinal column to block the perineal area. Blood pressure should be monitored during administration of these types of anesthesia because a decrease in blood pressure resulting from the drug and procedure might occur. Further discussion of labor and delivery drugs can be found in Chapter 50.
Evaluation
• Evaluate the patient’s response to the anesthetics. Continue to monitor for adverse reactions.
Nurses play an important role in patient assessment before and after general and local anesthesia is administered. Preparing the patient for surgery by explaining the preparations and completing the preoperative orders, including premedications, is necessary to enhance the safety and effectiveness of anesthesia and surgery.
Critical Thinking Case Study
JZ, a 72-year-old woman, has difficulty staying asleep. She asks the nurse whether she should take a sleeping medication, such as lorazepam, before bedtime.
1. Before JZ takes any sleep aid or hypnotic, what nursing assessments should be made?
2. Describe a nursing plan that may help alleviate JZ’s sleep disturbance.
3. Would JZ be a candidate for taking a benzodiazepine? Explain your answer.
4. What follow-up plan should the nurse have related to JZ’s sleep problem?