Chapter 593 Demyelinating Disorders of the CNS
Demyelinating disorders of the central nervous system (CNS) cause acute or relapsing-remitting encephalopathy and other multifocal signs of brain, brainstem, and spinal cord dysfunction. They affect white matter, which is formed by myelin contained within oligodendrocytes, providing electrical insulation for neurons and neuronal connections. In contrast to genetically determined leukodystrophies (sometimes called dysmyelinating disorders) that also produce disrupted white matter, demyelinating disorders generally target normally formed white matter through immune-mediated mechanisms. Major demyelinating disorders in childhood include multiple sclerosis (MS) and acute disseminated encephalomyelitis (ADEM). The rare macrophage activating syndromes and isolated angiitis of the CNS can sometimes be confused with ADEM (Table 593-1).
Table 593-1 SUMMARY OF CONSENSUS DEFINITIONS FOR PEDIATRIC CENTRAL NERVOUS SYSTEM INFLAMMATORY DEMYELINATION
| MONOPHASIC CNS INFLAMMATORY DEMYELINATION | |
| ADEM | Clinical event must include encephalopathy (behavioral change and/or altered consciousness) |
| New symptoms or signs within 3 months are considered part of same ADEM event | |
| CIS | Clinical event that can be monofocal (e.g., isolated optic neuritis) or polyfocal, but cannot include encephalopathy |
| NMO | Must have optic neuritis and transverse myelitis as major criteria. Must have spinal MRI lesion extending over 3 or more segments or be NMO-IgG positive |
| RELAPSING CNS INFLAMMATORY DEMYELINATION | |
| Recurrent ADEM | New event of ADEM (must have encephalopathy) with recurrence of initial ADEM symptoms and signs 3 or more months after initial event and not related to withdrawal of steroids |
| Multiphasic ADEM | ADEM followed by new clinical event also meeting criteria for ADEM, but involving new CNS lesions (clinically and radiologically) |
| Relapsing NMO | Relapse of NMO as described above. Additional clinical and radiologic features extrinsic to optic nerve and spinal cord are well described and acceptable for diagnosis |
| Pediatric MS | Two or more events separated in time (4 or more weeks) and space. First episode cannot be ADEM. If 1st episode is ADEM, 2 or more non-ADEM events are required for diagnosis of MS. New MRI lesions 3 months or longer after the initial clinical event can be used to satisfy criteria for dissemination in time |
All events must include compatible MRI features of CNS inflammatory demyelination and exclude alternative causes.
ADEM, acute disseminated encephalomyelitis; CIS, clinically isolated syndrome; CNS, central nervous system; MS, multiple sclerosis; NMO, neuromyelitis optica.
(Data from Krupp LB, Banwell B, Tenembaum S: Consensus definitions proposed for pediatric multiple sclerosis and related disorders, Neurology 68[16 Suppl 2]:S7–S12, 2007.)
593.1 Multiple Sclerosis
Clinical Manifestations
Presenting symptoms in pediatric MS include hemiparesis or paraparesis, unilateral or bilateral optic neuritis, focal sensory loss, ataxia, diplopia, dysarthria, or bowel/bladder dysfunction (Table 593-2). Polyregional symptoms are reported in 30% of patients. Encephalopathy is less common and suggests consideration of acute disseminated encephalomyelitis (ADEM).
Table 593-2 SYMPTOMS AND SIGNS OF MULTIPLE SCLEROSIS BY SITE
| SYMPTOMS | SIGNS | |
|---|---|---|
| Cerebrum | Cognitive impairment | Deficits in attention, reasoning, and executive function (early); dementia (late) |
| Hemisensory and motor | Upper motor neuron signs | |
| Affective (mainly depression) | ||
| Epilepsy (rare) | ||
| Focal cortical deficits (rare) | ||
| Optic nerve | Unilateral painful loss of vision | Scotoma, reduced visual acuity, color vision, and relative afferent papillary defect |
| Cerebellum and cerebellar pathways | Tremor | Postural and action tremor, dysarthria |
| Clumsiness and poor balance | Limb incoordination and gait ataxia | |
| Brainstem | Diplopia, oscillopsia | Nystagmus, internuclear and other complex ophthalmoplegias |
| Vertigo | ||
| Impaired swallowing | Dysarthria | |
| Impaired speech and emotional lability | Pseudobulbar palsy | |
| Paroxysmal symptoms | ||
| Spinal cord | Weakness | Upper motor neuron signs |
| Stiffness and painful spasms | Spasticity | |
| Bladder dysfunction | ||
| Erectile impotence | ||
| Constipation | ||
| Other | Pain | |
| Fatigue | ||
| Temperature sensitivity and exercise intolerance |
Modified from Compston A, Coles A: Multiple sclerosis, Lancet 372:1502–1517, 2008, p 1503.
Laboratory Findings
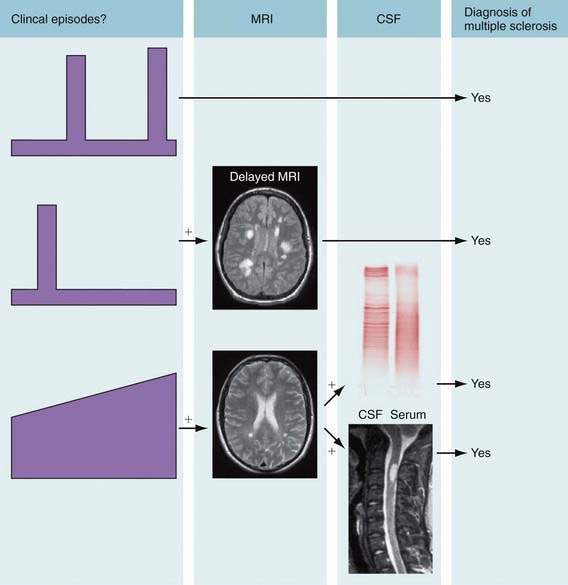
Cranial MRI exhibits discrete T2 lesions in cerebral white matter, particularly periventricular regions as well as brainstem, cerebellum, and juxtacortical and deep gray matter. Alternatively, tumefactive T2 lesions are also seen. Spine MRI typically shows partial-width cord lesions restricted to 1-2 spine segments. CSF may be normal or exhibit mild pleocytosis, particularly in younger children. Abnormal MS profiles (increased IgG index, and/or CSF oligoclonal bands) increase likelihood of MS but may be negative in 10-60% of pediatric MS patients, particularly prepubertal children (Fig. 593-1). Abnormal evoked potential studies can localize disruptions in visual, auditory, or somatosensory pathways.
Diagnosis and Differential Diagnosis
Like adult MS, pediatric MS can be diagnosed following 2 demyelinating episodes localizing to distinct CNS regions, lasting >24 hr and separated by >30 days, provided no other plausible explanation exists. Alternatively, accumulation of T2 or gadolinium-enhancing lesions in the brain or spine >3 mo later can demonstrate dissemination in time, enabling MS diagnosis after the 1st event. Challenges arise in distinguishing pediatric MS from other demyelinating syndromes such as acute disseminated encephalomyelitis (ADEM) or neuromyelitis optica (NMO), ADEM is a self-limited syndrome characterized by encephalopathy, polyregional neurologic deficits, and diffuse multifocal MRI T2 abnormalities followed by subsequent clinical improvement and resolution of MRI T2 lesions (see Tables 593-1 and 593-3). However, a subset of pediatric MS patients (10-25%) present with an ADEM phenotype and then experience multiple relapses with accumulation of MRI T2 lesions. NMO, traditionally a combined myelitis and optic neuritis with normal brain MRI, now has a broader phenotype with the recent identification of the NMO antibody against the CNS water channel aquaporin-4. The NMO spectrum now includes isolated bilateral ON or longitudinally extensive transverse myelitis even in the presence of brain MRI abnormalities or encephalopathy.
Table 593-3 CLINICAL AND MRI FEATURES THAT MAY DISTINGUISH ADEM FROM FIRST ATTACK OF MS
| ADEM | MS | |
|---|---|---|
| Age | <10 yr | >10 yr |
| Stupor/coma | + | − |
| Fever/vomiting | + | − |
| Family history | No | 20% |
| Sensory complaints | + | + |
| Optic neuritis | Bilateral | Unilateral |
| Manifestations | Polysymptomatic | Monosymptomatic |
| MRI imaging | Widespread lesions: basal ganglia, thalamus, cortical gray-white junction | Isolated lesions: periventricular white matter, corpus callosum |
| CSF | Pleocytosis (lymphocytosis) | Oligoclonal bands |
| Response to steroids | + | + |
| Follow-up | No new lesions | New lesions |
Some features that may help distinguish an initial acute episode of demyelination from a 1st attack of MS in children. Final diagnosis of MS is based on follow-up evaluation and possibly MRI.
ADEM, acute disseminated encephalomyelitis; CSF, cerebrospinal fluid; MS, multiple sclerosis; +, more likely to be present; –, less likely to be present.
Banwell B, Kennedy J, Sadovnick D, et al. Incidence of acquired demyelination of the CNS in Canadian children. Neurology. 2009;72:232-239.
Callen DJ, Shroff MM, Branson HM, et al. MRI in the diagnosis of pediatric multiple sclerosis. Neurology. 2009;72:961-967.
The CAMMS223 Trial Investigators. Alemtuzumab vs. interferon beta-1a in early multiple sclerosis. N Engl J Med. 2008;359:1786-1801.
Cohen JA, Barkhof F, Comi G, et al. Oral fingolimod or intramuscular interferon for relapsing multiple sclerosis. N Engl J Med. 2010;362:402-414.
Compston A, Coles A. Multiple sclerosis. Lancet. 2008;372:1502-1517.
Franklin RJM. Stem cell treatments and multiple sclerosis. BMJ. 2010;340:985-986.
Gajofatto A, Monaco S, Fiorini M, et al. Assessment of outcome predictors in first-episode acute myelitis. Arch Neurol. 2010;67(6):724-730.
Giovannoni G, Comi G, Cook S, et al. A placebo-controlled trial of oral cladribine for relapsing multiple sclerosis. N Engl J Med. 2010;362:416-426.
Goodman AD, Brown TR, Edwards KR, et al. A phase 3 trial of extended release oral dalfampridine in multiple sclerosis. Ann Neurol. 2010;68:494-502.
Kalluri SR, Illes Z, Srivastava R, et al. Quantification and functional characterization of antibodies to native aquaporin 4 in neuromyelitis optica. Arch Neurol. 2010;67(10):1201-1208.
Krupp LB, Banwell B, Tenembaum S, et al. Consensus definitions proposed for pediatric multiple sclerosis and related disorders. Neurology. 2007;68:S7-S12.
Linda H, von Heijne A, Major EO, et al. Progressive multifocal leukoencephalopathy after natalizumab monotherapy. N Engl J Med. 2009;361:1081-1087.
The Medical Letter. Interferon beta-lb (extavia) for multiple sclerosis. Med Lett. 2010;52:86-87.
The Medical Letter. Oral fingolimod (gilenya) for multiple sclerosis. Med Lett. 2010;52:98-100.
Pohl D, Waubant E, Banwell B, et al. Treatment of pediatric multiple sclerosis and variants. Neurology. 2007;68:S54-S65.
Thompson A, Polman C. Improving function: a new treatment era for multiple sclerosis? Lancet. 2009;373:697-698.
Weng WC, Yang CC, Yu TW, et al. Multiple sclerosis with childhood onset: report of 21 cases in Taiwan. Pediatr Neurol. 2006;35:327-334.
Venkateswaran S, Banwell B. Pediatric multiple sclerosis. Neurologist. 2010;16:92-105.
Yeh EA, Chitnis T, Krupp L, et al. US Network of Pediatric Multiple Sclerosis Centers of Excellence. Pediatric multiple sclerosis. Nat Rev Neurol. 2009;5:621-631.
593.2 Neuromyelitis Optica
Diagnosis and Differential Diagnosis
Clinical criteria for the diagnosis of NMO include finding at least 2 of the following: normal brain MRI, spinal cord widening and cavitation involving at least 3 spinal segments, decreased serum/CSF albumin ratio with normal IgG synthesis rate and the absence of oligoclonal bands, and acute episode(s) of spinal cord and/or optic nerve involvement separated by months or years without any other systemic or neurologic features. The differential diagnosis includes MS; ADEM (Chapter 593.3); rheumatologic etiologies of transverse myelitis and/or optic neuritis including systemic lupus erythematosus, Behçet disease, and neurosarcoidosis (usually accompanied by other nonneurologic manifestations); idiopathic transverse myelitis, tropical spastic paraparesis, and viral encephalomyelitis (none of which have NMO antibodies in the serum or CSF); and metabolic and idiopathic causes of isolated optic neuritis or other acute monocular or binocular visual loss (Chapter 623).
593.3 Acute Disseminated Encephalomyelitis (ADEM)
Neuroimaging
Head CT may be normal or show hypodense regions. Cranial MRI, the imaging study of choice, typically exhibits large, multifocal and sometimes confluent or tumefactive T2 lesions with variable enhancement within white and often gray matter of the cerebral hemispheres, cerebellum, and brainstem (Fig. 593-2). Deep gray matter structures (thalami, basal ganglia) are often involved although this may not be specific to ADEM. Spinal cord may have abnormal T2 signal or enhancement, with or without clinical signs of myelitis. MRI lesions of ADEM typically appear to be of similar age but their evolution may lag behind the clinical presentation. Serial MRI imaging 3-12 mo following ADEM shows improvement and often complete resolution of T2 abnormalities although residual gliosis may remain.
Differential Diagnosis
The differential diagnosis for ADEM is broad but can be narrowed by careful history, appropriate laboratory evaluations, and MRI. Empirical antibiotic and antiviral treatment should be considered while infectious evaluations are pending. Follow-up MRI examinations 3-12 mo after ADEM should show improvement; new or enlarging T2 lesions should prompt re-evaluation for other etiologies such as MS, leukodystrophies, tumor, vasculitis, or mitochondrial, metabolic, or rheumatologic disorders (see Table 593-3).
Dale RC, Brilot F, Banwell B. Pediatric central nervous system inflammatory demyelination: acute disseminated encephalomyelitis, clinically isolated syndromes, neuromyelitis optica, and multiple sclerosis. Curr Opin Neurol. 2009;22:233-240.
Huynh W, Cordato DJ, Kehdi E, et al. Post-vaccination encephalomyelitis: literature review and illustrative case. J Clin Neurosci. 2008;15:1315-1322.
Tenembaum S, Chitnis T, Ness J, et al. Acute disseminated encephalomyelitis. Neurology. 2007;68:S23-S36.
Yiu EM, Kornberg AJ, Ryan MM, et al. Acute transverse myelitis and acute disseminated encephalomyelitis in childhood: spectrum or separate entities? J Child Neurol. 2009;24:287-296.