Chapter 85 Degenerative Rotatory Scoliosis
Three- Dimensional Thoracic and Lumbar Spine Deformity Correction
Degenerative scoliosis is the most common cause of adult scoliosis.1 It develops de novo during adulthood and is largely due to asymmetrical disc degeneration; the resultant curve has even been referred to as a “discogenic curve.”1 Additionally, it may be related to osteoporosis and associated compression fractures. The apex of this curve is most often present at L2-3 or L3-4 and is usually limited to the lumbar or thoracolumbar regions. Its extent, as illustrated by imaging studies, does not necessarily correlate with symptoms or neurologic deficits, a fact that presents a significant dilemma to the treating physician. Management options are complicated by the wide variety of treatment choices.
Pathophysiology of Disc Degeneration and the Spondylotic Process
Lumbar spondylosis is not a pathologic process; it is but a manifestation of the wear and tear associated with aging, specifically the consequences of loading. It is defined as vertebral osteophytosis secondary to degenerative disc disease2 and is not an inflammatory process. Noninfectious inflammatory processes are grouped together as arthritides and are excluded from this discussion.
Spondylosis and associated osteophytosis are universally accompanied by degeneration of the intervertebral disc. The intervertebral disc is an amphiarthrodial joint (no synovial membrane) with particular traits that result in a characteristic degeneration pattern. Conversely, arthritides classically involve the synovial membranes of diarthrodial joints (joints lined with synovium and lubricated with synovial fluid, such as facet joints). Facet joints, however, are also affected by the spondylotic process.3,4
The degenerative process primarily involves the disc interspace and alters intradiscal dynamics that result in spine deformation. The resultant excessive motion and stresses cause extradiscal soft tissue proliferation. Finally, spine deformation predisposes to further deformation (see the section titled “Osteoporosis”). Osteoporosis contributes to the latter process, with a resultant asymmetrical vertebral body collapse.
Intradiscal Dynamics
The water content of the disc interspace gradually decreases throughout life, which contributes to alterations in the chemical and anatomic makeup of the disc. Fibroblasts become defective, and the desiccated disc is less effective as a cushion. Fissures then develop in the cartilaginous end plates. Schmorl nodes are manifestations of this pathologic process. Gas may accumulate in the disc (the vacuum phenomenon). An ingrowth of fibrocartilage (mucoid degeneration) with obliteration of the nucleus fibrosus ensues. Relative incompetence of the disc itself and relative instability result, and anulus fibrosus bulging and tension occur as a result of this process.3
Disc Deformation
Form follows function, even during the process of degeneration. Therefore, osteophyte formation occurs predominantly on the concave side of a scoliotic curvature (where anulus fibrosus bulging is most significant), while disc herniation occurs commonly on the convex side of a spinal bend. The thin dorsal anulus fibrosus and relatively weak lateral aspect of the posterior longitudinal ligament combine with the migratory tendencies of the nucleus pulposus to encourage dorsolateral disc herniation.3
In the laboratory, (1) flexion (causing dorsal nucleus pulposus migration), (2) lateral bending away from the side of disc herniation (causing lateral nucleus pulposus migration), and (3) application of an axial load (causing an increase in intradiscal pressure) are required for the creation of a herniated lumbar disc. A degenerated disc is also necessary as a predisposing factor.5 This complex loading pattern results in the application of tension on the weakest portion of the anulus fibrosus (the dorsolateral position, the location of the herniation), migration of the nucleus pulposus toward this position, and an asymmetrical increase in intradiscal pressure. The age-related increased frequency of anulus fibrosus tears and a peaking of nucleus fibrosus pressures in people 35 to 55 years of age4 also predispose to an increased incidence of disc herniation. Asymmetrical collapse of the disc interspace is often a result of the disc degeneration process and places asymmetrical focal stresses on portions of the spine.
Spinal Configuration
The coupling phenomenon (whereby one movement of the spine about or along an axis obligates another movement about or along another axis)3 plays a significant role in the development of degenerative spine deformations in the lumbar region (whereas it is of minimal significance regarding degenerative deformities in the thoracic region). This is because thoracic degenerative deformities are often oriented in the sagittal plane, whereas degenerative lumbar deformities are usually oriented in the coronal plane (excluding degenerative lumbar spondylolisthesis). The absence of uncovertebral joints (in contrast to the cervical region) and the sagittal orientation of the facet joints (in contrast to the cervical and thoracic regions) create a situation that causes obligatory rotation of the spine in response to lateral bending (coupling) and, commonly, a loss of normal lumbar lordosis. The progression of lateral bending deformities in the lumbar spine (scoliosis) thus predisposes to rotation of the spine (Fig. 85-1), and the influence of an uncompensated thoracic kyphosis predisposes the lumbar spine to greater “flattening” or loss of the normal lordotic curve.
Not all scoliotic curves are symptomatic, as patients may be able to compensate for these deformities by “rebalancing” the spine through other skeletal structures, such as pelvic tilt. When curve progression can no longer be compensated, the subsequent displacement of the load causes worsening of curve that caused it in the first place. Therefore, lateral bending deformation predisposes to lateral bending deformity progression in the lumbar spine, as the presence of kyphotic deformation predisposes to the progression of kyphotic deformation in the thoracic spine. An asymmetrical loss of height of the lumbar intervertebral disc may progress to an asymmetrical collapse of the vertebral body, as described previously in this chapter. As this scoliotic deformity progresses, it is obligatorily associated with rotation of the spine, with the spinous processes rotating toward the concave side of the curve (coupling).3 Of note is that because of the aforementioned osteophyte development propensities, osteophytes occur predominantly on the concave side of the curvature.
Operative Treatment
The operative treatment of scoliosis is reserved for patients with refractory pain due to the scoliosis curve, significant curve progression, gait disturbance, and neurologic deficit all leading to a significant limitation of activities of daily living.6,7 Preoperative preparation should include adequate imaging, as was already mentioned.
Any patient being considered for surgery not should only get detailed radiographic spine imaging but may also need a variety of complementary studies. A dual-energy x-ray absorptiometry scan can provide useful information about bone quality that may affect surgical planning. Patients with suspected pulmonary compromise should be sent for pulmonary function testing, although pulmonary compromise is rare in patients with curves less than 80 degrees.8 Medical and cardiac risk stratification should be obtained for anyone with a significant medical history. It should be noted that occult cardiac disease can be seen in adult scoliotic patients owing to severe deconditioning and the patient’s inability to experience exercise-related stress. Smoking cessation should be pursued, and a general rule of thumb is that elective surgery for deformity correction be offered to patients only after they have quit smoking.
The current approach to the surgical treatment of scoliosis is primarily pedicle screw and rod instrumentation. A recent report comparing hook-rod constructs and pedicle screw-rod constructs found that no pedicle screw patient required revision surgery for instrumentation-related complications and, overall, pedicle screw patients were 89% less likely to require revision surgery.9 These patients were also found to have better curve correction and maintenance of thoracic kyphosis, and pedicle screw-rod constructs often negated the need for ventral release surgery.10 However, hooks remain a valuable alternative when pedicle screws are contraindicated.
Goals of surgical correction of scoliosis are correction of coronal and sagittal balance to decrease pain, to decompress the neurologic elements, to correct balance so as to improve function, and to provide cosmesis.11
Deformity Correction
A variety of techniques can be used to correct lumbar spine deformities. Deformity correction is accomplished via the application of rotatory or translational forces to the spine along one or a combination of the three axes of the Cartesian coordinate system.3 It is tempting to use distraction to reduce compression and translational deformations, but this maneuver in the lumbar spine invariably introduces a kyphotic force that can be very injurious to the patient’s sagittal balance. Compression is preferable because of its favorable effects on sagittal contour, and is especially useful when combined with interbody devices. Similarly, three- or four-point bending forces can be applied. Finally, bending moments can be applied in either the coronal or sagittal plane to correct spinal curvatures. Complex bending moment forces are often applied.
Distraction and Compression
Distraction force application on the concave side of the curve and compression force application on the convex side of the curve can be used to correct coronal plane deformities. This force couple3 applies a coronal plane bending moment.
Three- and Four-Point Bending Fixation
Three- and four-point bending of the spine, as defined by White and Panjabi,12 involves the loading of a long structure (i.e., the spine) with one or two transverse forces on one side and two on the other.12 In a four-point bending construct, the bending moment is constant between the two intermediate points of force application if all forces are equal. In a three-point bending construct, the bending moment peaks at the intermediate point of force application.
The crossed-rod technique is a complex variant of three- or four-point bending fixation. It is a traditional and common method of thoracic and lumbar kyphotic deformity correction and was first used with Harrington distraction rods. Subsequently, it involved the Luque multisegmental sublaminar wiring technique.13 Most recently, it has been employed with sequential pedicle screw fixation with universal spinal instrumentation constructs.14 Regardless of the specific method used, the crossed-rod technique involves sequential and gradual application of kyphosis reduction forces to the spine via moment arms through longitudinal members.
Applied Moment Arm Cantilever Beam Force Application
Applied moment arm cantilever beam constructs are most appropriate in situations in which short-segment constructs are particularly desirable.3 This type of construct mandates that a significant force be applied by the implant to the spine. Although this type of construct is most often applied for sagittal plane deformities, it can also be used (although uncommonly) for coronal plane deformity correction.
These are constructs that are frequently applied as either flexion or extension bending moments via pedicle screws.15 They can be used with distraction, compression, or coronal plane bending moment force application and can also be applied with an accompanying ventral dural sac decompression and interbody bone graft placement. Furthermore, they can be applied so that deformity is reduced and compression of the bone graft is achieved. This technique of (1) sequential application of distraction (load bearing), (2) decompression of the dural sac, (3) interbody fusion placement, and (4) compression of the construct to share the load with the ventral spinal elements is termed load-bearing to load-sharing force application. It provides biomechanical advantages (load sharing) as well as clinical advantages.3
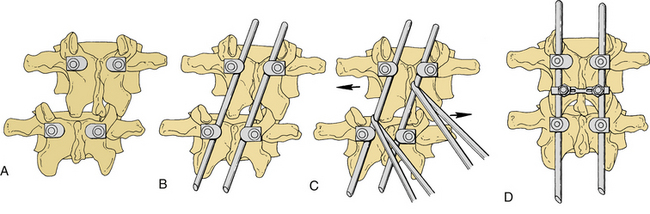
Short-Segment Parallelogram Deformity Reduction
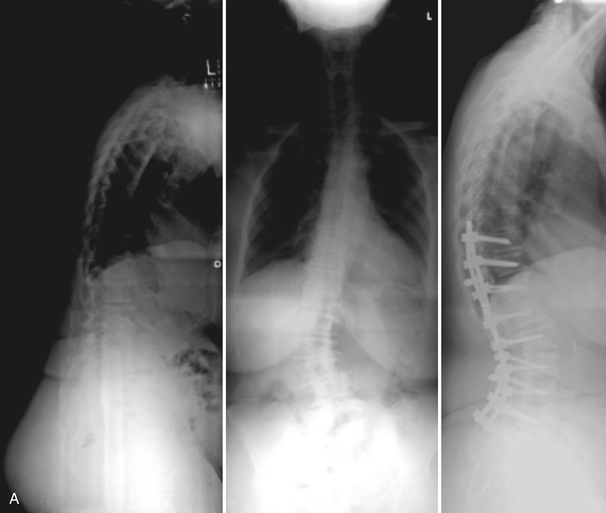
Short-segment parallelogram deformity reduction is a rigid cantilever beam pedicle fixation technique that applies bending moments for the reduction of lateral translational deformations.3 This technique is most useful when short-segment fixation is deemed optimal. It involves (1) placement of pedicle screws, (2) appropriate dural sac decompression, (3) attachment of the longitudinal members to the screws (rods), (4) application of a rotatory and distraction force to the rods, (5) maintenance of the achieved spine reduction via rigid cross-fixation, (6) placement of a fusion (interbody and/or lateral), and, finally, (7) compression of the screws so that load sharing is achieved and the interbody bone graft is secured in its acceptance bed.3 It applies load-bearing to load-sharing forces (Fig. 85-2).
In Vivo Implant Contouring
Segmental relationships can be altered by rod contouring. Employment of in vivo implant contouring for segmental relationship alteration is an effective method of deformity reduction. A multisegmental fixation system can be inserted in such a manner that it conforms to a spine deformity, such as scoliosis. After insertion, rod contouring can be used to “straighten” the spine. Adequate implant-bone juncture security is mandatory. Implant contouring alters the forces applied by the implant to the spine at each segmental level. Typically, this method is used to fine-tune a scoliotic repair to correct for several important hazards. Hooks can overtighten or loosen, infringe on the spinal canal, or migrate laterally or medially.3 The screw-bone interface is also exposed to significant forces and may loosen. Additionally, the application of significant force through bulky in situ rod benders in close proximity to the spinal canal risks direct trauma to the spinal cord or cauda equina.
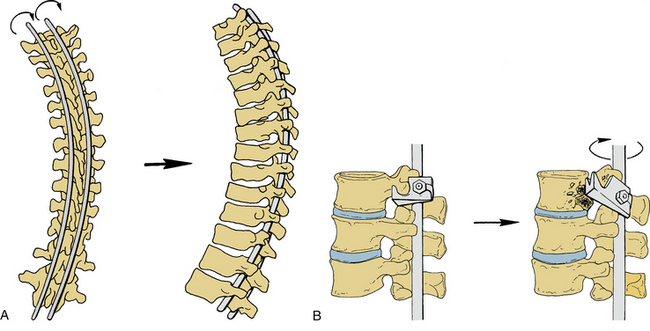
Intrinsic Implant Bending Moment Application about the Long Axis of the Spine: The Derotation Maneuver
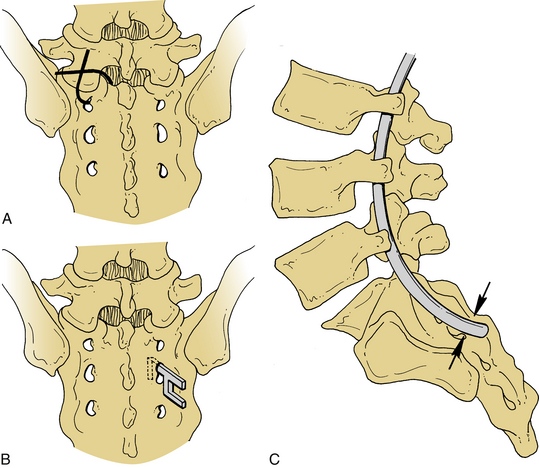
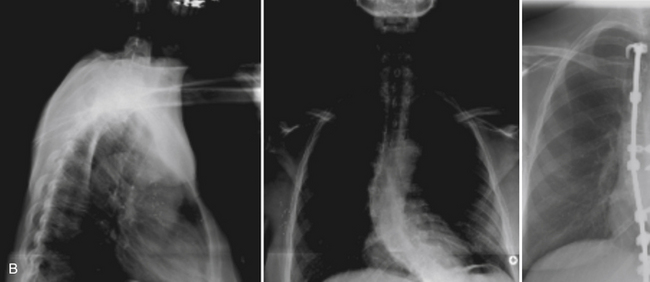
An obligatory rotatory component coexists with scoliotic deformities (coupling). This phenomenon can be used to an advantage by applying the spine derotation maneuver. Spinal derotation involves conversion of a scoliotic curvature to a kyphotic curvature.16 The resultant kyphotic curvature can be reduced, if appropriate, via rod contouring. The derotation maneuver is accomplished by first inserting the rods via hooks, screws, or wires, which are relatively loosely attached to the rod (with friction-glide tightness), so that rotation of the rod can occur at its juncture with the hooks, screws, or wires. The attachment should not be so tight as to allow dislodgement (friction-glide tight or “just right tight” is preferable). This allows the hooks, screws, or wires to maintain their relationship with the spinal attachment site. The rods are then simultaneously rotated 90 degrees, which converts a scoliotic deformity to a kyphotic deformity. The rods can be contoured to eliminate an excessive kyphotic curvature. The junctures are then tightened and secured, and cross-fixation is employed to maintain the reduction (Fig. 85-3A).
These maneuvers should be used in a gradual manner so that continuous assessment and reassessment of the implant-spine relationships can be made. For example, a hook might not rotate on the rod during the derotation maneuver, thus placing significant stress on the hook-bone attachment (Fig. 85-3B).
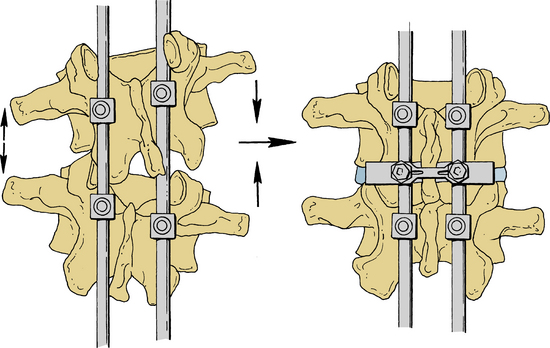
Intrinsic Implant Bending Moment Application about the Axial Axes of the Spine
Intrinsic implant bending moment can be applied in either the sagittal or the coronal plane. One- or two-segment lumbar scoliotic deformations can be partially or completely corrected by this technique. In applying this procedure, pedicle screws are inserted, and the rods are attached to the screws. The screws on the concave side of the curvature are then distracted (usually 1–2 cm), whereas the screws on the convex side of the curvature are compressed. Cross-fixation to maintain the correction is then used (Fig. 85-4). A similar technique can be employed to correct sagittal plane deformities by using rod or plate-screw systems on the lateral aspect of the spine.
Ventral Interbody Correction
A relatively new form of surgical management of lumbar scoliotic deformities involves the placement of ventral-lateral interbody cages.17 Because these devices result in the distraction of the ventral half of the disc space, they also provide some increase in lumbar lordosis. Although technically easier to place from the spinal convexity, these devices can be placed so as to distract the concavity and therefore reduce the scoliotic curve. When combined with dorsal decompression and instrumentation, these devices theoretically reduce the strain on the dorsal implant in maintaining correction. Anatomic features of the lateral lumbar spine limit application of these devices to the upper lumbar segments—a convenience, since the apex of these deformities is often in this spinal region. Various protocols have been reported, including stand-alone interbody devices used for this purpose, but long-term results are still lacking.
Maintenance of Correction
Implant Selection and Cross-Fixation
In an effort to allow greater flexibility in construct design and rigidity, several new metallic hybrid rods have recently been used to correct deformities. Cobalt-chrome alloys, for example, are biomechanically superior to titanium rods in maintaining sagittal and coronal correction, produce less imaging artifact than stainless steel rods, and can be used with titanium screws.18 Recent improvements in pedicle screws include varied thread designs that resist pull-out and hydroxyapatite coating, which improves fixation in osteoporotic bone.
Cross-fixation is the connection of bilaterally placed constructs to each other and can result in a substantial increase in the integrity of the construct. In general, cross-fixation of short constructs is of no significant benefit. However, in selected cases, it can be used to maintain deformity reduction and help prevent implant failure. In such situations, very rigid cross-members should be used because substantial bending moments are applied (resisted) at the cross-member-rod juncture.
With longer constructs, cross-fixation provides a quadrilateral, framelike construct. This is especially valuable when screws are angled in a nonparallel fashion in both the sagittal and coronal planes. By essentially binding the screws both longitudinally and cross-sectionally, rotatory stability and implant-bone juncture integrity are augmented. With long constructs, two cross-members are better than one; however, more than two add very little to construct integrity.3 Cross-members should be placed approximately at the junction of the thirds of the length of the construct.3
Screw Toe-In
By toeing-in pedicle screws, one can increase the length of a pedicle screw and provide much greater resistance to implant failure. Screw toe-in can also play an important role in lateral translational deformity prevention. It can be used with cross-fixation to achieve maintenance of deformity reduction.3
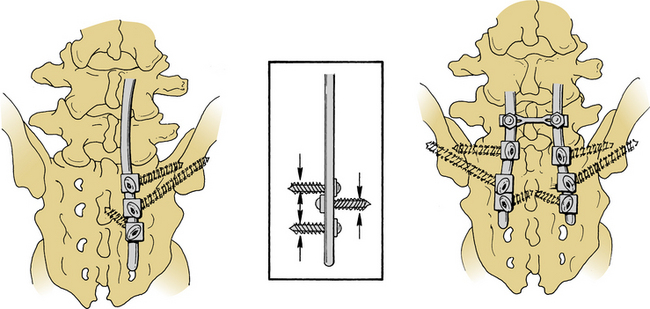
Low Lumbar and Lumbosacropelvic Techniques
The distal end of a spinal implant used to reduce an adult deformity has several significant implications. Ending the construct at L5 will certainly result in accelerated degenerative changes at that level. Since many adult deformities have an apex within the lumbar spine, instrumentation and fusion of the lumbosacral junction are common. L5-S1 interbody grafts and ilial-pelvic fixation (iliac screws) have been used as supplemental surgical techniques to combat high L5-S1 pseudarthrosis rates and the poor anatomic configuration of the S1 pedicles for screw fixation. Interbody grafts at the lumbosacral junction whether placed via anterior lumbar interbody fusion or transforaminal lumbar interbody fusion provide circumferential fusion, can help restore disc space and neuroforaminal height, and provide axial loading capacity. If interbody fusion is not used, acquisition of lumbosacral spine stability will indeed be complex and difficult. Surgical alternatives include pedicle fixation with orientation of the S1 screws upward toward the sacral promontory and complex iliac fixation techniques. It should be noted that pedicle fixation in the absence of adequate axial load-supporting capacity places excessive stresses on the implant and the implant-bone juncture. Repetitive loading of such a construct may produce failure at the screw-bone interface or the screw-plate or screw-rod juncture.3
Nonrigid lumbosacroiliac techniques, such as the slingshot and Galveston techniques, are cumbersome and involve fixation to predominantly low-density medullary bone. Thus, they may provide inadequate fixation. Prevention of lumbosacral fixation and extension therefore may be inadequate because of poor implant-bone juncture integrity (as was mentioned previously) and because of an inability to apply an adequate moment arm.19 Furthermore, the ability of these techniques to effectively reduce coronal plane deformities is poor because of their rigid one-piece design.
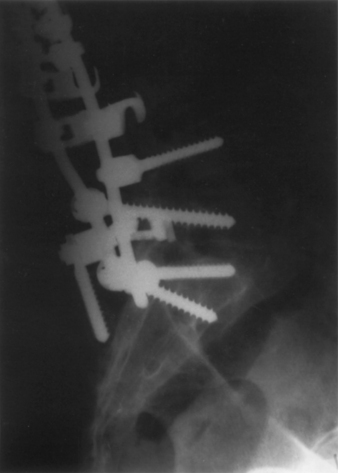
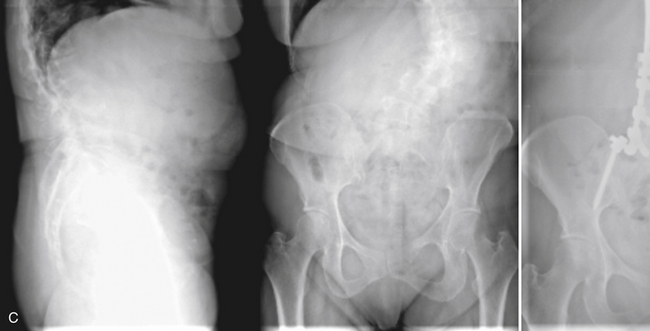
More rigid iliac screw fixation techniques using bicortical ilial fixation are a more acceptable alternative and are readily available in universal instrumentation systems.20 They allow the surgeon to use a tripod-like implant geometry for buttressing the sacroiliac segment (Fig. 85-5) and are especially helpful in preventing pull-out of the caudal end of an implant.3,20 This is particularly important following significant correction of sagittal balance or to counter the long moment arms associated with implants that extend cranially beyond the thoracolumbar junction.
A ventromedial orientation of sacral screws is, in general, superior to a ventrolateral (alar) orientation. Greater bone density and, hence, provision of a stronger implant-bone juncture can be achieved in the region of the midline sacral promontory or the L5-S1 disc interspace.3,21 Additional implant-sacrum junctures can be used to prevent lumbosacral flexion and extension, including the first sacral lamina (for sublaminar wire fixation), the second dorsal sacral neuroforamina (for hook fixation), and the dorsum of the sacrum itself (via a buttressing effect) (Fig. 85-6).
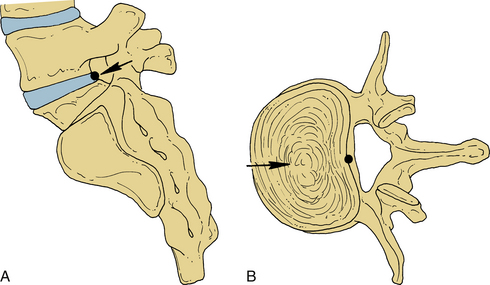
Lumbosacroiliac fixation techniques should be used with the lumbosacral pivot point in mind. This is defined as the point of intersection of the middle osteoligamentous column (a region of the posterior longitudinal ligament) in the sagittal plane and the L5-S1 intervertebral disc (Fig. 85-7). Constructs that employ lumbosacroiliac fixation via bone screws are most effective in resisting flexion and extension deformation if the ventral extent of the screws extends ventrally to this point (Fig. 85-8).22
Clinical Applications
Even when reduction and fusion are indicated, the universal application of a single surgical technique to all clinical situations is imprudent. For example, although pedicle fixation is, in general, a useful and efficacious technique, its universal application is inappropriate. For instance, it should not be applied over an unstable segment if ventral axial load-supporting ability is inadequate. Longer techniques or the use of ilial fixation augmentation may be beneficial (Fig. 85-9).
It is also important to remember that the major determinant of clinical success in adult patients undergoing deformity correction is the resultant sagittal contour, as discussed elsewhere.23,24 Therefore, whatever technique is used to correct a scoliotic deformity, consideration must be given to the effects on global balance. For example, distraction in the lumbar spine along the concavity of the scoliotic curve introduces a potentially deleterious kyphotic force that may result in a painful hypolordosis or a relatively “flat back.”
Similarly, several options are available to correct scoliotic deformities. These include distraction, short-segment parallelogram deformity reduction techniques (see Fig. 85-2), the derotation maneuver (see Fig. 85-3), and intrinsic implant bending moment application (see Fig. 85-4). Each procedure is indicated in specific circumstances; however, these indications are currently poorly defined.
Adams M.A., Huton W.C. Prolapsed intervertebral disc: a hyperflexion injury. Spine (Phila Pa 1976). 1982;7:184-191.
Cotrel Y., Dubousset J., Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988;227:10-23.
Heary R.F., Kumar S., Bono C.M. Decision making in adult deformity. Neurosurgery. 2008;63(3):A69-A77.
McCord D.H., Cunningham B.W., Shono Y., et al. Biomechanical analysis of lumbosacral fixation. Spine (Phila Pa 1976). 1992;17:5235-8243.
Rose P.S., Lenke L.G., Bridwell K.H., et al. Pedicle screw instrumentation for adult idiopathic scoliosis. Spine (Phila Pa 1976). 2009;34(8):852-857.
White A.A., Panjabi M.M. Clinical biomechanics of the spine, ed 2. Philadelphia: JB Lippincott; 1990.
1. Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925-948.
2. Weinstein P.R., Ehni G., Wilson C.B. Lumbar spondylosis: diagnosis, management and surgical treatment. Chicago: Year Book Medical; 1977.
3. Benzel E.C., editor. Biomechanics of spine stabilization: principles and clinical practice. New York: McGraw-Hill. 1995:101-278.
4. Kramer J. Intervertebral disc disease: causes, diagnosis, treatment, and prophylaxis, ed 2. New York: Thieme; 1990.
5. Adams M.A., Huton W.C. Prolapsed intervertebral disc: a hyperflexion injury. Spine (Phila Pa 1976). 1982;7:184-191.
6. Everett C.R., Patel R.K. A systematic literature review of nonsurgical treatment in adult scoliosis. Spine (Phila Pa 1976). 2007;32(19S):S130-S134.
7. Heary R.F., Kumar S., Bono C.M. Decision making in adult deformity. Neurosurgery. 2008;63(3):A69-A77.
8. Birknes J.K., White A.P., Albert T.J., et al. Adult degenerative scoliosis: a review. Neurosurgery. 2008;63(3):A94-A103.
9. Rose P.S., Lenke L.G., Bridwell K.H., et al. Pedicle screw instrumentation for adult idiopathic scoliosis. Spine (Phila Pa 1976). 2009;34(8):852-857.
10. Carreon L.Y., Puno R.M., Dimar J.R., et al. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg [Am]. 2003;85(11):2089-2092.
11. Glassman S.D., Hamill C.L., Bridwell K.H., et al. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976). 2007;32(24):2764-2770.
12. White A.A., Panjabi M.M. Clinical biomechanics of the spine, ed 2. Philadelphia: JB Lippincott; 1990.
13. Benzel E.C. Luque rod segmental spinal instrumentation. Rengachary S.S., Wilkins R.H., editors. Neurosurgical operative atlas, Park Ridge, IL, American Association of Neurological Surgeons. 1992:433-438.
14. Benzel E.C., Ball P.A., Baldwin N.G., Marchand E.P. The sequential hook insertion technique for universal spinal instrumentation application. J Neurosurg. 1993;79:608-611.
15. Dick W. The “fixateur interne” as a versatile implant for spine surgery. Spine (Phila Pa 1976). 1987;12:882-900.
16. Cotrel Y., Dubousset J., Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988;227:10-23.
17. Isaacs R.E., Hyde J., Goodrich J.A., et al. A prospective, nonrandomized, multicenter evaluation of extreme lateral interbody fusion for the treatment of adult degenerative scoliosis: perioperative outcomes and complications. Spine (Phila Pa 1976). 2010;35(Suppl 26):S322-S330.
18. Nguyen T.Q., Buckley J.M., Ames C., Deviren V. The fatigue life of contoured cobalt chrome posterior spinal fusion rods. Proc Inst Mech Eng [H]. 2011;225(2):194-198.
19. Kasten M.D., Rao L.A., Priest B. Long-term results of iliac wing fixation below extensive fusions in ambulatory adult patients with spinal disorders. J Spinal Disord Tech. 2010;23(7):e37-e42.
20. Baldwin N.G., Benzel E.C. Sacral fixation using iliac instrumentation and a variable-angle screw device. J Neurosurg. 1994;81:313-316.
21. Carlson G.D., Abitbol J.J., Anderson D.R., et al. Screw fixation in the human sacrum. Spine (Phila Pa 1976). 1992;17:5196-5203.
22. McCord D.H., Cunningham B.W., Shono Y., et al. Biomechanical analysis of lumbosacral fixation. Spine (Phila Pa 1976). 1992;17:5235-8243.
23. Schwab F., Lafage V., Farcy J.P., et al. Surgical rates and operative outcome analysis in thoracolumbar and lumbar major adult scoliosis. Spine (Phila Pa 1976). 2007;32(24):2723-2730.
24. Schwab F., Patel A., Ungar B., et al. Adult spinal deformity—postoperative standing imbalance. How much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010;35(25):2224-2231.