Chapter 50
Deep Vein Thrombosis
1. What three primary factors promote venous thromboembolic (VTE) disease?
Development of venous thrombosis is promoted by the following (the Virchow Triad):
2. List the risk factors for thromboembolic disease.
The numerous risk factors for thromboembolic disease include surgery, trauma, immobility, cancer, pregnancy, prolonged immobilization, estrogen-containing oral contraceptives or hormone replacement therapy, and acute medical illnesses. A more complete listing of these risk factors is given in Box 50-1.
3. What is the natural history of venous thrombosis?
Resolution of fresh thrombi occurs by endogenous fibrinolysis and organization. Fibrinolysis results in actual clot dissolution. Organization reestablishes venous blood flow by restoring endothelial cells and incorporating into the venous wall residual clot not dissolved by fibrinolysis. Incomplete recanalization can cause postphlebitic syndrome in >20% of patients.
4. Can patients with deep vein thrombosis (DVT) be accurately diagnosed clinically?
5. Where is the most common origin for thrombi that result in pulmonary emboli?
Thromboses in the deep veins of the lower extremities (Fig. 50-1) account for 90% to 95% of pulmonary emboli. Less common sites of origin include thromboses in the right ventricle, in upper extremity, prostatic, uterine, and renal veins; and, rarely, in superficial veins.
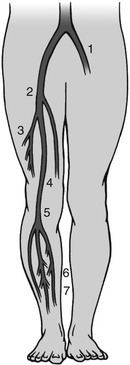
Figure 50-1 Common sites of deep venous thrombosis (DVT) in the lower body. 1, Left iliac vein; 2, common femoral vein; 3, termination of deep femoral vein (profunda femoris); 4, femoral vein; 5, popliteal vein at adductor canal; 6, posterior tibial vein; 7, intramuscular veins of calf. (From Pfenninger JL, Fowler GC: Pfenninger and Fowler’s procedures for primary care, ed 3, Philadelphia, 2010, Saunders.)
6. How is the diagnosis of lower extremity DVT confirmed?
Contrast venography is no longer appropriate as the initial diagnostic test in patients exhibiting DVT symptoms, although it remains the gold standard for confirmatory diagnosis of DVT. It is nearly 100% sensitive and specific and provides the ability to investigate the distal and proximal venous system for thrombosis. Venography is still warranted when noninvasive testing is inconclusive or impossible to perform, but its use is no longer widespread because of the need for administration of a contrast medium and the increased availability of noninvasive diagnostic strategies.
Ultrasound is safe and noninvasive and has a higher specificity than impedance plethysmography for the evaluation of suspected DVT. With color flow Doppler and compression ultrasound, DVT is diagnosed based on the inability to compress the common femoral and popliteal veins (Fig. 50-2). In patients with lower extremity symptoms, the sensitivity is 95% and specificity 96%. The diagnostic accuracy of ultrasound in asymptomatic patients, those with recurrent DVT, or those with isolated calf DVT is less reliable. The sensitivity of ultrasound improves with serial testing in untreated patients. Repeat testing at 5 to 7 days will identify another 2% of patients with clots not apparent on the first ultrasound. Serial testing can be particularly valuable in ruling out proximal extension of a possible calf DVT. Because the accuracy of ultrasound in diagnosing calf DVT is acknowledged to be lower (81% for DVT below the knee versus 99% for proximal DVT), follow-up ultrasounds at 5 to 7 days are reasonable because most calf DVTs that extend proximally will do so within days of the initial presentation.
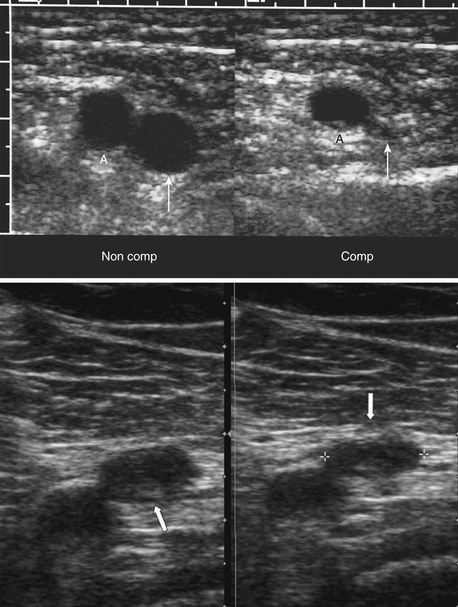
Figure 50-2 Normal and abnormal compression of the femoral vein with ultrasound examination. Top Images: Transverse image of the femoral artery (A) and vein (thin white arrow) before (Non Comp) and after (Comp) compression with the sonographic transducer, demonstrated normal vein collapse with compression. Bottom Images: There is minimum compression of the common femoral vein (thick white arrow) in this patient with deep vein thrombosis. (Top images from Rumack CM, Wilson SR, Charboneau JW, Levine D: Diagnostic ultrasound, ed 4, Philadelphia, 2010, Mosby. Bottom images from Mason RJ, Broaddus VC, Martin T, et al: Murray and Nadel’s textbook of respiratory medicine, ed 5, Philadelphia, 2010, Saunders.)
7. When should prophylaxis of DVT be considered?
8. What prophylactic measures are available?
9. What is the approach to DVT prophylaxis in the hospitalized, medically ill patient?
 UFH: 5000 units subcutaneously (SC) every 8 or 12 hours
UFH: 5000 units subcutaneously (SC) every 8 or 12 hours
 LMWH: dalteparin: 5000 IU SC every 24 hours or enoxaparin: 40 mg SC every 24 hours
LMWH: dalteparin: 5000 IU SC every 24 hours or enoxaparin: 40 mg SC every 24 hours
10. Should patients undergoing surgery receive DVT prophylaxis based on specific recommendations for each respective procedure?
Yes. Most surgical procedures have defined recommendations for preventing DVT in the postoperative period if age and other clinical comorbidities demonstrate an elevated risk based upon risk assessment models, such as that of the Rogers or Caprini score. The various prophylaxis regimens for different surgical procedures are listed in Box 50-2.
11. Are there specific surgical groups that require extended DVT prophylaxis following hospital discharge?
For a patient undergoing total hip replacement, total knee replacement, and hip fracture surgery, extended DVT prophylaxis is recommended for up to 35 days after surgery, with LMWH, UFH, fondaparinux, warfarin, rivaroxaban, or aspirin.
12. What treatment regimens are available for the treatment of DVT?
Several treatment regimens using UFH or a LMWH are available for the treatment of DVT. These are listed in Box 50-3.
13. Which LMWHs are renally excreted?
14. When should warfarin be started with the regimens of treatment of DVT listed earlier?
15. When should these therapeutic regimens for treating DVT be discontinued and warfarin remain as the sole therapy?
These therapies must be used for at least 5 days and until the INR is more than 2 for 24 hours.
16. What is the target INR for treating patients with DVT?
The target INR for the treatment of DVT to prevent recurrent disease is 2 to 3.
17. How long should patients with acute DVT be treated with warfarin?
For patients with DVT secondary to a transient risk factor, 3 months of warfarin is appropriate. Idiopathic proximal DVT in patients without risk factors for bleeding should receive long-term warfarin therapy with a target INR of 2 to 3. Patients with DVT and cancer should receive LMWH for 3 to 6 months as the initial approach to management and long-term treatment with either warfarin or LMWH until the cancer is resolved or in remission.
18. When can patients with acute DVT ambulate?
19. Can patients with acute DVT be treated as outpatients?
20. When should catheter-directed thrombolysis be used to treat acute DVT?
21. Are inferior vena caval filters indicated for the initial treatment of acute DVT?
22. When are gradient elastic stockings recommended as part of the treatment of acute DVT?
23. When is a low-intensity INR anticoagulant therapy indicated for the treatment of DVT?
24. Are there other INR ranges for DVT prophylaxis in orthopedic surgery?
25. Should compression ultrasound be used as routine screening in the total joint replacement surgery patient at the time of discharge?
Bibliography, Suggested Readings, and Websites
1. British Thoracic Society Standards of Care Committee: Pulmonary Embolism Guideline Development Group. British Thoracic Society guidelines for the management of suspected acute pulmonary embolism. Thorax. 2003;58:470–483.
2. Cardiovascular Disease Educational and Research Trust, Cyprus Cardiovascular Disease Educational and Research Trust, European Venous Forum, et al. Prevention and treatment of venous thromboembolism. International consensus statement (guidelines according to scientific evidence). Int Angiol. 2006;25:101–161.
3. Decousus, H., Leizorovicz, A., Parent, F., et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. N Engl J Med. 1998;338:409–415.
4. Gould, M.K., Garcia, D.A., Wren, S.M., et al. Prevention of VTE in Nonorthopedic Surgical Patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(Suppl 2):e227S–e277S.
5. Kahn, S.R., Lim, W., Dunn, A.S., et al. Prevention of VTE in Nonsurgical Patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(Suppl 2):e195S–e226S.
6. Kearon, C., Ginsberg, J.S., Julian, J.A., et al. Comparison of fixed-dose weight adjusted unfractionated heparin and low-molecular weight heparin for acute treatment of venous thromboembolism. JAMA. 2006;296:935–942.
7. Koopman, M.M., Prandoni, P., Piovella, F., et al. Treatment of venous thrombosis with intravenous unfractionated heparin administered in the hospital as compared with subcutaneous low-molecular-weight heparin administered at home. N Engl J Med. 1996;334:682–687.
8. Levine, M., Gent, M., Hirsh, J., et al. A comparison of low-molecular-weight heparin administered primarily at home with unfractionated heparin administered in the hospital for proximal deep vein thrombosis. N Engl J Med. 1996;334:677–681.
9. The Matisse Investigators. Subcutaneous fondaparinux versus intravenous unfractionated heparin in the initial treatment of pulmonary embolism. N Engl J Med. 2003;349:1695–1702.
10. Merli, G.J. Pathophysiology of venous thrombosis and the diagnosis of deep vein thrombosis-pulmonary embolism in the elderly. Cardiol Clin. 2008;26:203–219.
11. Merli, G., Spiro, T., Olsson, C.G., et al. Subcutaneous enoxaparin once or twice daily compared with intravenous unfractionated heparin for treatment of venous thromboembolic disease. Ann Intern Med. 2001;134:191–202.
12. Snow, V., Qaseem, A., Barry, P., et al. Management of venous thromboembolism: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2007;146(3):204–210.
13. Wells, P.S., Anderson, D.R., Rodger, M.A., et al. A randomized trial comparing 2 low-molecular-weight heparins for the outpatient treatment of deep vein thrombosis and pulmonary embolism. Arch Intern Med. 2005;165:733–738.
14. Falck-Ytter, Y., Francis, C.W., Johanson, N.A., et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(Suppl 2):e278S–e325S.





























































