Complete fatty infiltration and replacement of parenchyma (often by end of teenage years)
 Pancreatic cysts: Usually small (< 3 mm), but can be larger and can completely replace pancreas (cystosis)
Pancreatic cysts: Usually small (< 3 mm), but can be larger and can completely replace pancreas (cystosis)• Bowel

 in a young adult patient with cystic fibrosis (CF).
in a young adult patient with cystic fibrosis (CF).
 and collapsed distal small bowel
and collapsed distal small bowel  . Just proximal to the point of transition is the classic “small bowel feces sign”
. Just proximal to the point of transition is the classic “small bowel feces sign”  associated with mechanical small-bowel obstruction, with the obstruction caused by inspissated enteric contents (distal intestinal obstruction syndrome or DIOS).
associated with mechanical small-bowel obstruction, with the obstruction caused by inspissated enteric contents (distal intestinal obstruction syndrome or DIOS).
 but less pseudohypertrophy. This 29-year-old woman had longstanding pancreatic exocrine dysfunction due to CF.
but less pseudohypertrophy. This 29-year-old woman had longstanding pancreatic exocrine dysfunction due to CF.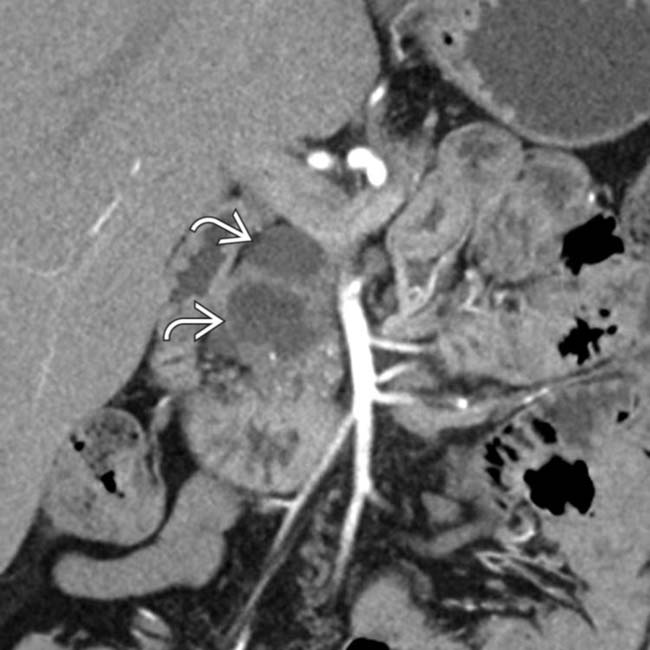
 in the pancreatic head in a young patient with CF. While pancreatic cysts are often very small in CF patients, they can rarely be larger, as in this case.
in the pancreatic head in a young patient with CF. While pancreatic cysts are often very small in CF patients, they can rarely be larger, as in this case.IMAGING
General Features
Other Abdominal Findings
• Biliary
 Gallstones in up to 1/4 of patients with CF, often with nonspecific gallbladder wall thickening and sludge
Gallstones in up to 1/4 of patients with CF, often with nonspecific gallbladder wall thickening and sludge
 Gallstones in up to 1/4 of patients with CF, often with nonspecific gallbladder wall thickening and sludge
Gallstones in up to 1/4 of patients with CF, often with nonspecific gallbladder wall thickening and sludge• Bowel
 Obstruction
Obstruction
 Increased risk for intussusception
Increased risk for intussusception
 Obstruction
Obstruction
– Bubbly fecal mass within bowel causing proximal obstruction, most often in infants (meconium ileus)
 Increased risk for intussusception
Increased risk for intussusception
CLINICAL ISSUES
Presentation
• Clinical profile
 Symptoms of hepatobiliary dysfunction
Symptoms of hepatobiliary dysfunction
 Symptoms of hepatobiliary dysfunction
Symptoms of hepatobiliary dysfunction

 of the transverse and left colon. The patient was completely asymptomatic, and this was felt to be benign pneumatosis due to gas dissecting from the chest into the bowel wall as a result of the patient’s lung disease.
of the transverse and left colon. The patient was completely asymptomatic, and this was felt to be benign pneumatosis due to gas dissecting from the chest into the bowel wall as a result of the patient’s lung disease.
 . Scattered, small calcifications are a more common finding in this disease.
. Scattered, small calcifications are a more common finding in this disease.
 of the body and tail of the pancreas. Note that the pancreas consequently shows high T1WI signal.
of the body and tail of the pancreas. Note that the pancreas consequently shows high T1WI signal.
 that mimics a cystic neoplasm. However, pancreatic cysts of variable size are commonly encountered in patients with CF.
that mimics a cystic neoplasm. However, pancreatic cysts of variable size are commonly encountered in patients with CF.

 . The pancreas shows fatty replacement
. The pancreas shows fatty replacement  .
.
 in the pancreatic tail in a young patient with CF. Notice the fatty infiltration of the surrounding pancreatic tail. While pancreatic cysts are often very small in CF patients, they can rarely be larger, as in this case.
in the pancreatic tail in a young patient with CF. Notice the fatty infiltration of the surrounding pancreatic tail. While pancreatic cysts are often very small in CF patients, they can rarely be larger, as in this case.



































































 .
.

 . The pancreatic duct is of normal caliber
. The pancreatic duct is of normal caliber  .
.


