CHAPTER 329 Current Concepts of Hypothermia in Traumatic Brain Injury
This chapter reviews evidence for the use of therapeutic hypothermia in the treatment of traumatic brain injury (TBI). During the past decade, encouraging results have been reported in clinically relevant animal models of TBI; specifically, it has been shown that modest levels of cooling for various periods after trauma can improve behavioral and histologic outcomes in a number of laboratory settings.1–8 Importantly, some of these results have been successfully translated to the clinic, and multiple clinical studies have reported the beneficial effects of mild cooling in head-injured patients.9–18
The results accumulated from many experimental and clinical studies indicate that hypothermic therapy may have a place in the standard care of severely head injured patients. However, controversies still exist regarding the efficacy of hypothermia, as well as the mechanisms by which cooling may protect the brain.19 Thus, there is a continued need to investigate the usefulness of mild cooling in both animal models and patients with severe TBI.
In reviewing the published data on the use of hypothermia, it is clear that relatively small variations in pretraumatic or posttraumatic brain temperature can critically alter the cellular, biochemical, and molecular responses of the brain to injury.20–29 Thus, laboratory investigations have reported that this treatment affects multiple pathologic mechanisms thought to be important in trauma-induced cell death and the development of functional deficits. Indeed, one of the advantages of hypothermia is that cooling targets several of the major injury mechanisms believed to be important in the pathophysiology of TBI.
In addition to the importance of mild reductions in temperature on outcome after trauma, experimental and clinical investigations have emphasized the potentially detrimental effects of mild fever and brain hyperthermia on outcome after trauma.30–35 Experimental studies first demonstrated the detrimental effects of mild hyperthermia in animal models of TBI and emphasized the importance of maintaining normothermia in head-injured patients.30 Most recently, clinical studies have also reported that patients experiencing periods of hyperthermia in the intensive care unit may demonstrate worse outcomes after various neurological injuries.33,34 Because at the current time no therapeutic interventions have been successfully translated to head-injured patients that significantly improve functional outcome,36,37 it is important that treatment strategies including therapeutic hypothermia and the inhibition of reactive hyperthermia continue to be discussed and evaluated in the experimental and clinical TBI literature.
Experimental Brain Trauma
Renewed interest in the application of modest levels of brain hypothermia in experimental models of TBI occurred in the 1990s. This renewed interest followed mainly from the cerebral ischemia literature, which showed for the first time that relatively small variations in brain temperature critically determine the vulnerability of hippocampal neurons to a transient ischemic insult.20 Clifton and colleagues first reported that modest hypothermia before and after TBI improved beam walking in a rat model of fluid percussion brain injury.2 In that study, hypothermia of 30° C significantly reduced mortality rates, as well as attenuated deficits in beam balance and body weight loss in comparison to normothermic treatment. The effect of hypothermia (30° C) for 1 hour after injury on behavioral outcome was also evaluated by Lyeth and colleagues, who reported evidence of improved behavioral outcome.6 Dietrich and colleagues in 1994 showed that posttraumatic hypothermia (30° C) initiated 5 minutes after parasagittal fluid percussion brain injury significantly reduced overall contusion volume and preserved the survival of pericontusional cortical neurons.3 In addition to fluid percussion brain injury, hypothermia was also tested in other models of brain injury, including the controlled cortical impact and diffuse injury models.4,7 In a study by Dixon and colleagues, posttraumatic hypothermia reduced overall contusion volume in a controlled cortical impact injury model.4 In other studies, posttraumatic hypothermia reduced sensory, motor, and cognitive deficits relative to normothermic animals.1,6 In terms of the treatment window for hypothermia, Markgraf and colleagues reported improved neurological outcome if hypothermia (3 hours at 30°C) was initiated 60 minutes but not 90 minutes after cortical impact injury.8 Thus, data from multiple laboratories using different TBI models show that hypothermia protects against behavioral and neuropathologic deficits if treatment is initiated fairly early after injury.
Posttraumatic hypothermia has also been shown to reduce the extent of axonal damage in models of TBI.5,38–40 In one study, the use of preinjury or early posttraumatic hypothermia of relatively brief duration (60 minutes) provided significant axonal protection in the brain’s major projection systems.5 A well-known marker of axonal injury, amyloid precursor protein immunoreactive axonal profiles, was significantly reduced in traumatized animals treated with hypothermia. Because of the importance of diffuse axonal injury in the functional consequences of TBI,41 these findings emphasize the potential usefulness of this therapy in head-injury patients.
Rewarming Phase
Experimental data have emphasized that the rate of rewarming after a hypothermic period is critical in whether hypothermic protection is demonstrated. In a study in which axonal pathology was targeted for hypothermic intervention, Suerhio and Povlishock reported an exacerbation of traumatically induced axonal injury by rapid post-hypothermic rewarming.42 In contrast, posttraumatic hypothermia followed by a slow rewarming period was reported to protect the injured axons. In a related study, Matsushita and colleagues showed that posttraumatic hypothermia combined with slow rewarming was neuroprotective in a model of TBI complicated by a secondary hypoxic insult.43 The modest hypothermia induced in this complicated TBI model with slow but not rapid rewarming significantly reduced overall contusion volume in comparison to normothermic animals. These studies emphasize the importance of the rewarming phase when considering both the experimental and the clinical use of modest hypothermia.
The Importance of Gender
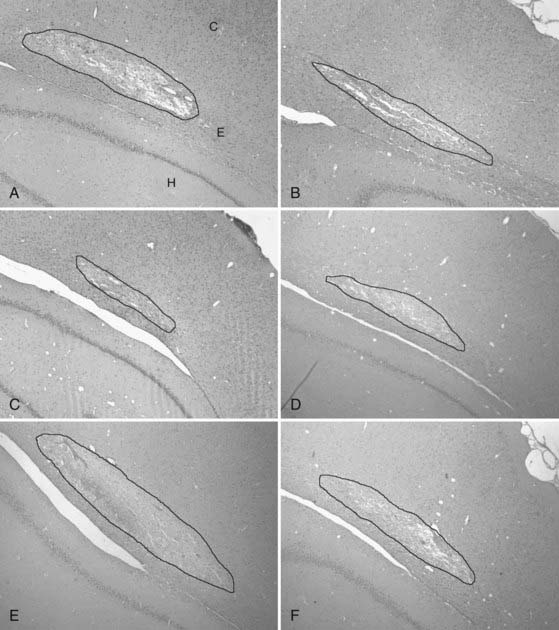
Gender may play an important role in the response of the brain to a variety of insults, including cerebral ischemia and trauma.44–49 Recently, the significance of gender has been reported after experimental TBI, with female animals showing smaller contusion volumes than corresponding traumatized male animals.47 The importance of endogenous sex hormones on this gender difference in vulnerability was also shown in this study; ovariectomized rats did not appear to be protected against TBI, whereas corresponding intact females did. Because of this potentially important gender factor in terms of therapeutic interventions, recent studies have determined whether gender also plays a role in the beneficial effects of modest hypothermia. In a study by Suzuki and colleagues, the importance of gender on the consequences of posttraumatic hypothermia after fluid percussion brain injury was assessed.48 Importantly, posttraumatic hypothermia (4 hours at 33° C) did not affect the short-term histologic outcome in intact female rats but significantly reduced contusion volume in ovariectomized rats (Fig. 329-1). In another study, the consequences of posttraumatic hyperthermia were found to be more severe in ovariectomized rats than in intact female or male animals.49 These data and others emphasize the potential importance of gender in both the beneficial effects of hypothermic therapy and the detrimental consequences of secondary injury mechanisms such as reactive hyperthermia in the TBI patient population.
Mechanisms of Hypothermic Protection
In early studies, profound brain cooling was reported to decrease O2 consumption and CO2 production, as well as other indicators of metabolism.50,51 Thus, the beneficial effects of hypothermic therapy were thought to primarily involve metabolic and energy demands. However, investigative studies over the past decade have shown that mild variations in temperature have profound effects on many injury mechanisms thought to be responsible for irreversible neuronal death and secondary injury mechanisms.52 In this regard, variations in ischemic brain injury or TBI have been shown to affect hemodynamic events, excitotoxicity, calcium-dependent intercellular signaling, inflammation and edema, apoptosis, and molecular changes in the postinjured brain. In the area of excitotoxicity, early studies showed that mild hypothermia reduced extracellular levels of the excitatory amino acid glutamate, as well as other neurotransmitters, after brain injury.24,53–55 In addition to hypothermia affecting neuronal vulnerability, mild cooling was also shown to protect against blood-brain barrier permeability after ischemia and trauma.56–58 A major mechanism by which hypothermia may confer protection is by reducing deleterious inflammatory events and trauma-induced increases in a number of proinflammatory cytokines that appear to represent important secondary injury mechanisms.21,25,26,35,57–62
Apoptotic cell death has now been shown to also participate in the vulnerability of different cell types after trauma.63 Recent studies have demonstrated that posttraumatic hypothermia can reduce levels of caspase-3, an important initiator of apoptotic cell death, as well as reduce release of cytochrome c.27 The molecular mechanisms regulating these cellular events after trauma have also recently been shown to be temperature sensitive.64 In a recent study, hypothermic therapy was shown to selectively reduce specific inflammatory genes believed to be important in secondary injury processes.64 Thus, the ability of posttraumatic temperature to affect the acute and more delayed biochemical and genetic responses to injury has expanded our understanding of the complexity of the consequences that temperature may have on pathophysiology and recovery after brain injury.
Clinical Studies
In the early 1960s, profound levels of hypothermia were used in a number of centers as part of the routine treatment of severe TBI.50,65 By the end of the 1970s, however, the use of hypothermia to treat TBI patients was mainly discontinued because of a number of reasons, including serious side effects such as infectious complications, cardiovascular incidents, and the general difficulty in cooling patients. In addition, laboratory work was just clarifying injury mechanisms that could be targeted with new pharmacologic agents, including barbiturates.
In the 1990s, because of the demonstration that more modest levels of hypothermia improved outcomes in clinically relevant models of TBI, attention was turned to the use of mild hypothermia in several clinical studies.11,12,16,18,66,67 In a study of 82 patients with severe head injury, Marion and colleagues (1993) first reported that 62% of patients in the hypothermia group had good outcomes 12 months after injury versus 38% of those in the normothermic group.11
Jiang and colleagues investigated the effects of long-term (3 to 14 days) mild hypothermia therapy (33° C to 35° C) on outcome in 87 patients with severe TBI.68 These investigators found that the rate of complications between the normothermic and hypothermic patients was not significantly different and that induced hypothermia markedly reduced intracranial pressure and inhibited hyperglycemia. The importance of cooling duration has been emphasized in both preclinical and clinical investigations. Although short periods of hypothermia may not provide long-term protection, longer periods of cooling appear to lead to improved outcome even months after the treatment has been terminated. Thus, in a recent study, Jiang and colleagues critically assessed the importance of the duration of hypothermia on behavioral outcome after severe TBI.16 Importantly, patients who were cooled for 5 days did significantly better than those that were cooled for only a 3-day period. Accordingly, future studies need to take into account the fact that in specific clinical cases, a prolonged cooling period may be necessary to achieve the best recovery after severe TBI.
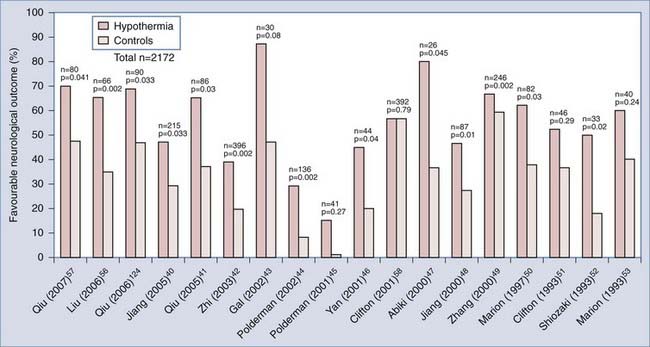
Based on encouraging single-center studies summarized by Polderman in 2008 (Fig. 329-2),10 a multicenter trial was initiated to test the efficacy of modest hypothermia in a large number of patients.19 In that study, 392 adult patients with severe trauma were randomly assigned to treatment with hypothermia or normothermia. In contrast to previous clinical studies,12,18 mortality was reported to be no different in the normothermic and hypothermic groups, and beneficial effects on outcome were not observed. It should be emphasized that several important limitations of this multicenter trial have been identified, including inconsistencies in patient care between the different investigative sites and delay in initiating the hypothermic therapy.69
A new meta-analysis of hypothermia clinical trials was recently reported in the third edition of the guidelines for the management of severe TBI in 2007.70 This analysis included 354 patients assigned to hypothermia groups and 340 patients assigned to normothermia groups from six clinical trials for which sufficient data were available.11,18,68,69,71,72 Although the risk for mortality was not significantly different between the hypothermic and normothermic groups, hypothermia was associated with a 46% increased chance of a good outcome. Currently, although hypothermic treatment is an experimental therapy and not considered a standard of care for patients with severe TBI, it may be considered an option for patients with refractory intracranial hypertension by clinicians experienced in its use. Finally, based on prospective results from the published multicenter trial on hypothermic treatment, a new hypothermia clinical trial focusing on adult patients younger than 45 years with severe TBI has been initiated. This trial emphasizes early cooling and more consistent management of the patients from various centers. A demonstration that hypothermia provides clinically relevant benefits in a large multicenter trial will be critical for successful translation of this experimental therapy to large numbers of severely injured patients.
Methods of Cooling
Recent technical advances in the development of cooling devices have improved the ability to induce modest hypothermia quickly in patients, as well as to maintain cooling levels for several days within relatively restricted ranges.73–81 In addition, these new approaches allow one to rigorously control the rewarming phase, which now appears to be so critical in hypothermic treatments. Although selective head cooling methodologies have been attempted in some patient populations, whole-body cooling is currently being tested in a number of clinical studies involving patients with neurological insults. In pediatric patients, for example, selective head cooling may be most advantageous to limit the potential adverse effects of systemic hypothermia.
Strategies that include surface cooling and the use of endovascular catheters appear to be advantageous in specific clinical conditions. The intravenous infusion of ice-cold fluids is a commonly used method to initiate early cooling, even in the out-of-hospital environment.75,82,83 In situations in which a central line is not required, surface cooling may be satisfactory in inhibiting periods of reactive hyperthermia, as well as in producing a mild hypothermic state.81 In contrast, intravascular catheters may have the advantage of reducing temperature in some patient populations at a faster rate and may provide more critical control over the range of temperatures during a prolonged cooling period.77–80 Whether surface or endovascular cooling is used will depend on the patient population being treated and the experience of the treating physician.
Pediatric Traumatic Brain Injury
The potential beneficial effects of modest hypothermia are also being evaluated in the pediatric patient population.84–86 Preclinical data support the concept that modest hypothermia may be protective in models of pediatric TBI. Thus, some studies have been initiated to test the efficacy of cooling in the pediatric TBI population.84–86 In particular, temperature regulation and the use of hypothermia in initial case studies of small numbers of patients provided encouraging results. However, a recently published phase III multicenter international study involving the use of moderate hypothermia (32.5° C for 24 hours) initiated within 8 hours in children and adolescents with severe TBI was reported to be negative.86 Discussions in the published manuscript and scientific literature have suggested potential shortcomings of this study, including delay in the initiation of treatment, critical care management issues, and problems with the rewarming procedure. Thus, additional work is required to determine the efficacy of this treatment in this specific TBI patient population.
Posttraumatic Hyperthermia
A high percentage of patients with neurological injuries have periods of reactive hyperthermia at variable points in time after the primary injury.10,32–35,75–77 Experimental studies have emphasized the detrimental effects of posttraumatic hyperthermia in terms of mortality and morbidity after TBI.30,35 Mechanistic studies have indicated that elevations in temperature after injury aggravate many of the pathologic mechanisms thought to participate in neuronal vulnerability and long-term behavioral deficits.21,30,49,87 Recently, several clinical studies have emphasized the importance of fever in extending hospital stay and worsening neurological outcome in patients with different neurological insults, including brain trauma.33,34,88,89 Another important observation is that dissociations between brain temperature and core temperature may occur in selected patients after head injury.90–92 In some patients, central nervous system temperature may be 1° C or 2° C higher than that being registered from the bladder or other organs from which systemic temperature readings are being monitored.90,91 Thus, it is critical that steps be aggressively taken to inhibit or at least minimize refractive hyperthermia.
Adelson PD, Ragheb J, Kanev P, et al. Phase II clinical trial of moderate hypothermia after severe traumatic brain injury in children. Neurosurgery. 2005;56:740-754.
Atkins CM, Oliva AAJr, Alonso OF, et al. Hypothermia treatment potentiates ERK1/2 activation after traumatic brain injury. Eur J Neurosci. 2007;26:810-819.
Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557-563.
Bramlett HM, Green EJ, Dietrich WD, et al. Posttraumatic brain hypothermia provides protection from sensorimotor and cognitive behavioral deficits. J Neurotrauma. 1995;12:289-298.
Bratton SL, Chestnut RM, Ghajar J, et al. III. Prophylactic hypothermia. J Neurotrauma. 2007;24(suppl 1):S21-S25.
Clifton GL, Choi SC, Miller ER, et al. Intercenter variance in clinical trials of head trauma—experience of the National Acute Brain Injury Study: hypothermia. J Neurosurg. 2001;95:733-734.
Clifton GL, Jiang JY, Lyeth BG, et al. Marked protection by moderate hypothermia after experimental traumatic brain injury. J Cereb Blood Flow Metab. 1991;11:114-121.
Clifton GL, Miller ER, Choi SC, et al. Lack of effect of induction of hypothermia after acute brain injury. N Engl J Med. 2001;344:556-563.
Dietrich WD, Alonso O, Busto R, et al. Post-traumatic brain hypothermia reduces histopathological damage following concussive brain injury in the rat. Acta Neuropathol. 1994;87:250-258.
Dietrich WD, Alonso O, Halley M, et al. Delayed posttraumatic brain hyperthermia worsens outcome after fluid percussion brain injury: a light and electron microscopic study in rats. Neurosurgery. 1996;38:533-541.
Dietrich WD, Bramlett HM. Hyperthermia and central nervous system injury. Prog Brain Res. 2007;162:201-217.
Diringer MN. Neurocritical Care Fever Reduction Trial Group: Treatment of fever in the neurologic intensive care unit with a catheter-based heat exchange system. Crit Care Med. 2004;32:559-564.
Diringer MN, Reaven NL, Funk SE, et al. Elevated body temperature independently contributes to increased length of stay in neurologic intensive care unit patients. Crit Care Med. 2004;32:1489-1495.
Hutchison JS, Ward RE, Lacroix J, et al. Hypothermia Pediatric Head Injury Trial Investigators and the Canadian Critical Care Trials Group: hypothermia therapy after traumatic brain injury in children. N Engl J Med. 2008;358:2447-2456.
Jiang JY, Lyeth BG, Kapasi MZ, et al. Moderate hypothermia reduces blood-brain barrier disruption following traumatic brain injury in the rat. Acta Neuropathol. 1992;84:495-500.
Jiang JY, Xu W, Li WP, et al. Effect of long-term mild hypothermia or short-term mild hypothermia on outcome of patients with severe traumatic brain injury. J Cereb Blood Flow Metab. 2006;26:771-776.
Koizumi H, Povlishock JT. Posttraumatic hypothermia in the treatment of axonal damage in an animal model of traumatic axonal injury. J Neurosurg. 1998;89:303-309.
Marion DW, Penrod LE, Kelsey SF, et al. Treatment of traumatic brain injury with moderate hypothermia. N Engl J Med. 1997;336:540-546.
Markgraf CG, Clifton GL, Moody MR. Treatment window for hypothermia in brain injury. J Neurosurg. 2001;95:979-983.
Mayer SA, Kowalski RG, Presciutti M, et al. Clinical trial of a novel surface cooling system for fever control in neurocritical care patients. Crit Care Med. 2004;32:2508-2515.
Polderman KH. Induced hypothermia and fever control for prevention and treatment of neurological injuries. Lancet. 2008;371:1955-1969.
Stein DG. Brain damage, sex hormones and recovery: a new role for progesterone and estrogen? Trends Neurosci. 2001;24:386-391.
Suehiro E, Povlishock JT. Exacerbation of traumatically induced axonal injury by rapid posthypothermic rewarming and attenuation of axonal change by cyclosporin A. J Neurosurg. 2001;94:493-498.
Suzuki T, Bramlett HM, Dietrich WD. The importance of gender on the beneficial effects of posttraumatic hypothermia. Exp Neurol. 2003;184:1017-1026.
Whalen MJ, Carlos TM, Clark RS, et al. The effect of brain temperature on acute inflammation after traumatic brain injury in rats. J Neurotrauma. 1997;14:561-572.
1 Bramlett HM, Green EJ, Dietrich WD, et al. Posttraumatic brain hypothermia provides protection from sensorimotor and cognitive behavioral deficits. J Neurotrauma. 1995;12:289-298.
2 Clifton GL, Jiang JY, Lyeth BG, et al. Marked protection by moderate hypothermia after experimental traumatic brain injury. J Cereb Blood Flow Metab. 1991;11:114-121.
3 Dietrich WD, Alonso O, Busto R, et al. Post-traumatic brain hypothermia reduces histopathological damage following concussive brain injury in the rat. Acta Neuropathol. 1994;87:250-258.
4 Dixon CE, Markgraf CG, Angileri F, et al. Protective effects of moderate hypothermia on behavioral deficits but not necrotic cavitation following cortical impact injury in the rat. J Neurotrauma. 1998;15:95-103.
5 Koizumi H, Povlishock JT. Posttraumatic hypothermia in the treatment of axonal damage in an animal model of traumatic axonal injury. J Neurosurg. 1998;89:303-309.
6 Lyeth BG, Jiang JY, Liu S. Behavioral protection by moderate hypothermia initiated after experimental traumatic brain injury. J Neurotrauma. 1993;10:57-64.
7 Yamamoto M, Marmarou CR, Stiefel MF, et al. Neuroprotective effect of hypothermia on neuronal injury in diffuse traumatic brain injury coupled with hypoxia and hypotension. J Neurotrauma. 1999;16:487-500.
8 Markgraf CG, Clifton GL, Moody MR. Treatment window for hypothermia in brain injury. J Neurosurg. 2001;95:979-983.
9 Gal R, Cundrle I, Zimova I, et al. Mild hypothermia therapy for patients with severe brain injury. Clin Neurol Neurosurg. 2002;104:318-321.
10 Polderman KH. Induced hypothermia and fever control for prevention and treatment of neurological injuries. Lancet. 2008;371:1955-1969.
11 Marion DW, Obrist WD, Carlier PM, et al. The use of moderate therapeutic hypothermia for patients with severe head injuries: a preliminary report. J Neurosurg. 1993;79:354-362.
12 Marion DW, Penrod LE, Kelsey SF, et al. Treatment of traumatic brain injury with moderate hypothermia. N Engl J Med. 1997;336:540-546.
13 Qiu W, Zhang Y, Sheng H, et al. Effects of therapeutic mild hypothermia on patients with severe traumatic brain injury after craniotomy. J Crit Care. 2007;22:229-235.
14 Qiu WS, Liu WG, Shen H, et al. Therapeutic effect of mild hypothermia on severe traumatic head injury. Chin J Traumatol. 2005;8:27-32.
15 Shiozaki T, Nakajima Y, Taneda M, et al. Efficacy of moderate hypothermia in patients with severe head injury and intracranial hypertension refractory to mild hypothermia. J Neurosurg. 2003;99:47-51.
16 Jiang JY, Xu W, Li WP, et al. Effect of long-term mild hypothermia or short-term mild hypothermia on outcome of patients with severe traumatic brain injury. J Cereb Blood Flow Metab. 2006;26:771-776.
17 Zhi D, Zhang S, Lin X. Study on therapeutic mechanism and clinical effect of mild hypothermia in patients with severe head injury. Surg Neurol. 2003;59:381-385.
18 Clifton GL, Allen S, Barrodale P, et al. A phase II study of moderate hypothermia in severe brain injury. J Neurotrauma. 1993;10:263-271.
19 Clifton GL, Miller ER, Choi SC, et al. Lack of effect of induction of hypothermia after acute brain injury. N Engl J Med. 2001;344:556-563.
20 Busto R, Dietrich WD, Globus MY, et al. Small differences in intraischemic brain temperature critically determine the extent of ischemic neuronal injury. J Cereb Blood Flow Metab. 1987;7:729-738.
21 Chatzipanteli K, Alonso OF, Kraydieh S, et al. Importance of posttraumatic hypothermia and hyperthermia on the inflammatory response after fluid percussion brain injury: biochemical and immunocytochemical studies. J Cereb Blood Flow Metab. 2000;20:531-542.
22 Büki A, Koizumi H, Povlishock JT. Moderate posttraumatic hypothermia decreases early calpain-mediated proteolysis and concomitant cytoskeletal compromise in traumatic axonal injury. Exp Neurol. 1999;159:319-328.
23 Atkins CM, Oliva AAJr, Alonso OF, et al. Hypothermia treatment potentiates ERK1/2 activation after traumatic brain injury. Eur J Neurosci. 2007;26:810-819.
24 Globus MY, Alonso O, Dietrich WD, et al. Glutamate release and free radical production following brain injury: effects of posttraumatic hypothermia. J Neurochem. 1995;65:1704-1711.
25 Goss JR, Styren SD, Miller PD, et al. Hypothermia attenuates the normal increase in interleukin 1 beta RNA and nerve growth factor following traumatic brain injury in the rat. J Neurotrauma. 1995;12:159-167.
26 Kinoshita K, Chatzipanteli K, Vitarbo E, et al. Interleukin-1beta messenger ribonucleic acid and protein levels after fluid-percussion brain injury in rats: importance of injury severity and brain temperature. Neurosurgery. 2002;51:195-203.
27 Lotocki G, de Rivero Vaccari JP, Perez ER, et al. Therapeutic hypothermia modulates TNFR1 signaling in the traumatized brain via early transient activation of the JNK pathway and suppression of XIAP cleavage. Eur J Neurosci. 2006;24:2283-2290.
28 Sakamoto KI, Fujisawa H, Koizumi H, et al. Effects of mild hypothermia on nitric oxide synthesis following contusion trauma in the rat. J Neurotrauma. 1997;14:349-353.
29 Whalen MJ, Carlos TM, Clark RS, et al. The effect of brain temperature on acute inflammation after traumatic brain injury in rats. J Neurotrauma. 1997;14:561-572.
30 Dietrich WD, Alonso O, Halley M, et al. Delayed posttraumatic brain hyperthermia worsens outcome after fluid percussion brain injury: a light and electron microscopic study in rats. Neurosurgery. 1996;38:533-541.
31 Verlooy J, Heytens L, Veeckmans G, et al. Intracerebral temperature monitoring in severely head injured patients. Acta Neurochir (Wien). 1995;134:76-78.
32 Cairns CJ, Andrews PJ. Management of hyperthermia in traumatic brain injury. Curr Opin Crit Care. 2002;8:106-110.
33 Diringer MN, Reaven NL, Funk SE, et al. Elevated body temperature independently contributes to increased length of stay in neurologic intensive care unit patients. Crit Care Med. 2004;32:1489-1495.
34 Oliveira-Filho J, Ezzeddine MA, Segal AZ, et al. Fever in subarachnoid hemorrhage: relationship to vasospasm and outcome. Neurology. 2001;56:1299-1304.
35 Thompson HJ, Hoover RC, Tkacs NC, et al. Development of posttraumatic hyperthermia after traumatic brain injury in rats is associated with increased periventricular inflammation. J Cereb Blood Flow Metab. 2005;25:163-176.
36 Marklund N, Bakshi A, Castelbuono DJ, et al. Evaluation of pharmacological treatment strategies in traumatic brain injury. Curr Pharm Des. 2006;12:1645-1680.
37 Narayan RK, Michel ME, Ansell B, et al. Clinical trials in head injury. J Neurotrauma. 2002;19:503-557.
38 Marion DW, White MJ. Treatment of experimental brain injury with moderate hypothermia and 21-aminosteroids. J Neurotrauma. 1996;13:139-147.
39 Maxwell WL, Donnelly S, Sun X, et al. Axonal cytoskeletal responses to nondisruptive axonal injury and the short-term effects of posttraumatic hypothermia. J Neurotrauma. 1999;16:1225-1234.
40 Taft WC, Yang K, Dixon CE, et al. Hypothermia attenuates the loss of hippocampal microtubule-associated protein 2 (MAP2) following traumatic brain injury. J Cereb Blood Flow Metab. 1993;13:796-802.
41 Povlishock JT. Traumatically induced axonal injury: pathogenesis and pathobiological implications. Brain Pathol. 1992;2:1-12.
42 Suehiro E, Povlishock JT. Exacerbation of traumatically induced axonal injury by rapid posthypothermic rewarming and attenuation of axonal change by cyclosporin A. J Neurosurg. 2001;94:493-498.
43 Matsushita Y, Bramlett HM, Alonso O, et al. Posttraumatic hypothermia is neuroprotective in a model of traumatic brain injury complicated by a secondary hypoxic insult. Crit Care Med. 2001;29:2060-2066.
44 Hurn PD, Macrae IM. Estrogen as a neuroprotectant in stroke. J Cereb Blood Flow Metab. 2000;20:631-652.
45 Roof RL, Hall ED. Estrogen-related gender difference in survival rate and cortical blood flow after impact-acceleration head injury in rats. J Neurotrauma. 2000;17:1155-1169.
46 Stein DG. Brain damage, sex hormones and recovery: a new role for progesterone and estrogen? Trends Neurosci. 2001;24:386-391.
47 Bramlett HM, Dietrich WD. Neuropathological protection after traumatic brain injury in intact female rats versus males or ovariectomized females. J Neurotrauma. 2001;18:891-900.
48 Suzuki T, Bramlett HM, Dietrich WD. The importance of gender on the beneficial effects of posttraumatic hypothermia. Exp Neurol. 2003;184:1017-1026.
49 Suzuki T, Bramlett HM, Ruenes G, et al. The effects of early post-traumatic hyperthermia in female and ovariectomized rats. J Neurotrauma. 2004;21:842-853.
50 Rosomoff HL. The effects of hypothermia on the physiology of the nervous system. Surgery. 1956;40:328-336.
51 Rosomoff HL. Cerebral blood flow and cerebral oxygen consumption during hypothermia. Am J Physiol. 1954;179:85-88.
52 Dietrich WD. The importance of brain temperature in cerebral injury. J Neurotrauma. suppl 2. 1992:S475-S485.
53 Jiang JY, Liang YM, Luo QZ, et al. Effect of mild hypothermia on brain dialysate lactate after fluid percussion brain injury in rodents. Neurosurgery. 2004;54:713-717.
54 Lyeth BG, Jiang JY, Robinson SE, et al. Hypothermia blunts acetylcholine increase in CSF of traumatically brain injured rats. Mol Chem Neuropathol. 1993;18:247-256.
55 Koizumi H, Fujisawa H, Ito H, et al. Effects of mild hypothermia on cerebral blood flow–independent changes in cortical extracellular levels of amino acids following contusion trauma in the rat. Brain Res. 1997;747:304-312.
56 Jiang JY, Lyeth BG, Kapasi MZ, et al. Moderate hypothermia reduces blood-brain barrier disruption following traumatic brain injury in the rat. Acta Neuropathol. 1992;84:495-500.
57 Kinoshita K, Chatzipanteli K, Alonso OF, et al. The effect of brain temperature on hemoglobin extravasation after traumatic brain injury. J Neurosurg. 2002;97:945-953.
58 Arican N, Kaya M, Yorulmaz C, et al. Effect of hypothermia on blood-brain barrier permeability following traumatic brain injury in chronically ethanol-treated rats. Int J Neurosci. 2006;116:1249-1261.
59 Chatzipanteli K, Wada K, Busto R, et al. Effects of moderate hypothermia on constitutive and inducible nitric oxide synthase activities after traumatic brain injury in the rat. J Neurochem. 1999;72:2047-2052.
60 Whalen MJ, Carlos TM, Clark RS, et al. The relationship between brain temperature and neutrophil accumulation after traumatic brain injury in rats. Acta Neurochir Suppl. 1997;70:260-261.
61 Vitarbo EA, Chatzipanteli K, Kinoshita K, et al. Tumor necrosis factor alpha expression and protein levels after fluid percussion injury in rats: the effect of injury severity and brain temperature. Neurosurgery. 2004;55:416-424.
62 Truettner JS, Alonso OF, Dalton Dietrich W. Influence of therapeutic hypothermia on matrix metalloproteinase activity after traumatic brain injury in rats. J Cereb Blood Flow Metab. 2005;25:1505-1516.
63 Keane RW, Kraydieh S, Lotocki G, et al. Apoptotic and antiapoptotic mechanisms after traumatic brain injury. J Cereb Blood Flow Metab. 2001;21:1189-1198.
64 Truettner JS, Suzuki T, Dietrich WD. The effect of therapeutic hypothermia on the expression of inflammatory response genes following moderate traumatic brain injury in the rat. Brain Res Mol Brain Res. 2005;138:124-134.
65 Sedzimir CB. Therapeutic hypothermia in cases of head injury. J Neurosurg. 1959;16:407-414.
66 Metz C, Holzschuh M, Bein T, et al. Moderate hypothermia in patients with severe head injury: cerebral and extracerebral effects. J Neurosurg. 1997;86:911-914.
67 Tateishi A, Soejima Y, Taira Y, et al. Feasibility of the titration method of mild hypothermia in severely head-injured patients with intracranial hypertension. Neurosurgery. 1998;42:1065-1069.
68 Jiang J, Yu M, Zhu C. Effect of long-term mild hypothermia therapy in patients with severe traumatic brain injury: 1-year follow-up review of 87 cases. J Neurosurg. 2000;93:546-549.
69 Clifton GL, Choi SC, Miller ER, et al. Intercenter variance in clinical trials of head trauma—experience of the National Acute Brain Injury Study: hypothermia. J Neurosurg. 2001;95:733-734.
70 Bratton SL, Chestnut RM, Ghajar J, et al. III. Prophylactic hypothermia. J Neurotrauma. 2007;24(suppl 1):S21-S25.
71 Aibiki M, Maekawa S, Yokono S. Moderate hypothermia improves imbalances of thromboxane A2 and prostaglandin I2 production after traumatic brain injury in humans. Crit Care Med. 2000;28:3902-3906.
72 Qiu W, Zhang Y, Sheng H, et al. Effects of therapeutic mild hypothermia on patients with severe traumatic brain injury after craniotomy. J Crit Care. 2007;22:229-235.
73 Steinberg GK, Ogilvy CS, Shuer LM, et al. Comparison of endovascular and surface cooling during unruptured cerebral aneurysm repair. Neurosurgery. 2004;55:307-314.
74 Axelrod YK, Diringer MN. Temperature management in acute neurologic disorders. Crit Care Clin. 2006;22:767-785.
75 Badjatia N, Bodock M, Guanci M, et al. Rapid infusion of cold saline (4 degrees C) as adjunctive treatment of fever in patients with brain injury. Neurology. 2006;66:1739-1741.
76 Badjatia N, O’Donnell J, Baker JR, et al. Achieving normothermia in patients with febrile subarachnoid hemorrhage: feasibility and safety of a novel intravascular cooling catheter. Neurocrit Care. 2004;1:145-156.
77 Diringer MN. Neurocritical Care Fever Reduction Trial Group: Treatment of fever in the neurologic intensive care unit with a catheter-based heat exchange system. Crit Care Med. 2004;32:559-564.
78 Hinz J, Rosmus M, Popov A, et al. Effectiveness of an intravascular cooling method compared with a conventional cooling technique in neurologic patients. J Neurosurg Anesthesiol. 2007;19:130-135.
79 Holzer M, Müllner M, Sterz F, et al. Efficacy and safety of endovascular cooling after cardiac arrest: cohort study and Bayesian approach. Stroke. 2006;37:1792-1797.
80 Keller E, Imhof HG, Gasser S, et al. Endovascular cooling with heat exchange catheters: a new method to induce and maintain hypothermia. Intensive Care Med. 2003;29:939-943.
81 Mayer SA, Kowalski RG, Presciutti M, et al. Clinical trial of a novel surface cooling system for fever control in neurocritical care patients. Crit Care Med. 2004;32:2508-2515.
82 Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557-563.
83 Polderman KH, Rijnsburger ER, Peerdeman SM, et al. Induction of hypothermia in patients with various types of neurologic injury with use of large volumes of ice-cold intravenous fluid. Crit Care Med. 2005;33:2744-2751.
84 Biswas AK, Bruce DA, Sklar FH, et al. Treatment of acute traumatic brain injury in children with moderate hypothermia improves intracranial hypertension. Crit Care Med. 2002;30:2742-2751.
85 Adelson PD, Ragheb J, Kanev P, et al. Phase II clinical trial of moderate hypothermia after severe traumatic brain injury in children. Neurosurgery. 2005;56:740-754.
86 Hutchison JS, Ward RE, Lacroix J, et al. Hypothermia Pediatric Head Injury Trial Investigators and the Canadian Critical Care Trials Group: hypothermia therapy after traumatic brain injury in children. N Engl J Med. 2008;358:2447-2456.
87 Fernandez A, Schmidt JM, Claassen J, et al. Fever after subarachnoid hemorrhage: risk factors and impact on outcome. Neurology. 2007;68:1013-1019.
88 Kilpatrick MM, Lowry DW, Firlik AD, et al. Hyperthermia in the neurosurgical intensive care unit. Neurosurgery. 2000;47:850-855.
89 Dietrich WD, Bramlett HM. Hyperthermia and central nervous system injury. Prog Brain Res. 2007;162:201-217.
90 Hayashi N, Hirayama T, Utagawa A. The cerebral thermo-pooling and hypothermia treatment of critical head injury patients. In: Nagai H, editor. Intracranial Pressure IX. Berlin: Springer; 1993:589-599.
91 Henker RA, Brown SD, Marion DW. Comparison of brain temperature with bladder and rectal temperatures in adults with severe head injury. Neurosurgery. 1988;42:1071-1075.
92 Mellergård P, Nordström CH. Intracerebral temperature in neurosurgical patients. Neurosurgery. 1991;28:709-713.