Cricothyrotomy and Percutaneous Translaryngeal Ventilation
Few clinical scenarios are as critical as when a patient’s airway cannot be controlled with traditional endotracheal (ET) intubation. Although cricothyroidotomy is rarely required,1–4 the incidence of surgical airways has decreased even further since the advent of adjunctive intubation techniques.5,6 The conditions accompanying an airway emergency are often stressful and chaotic and require the emergency department (ED) physician to be intimately familiar with this procedure.
Anatomy
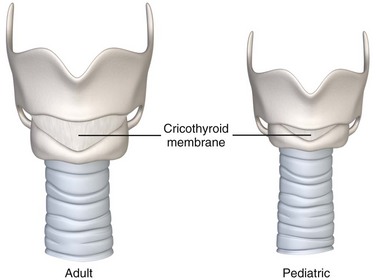
Identify the cricothyroid membrane between the previously mentioned structures as a shallow depression measuring about 9 mm longitudinally and 30 mm transversely. If the depression is obscured by soft tissue swelling, estimate the location of the cricothyroid membrane at about 2 to 3 cm inferior to the laryngeal prominence or four fingerbreadths above the sternal notch.7–9
The area overlying and immediately adjacent to the cricothyroid membrane is relatively avascular and free of other significant anatomic structures. The cricothyroid arteries branch from the superior thyroid arteries and may form a small anastomotic arch traversing the superior aspect of the cricothyroid membrane. The external branch of the superior laryngeal nerve runs along the lateral aspect of the larynx and innervates the cricothyroid muscles inferior to the membrane. The isthmus of the thyroid gland most often overlies the second and third tracheal rings, although an aberrant pyramidal lobe of the gland may extend just superior to the cricothyroid membrane. The anterior attachments of the vocal cord structures are protected by the thyroid cartilage10,11 (Fig. 6-1).
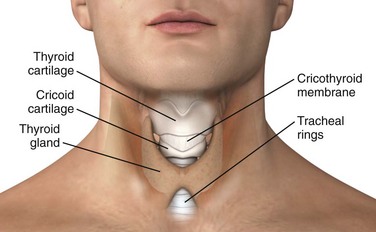
Figure 6-1 Normal adult larynx.
In children, the larynx is positioned more superiorly than in adults.12 There is also more overlap between the thyroid cartilage and the cricoid cartilage, thus making the cricoid membrane proportionally smaller13 (Fig. 6-2).
Surgical Cricothyrotomy
Indications and Contraindications
The chief indication for surgical cricothyrotomy is an inability to secure the airway with less invasive techniques in a patient with impending or ongoing hypoxia.14
Surgical cricothyrotomy, like any invasive procedure, is associated with significant complications and should not be attempted until less invasive measures have failed. No simple algorithm fits all cases. When time and the clinical situation allow, it may be appropriate to attempt to intubate multiple times with traditional laryngoscopy or to try alternative intubation techniques. Emergency decisions are subject to controversy and differ on a case-by-case analysis, but alternatives to cricothyrotomy include bag-valve-mask ventilation, the gum elastic bougie, and laryngeal mask airways. At some point, further attempts at intubation become futile and the benefits of a surgical airway outweigh the risks associated with ongoing hypoxia.15
When approaching a patient with a compromised airway, the clinician must have a clear potential algorithm in mind with a well-defined plan that shifts the airway approach from laryngoscopy to alternative techniques to cricothyrotomy.16 The first step in deciding whether cricothyrotomy is indicated is anticipating a possible difficult intubation.17
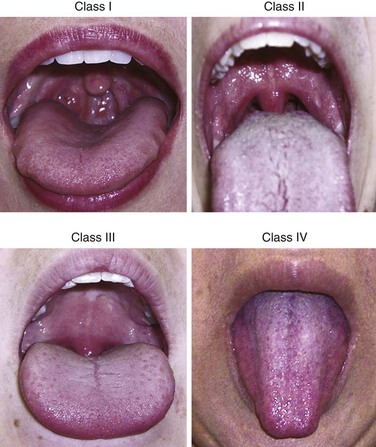
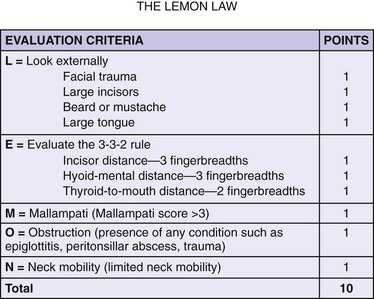
Several studies in the anesthesia and emergency medicine literature have attempted to identify predictors of a difficult airway. A Mallampati score can be determined in cooperative patients who are able to sit upright. It classifies the degree that the faucial pillars, soft palate, and uvula can be visualized (Fig. 6-3). A higher score predicts a more difficult ET intubation.18 A Mallampati score can be obtained only in a limited number of ED patients requiring intubation.19 A modified LEMON score, when excluding the Mallampati score, is more easily applied to ED patients for prediction of more difficult ET intubation20 (Fig. 6-4). Additional indicators of a difficult airway include obesity, oropharyngeal edema, hemorrhage, and laryngospasm21–24 (Box 6-1).
Cricothyrotomy is indicated when a difficult airway becomes a “failed airway,” and this is somewhat difficult to define in emergency medicine. The American Society of Anesthesiologists suggests defining a failed airway as an inability to maintain oxygen saturation greater than 90%, signs of inadequate ventilation (cyanosis, absent breath sounds, hemodynamic instability) with positive pressure bag-mask ventilation, or more than three failed attempts at ET intubation or failure to intubate after 10 minutes by an experienced operator.25 As more rescue airway adjunctive devices such as the laryngeal mask airway, gum elastic bougie, or lighted stylet become available, it is reasonable to continue beyond three attempts at ET intubation if adequate ventilation and oxygen saturation greater than 90% can be maintained.26,27
Because of the anatomic differences between children and adults, including a smaller cricothyroid membrane and a rostral, funnel-shaped, and more compliant pediatric larynx, surgical cricothyrotomy has been contraindicated in infants and young children. The exact age at which surgical cricothyrotomy can be done is controversial and not well defined. Various textbooks list the lower age limit from 5 years28 to 10 years29 or 12 years.30 The advanced cardiac life support (ACLS) and pediatric advanced life support (PALS) define an infant airway as age up to 1 year and a child airway as age 1 to 8 years.
Some authors also identify tracheal transection or low tracheal obstruction (below the cricoid) as absolute contraindications to cricothyrotomy because of the need to secure the airway below the injury31 (Box 6-2).
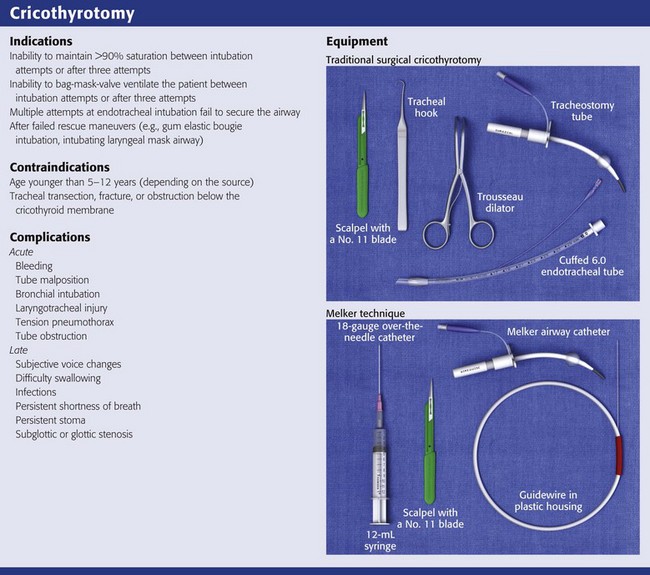
Equipment
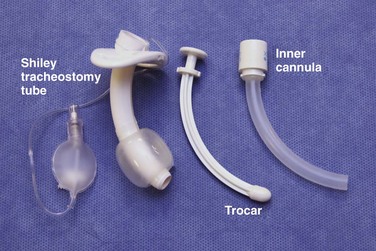
The equipment necessary to perform a traditional surgical cricothyrotomy includes a scalpel with a No. 11 blade, a Trousseau dilator, a tracheal hook, and a tracheostomy tube or modified ET tube (see Review Box 6-1). Bent 18-gauge needles may substitute for tracheal hooks. In addition, the sterile tray may include a syringe and lidocaine with epinephrine for local anesthesia, sterile drapes or towels, antiseptic preparation solution, 4 × 4-cm sterile gauze, scissors, hemostats, and suture material. The average adult’s cricothyroid membrane is about 9 mm longitudinally and 30 mm horizontally. Familiarity with the dimensions of several standard tracheostomy and ET tubes is essential when selecting the appropriate size for surgical airways. Cuffed tracheostomy tubes are recommended, and they come in various sizes. Shiley tracheostomy tubes are commonly available in most EDs. The No. 4 tube has an inner diameter (ID) of 5.0 mm and an outer diameter (OD) of 9.4 mm, and the No. 6 tube has an ID of 6.4 mm and an OD of 10.8 mm. Shiley tracheostomy tubes come with three parts: a cuffed outer cannula, a removable inner cannula, and a removable obturator that is solid and removed after insertion (Fig. 6-5). ET tubes are often used temporarily in place of a tracheostomy tube. With respect to ID, ET tube OD can vary with the manufacturer. As an example, the Mallinckrodt TaperGuard Evac Endotracheal Tube with IDs of 6.0 and 8.0 mm have ODs of 9.0 and 11.8 mm, respectively.32 Although a No. 11 scalpel blade is most commonly used, a No. 20 blade is recommended in some variations of the technique. Commercially available kits include the Melker Cricothyrotomy Kit (Cook Critical Care, Bloomington, IN) for percutaneous cricothyrotomy, which uses the Seldinger technique to insert a cuffed or uncuffed airway catheter.
Procedure
Positioning plays a critical role in success, but the ideal patient position may be impossible because of clinical parameters. For example, hypoxic patients often cannot recline. Ketamine anesthesia does not suppress the respiratory drive and may aid in patient cooperation and positioning. When feasible, use the supine position with the neck exposed. Unless the patient has a known or suspected cervical spine injury, it is important to hyperextend the neck to more readily identify the landmarks. Surgical cricothyrotomy can safely and successfully be performed with minimal cervical spine movement.33 Preoxygenate the patient by bag-mask ventilation. Prepare the skin of the anterior aspect of the neck with antiseptic solution and create a sterile field with the use of drapes or towels. If the patient is awake or responding to pain, give a subcutaneous and translaryngeal injection of lidocaine with epinephrine as a local anesthetic. Test the integrity of the balloon on the tracheostomy or ET tube by injecting it with 10 mL of air. Wear sterile gloves and take standard precautions by wearing a mask, goggles, and gown. All preparatory steps are optional and depend on the urgency of the procedure.
Traditional Technique
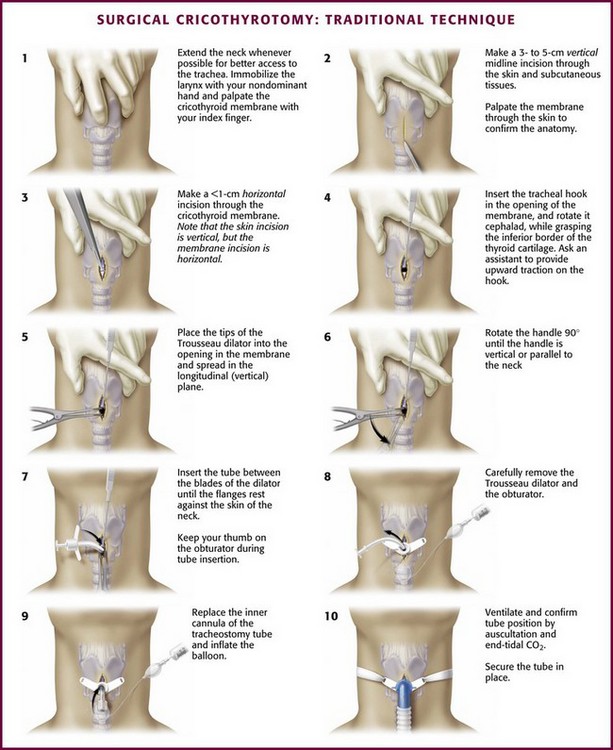
The “traditional” (open) cricothyrotomy technique (Fig. 6-6) has changed little since the original description of elective cricothyroidotomy by Brantigan and Grow in 1976.34 McGill and colleagues35 described the addition of a tracheal hook for emergency cricothyrotomy in 1982. In a follow-up report in 1989, Erlandson and colleagues36 emphasized the importance of making an initial vertical skin incision and using a relatively small (No. 4 Shiley) tracheal tube. These modifications have generally been accepted and are commonly described as part of the traditional technique.37
If you are right hand dominant, stand on the patient’s right side. Stabilize the larynx with the nondominant hand by grasping both sides of the lateral thyroid cartilage with the thumb and middle finger. Palpate the depression over the cricothyroid membrane with the index finger. Control the larynx throughout the procedure by stabilizing it in this manner (Fig. 6-6, step 1). If the laryngeal landmarks are not easily identifiable because of obesity or swelling, bedside ultrasonography may assist in identifying the cricothyroid membrane38,39 (Fig. 6-7).
While holding the scalpel with a No. 11 blade in the dominant hand, make an approximately 2- to 3-cm vertical incision through the skin and subcutaneous tissue (Fig. 6-6, step 2). With the index finger of the nondominant hand, palpate the cricothyroid membrane through the incision. It is important to understand that the remainder of the procedure should be performed by palpation of the anatomy, not visualization, because bleeding may obscure the field and there is no time to delay while trying to achieve hemostasis. If the cricothyroid membrane cannot be palpated, extend the initial incision superiorly and inferiorly and try to palpate again. Using the stabilizing index finger as a guide, make a horizontal incision of less than 1.0 cm in length through the cricothyroid membrane (Fig. 6-6, step 3). Note that the skin incision is vertical but the membrane incision is horizontal. Place the index finger into the stoma momentarily to exchange the scalpel for the tracheal hook.40
Using the dominant hand, place the tracheal hook into the opening in the cricothyroid membrane. Rotate the handle cephalad while grasping the inferior border of the thyroid cartilage with it. Ask an assistant to provide upward traction or provide traction yourself by passing the handle of the hook to the nondominant hand (Fig. 6-6, step 4). Use the tracheal hook to stabilize the larynx and keep it in place throughout the remainder of the procedure.
With the dominant hand, place the tips of the Trousseau dilator into the opening in the membrane with the spreading action oriented initially in the longitudinal or vertical plane so that the handle is facing horizontal or perpendicular to the direction of the neck (Fig. 6-6, step 5). This instrument works opposite that of most ordinary instruments, such as hemostats. Squeezing the handles opens rather than closes the blades. This can be confusing the first time you use this instrument, and it is worth practicing before you need it in an emergency. If this instrument is not available in an emergency, Mayo scissors, a hemostat, or even the blunt end of a scalpel handle can be used to dilate the incision in the cricothyroid membrane.41
Dilate the incision vertically with the Trousseau dilator. Hold the handles of the Trousseau dilator with the nondominant hand and rotate the handle 90 degrees until the handle is vertical or parallel to the neck (Fig. 6-6, step 6). Perform this rotation because if the dilator is still horizontal, the blades of the dilator prevent passage of the tracheostomy tube into the trachea. Prepare the tracheostomy tube by testing the balloon, removing the inner cannula, and inserting the solid white obturator. While holding the dilator with the nondominant hand, take the tube in the dominant hand and insert it between the blades of the dilator until the flanges rest against the skin of the neck (Fig. 6-6, step 7). Keep the thumb on the obturator throughout the procedure. Carefully remove the Trousseau dilator (Fig. 6-6, step 8). Remove the obturator and insert the inner cannula. Inflate the balloon (Fig. 6-6, step 9). Remove the tracheal hook while being especially careful to not puncture the cuff.42,43
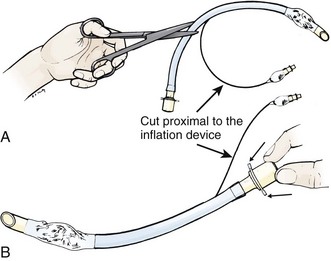
If a tracheostomy tube is not available or if there is difficulty placing the tracheostomy tube into the opening in the cricothyroid membrane, try using a 6-0 cuffed ET tube cut to a shorter length. The ID/OD ratios of tracheostomy tubes are comparable to those of ET tubes. Use of a gum elastic bougie may facilitate and even hasten placement of an ET tube through the cricothyroid membrane into the trachea.44 The advantage of using the bougie is that you can get immediate confirmation that the device is inside the trachea because of the “washboard” vibration that the curved tip makes as it contacts the tracheal rings.45 Modify the ET tube by cutting the distal end and replacing the adapter to the cut end (Fig. 6-8). Be careful to not cut the pilot balloon or inflation port. If the ET tube is shortened, it is less likely to kink once it is attached to a ventilator. Advance the ET tube only about 5 cm from the tip to avoid main stem intubation. Keep in mind that standard ET tubes do not have centimeter markings at the distal end. Inserting the ET tube so that the distal cuff is about 2 cm beyond the cricothyroid membrane usually ensures proper placement.
Confirm proper placement in the same manner as with ET tube placement: end-tidal CO2, bilateral chest movement, and breath sounds. Secure the tracheostomy tube with a circumferential tie around the neck or with sutures (Fig. 6-6, step 10). Order a postprocedure portable chest radiograph.
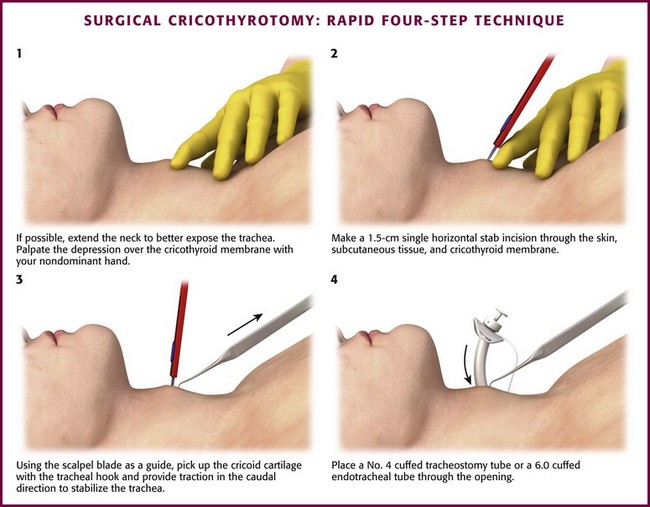
Rapid Four-Step Technique (Brofeldt)
Brofeldt and colleagues46 developed a rapid four-step technique (RFST) to decrease the amount of time required to establish an airway and reduce complications of hypoxia. It combines aspects of traditional cricothyroidotomy and ET intubation. For right hand–dominant operators, stand at the bedside to the patient’s left. Palpate the depression over the cricothyroid membrane with the nondominant hand (Fig. 6-9, step 1). With the dominant hand, make a single horizontal stab incision with a No. 20 scalpel blade approximately 1.5 cm in length through the skin, subcutaneous tissue, and cricothyroid membrane (Fig. 6-9, step 2). With the scalpel blade as a guide, pick up the cricoid cartilage with the tracheal hook and provide traction in the caudal direction to stabilize the trachea (Fig. 6-9, step 3). Place a No. 4 cuffed tracheostomy tube or a 6-0 cuffed ET tube through the opening (Fig. 6-9, step 4).
Because this technique omits dilating the stoma with the Trousseau dilator, it may be more difficult to pass a tracheostomy tube. A gum elastic bougie, using the Seldinger technique, may assist in this step.46
Bair and colleagues47 modified this technique further by introducing a new device called a “Bair Claw” to replace the tracheal hook. The technique is similar to the four-step method except for positioning the operator at the head of the bed instead of the patient’s side and the use of a double-hook device rather than a single hook. By replacing the single hook with the double hook, they found a decrease in the incidence of cricoid ring fractures in cadavers (Fig. 6-10).

Figure 6-10 Bair Claw.
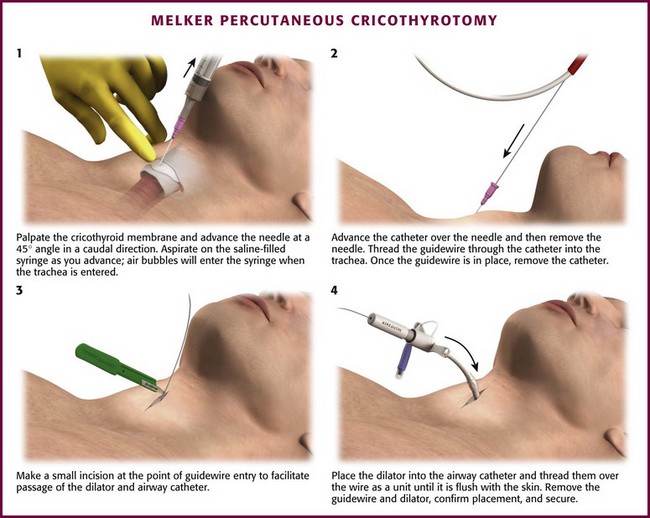
Melker Percutaneous Cricothyrotomy Technique
Preparation for this technique is similar to that for the other techniques. Palpate the cricothyroid membrane with the nondominant hand. With the dominant hand, attach the needle to the syringe and insert it through the cricothyroid membrane pointing caudally at a 45-degree angle relative to the skin surface (Fig. 6-11, step 1). Be careful to not advance the needle too far because this may result in perforation of the posterior aspect of the trachea. To help recognize when the trachea has been entered, place a small amount of saline in the syringe before the procedure. Apply gentle negative pressure while advancing the syringe. When the membrane is pierced and the trachea is entered, air will be aspirated into the syringe and air bubbles will appear in the saline.
When the needle is in the trachea, pull the syringe and needle back and advance the flexible TFE catheter through the distal end of the trachea to its hub. If the needle does not have an overlying catheter, leave the needle in place and remove the syringe. Thread the guidewire through the needle or the catheter (Fig 6-11, step 2). Once the guidewire is placed securely in the trachea, remove the needle or catheter. With a disposable No. 15 scalpel, make a small incision in the skin at the point of guidewire entry to facilitate passage of the dilator and airway catheter (Fig. 6-11, step 3).
Place the gray-tipped dilator into the airway catheter and thread it over the wire as one unit (Fig. 6-11, step 4). Once it is through the skin and into the trachea, advance the airway catheter to its hub until it is flush against the neck. Remove the guidewire and dilator. Confirm placement in the trachea by standard methods. Secure the kit in place with “trach tape.”
Melker kits on the market differ with respect to airway catheter ID and whether the airway catheter is cuffed. Some kits do not contain a needle with an overlying catheter.48
Complications
Surgical cricothyrotomy is performed infrequently and usually under circumstances that are inherently chaotic. These patients often have confounding medical issues, as well as high morbidity and mortality rates. Evaluation of short- and long-term complications in this population is also difficult.49
Regardless of which technique is used, surgical cricothyrotomy has been studied to assess the periprocedure and short-term complications that occur with significant frequency. Acute complication rates have been reported to be between 8.7%50 and 40%.36 The most frequent complications are uncontrollable bleeding and misplacement of the tube.35,51 Most bleeding is from small superficial vessels that can be controlled, but significant bleeding can also occur as a result of the procedure. The cricoid arteries branch from the superior thyroid arteries and anastomose at the anterior superior aspect of the cricothyroid membrane. The laterally running superior thyroid arteries are more often damaged when the initial incision is broad and horizontal. To prevent hemorrhage from these vessels, make the initial skin incision longitudinally as in the traditional technique and maintain careful awareness of the landmarks.52 When making the horizontal incision in the cricothyroid membrane, avoid the cricoid artery by incising the membrane at its inferior aspect. Misplacement of the tracheostomy or ET tube during cricothyrotomy is a concern, just as esophageal intubation is a concern with ET intubation. If the opening in the cricothyroid membrane is not carefully stabilized during the procedure, the tube may inadvertently be inserted into subcutaneous tissue. This complication can be recognized by the presence of subcutaneous emphysema when attempting to ventilate the patient. It is essential to recognize this immediately to prevent the development of hypoxia and obliteration of anatomic landmarks. In addition, failure to detect end-tidal CO2 and absence of breath sounds by auscultation should alert the physician to a misplaced tube. If suspected, remove the tube and reassess the airway. A misplaced tube can pass into any location other than through the cricothyroid membrane, but the most crucial locations are those that do not enter the airway because this will lead to hypoxia and death if not recognized.
Many other occult complications have been reported less frequently or have been described in case reports, such as main stem bronchial intubation,53 laryngotracheal injury,54 tension pneumothorax,55 and obstruction of the tracheostomy tube with blood or secretions.56 Slobodkin and colleagues57 reported one case of retrograde pharyngeal intubation (Box 6-3).
Chevalier Jackson’s 1921 report58 highlighted the concern that subglottic stenosis was a major and frequent complication of cricothyrotomy. It was later refuted by Brantigan and Grow’s 1976 study,34 which reported not only an overall complication rate of just 6.1% but also no occurrence of chronic subglottic stenosis as a long-term complication. Since the publication of this latter report, numerous other studies have corroborated their findings that chronic subglottic stenosis is an infrequent long-term complication of surgical cricothyrotomy.59–63 Factors that increase the likelihood of development of subglottic stenosis include concurrent laryngotracheal pathology, prolonged time until decannulation, old age, and diabetes.64,65
Long-term complications resulting in “minor airway problems” have been reported more frequently than subglottic stenosis.66 Of these complications, subjective voice change is the most frequently reported.67 Other reported complications include difficulty swallowing, subjective shortness of breath, wound infections, and “noisy breathing.”68
To decrease the morbidity and mortality associated with prolonged hypoxia and other factors inherent in an airway emergency, researchers have attempted to determine whether any of the techniques is superior with regard to complication rate and time needed to secure the airway. When comparing Brofeldt and colleagues’ RFST with the traditional five-step technique, Davis and colleagues54 found an increased incidence of cricoid ring fracture when the single hook was used for caudal traction on the cricoid cartilage and concluded that the traditional technique produced a lower complication rate. A study by Holmes and coworkers40 in which the same two techniques were performed by inexperienced medical students and residents on human cadavers concluded that the single-hook RFST was executed significantly faster than the traditional technique. They noted that there were more complications with the RFST but that the difference in complication rates failed to reach statistical significance. Davis and colleagues69 revisited this comparison in a later study and replaced the single hook in the RFST with the double-hooked Bair Claw. The revised study showed that the airway could be secured faster with the RFST and that the complication rate was comparable; they also observed that the Bair Claw did not cause any fractures of the cricoid cartilage. Bair and colleagues’ retrospective report70 of ED cricothyrotomy showed a lower complication rate with the RFST than with the traditional technique.
Consensus cannot be drawn from the literature comparing the traditional method with the percutaneous Seldinger (Melker kit) method. Some studies show no difference in time to ventilation or complication rate when the traditional technique is compared with the Seldinger technique.71 Some studies report that the surgical method is faster than the Seldinger method,72–76 whereas others conclude the opposite.77,78
Success Rates
Success rates for first-attempt ET intubation in the ED are quite high (90% success for all ED intubators, including residents; 98% success rate if an attending), with the “rescue” cricothyrotomy rate reported to be just 0.7% according to the National Emergency Airway Registry.3 A study including more than 6000 trauma patients reported a 0.3% cricothyrotomy rate in those requiring airway management within the first hour after arrival.79 In pediatric patients, the success rate with the first attempt for all ED intubators is slightly less at 85%, with rescue cricothyrotomy performed less than 1% of the time (1 of 156 patients).80 As an overview, few emergency physicians have the opportunity to gain extensive experience with surgical airways, and no standards of care have been developed that define the exact role of cricothyrotomy in clinical practice. In reality, it is difficult to successfully perform an emergency surgical airway, and even with proper training and standard experience, not all attempts with this technically difficult procedure will be successful. Although the reported success rate for cricothyrotomy has been quite high (89% to 100%) in most studies,* one study found only a 62.5% success rate.82 In a community hospital setting, the rather optimistic success rate reported from trauma centers probably cannot be duplicated. In one ED study, the incidence of failed cricothyrotomy (e.g., tube misplacement into the pretracheal space or failed attempts) was 3.6%,70 with earlier ED studies being in the 7.9% to 10% range.35,36 In the prehospital setting, the reported failure rates are 6% to 12% for paramedics,24,49,81 0% for physicians,60 and 0% to 38% for air transport medics.82,83 In a cadaver model, the first-time performance of cricothyrotomy by intensive care unit clinicians, versus standard surgical cricothyrotomy with the Seldinger technique, resulted in successful tracheal placement in only 70% with the standard technique and 60% with the Seldinger technique.71 In an animal model, paramedics had a 90.9% success rate with a percutaneous technique and a 100% success rate with the open surgical technique.73
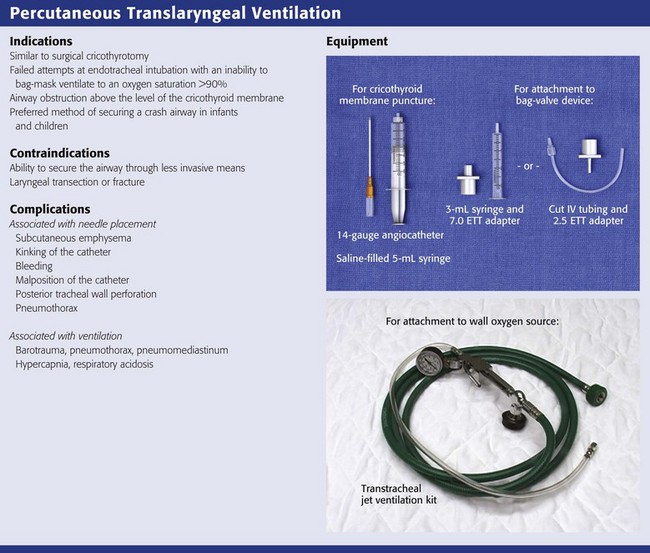
Percutaneous Translaryngeal Ventilation
PTLV is a procedure in which oxygen is delivered through a 12- to 14-gauge catheter inserted through the cricothyroid membrane via needle cricothyrotomy. Needle cricothyrotomy does not differ greatly from the Seldinger technique variation of surgical cricothyrotomy. Administer oxygen by bag insufflation for pediatric patients younger than 5 years, but use jet ventilation in older children and adults. For jet ventilation, supply the oxygen from a high-flow source and deliver it to the percutaneous translaryngeal catheter through a relatively small-caliber tube. The method for controlling jet ventilation has evolved over recent years. The initial use of continuous oxygen flow provided adequate oxygenation but not ventilation,84 so the technique has advanced to giving shorter bursts of oxygen followed by a longer passive exhalation to resemble a more physiologic respiratory state.
Indications and Contraindication
The indications for and contraindications to needle cricothyrotomy with PTLV are similar to those for surgical cricothyrotomy. Indications include failed attempts at ET intubation, inability to bag-mask ventilate to an oxygen saturation greater than 90%, or airway obstruction above the level of the cricothyroid membrane. Based on the operator’s experience, needle cricothyrotomy may be relatively indicated over surgical cricothyrotomy in adult patients. Much of the otolaryngology literature supports the use of PTLV as a means of nonemergency ventilation during head and neck surgery because the smaller ventilation catheter provides a relatively unobstructed field in which to work.85–87 In an emergency airway situation, needle cricothyrotomy is a successful bridge to establishing an airway via the ET route.88 Case reports describe PTLV to be relatively indicated over the more invasive surgical cricothyrotomy when ET intubation has failed as a result of copious oropharyngeal secretions. Providing temporary ventilation through the needle catheter may allow sufficient time to clear the upper airway of secretions or obstructions and give the operator more time to establish ET intubation.89,90
Surgical cricothyrotomy is contraindicated in infants and young children. The contraindication arises from the fact that the cricothyroid membrane is too small to insert a tracheostomy tube and there is a significant risk for injury to surrounding structures. Therefore, needle cricothyrotomy is the preferred method of securing the airway in crash airway situations in infants and young children.91
An absolute contraindication to needle cricothyrotomy is the ability to secure the airway without difficulty through less invasive means.92 Similar to surgical cricothyrotomy, needle cricothyrotomy is contraindicated in cases of laryngotracheal transection or fracture because the airway needs to be established below this level.31 It has been suggested that in cases of complete upper airway obstruction, needle cricothyrotomy is relatively contraindicated in comparison to surgical cricothyrotomy. This concern, which is debatable, is due to the fact that the PTLV catheter theoretically does not permit adequate expiration volumes and results in hypercapnia and barotrauma.93
Equipment
Commercial kits are available, but a standard 12- or 14-gauge Angiocath attached to a 3- or 5-mL syringe can be used to make the puncture through the cricothyroid membrane. The catheter can be left in place to serve as the conduit for oxygen delivery. The larger the diameter of the catheter, the greater the oxygen flow, depending on the method of oxygen delivery.94 Commercial catheters such as wire-coiled nonkinking catheters and fenestrated catheters are available as part of prearranged kits (Fig. 6-12). Larger-caliber, 3.0- to 4.0-mm-ID percutaneous tracheal catheter devices are also available.

Figure 6-12 ENK oxygen flow modulator set available as separate kit. (Courtesy of Cook Critical Care, Bloomington, IN.)
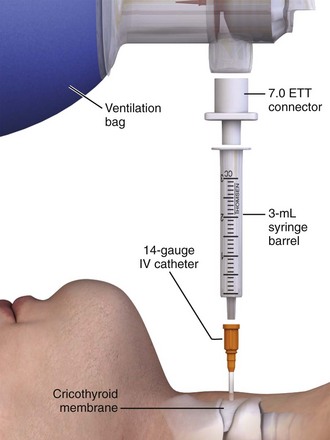
There are two different basic means and therefore armories of equipment to choose from to deliver oxygen through the transtracheal catheter. One method uses a standard ventilation bag to supply oxygen through the needle. This requires the constant effort of manual bag insufflation as long as the patient is being oxygenated and ventilated. Attach the bag to the adapter of a 7.0-mm ET tube and insert it into the back of a plungerless 3-mL syringe connected to the translaryngeal catheter (Fig. 6-13). Alternatively, attach the bag directly to the catheter with the adapter of a 3.5-mm pediatric ET tube.95 An inherent problem with this setup is the rigidity of the system. Although the translaryngeal catheter itself is flexible, there is no flexibility from the hub of the catheter to the bag. Thus, slight movements of the bag relative to the patient may cause dislodgment of the catheter. To ameliorate this obstacle, connect standard intravenous infusion tubing directly to the translaryngeal catheter and attach the distal cut end of a 2.5-mm ET tube to the bag.
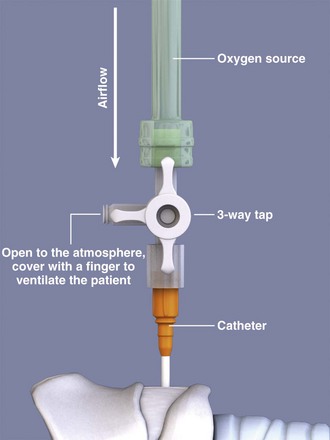
In an alternative method, supply oxygen from a standard 50-psi wall source. Connect the high-pressure oxygen tubing to the wall source. Then connect the oxygen tubing to a manual on/off valve that is connected to the hub of the catheter. The on/off valve controls the inspiratory-to-expiratory ratio. This valve can be a separate component that is pushed down and released, the third arm of a three-way stopcock open to the atmosphere (Fig. 6-14), or holes placed at the end of the oxygen tubing. A pressure gauge connected to a hand-triggered jet injector may also be used to control the amount of air pressure reaching the catheter96 (Fig. 6-15). Commercial kits are available that contain prepackaged systems already assembled. Otherwise, assemble the apparatus in the ED. In an emergency situation, it is unlikely that one would be able to assemble an apparatus for PTLV from individual components in a timely manner. If a prepackaged PTLV kit is not available, prepare the appropriate components from the ED ahead of time and place them with other airway supplies for easy access.
Procedure
Similar to the needle insertion technique used for guidewire-assisted surgical cricothyrotomy, locate the cricothyroid membrane with the nondominant hand. Locate the thyroid cartilage and cricoid cartilage and palpate the cricothyroid membrane in the depression between the two while keeping in mind that this depression will be proportionately smaller in children (Fig. 6-16, step 1).
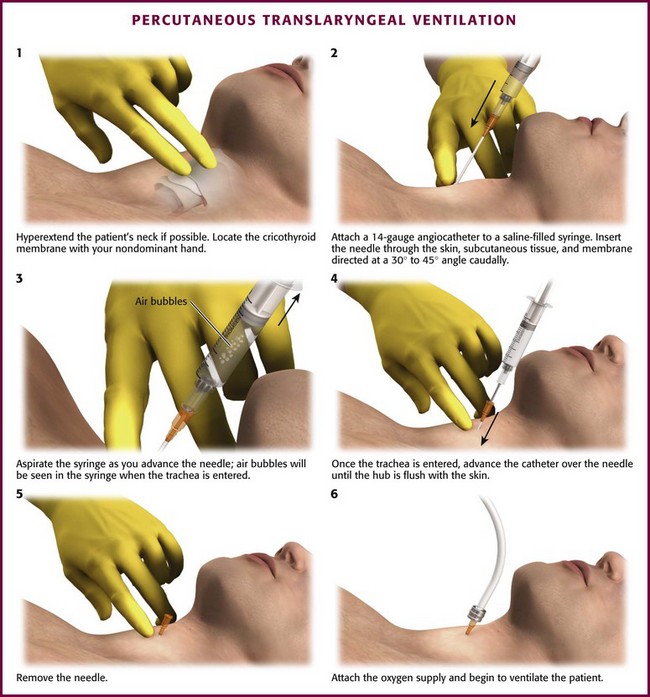
Figure 6-16 Percutaneous translaryngeal ventilation.
Attach a 12- to 14-gauge Angiocath to a 3- or 5-mL syringe filled with 1 to 2 mL of saline or lidocaine. Once the cricothyroid membrane has been located, insert the catheter through the overlying skin, subcutaneous tissue, and membrane directed at a 30- to 45-degree angle caudally (Fig. 6-16, step 2). While doing so, aspirate gently with the syringe. The cricothyroid membrane has been pierced and the airway entered when air bubbles are seen in the fluid or there is an increase in the ease of air aspiration (Fig. 6-16, step 3). Once through the membrane, hold the needle in place, advance the catheter to the hub, and then remove the needle (Fig 6-16, steps 4 and 5). Hold the catheter by hand until the oxygen supply is connected and appropriate placement is confirmed (Fig. 6-16, step 6). Make sure that the hub of the catheter is flush against the skin to avoid an air leak and then secure it with a circumferential tie around the neck. To prevent the tube from being dislodged, keep one hand on the hub of the catheter until the entire procedure is completed and the airway is secured.
Oxygen can be supplied to the catheter through several different conduits. With the resuscitation bag setup, manually ventilate the lungs through the catheter by squeezing and releasing the bag. When coupled with a 14-gauge Angiocath, ventilation with a resuscitation bag produces low maximal tidal volumes, approximately 100 mL per 1 second of inspiratory time in one study.97 Children, especially those younger than 5 years, have small total lung capacities and need smaller tidal volumes. In these cases, use the bag instead of the jet ventilator. To use this setup, control the volume of air inspired and adjust it breath by breath based on chest wall motion and pulse oximetry. This method is not appropriate for adults because the operator cannot provide adequate tidal volumes and allow enough time for exhalation.98,99
If using high-flow oxygen supplied from a wall source, attach the oxygen tubing to the wall source and secure the distal end of the tubing apparatus to the hub of the translaryngeal catheter. The flow rate recommended for children is 1 L/min per year of age, with titration upward in increments of 1 L/min based on chest wall movement.100 Most wall-mounted oxygen flowmeters have a maximum flow rate marked at 15 L/min. Pressures generated at this flow rate have been shown to be inadequate to sustain ventilation in adults.101,102 To provide the additional pressure necessary to ventilate an adult, open the oxygen flowmeter to full output.103 Ventilate the patient by alternating between allowing and inhibiting airflow through the catheter. This is done by occluding and then releasing the hole or holes if using a stopcock or the ENK oxygen flow modulator or by pushing and releasing a trigger if using this type of modulator. Watch for chest wall rise and fall, and make sure to allow enough time for exhalation before the next cycle. A pressure gauge, if attached, can help guide inspiration time.
Complications
Complications reported with needle cricothyrotomy are similar to those associated with surgical cricothyrotomy: bleeding, misplacement of the catheter, subcutaneous emphysema, and pneumothorax.104,105 Complications more specific to needle cricothyrotomy include catheter kinking106 and perforation of the posterior aspect of the trachea.107
One would assume that a translaryngeally placed catheter would not afford any airway protection against aspiration because the diameter of the catheter is not nearly large enough to occlude the lumen of the trachea. A few studies, though, have shown a decreased rate of aspiration in dogs that were ventilated with PTLV versus control animals who were not ventilated, thus suggesting some airway protection with this mode of ventilation.108,109
The potential complications more specific to PTLV than to ventilation through a tracheostomy tube stem from the idea that especially in cases of complete upper airway obstruction, egress of inspired gas is limited through the relatively small translaryngeal catheter. It has been reported that PTLV inevitably causes retention of CO2 in adults. This leads to poor ventilation despite adequate oxygenation. This assumption may be a remnant of earlier oxygenation techniques in which continuous low-flow “apneic oxygenation” was used without ventilation.110 Many animal studies have shown that adequate ventilation, normal blood pH, and normal arterial CO2 partial pressure can be maintained with PTLV for 30 or even 60 minutes.111–116 Factors that seem to improve ventilation are increased expiratory time117 and a high-flow oxygen source.118 Even with partial or nearly complete oropharyngeal obstruction, adequate ventilation has been achieved.119,120 Unfortunately, none of these studies looked at ventilation for extended periods. Barotrauma is a significant risk associated with PTLV and occurs when upper airway obstruction is preventing air from being exhaled. This causes an increase in lung volume and pressure and leads to lung injury.122,123 Lenfant and colleagues124 found that use of a lower respiratory rate and the ENK oxygen flow modulator versus the Manujet decreases pulmonary pressure, which theoretically reduces the likelihood of barotrauma. The ENK oxygen flow modulator may also be superior to a three-way stopcock for similar reasons.125 Use of a bidirectional valve or an expiratory ventilation assistance ejector device has been shown to improve ventilation dynamics and decrease the complications associated with PTLV in patients with complete upper airway obstruction126,127 (Box 6-4).
Conclusion
Researchers have attempted to delineate which method of gaining emergency airway access is superior by comparing all techniques across the spectrum from traditional surgical cricothyrotomy to needle cricothyrotomy to commercially available kits such as the QuickTrack. Given the variety of equipment and techniques to choose from and the advantages and disadvantages reported about each throughout the literature, it would be difficult for an inexperienced physician to know which to choose in a critical situation. Aside from being familiar with the equipment available in the ED, research shows that overall success rates increase if physicians are trained in simulated situations before an actual airway emergency.126,127
References
1. Bair, AE, Filbin, MR, Kulkarni, RG, et al. The failed intubation attempt in the emergency department: analysis of prevalence, rescue techniques, and personnel. J Emerg Med. 2002;23:131.
2. Sakles, JC, Laurin, EG, Rantapaa, AA, et al. Airway management in the emergency department: a one-year study of 610 tracheal intubations. Ann Emerg Med. 1998;31:325.
3. Sagarin, MJ, Barton, ED, Yi-Mei, C, et al. Airway management by US and Canadian emergency medicine residents: a multicenter analysis of more than 6,000 endotracheal intubations. Ann Emerg Med. 2005;46:328.
4. Hawkins, ML, Shapiro, MB. Emergency cricothyrotomy: a reassessment. Am Surg. 1995;61:52.
5. Greene, AE, Bair, AE. The impact of gum elastic bougie on emergency department cricothyrotomy rate. Ann Emerg Med. 2006;48:S28.
6. Berkow, LC. Need for emergency surgical airway reduced by a comprehensive difficult airway program. Anesth Analg. 2009;109:1860.
7. Simon, RR. Emergency tracheotomy in patients with massive neck swelling. Emerg Med Clin North Am. 1989;7:95.
8. Simon, RR, Brenner, BE. Emergency cricothyroidotomy in the patient with massive neck swelling: I: anatomical aspects. Crit Care Med. 1983;11:114.
9. Simon, RR, Brenner, BE, Rosen, MA. Emergency cricothyroidotomy in the patient with massive neck swelling: II: clinical aspects. Crit Care Med. 1983;11:119.
10. Netter, FJ. Head and neck. In: Hansen JT, ed. Atlas of Human Anatomy. 3rd ed. Peterboro, NJ: ICON Learning Systems; 2003:59.
11. Gray, H. The organs of voice and respiration. In: Pickering TP, Howden R, eds. Gray’s Anatomy. 15th ed. New York: Portland House; 1977:955.
12. Levitan, RM. Pediatric laryngoscopy. In: Levitan RM, ed. The Airway-Cam Guide to Intubation and Practical Emergency Airway Management. Wayne, PA: Airway Cam Technologies; 2004:201.
13. Navsa, N, Tossel, G, Boon, JM. Dimensions of the neonatal cricothyroid membrane—how feasible is a surgical cricothyrotomy. Paediatr Anaesth. 2005;15:402.
14. Butler, KH, Clyne, B. Management of the difficult airway: alternative airway techniques and adjuncts. Emerg Med Clin North Am. 2003;21:259.
15. Jacobson, S. Upper airway obstruction. Emerg Med Clin North Am. 1989;7:205.
16. Combes, X. Cricothyrotomy in emergency context: assessment of a cannot intubate cannot ventilate scenario. Ann Fr Anesth Reanim. 2011;30:113.
17. Samsoon, GL, Young, JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987;42:487.
18. Mallampati, SR. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985;32:429.
19. Reed, MJ, Dunn, MJG, McKeown, DW. Can an airway assessment score predict a difficult intubation in the emergency department? Emerg Med J. 2005;22:99.
20. Soyuncu, S. Determination of difficult intubation in the ED. Ann J Emerg Med. 2009;8:905.
21. Langeron, O, Masso, E, Huraux, C, et al. Prediction of difficult mask ventilation. Anaesthesia. 2000;92:1229.
22. Orebaugh, SL. Difficult airway management in the emergency department. J Emerg Med. 2002;22:31.
23. Gerich, TG, Schmidt, U, Hubrich, V, et al. Prehospital airway management in acutely injured patient. The role of surgical cricothyrotomy revisited. J Trauma Inj Infect Crit Care. 1998;45:312.
24. Fortune, JB, Judkins, DG, Scanzaroli, D, et al. Efficacy of prehospital surgical cricothyrotomy in trauma patients. J Trauma Inj Infect Crit Care. 1997;42:832.
25. Caplan, RA, Benumof, JL, Berry, FA, et al. Practice guidelines for management of the difficult airway. Anesthesiology. 1993;78:597.
26. Walls, RM. The emergency airway algorithm. In: Walls RM, ed. Manual of Emergency Airway Management. 2nd ed. Philadelphia: Lippincott, Williams & Wilkins; 2004:8–21.
27. Parmet, JL, Colonna-Romano, JC, Horrow, JC, et al. The laryngeal mask airway reliably provides rescue ventilation in cases of unanticipated difficult tracheal intubation along with difficult mask. Anesth Analg. 1998;87:661.
28. Strange, GR, Niederman, LG. Surgical cricothyrotomy. In: Henretig FM, King C, eds. Textbook of Pediatric Emergency Procedures. Baltimore: Williams & Wilkins; 1997:351.
29. Gens, DR. Surgical airway management. In: Tintinalli JE, Kelen GD, Stapczynski JS, eds. Emergency Medicine: A Comprehensive Study Guide. 6th ed. New York: McGraw-Hill; 2004:119.
30. Walls, RM, Airway. Rosen’s Emergency Medicine: Concepts and Clinical Practice, 6th ed. Marx, JA, Hockberger, RS, Walls, RM, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice, Philadelphia, Mosby, 2006;Vol. 1:2.
31. Stewart, CE. Surgical airways. In: Stewart CE, ed. Advanced Airway Management. Upper Saddle River, NJ: Pearson Education, Inc.; 2002:125.
32. Covidien product information. Available at http://www.covidien.com/.
33. Gerling, MC, Davis, DP, Hamilton, RS, et al. Effect of surgical cricothyrotomy on the unstable cervical spine in a cadaver model of intubation. J Emerg Med. 2001;20:1.
34. Brantigan, CO, Grow, JB. Cricothyroidotomy: elective use in respiratory problems requiring tracheotomy. J Thorac Cardiovasc Surg. 1976;71:72.
35. McGill, J, Clinton, JE, Ruiz, E. Cricothyrotomy in the emergency department. Ann Emerg Med. 1982;11:361.
36. Erlandson, MJ, Clinton, JE, Ruiz, E, et al. Cricothyrotomy in the emergency department revisited. J Emerg Med. 1989;7:115.
37. Vissers, RJ, Bair, AE. Surgical airway techniques. In: Walls RM, ed. Manual of Emergency Airway Management. 2nd ed. Philadelphia: Lippincott, Williams & Wilkins; 2004:158.
38. Elliott, DSJ. Accuracy of surface landmark identification for cannula cricothyrotomy. Anaesthesia. 2010;65:889.
39. Nicholls, SE. Bedside sonography by emergency physicians for the rapid identification of landmarks relevant to cricothyrotomy. Am J Emerg Med. 2008;26:852.
40. Holmes, JF, Panacek, EA, Sakles, JC, et al. Comparison of 2 cricothyrotomy techniques: standard method versus rapid 4-step technique. Ann Emerg Med. 1998;32:442.
41. Bramwell, KJ, Davis, DP, Cardill, TV, et al. Use of the Trousseau dilator in cricothyrotomy. J Emerg Med. 1999;17:433.
42. Narrod, JA, Moore, EE, Rosen, P. Emergency cricothyrotomy—technique and anatomical consideration. J Emerg Med. 1985;2:443.
43. Mace, SE. Cricothyrotomy. J Emerg Med. 1988;6:309.
44. Hill, C. Cricothyrotomy technique using gum elastic bougie is faster than standard technique: a study of emergency medicine residents and medical students in an animal lab. Acad Emerg Med. 2010;17:666.
45. Braude, D. The bougie-aided cricothyrotomy. Air Med J. 2009;28:191.
46. Brofeldt, BT, Panacek, EA, Richards, JR. An easy cricothyrotomy approach: the Rapid Four-Step Technique. Acad Emerg Med. 1996;3:1060.
47. Bair, AE, Laurin, EG, Karchin, A, et al. Cricoid ring integrity: implications for cricothyrotomy. Ann Emerg Med. 2003;41:331.
48. Melker Emergency Cricothyrotomy Catheter Kit product information. Bloomington, IN: Cook Medical, Inc. Available at http://www.cookmedical.com.
49. Spaite, DW, Joseph, M. Prehospital cricothyrotomy: an investigation of indications, technique, complications, and patient outcome. Ann Emerg Med. 1990;19:279.
50. Boyle, MF, Hatton, D, Sheets, C. Surgical cricothyrotomy performed by air ambulance flight nurses: a 5-year experience. J Emerg Med. 1993;11:41.
51. Issacs, JH, Pederson, AD. Emergency cricothyrotomy. Am Surg. 1997;63:364.
52. American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269.
53. Gerich, TG, Schmidt, U, Hubrich, V, et al. Prehospital airway management in the acutely injured patient. The role of surgical cricothyrotomy revisited. J Trauma. 1998;45:312.
54. Davis, DP, Bramwell, KJ, Vilke, GM, et al. Cricothyrotomy technique: standard versus rapid four-step approach. J Emerg Med. 1999;17:17.
55. Engoren, M, de St Victor, P. Tension pneumothorax and contralateral presumed pneumothorax from endotracheal intubation via cricothyroidotomy. Chest. 2000;118:1833.
56. Nugent, WL, Rhee, KJ, Wisner, DH. Can nurses perform surgical cricothyrotomy with acceptable success and complication rates? Ann Emerg Med. 1991;20:367.
57. Slobodkin, D, Topliff, S, Raife, JH. Retrograde intubation of the pharynx: an unusual complication of emergency cricothyrotomy. Ann Emerg Med. 1992;21:220.
58. Jackson, C. High tracheotomy and other errors. The chief causes of chronic laryngeal stenosis. Surg Gynecol Obstet. 1921;32:392.
59. Isaacs, JH. Emergency cricothyrotomy. Long-term results. Am Surg. 2001;67:346.
60. Miklus, RM, Elliott, C, Snow, N. Surgical cricothyrotomy in the field: experience of a helicopter transport team. J Trauma. 1989;29:506.
61. Boyd, AD, Romita, MC, Conlon, AA. A clinical evaluation of cricothyroidotomy. Surg Gynecol Obstet. 1979;148:365.
62. van Hasselt, EJ, Bruining, HA, Hoeve, LJ. Elective cricothyroidotomy. Intensive Care Med. 1985;11:207.
63. McDowell, DE. Cricothyroidostomy for airway access. South Med J. 1982;75:282.
64. Kuriloff, DB, Setzen, M, Portnoy, W, et al. Laryngotracheal injury following cricothyroidotomy. Laryngoscope. 1989;99:125.
65. Brantigan, CO, Grow, JB. Subglottic stenosis after cricothyroidotomy. Surgery. 1982;91:217.
66. Gleeson, MJ, Pearson, RC, Armistead, S, et al. Voice changes following cricothyroidotomy. J Laryngol Otol. 1984;98:1015.
67. Cole, RR, Aguilar, EA. Cricothyroidotomy versus tracheotomy: an otolaryngologist’s perspective. Laryngoscope. 1988;98:131.
68. Salvino, CK, Dries, D, Gamelli, R, et al. Emergency cricothyroidotomy in trauma victims. J Trauma. 1993;34:503.
69. Davis, DP, Bramwell, KJ, Hamilton, RS, et al. Safety and efficacy of the Rapid Four-Step Technique for cricothyrotomy using a Bair Claw. J Emerg Med. 2000;19:125.
70. Bair, AE, Panacek, EA, Wisner, DH, et al. Cricothyrotomy: a 5-year experience at one institution. J Emerg Med. 2003;24:151.
71. Eisenburger, P, Laczika, K, List, M, et al. Comparison of conventional surgical versus Seldinger technique emergency cricothyrotomy performed by inexperienced clinicians. Anesthesiology. 2000;92:687.
72. Chan, TC, Vilke, GM, Bramwell, KJ, et al. Comparison of wire-guided cricothyrotomy versus standard surgical cricothyrotomy technique. J Emerg Med. 1999;17:957.
73. Keane, MF, Brinsfield, KH, Dyer, KS, et al. A laboratory comparison of emergency percutaneous and surgical cricothyrotomy by prehospital personnel. Prehosp Emerg Care. 2004;8:424.
74. Sulaiman, L, Tighe, SQ, Nelson, RA. Surgical vs. wire-guided cricothyroidotomy: a randomized crossover study of cuffed and uncuffed tracheal tube insertion. Anaesthesia. 2006;62:565.
75. Johnson, DR, Dunlap, A, McFeeley, P, et al. Cricothyrotomy performed by prehospital personnel: a comparison of two techniques in a human cadaver model. Am J Emerg Med. 1993;11:207.
76. Schober, P. Emergency cricothyrotomy—a comparative study of different techniques in human cadavers. Resuscitation. 2009;80:204.
77. Schaumann, N, Lorenz, V, Schellongowski, P, et al. Evaluation of Seldinger technique emergency cricothyroidotomy versus standard surgical cricothyroidotomy in 200 cadavers. Anesthesiology. 2005;102:7.
78. Mariappa, V. Cricothyrotomy: comparison of three different techniques on a porcine airway. Anaesth Intensive Care. 2009;37:961.
79. Stephens, CT, Kahntroff, S, Dutton, RP. The success rate of emergency endotracheal intubation in trauma patients: a 10-year experience at a major trauma referral center. Anesth Analg. 2009;109:866.
80. Sagarin, MJ, Chiang, V, Sakles, JC, et al. Rapid sequence intubation for pediatric emergency airway management. Pediatr Emerg Care. 2002;18:417.
81. Jacobson, LE, Gomez, G, Sobieray, RJ, et al. Surgical cricothyrotomy in trauma patients: analysis of its use by paramedics in the field. J Trauma. 1996;41:15.
82. Robinson, KJ, Katz, R, Jacobs, LM. A 12-year experience with prehospital cricothyrotomies. Air Med J. 2001;20:27.
83. McIntosh, SE, Swanson, ER, Barton, ED. Cricothyrotomy in air medical transport. J Trauma. 2008;64:1543.
84. Okamoto, K, Morioka, T. Transtracheal O2 insufflation (TOI) as an alternative method of ventilation during cardiopulmonary resuscitation. Resuscitation. 1990;20:253.
85. Monnier, PH, Ravussin, P, Savary, M, et al. Percutaneous transtracheal ventilation for laser endoscopic treatment of laryngeal and subglottic lesions. Clin Otolaryngol. 1988;13:209.
86. Gulleth, Y, Spiro, J. Percutaneous transtracheal jet ventilation in head and neck surgery. Arch Otolaryngol Head Neck Surg. 2005;131:886.
87. Layman, PR. Transtracheal ventilation in oral surgery. Ann R Coll Surg Engl. 1983;65:318.
88. Patel, RG. Percutaneous transtracheal jet ventilation: a safe, quick, and temporary way to provide oxygenation and ventilation when conventional methods are unsuccessful. Chest. 1999;116:1689.
89. Chandradeva, K, Palin, C, Ghosh, SM, et al. Percutaneous transtracheal jet ventilation as a guide to tracheal intubation in severe upper airway obstruction from supraglottic oedema. Br J Anaesth. 2005;94:683.
90. McHugh, R. Transtracheal jet ventilation in the management of the difficult airway. Anaesth Intensive Care. 2007;35:406.
91. Luten, RC, Godwin, SA. Pediatric airway techniques. In: Walls RM, ed. Manual of Emergency Airway Management. 2nd ed. Philadelphia: Lippincott, Williams & Wilkins; 2004:228.
92. Mace, SE. Needle cricothyrotomy. Emerg Med Clin North Am. 2008;26:1085.
93. Jordan, RC, Moore, EE, Marx, JA, et al. A comparison of PTV and endotracheal ventilation in an acute trauma model. J Trauma. 1985;25:978.
94. Marr, JK, Yamamoto, LG. Gas flow rates through transtracheal ventilation catheters. Am J Emerg Med. 2004;22:264.
95. Chee-Fah, C, Tzong-Luen, W, Hang, C. Percutaneous transtracheal ventilation without a jet ventilator. Am J Emerg Med. 2003;21:507.
96. Yildiz, Y, Preussler, NP, Schreiber, J, et al. Percutaneous transtracheal emergency ventilation during respiratory arrest: comparison of the oxygen flow modulator with a hand-triggered emergency jet injector in an animal model. Am J Emerg Med. 2006;24:455.
97. Hooker, EA. Percutaneous transtracheal ventilation: resuscitation bags do not provide adequate ventilation. Prehosp Disaster Med. 2006;21:431.
98. Yealy, DM, Stewart, RD, Kaplan, RM. Myths and pitfalls in emergency translaryngeal ventilation: correcting misimpressions. Ann Emerg Med. 1988;17:690.
99. Yealy, DM, Plewa, MC, Stewart, RD. An evaluation of cannulae and oxygen sources for pediatric jet ventilation. Am J Emerg Med. 1991;9:20.
100. Advanced Life Support Group. Advanced Pediatric Life Support, 4th ed. London: BMJ Books; 2005.
101. Scarse, I, Woollard, M. Needle vs surgical cricothyroidotomy: a short cut to effective ventilation. Anaesthesia. 2006;61:962.
102. Bould, MD, Bearfield, P. Techniques for emergency ventilation through a needle cricothyrotomy. Anaesthesia. 2008;63:535.
103. Fassl, J. Pressures available for transtracheal jet ventilation from anesthesia machines and wall-mounted oxygen flow meters. Anesth Analg. 2010;110:94.
104. Russell, WC, Maguire, AM, Jones, GW. Cricothyroidotomy and transtracheal high frequency jet ventilation for elective laryngeal surgery. An audit of 90 cases. Anaesth Intensive Care. 2000;28:62.
105. Weymuller, EA, Pavlin, EG, Paugh, D, et al. Management of difficult airway problems with percutaneous transtracheal ventilation. Ann Otol Rhinol Laryngol. 1987;96:34.
106. Swartzman, S, Wilson, MA, Hoff, BH, et al. Percutaneous transtracheal jet ventilation for cardiopulmonary resuscitation: evaluation of a new jet ventilator. Crit Care Med. 1984;12:8.
107. Abbrecht, PH, Kyle, RR, Reams, WH, et al. Insertion forces and risk of complications during cricothyroid cannulation. J Emerg Med. 1992;10:417.
108. Yealy, DM, Plewa, MC, Reed, JJ, et al. Manual translaryngeal jet ventilation and the risk of aspiration in a canine model. Ann Emerg Med. 1990;19:1238.
109. Jawan, B, Cheung, HK, Chong, ZK, et al. Aspiration and transtracheal jet ventilation with different pressures and depths of chest compression. Crit Care Med. 1999;27:142.
110. Okamoto, K, Morioka, T. Transtracheal O2 insufflation (TOI) as an alternative method of ventilation during cardiopulmonary resuscitation. Resuscitation. 1990;20:253.
111. Cote, CJ, Eavey, RD, Todres, ID, et al. Cricothyroid membrane puncture: oxygenation and ventilation in a dog model using an intravenous catheter. Crit Care Med. 1988;16:615.
112. Tran, TP, Rhee, KJ, Schultz, HD, et al. Gas exchange and lung mechanics during percutaneous transtracheal ventilation in an unparalyzed canine model. Acad Emerg Med. 1998;5:320.
113. Stewart, RD. Manual translaryngeal jet ventilation. Emerg Med Clin North Am. 1989;7:155.
114. Carl, ME, Rhee, KJ, Schelegle, ES, et al. Pulmonary mechanics of dogs during transtracheal jet ventilation. Ann Emerg Med. 1994;24:1126.
115. Manoach, S, Corinaldi, C. Percutaneous transcricoid jet ventilation compared with surgical cricothyrotomy in a sheep airway salvage model. Resuscitation. 2004;62:79.
116. Scuderi, PE, McLeskey, CH, Comer, PB. Emergency percutaneous transtracheal ventilation during anesthesia using readily available equipment. Anesth Analg. 1982;61:867.
117. Stothert, JC, Jr., Stout, MJ, Lewis, LM, et al. High pressure percutaneous transtracheal ventilation: the use of large gauge intravenous-type catheters in the totally obstructed airway. Am J Emerg Med. 1990;8:184.
118. Frame, SB, Simon, JM, Kerstein, MD, et al. Percutaneous transtracheal catheter ventilation (PCTV) in complete airway obstruction—a canine model. J Trauma. 1989;29:774.
119. Ward, KR, Menegazzi, JJ, Yealy, DM, et al. Translaryngeal jet ventilation and end-tidal PCO2 monitoring during varying degrees of upper airway obstruction. Ann Emerg Med. 1991;20:1193.
120. Campbell, CT, Harris, RC, Cook, MH, et al. A new device for emergency percutaneous transtracheal ventilation in partial and complete airway obstruction. Ann Emerg Med. 1988;17:927.
121. Jaquet, Y, Monnier, P, Van Melle, G, et al. Complications of different ventilation strategies in endoscopic laryngeal surgery: a 10-year review. Anesthesiology. 2006;104:52.
122. Carl, ML, Rhee, KJ, Schelegle, ES, et al. Effects of graded upper-airway obstruction on pulmonary mechanics during transtracheal jet ventilation in dogs. Ann Emerg Med. 1994;24:1137.
123. Lenfant, F, Péan, D, Brisard, L, et al. Oxygen delivery during transtracheal oxygenation: a comparison of two manual devices. Anesth Analg. 2010;111:922.
124. Hamaekers, AE. The importance of flow and pressure release in emergency jet ventilation devices. Paediatr Anaesth. 2009;19:452.
125. Meissner, K. Successful transtracheal lung ventilation using a manual respiration valve: an in vitro and in vivo study. Anesthesiology. 2008;109:251.
126. Hamaekers, AE. Achieving an adequate minute volume through a 2 mm transtracheal catheter in a simulated upper airway obstruction using a modified industrial ejector. Br J Anaesth. 2010;104:382.
127. Wong, DT, Prabhu, AJ, Coloma, M, et al. What is the minimum training required for successful cricothyroidotomy?: a study in mannequins. Anesthesiology. 2003;98:349.
128. McCarthy, MC, Ranzinger, MR, Nolan, DJ, et al. Accuracy of cricothyroidotomy performed in canine and human cadaver models during surgical skills training. J Am Coll Surg. 2002;195:627.