Chapter 29 Craniovertebral Junction
A Reappraisal
• Atlantoaxial joint opening, manipulation, and direction fixation form important components of treatment of craniovertebral instability.
• Lateral masses of C1 and C2 are firm and largely cortical in nature and provide a solid ground for screw fixation.
• For atlantoaxial dislocation, atlantoaxial fixation should be done.
• Reduction of basilar invagination can be performed by distraction of the facets of the atlas and axis in a specific group of patients.
• Syringomyelia is always a secondary phenomenon. The primary cause should be identified and appropriately treated. Direct manipulation of the syrinx can be harmful.
Atlantoaxial Dislocation
Mobile and Reducible Atlantoaxial Dislocation
In the year 2001, we analyzed 160 cases with mobile and reducible AAD treated in our department during the years 1988 to 2001.1,2 In the series, the etiological factor for the dislocation included Morquio’s disease (9 cases), Down syndrome (8 cases), and craniosynostosis (5 cases). Although trauma leads to mechanical disruption of ligaments of the region, in “congenital” dislocation and dislocation related to known syndromes, laxity or incompetence of the ligaments is more often the cause. In several cases, the exact differentiation between a congenital and an acquired cause is difficult to decipher. The range of mobility of the dislocation is in general significantly higher in cases with congenital dislocation than in cases with trauma-related dislocation.
Surgical Treatment
The aim of surgery in general is to restore normal or the best possible alignment and to achieve stability of the atlantoaxial joint. The techniques of fixation for atlantoaxial dislocation can be divided into midline procedures that involve fixation of the arch of the atlas with the lamina of the axis and lateral mass fixation procedures. Midline methods of fixation include use of interlaminar clamps, Gallie’s posterior C1-C2 sublaminar wiring,3 Brooks-Jenkins fusion,4 and the Sonntag technique of sublaminar wiring.5 Lateral mass fixation procedures include Goel’s C1 lateral mass and C2 pedicle/pars screw fixation (interarticular)1,2 and the Magerl’s C1-C2 transarticular technique.6
Metal implants and fixation methods provide an initial period of fixation of the region, facilitating bony fusion. Bony fusion takes about 3 months and the metal implants should be strong enough to hold the region for that period. It ultimately depends on bony fusion to provide stability to the region. Bone harvested from the patient’s own iliac crest has been identified by several authors to be superior to any other form of bone graft or artificial material. Compromise on using the type of bone graft can lead to inadequate fusion, a phenomenon that can mar the entire operative procedure. Multiple pieces of corticocancellous bone graft should be placed in the craniovertebral region after elaborately preparing the host bone. The movements in the atlantoaxial region occur in the atlantoaxial joint. Any method of stabilization that directly fixes the joint and is segmental in nature has superiority over methods that employ fixation remote to the site of maximum movements and those that attempt to fix multiple bone segments. The lateral mass fixation techniques7 have been identified to be philosophically superior and biomechanically stronger to the techniques that involve fixation of the midline structures such as lamina and arch of atlas.
Craniovertebral Junction and Related Anatomy
The vertebral artery adopts a serpentine course in relation to the craniovertebral region. The artery has multiple loops and an intimate relationship with the atlas and axis bones. We observed a wide variability of the course of the artery in our specimens. The shape, size, and location of the vertebral artery groove on the inferior aspect of the superior articular facet of the C2 and over the posterior arch of the atlas have wide variations. The vertebral artery during its entire course is covered with a large plexus of veins. The venous plexuses are the largest in the region lateral to the C1-C2 joint. After a relatively linear ascent of the vertebral artery in the foramen transversarium of C6 to C3, the artery makes a loop medially toward an anteriorly placed superior articular facet of the C2 vertebra, making a deep groove on its inferior surface. The extent of medial extension of the loop varies. The distance of the artery from the midline of the vertebral body of C2 as would be observed during a transoral surgical procedure is an average of 12 mm.8 The vertebral artery loops away from the midline underneath the superior articular facet of the C2.
The dens or the odontoid process is flanked by two large, superior facets, extending laterally onto the adjoining pars interarticularis and articulating with the inferior atlantal facets. The superior facet of the C2 vertebra differs from the facets of all other vertebrae in two important characteristics. First, the superior facet of C2 is present in proximity to the body when compared to other facets, which are located in proximity to the lamina. Second, the vertebral artery foramen is present partially or completely in the inferior aspect of the superior facet of C2, but in other cervical vertebrae, the vertebral artery foramen is located entirely in relation to the transverse process. Unlike superior facets of all other vertebrae, they do not form a pillar with the inferior facets, being considerably anterior to them. The pedicle of the C2 vertebra is relatively small. The course of the vertebral artery in relation to the inferior aspect of the superior articular facet of the C2 makes it susceptible to injury during transarticular and interarticular screw implantation techniques. The average distance of the artery from the ganglion is 7.5 mm. This finding suggests that the dissection around the lateral end of the ganglion should be carefully done.
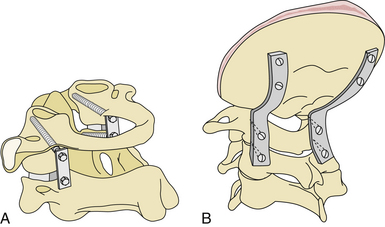
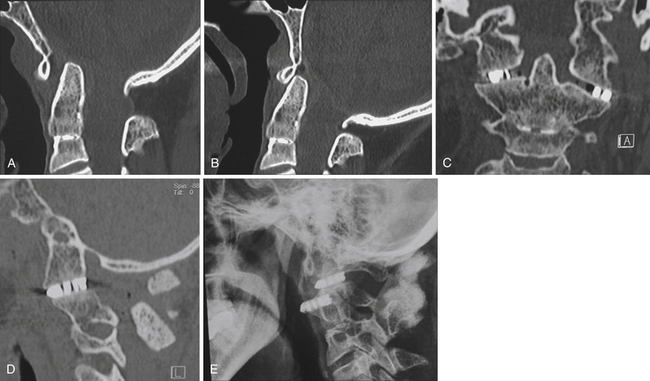
Lateral Mass Plate (or Rod) and Screw (Monoaxial or Polyaxial) Fixation (Figs. 29.1 to 29.6)1,2
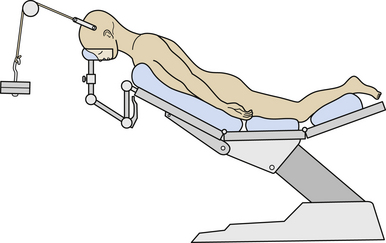
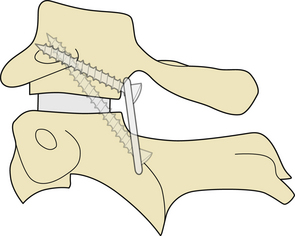
Cervical traction is set up prior to induction of anesthesia and the weights are progressively increased to approximately 5 to 8 kg or one sixth of the total body weight. The patient is placed prone with the head end of the table elevated to about 35 degrees (see Fig. 29.2). Cervical traction stabilizes the head in an optimally reduced extension position and prevents any rotation. The traction also ensures that the weight of the head is directed superiorly toward the direction of the traction and pressure over the face or eyeball by the headrest is avoided. The head is in a “hanging” position, the headrest being placed only for additional or minimal support. Elevation of the head end of the table, which acts as a countertraction, helps in reducing venous engorgement in the operative field. The suboccipital region and the upper cervical spine are exposed through an approximately 8-cm longitudinal midline skin incision centered on the spinous process of the axis. The spinous process of the axis is identified, and the attachment of paraspinal muscles to it is sharply sectioned. The large second cervical ganglion is closely related to the vertebral artery on its lateral aspect (see Fig. 29.3). It is first exposed widely and then sectioned sharply. This procedure provides a wide exposure of the lateral masses of the atlas and axis. Bleeding from the large venous sinuses in the region and in the extradural space can be troublesome. Packing of the region with Surgicel and Gelfoam can assist in the control of venous bleeding. The joint capsule is cut sharply, and the articular surfaces of the joint are exposed. The adjacent synovial articular surfaces of the atlantoaxial joint are decorticated widely with a microdrill, and pieces of bone harvested from the iliac crest are stuffed into the joint space. The lateral aspect of the lamina and a part of the pars of the axis are drilled to make the posterior surface of the lateral mass of the axis relatively flat so that the metal plate can be placed snugly and parallel to the bone. Drilling also helps in reducing the length of the plate and in placing the screw more superiorly and almost directly into the lateral mass of the axis. Actual vertebral artery exposure is unnecessary either lateral to the pars of the axis or superior to the arch of the atlas.
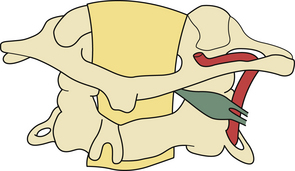
FIGURE 29.3 Drawing showing the relationship of the C2 ganglion, vertebral artery, and atlantoaxial joint.
Screws are implanted into the previously created guide holes in the lateral mass of the atlas and axis through a two- holed (approximately 2 cm in length) metal (stainless steel or titanium) plate. First, a screw is placed into the atlas. It is directed at an angle of approximately 15 degrees medial to the sagittal plane and 15 degrees superior to the axial plane. The preferred site of screw insertion is at the center of the posterior surface of the lateral mass, 1 to 2 mm above the articular surface. Whenever necessary, careful drilling of the inferior surface of the lateral aspect of the posterior arch of the atlas in relation to its lateral mass can provide additional space for the placement of the plate and screw implantation. The screw may even be implanted by choosing an insertion point on the articular surface of the lateral mass of the atlas. Such a site is useful more frequently in children than in adult patients. Screws can also be implanted into the facet of the atlas through the lateral aspect of the posterior arch of the atlas. Owing to the intimacy of vertebral artery relationships, screw implantation in the axis is relatively unsafe and needs to be precise. It was observed that the screw implantation in the superior facet of the C2 vertebra has to be sharply medial and directed toward the anterior tubercle of the C1 for transarticular fixation and toward the vertebral body of C2 for interarticular fixation. The pars interarticularis can be divided into nine quadrants;9 the superior and medial compartments can be used for the interarticular technique of screw implantation. Neuronavigation can be of assistance in identifying the best and the safest trajectory of the screw. The direction of screw implantation must be sharply medial and superior and should be toward the superior aspect of the body of the axis vertebra toward the midline. The medial surface of the pedicle of the axis is identified before the implantation of the screw. The screw is directed at an angle approximately 25 degrees medial to the sagittal plane and 15 degrees superior to the axial plane. The angle of screw insertion varies, depending on the local anatomy and the size of the bones. The quality of cancellous bone in the lateral masses of the atlas and axis in the proposed trajectory of screw implantation is generally good, providing an excellent purchase of the screw, and avoids the vertebral artery. The screws used are 2.9 mm in diameter in adult patients and 2.7 mm in diameter in pediatric patients. The length of the required screw is calculated on the basis of the size of the lateral masses observed on the preoperative radiological studies. The approximate lengths of the atlas screws are 26 to 28 mm in adults and 22 to 26 mm in children. The screws in the atlas and axis are almost similar in their length. The lateral masses of the atlas and axis are firm and cortical in nature, and, although preferable, it is not mandatory that the screws engage both the posterior and anterior cortices. If the screw traverses beyond the anterior cortex, it will lie harmlessly in the anteriorly displaced soft tissue. Injury to the critical neurovascular and pharyngeal wall is possible in such a situation but is extremely rare. Intraoperative fluoroscopic control and navigation were found to be helpful but not essential in determining the state of the screws. Large pieces of corticocancellous bone graft from the iliac bone are then placed over the adequately prepared posterior elements of atlas and axis. After the wound is closed, cervical traction is discontinued. The patients are mobilized as soon as possible and advised to wear a hard cervical collar for 3 months.
Double Insurance Fixation10
An alternative method of atlantoaxial fixation that combines the transarticular method of fixation and the interarticular fixation technique can be used. The technique combines the biomechanical strengths of both of the more commonly used techniques of fixation and provides maximal stability to the implants (see Figs. 29.4 and 29.5).
Basilar Invagination
Basilar invagination forms a prominent component of the craniovertebral anomalies. Chiari malformation and syringomyelia are commonly associated with basilar invagination and are the soft tissue components of the dysgenesis. Plain radiological and tomographic parameters have been principally used to diagnose basilar invagination for many years. There has been a renewed interest in the normal anatomy and pathological lesions of the craniovertebral junction with the development of imaging by high-resolution CT scan and MRI. Dynamic MRI and CT scans have helped in the evaluation of the pathology of basilar invagination, in the assessment of biomechanics of the joints, and in the formulation of a rationale for the surgical strategy. Despite the clarity of imaging, controversy regarding the management of basilar invagination continues. Even the natural history has not been clearly elucidated in the literature. The surgical indications for a given approach together with the timing of the surgical stages are still under discussion.
Pathogenesis
Several theories have been suggested to elucidate the probable cause and origin of basilar invagination. Most of these theories point toward embryological dysgenesis, genetic abnormalities, and viral infections.13–16 Several authors, for over a century, have thought that deformation had a mechanical cause and therefore applied the name: “impressio baseos cranii” (Berg and Retzius, 1855, cited by Virchow, 1876),17 or basilar impression.18 Grawitz (1880)19 believed that basilar invagination was often a result of under- or maldevelopment of the craniovertebral transition region. A range of malformations is frequently associated with anomalies of the atlas and axis, some of which may be quite atypical, and with fissures or defects and bone projections from the spinal column in the craniovertebral transition zone. The latter anomalies were grouped together by von Torklus and Gehle (1970) as suboccipital dysplasias.18 Basilar invagination can be secondary to abnormally inclined alignment of the facets of the atlas and axis.20 The progressive slippage of the atlas over the axis secondary to this malalignment, a process similar to spondylolisthesis in the lumbosacral spine, results in invagination of the odontoid process into the craniocervical cord.20,21 Short neck, low hairline, web-shaped neck muscles, torticollis, reduction in the range of neck movements, and several such physical variations have been described as hallmarks of basilar invagination for over a century. A number of bone fusion deformities and platybasia have also been recorded. Neck pain, muscle spasms, and restriction of neck movements are frequently noted and suggest instability of the region. Degeneration of the atlantoaxial joint and primary or secondary destruction of the facets of atlas or axis can lead to superior and posterior migration of the odontoid process and result in basilar invagination and fixed or irreducible atlantoaxial dislocation. Such involvement of the lateral masses can result in laxity of the posterior atlantoaxial or retro-odontoid ligaments that result in retro-odontoid pannus or “tumor-like” or “osteophyte-like” formation.
Classification into Groups I and II
In 1997, we presented a classification system for basilar invagination that divided it into two discrete categories. This classification helped in clarifying the understanding of the pathology and pathogenesis of the anomaly, in the selection of the surgical treatment, and in prediction of the outcome.22 Based on a single criterion of the absence or presence of Chiari malformation, the anomaly was classified into groups I and II, respectively.
Essentially, group I included cases in which there was invagination of the odontoid process into the foramen magnum and indented into the brainstem. The tip of the odontoid process distanced itself from the anterior arch of the atlas or the inferior aspect of the clivus. The distancing of the odontoid process from the anterior arch suggested the presence of instability in the region and atlantoaxial dislocation. The angle of the clivus and the posterior cranial fossa volume were essentially unaffected in these cases. In group II, on the other hand, the assembly of the odontoid process, anterior arch of the atlas, and the clivus migrated superiorly in unison, resulting in reduction of the posterior cranial fossa volume, which was the primary pathology in these cases. The Chiari malformation or herniation of the cerebellar tonsil was considered to be a result of reduction in the posterior cranial fossa volume. In 1997, Goel first defined the clinical implication of association of small posterior cranial fossa volume and Chiari malformation.22
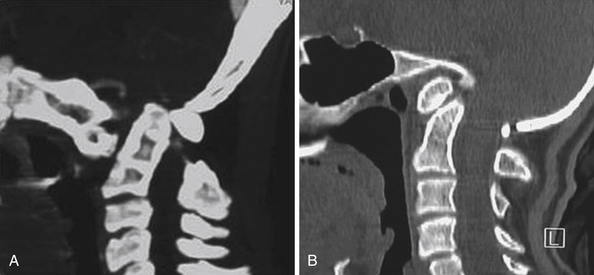
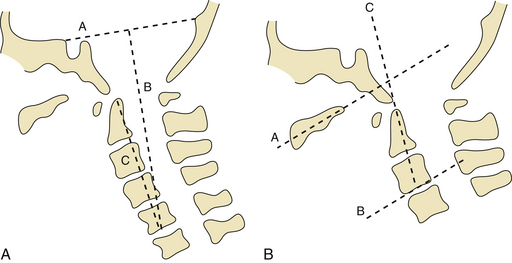
Classification into Groups A and B
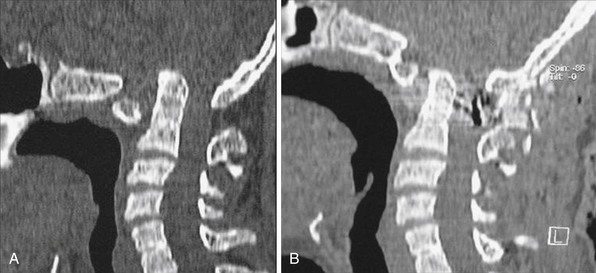
In our 2004 study, we identified a subgroup of patients in whom there was clear radiological evidence of instability of the region that was manifested by distancing of the odontoid process away from the anterior arch of the atlas, and the radiological features matching those of group I cases. Considering this current evaluation we have proposed a new classification for basilar invagination into two groups based on parameters that determined an alternative treatment strategy.23,24 In group A basilar invagination there was a “fixed” atlantoaxial dislocation and the tip of the odontoid process “invaginated” into the foramen magnum and was above the Chamberlain line,25 McRae line of the foramen magnum,26 and Wackenheim’s clival line.27 The definition of basilar invagination of prolapse of the cervical spine into the base of the skull, as suggested by von Torklus,18 was suitable for this group of patients (Fig. 29.7A). In group B basilar invagination the odontoid process and clivus remained anatomically aligned despite the presence of basilar invagination and other associated anomalies. In this group, the tip of the odontoid process was above the Chamberlain line but below the McRae and Wackenheim’s lines (Fig. 29.7B). The radiological findings suggested that the odontoid process in group A patients resulted in direct compression of the brainstem. Essentially, in group A basilar invagination, the pathogenesis appeared to be mechanical instability of the region that was manifested by the tip of the odontoid process distancing itself from the anterior arch of the atlas or the lower end of the clivus. In some group A patients there was Chiari malformation, and this feature differentiates the present classification from the earlier classification. In this group, the atlantoaxial joints were “active” and their orientation was oblique, as shown in Figure 29.8A, instead of the normally found horizontal orientation. Similarities of such a position of the C1-C2 facets with spondylolisthesis in the subaxial spine can be seen. It appears that the atlantoaxial joint in such cases is in an abnormal position and progressive worsening of the dislocation is probably secondary to increasing “slippage” of the facets of the atlas over the facets of the axis. In group B, the pathogenesis appeared to be congenital dysgenesis, and atlantoaxial joints were normally aligned or were entirely fused. The pathogenesis of basilar invagination appears to be different in the two groups. Understanding of these two types of basilar invaginations is crucial in understanding the various management issues involved.
Vertical mobile and reducible atlantoaxial dislocation occurs when there was basilar invagination when the neck was flexed, but the alignment was normal when the head was in an extended position.28 Although such mobility is only rarely identified, it does indicate the need for dynamic flexion-extension studies to preoperatively assess the craniovertebral instability. Vertical dislocation is due to incompetence of the atlantoaxial joint and lateral masses.
Diagnosis and Clinical Features
The majority of patients with group A basilar invagination (58%) had a history of minor to major head injury prior to the onset of the symptoms. The pyramidal symptoms formed a dominant component. Kinesthetic sensations were affected in 55% of these patients. Spinothalamic dysfunction was less frequent (36%). Neck pain was a major presenting symptom in 77% of cases. Torticollis was present in 41% of cases.23 The analysis of radiological and clinical features suggests that the symptoms and signs were a result of brainstem compression by the odontoid process. The presentation was relatively acute in group A cases but it was long-standing and slowly progressive in group B cases. In group B cases, the onset of symptoms and their evolution were insidious.
Precipitating Factors
Trauma of varying severity was a noteworthy precipitating factor in group A cases.29,30 Trauma seldom plays any major role in precipitating the symptoms in group B cases. The fact that trauma influenced the acute development of symptoms pointed toward an element of instability of the craniovertebral region in group A patients.
Associated Clinical Features
Mere inspection of the patients with basilar invagination was of diagnostic value in the majority of cases in both the groups. However, short neck and torticollis were more frequently encountered in cases with group A basilar invagination. The symptoms and signs in group B basilar invagination appeared to be directly related to the “crowding” of neural structures at the foramen magnum. Although the dimensions of the foramen magnum were large and sometimes larger than even in a normal state, the volume of its contents and probably the “pulsatile” compression of the structures at the foramen magnum resulted in neurological symptoms.31 The markedly reduced girth of the brainstem in group A cases clearly showed that direct compression of the brainstem by the odontoid process caused the neurological symptoms. Central cord symptoms and related signs were noted in cases associated with syringomyelia.
Radiological Criteria
The Chamberlain Line
Basilar invagination was diagnosed when the tip of the odontoid process was at least 2 mm above the Chamberlain line.25 Measurement of the Chamberlain line on lateral sagittal reconstruction pictures of CT scan and sagittal MRI were seen to be reliable and accurate. The analysis of basilar invagination in the two groups on the basis of the Chamberlain line suggested that the basilar invagination is much more severe in group B than in group A.
Distance Between the Odontoid Tip to the Pontomedullary Junction
The distance of the tip of the odontoid from the pontomedullary junction, as observed on MRI, is a useful index to define the reduction of the posterior cranial fossa bone size.25 The distance was markedly reduced in group B cases but it was relatively large in group A cases.
Wackenheim’s Clival Line
Wackenheim’s clival line is a line drawn along the clivus. The tip of the odontoid process was significantly superior to Wackenheim’s clival line in group A cases. In group B cases, the relationship of the tip of the odontoid process and the lower end of the clivus and the atlantodental and clivodental interval remained relatively normal. In a majority of these cases, the tip of the odontoid process remained below Wackenheim’s clival line4,27 and McRae’s line of the foramen magnum.26 The basilar invagination thus resulted from the rostral positioning of the plane of the foramen magnum in relation to the brainstem.
Posterior Cranial Fossa Volume
The Klaus’ height index,32 measured on MRI, was seen to be much more accurate than the conventional measurements based on plain radiographs. The tentorium could be clearly identified on MRI and the distance of the tip of the odontoid from the line of the tentorium indicated the height of the posterior cranial fossa. On the basis of Klaus’ index, the posterior fossa height was found to be markedly reduced in group B cases but it was only moderately affected in group A cases.
Omega Angle
Although not frequently used, the omega angle, or the angulation of the odontoid process from the vertical as described by Klaus, was found to be a useful guide.32 Goel described a modified omega angle as the measurement of the angle from the vertical and noted it was affected by the flexion and extension of the neck.22 A line was drawn traversing through the center of the base of the axis parallel to the line of the hard palate. The line of the hard palate was unaffected by the relative movement of the head and the cervical spine during the movement of the neck in these “fixed” craniovertebral anomalies. Facial hypoplasia or hard palate abnormality was not seen in any case in this series and did not affect the measurements. The omega angle depicted the direction of displacement of the odontoid process. The omega angle was severely reduced in group A cases but it was much larger in group B cases. The reduction in the omega angle in group A cases depicted that the odontoid process had tilted toward the horizontal and was posteriorly angulated in group A cases, but it was near vertical and superiorly migrated in group B cases (Fig. 29.9).
Brainstem Girth
The effective brainstem girth measured on MRI is a useful additional parameter.22 Although the brainstem girth is markedly reduced in group A cases, the girth is only marginally affected or unaffected in group B cases, indicating thereby that there is no direct brainstem compression as a result of the odontoid process in the latter group.
Occipitalization of the Atlas
Occipitalization of the atlas associated with basilar invagination was noted first by Rakitansky (cited by Grawitz 1880)19 and has since been referred to frequently.19,25,26,33,34 Many authors have regarded assimilation as a characteristic feature of basilar invagination. The assimilation of the atlas can be partial or incomplete.
Neck Size
Measurement of craniovertebral height can be done using a modification of Klaus’ posterior fossa height index.13,22,32 The cervical height was measured from the tip of the odontoid process to the midpoint of the base of the C7 vertebral body (see Fig. 29.9). Direct physical measurement of the neck length can be a useful parameter. The parameter of direct physical measurement of the neck length from the inion to the tip of the C7 spinous process can be useful.13,35 Cervical lordosis is evaluated with a modification of the Klaus omega angle13,32 and a modified omega angle.22
Surgical Management
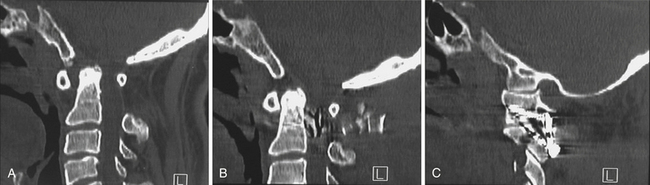
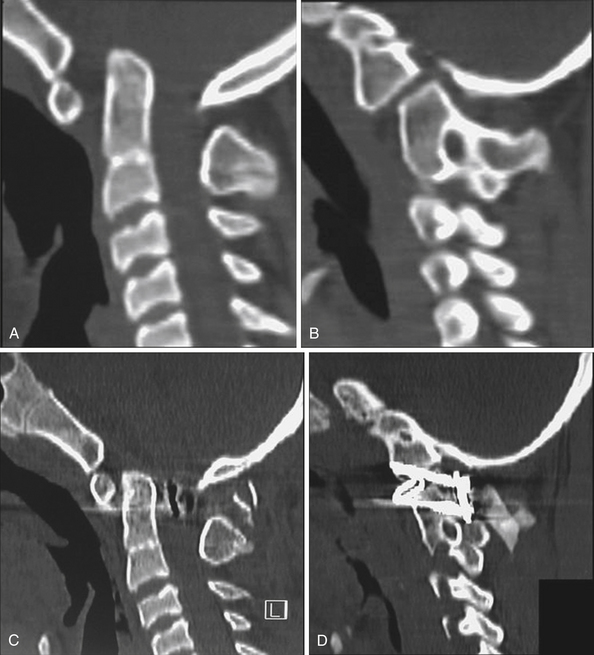
Craniovertebral Realignment for Group A Basilar Invagination
The conventional form of treatment of group A basilar invagination is a transoral decompression22,23,36 that is followed by posterior occipitocervical fixation. However, the long-term clinical outcome following the twin operation of transoral decompression followed by posterior stabilization was seen to be inferior to the clinical outcome following surgery that involves craniovertebral realignment without any bone, dural, or neural decompression. An attempt can be made to reduce basilar invagination by performing occipitocervical fixation following institution of cervical traction.22,36 However, all our cases treated in this manner subsequently needed transoral decompression as the reduction of the basilar invagination and of atlantoaxial dislocation could not be sustained by the implant. The technique of craniovertebral realignment by wide removal of the atlantoaxial joint capsule and articular cartilage by drilling and subsequent distraction of the joint by manual manipulation provides a unique opportunity to obtain reduction of the basilar invagination and of atlantoaxial dislocation.
Technique of Craniovertebral Realignment
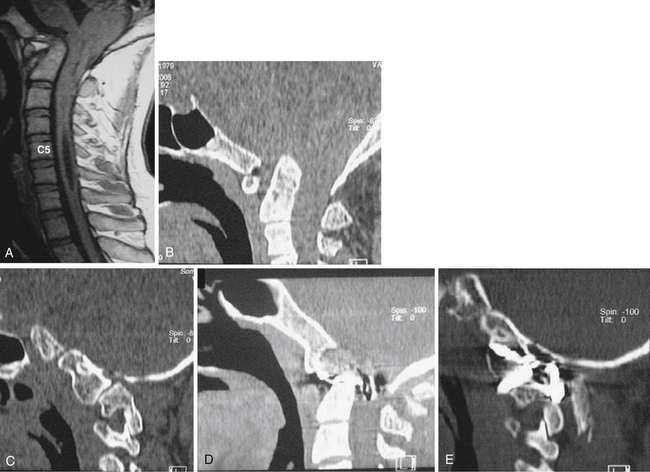
This operation is suitable for patients with group A basilar invagination. The exposure of the atlantoaxial joint in cases with basilar invagination is significantly more difficult and technically challenging when compared to a normally aligned atlantoaxial joint encountered during the treatment of post-traumatic instability. The joint is rostral in location and the microscope needs to be appropriately angled. The atlantoaxial facet joints are widely exposed on both sides after sectioning of the large C2 ganglion. The joint capsule is excised and the articular cartilage is widely removed using a microdrill. The joints on both sides are distracted using an osteotome. The flat edge of the osteotome is introduced into the joint and it is then turned vertical to effect distraction. The status of the dislocation and of basilar invagination is evaluated by intraoperative radiographic control. Corticocancellous bone graft harvested from the iliac crest is stuffed into the joint in small pieces. Specially designed titanium spacers are used in selected cases as strut graft and impacted into the joints to provide additional distraction and stability. Subsequent fixation of the joint with the help of interarticular screws and a metal plate provides a biomechanically firm fixation and sustained distraction. Holes in the titanium metal spacer provide space for bone fusion. The fixation is seen to be strong enough to sustain the vertical, transverse, and rotatory strains of the most mobile region of the spine. Postoperatively the traction is discontinued and the patient is placed in a four-post hard cervical collar for 3 months during which all physical activities involving the neck are restrained (Figs. 29.8 to 29.10).
Foramen Magnum Decompression for Group B Patients
Foramen magnum bony decompression appears to be ideal for group B basilar invagination. The procedure resulted in amelioration of symptoms and at least an arrest in the progression of the disability. Driesen (1960) reported that during operations for craniovertebral anomalies, he often had to remove noticeably thickened pieces of bone from the posterior edge of the foramen magnum.30 In our cases, the suboccipital bone and posterior rim of the foramen magnum and the dura overlying the herniated cerebellar tissue were thin in a significant number of cases. This probably was related to the chronic pressure changes secondary to the reduced posterior cranial fossa volume. The bulbous lipping of the posterior rim of the foramen magnum represents the rudiments of the posterior arch of the atlas assimilated into the occipital bone.16 Various authors have recommended that to achieve maximal decompression, it is necessary to open the dura mater and to cut all constrictive dural and arachnoidal bands. Some authors have recommended leaving the dura open while others have recommended the placement of a graft. Current papers do not recommend resection of the herniating tonsils37 or even sectioning of adhesions around them. The fact that dural opening was not necessary while performing posterior fossa or foramen magnum decompression was first described by Goel and co-workers in 1997.22 This finding was based on the understanding that the dura is an expansile structure and cannot be a compressive factor.22,38 Opening of the dura is not only unnecessary but also subjects the patient to an increased risk of cerebrospinal fluid fistula. It makes an otherwise simple surgery into a relatively complex and dangerous surgical maneuver.
Syringomyelia
Syringomyelia is a frequently encountered clinical and radiological entity. It is associated with a range of pathological conditions that include congenital craniovertebral anomalies, tumors, infections, trauma, and spinal deformities. Syringomyelia is rarely or never an acute phenomenon and is generally encountered in long-standing and persistent space-occupying or space-reducing lesions and in situations with subtle but persistent instability. Obstruction to the normal flow of spinal or cranial CSF by post-traumatic or infective arachnoiditis is also a less frequently encountered cause of syringomyelia. Acute injuries, acute infections, rapidly growing malignant tumors, mobile dislocations, and acute post-traumatic deformities are generally not associated with syringomyelia. The clinical presenting features are long-standing and relentlessly progressive. Syringomyelia or “hydrocephalus of the cord” is never a primary phenomenon. It is always secondary to an obvious or an unidentified pathological cause.38,39 The understanding of the pathophysiology of syringomyelia is crucially important to design a suitable treatment strategy and prognosticate the ultimate outcome. All attempts must be made to identify and treat the primary pathological cause. Syrinx drainage as a primary procedure may not be considered a therapeutic option. Syrinx drainage or shunting without dealing with the primary pathological cause can result in disastrous clinical consequences.
Rationale of Treatment
Treatment strategy in such cases should be directed toward increasing the posterior cranial fossa volume by posterior fossa volume expansion or foramen magnum decompression. Logue reported 75 patients treated with craniovertebral decompressions for Chiari malformations and syringomyelia.40 The patients were divided into two groups: one was treated with bone decompression alone, leaving the arachnoid intact, and one group was treated with Gardner’s procedure of opening the fourth ventricle and plugging the upper cervical canal. They concluded that muscle plugging did not seem to change the results. Levy and associates also concluded along the same lines.41 Logue and Edwards noticed that there was no significant need for performing a syringosubarachnoid shunt following craniovertebral decompression.40 Various subsequent studies have questioned the need for a syrinx drainage surgery following foramen magnum decompression. Di Lorenzo and colleagues concluded from their study that “conservative” craniocervical decompression should be considered the first option in the treatment of syringomyelia-Chiari I complex.42 The routine of opening of the posterior cranial fossa dura, resection of the cerebellar tonsils, arachnoidal sectioning, and syringostomy is unnecessary. It appears that if the primary problem of basilar invagination is dealt with early in the course of the disease, the secondary and the tertiary events will spontaneously regress.43 Craniovertebral realignment by atlantoaxial facet distraction can be a philosophical approach to treatment in cases having group A basilar invagination, Chiari malformation, and syringomyelia (Fig. 29.11). When there is syringomyelia and Chiari malformation but no definite basilar invagination, efforts can be made to identify the cause of the Chiari malformation.44,45 In such cases, it might be possible that the cerebellar mass is larger than normal. Even in such cases, volume expansion of the posterior cranial fossa is required. The theory that dura or dural bands can act as a compressive factor appears unacceptable and does not correlate well with the pathogenic events. The dura is an expansile structure and may never be a compressive factor.46,47
Syringomyelia secondary to primary cord pathology such as a tumor or kyphosis also appears to be a secondary and a “protective” phenomenon. Treatment in such cases should be directed toward treatment of the disease and not toward the treatment of syringomyelia.44 Our observation is that if the syringomyelia is treated without dealing with the primary pathological cause, more often than not the outcome is poor and the patient can be harmed.
Degenerative Arthritis
Like all other joints of the body, atlantoaxial joints are also subject to arthritis. With the general aging of the population, the issue of arthritis is becoming more relevant. Osteoarthritis of the atlantoaxial joint is a well-defined phenomenon that eventually results in atlantoaxial instability. The process of joint degeneration and instability is a progressive phenomenon and extends over several months to years. This instability is probably the result of degeneration of the articular cartilage, reduction of the joint space, and secondary incompetence of the ligaments controlling the movements.48–51
Clinical Features
Pain in the neck on movement often forms the earliest and most prominent symptom. The more classical pattern of presentation is of an elderly patient presenting with symptoms of pain in the neck on movements and restriction of neck movements and gradually progressive quadriparesis over a few days to several months. The incidence and severity of quadriparesis vary in different reports and this variation reflects the duration of the disease before the diagnosis is clinched. Sensory symptoms are relatively mild and typically include bilateral upper and lower extremity paresthesias and kinesthetic sensation deficits. History of mild to moderately severe trauma a few days to several years prior to diagnosis may be present in a substantial number of patients and in most of these cases, the symptoms in general progress from the time of trauma. Palpable crepitus with motion has also been identified as a presenting symptom.52 Carrying of heavy weights over the head has also been incriminated to cause increased incidence of cervical spondylotic changes and also basilar invagination.53
Radiological Features
Among the more constant radiological features is reduction of the height of lateral mass complex due to reduction of joint space. Erosion of bones of the lateral masses of atlas and axis and of the body is usually observed in more chronic situations.54 Degenerative erosion of the facets of the atlas and axis, of the odontoid process and body of the axis, and periodontoid ligamentous degenerative changes are also frequent.
The term basilar invagination in cases with a variety of forms of craniovertebral arthritis has been used synonymously with the terms cranial settling or vertical odontoid migration.23,24,53 The basilar invagination is only mild to moderate in cases with degenerative arthritis. This is in variance with the basilar invagination observed in cases of rheumatoid arthritis wherein the superior migration of the odontoid process is significantly more due to the more severe lateral mass bone collapse.
Atlantoaxial joint arthritis is expected to eventually result in atlantoaxial instability. The dislocation may only be partially reducible due to the presence of nonyielding tissues around the odontoid process. The subtlety of instability may make the diagnosis difficult in some cases.
Degenerative pannus, also termed as articular, ganglion, synovial, or juxta-facet cyst, may arise from the degenerating synovial lining of any joint in the body.55–58 Pannus related to atlantoaxial joint arthritis probably represents degenerative ligaments and secondary “osteophyte-like” tissue formation in the periodontoid region.50,59 Degenerating tissues are typically isointense on T1-weighted images and iso- to hypointense on T2-weighted images and do not enhance on contrast administration. In some cases, the retro-odontoid mass may give a “tumor-like” (pseudotumor) appearance resulting in posterior “buckling” of the posterior longitudinal ligament or the tectorial membrane and indentation of the cord substance.51 The retro-odontoid ligamentous hypertrophy appears to be related to laxity of ligaments due to reduced atlantoaxial height and secondary to progressive degenerative changes in the region. The pathogenesis of the degenerative changes simulates to an extent the formation of posterior osteophytes in cases with spinal degeneration. It appears that the presence of retro-odontoid ligamentous degenerative hypertrophy in an elderly patient can be diagnostic evidence that suggests atlantoaxial instability, even when such instability is not clearly visualized on radiological imaging. In general, it is observed that retro-odontoid ligamentous degenerative changes are identified and are thicker in cases in which the atlantoaxial instability is less marked and the entire degenerative process was more chronic in nature. As opposed to cases having rheumatoid arthritis where the process is more chronic or long-standing, the bone destruction of the facets of the atlas and axis and osteomalacia are not as pronounced in cases of degeneration-related arthritis. Degeneration of the atlantodental joint may be observed in a minority of patients. Cervical spondylotic degenerative disease is likely to be present in varying degrees in the rest of the spine in most cases.
Surgery (see Fig. 29.5)
For basilar invagination and retro-odontoid ligamentous hypertrophy, transoral decompression or subsequent posterior fixation has been the treatment protocol.52,60 Although some surgeons still prefer to resect the retro-odontoid degenerative mass,52 the current consensus appears to be that in such cases stabilization of the atlantoaxial joint is sufficient and results in regression of the retro-odontoid mass. Some surgeons advise incorporation of the occipital bone and cervical vertebrae up to C3 and C4 in the occipitocervical fixation and feel that such a fixation is necessary to avoid “cranial settling.”50,60 However, such an extended fixation does not seem to be necessary. The lateral mass plate and screw method of fixation can be useful. An attempt may additionally be made to distract the facets and restore the height of the lateral mass by impaction of bone chips harvested from the iliac crest alone or by additional impaction of spiked metal spacers.51 Distraction of the facets not only assists in the reduction and fixation of the atlantoaxial dislocation and basilar invagination but also stretches the buckled posterior spinal ligaments that appear to have a role in the pathogenesis of retro-odontoid ligamentous degenerative hypertrophic mass. Upon opening the joint, the presence of a relatively rough and pale yellow articular surface devoid of end plate, reduction of the joint space, and evidence of instability of the region are the more prominent observations. On reviewing the postoperative images, it was apparent that in all cases there was reduction of atlantoaxial dislocation and of basilar invagination. The postoperative reduction of the dislocation was significant but incomplete in about half the cases in which the reduction of the dislocation was incomplete during preoperative evaluation. This was probably due to the presence of nonyielding periodontoid ligamentous degenerative mass. Despite the incomplete reduction, the treatment resulted in an immediate postoperative and sustained neurological recovery. This improvement appeared to be related to elimination of abnormal mobility, realignment of bones, and probably by reduction of the indentation by the retro-odontoid mass. Postoperative CT scan showed evidence of reduced soft tissue shadow in the periodontoid space.
Rheumatoid Arthritis Affecting Craniovertebral Junction
Seropositive rheumatoid arthritis has been identified in approximately 0.9% of the white adult population of the United States and 1.1% of the adult population in Europe.59,61 Of these, as many as 10% of patients may need an operation for craniovertebral region instability. Rheumatoid arthritis is a disease of the articular capsule and bones forming the atlantoaxial joint. The articular capsule and the subcapsular bone may be affected leading to varying degrees of subluxation and basilar invagination. Such a joint can lead to “lateral mass collapse,” as has been identified by some authors in similar cases.53,59,61 The term basilar invagination in cases with rheumatoid arthritis has been used synonymously with the terms cranial settling or vertical odontoid migration.53,62,63 Basilar invagination is commonly associated with atlantoaxial dislocation and the complex results in a significant degree of neck pain and myelopathy, adding considerably to the disability secondary to involvement of other joints.
Surgery
A variety of instrumentation and methods have been adopted to secure the occipitocervical fixation. Recently, a number of authors have reported success after transarticular atlantoaxial fixation.64,65 For basilar invagination, transoral decompression and subsequent posterior fixation have been accepted treatment protocols. Menezes and co-workers observed that traction in cases with basilar invagination and atlantoaxial subluxation results in a significant improvement in the craniovertebral alignment.53
Retro-Odontoid Pannus
Pannus has uniformly been recognized to be secondary to an inflammatory response in cases of rheumatoid arthritis. However, it appears that reduction of the height of the lateral mass pillar secondary to bone destruction and reduced joint space can result in buckling of the retro-odontoid ligaments, giving a “pannus-like” formation. Surgery that involves restoration of the height of the lateral mass can lead to immediate reduction of the size of the pannus.66,67
Tuberculosis of Craniovertebral Junction
Natural Course of Disease
The general pattern of progression of craniovertebral tuberculosis can be divided into three stages.
Indications for Surgery
Neurological deficits are notably delayed and less pronounced despite the aggressive destruction and deformation by the disease. The disease is initially unilateral and the contralateral atlantoaxial joint is spared till late in the disease process. Owing to the relative stability of the craniovertebral region despite the unilateral facetal destruction and the effectiveness of modern antituberculosis drugs, surgery can be delayed or avoided. The extent and nature of involvement of the joints are determining factors for the need for any kind of surgery for stabilization of the region. Surgery for evacuation of pus or granulation tissue is seldom required. Despite the extensiveness of the bone destruction and inflammation, the patient is usually neurologically quite stable, and the systemic symptoms are not pronounced till late in the disease process. In the absence of progressive neurological symptoms and in the presence of an intact contralateral atlantoaxial joint, surgery can be avoided. The patient needs to be placed on antituberculosis drugs. In addition, the patient will need a firm four-poster cervical collar and all activities related to neck movements and weight bearing should be avoided for at least 3 months or till there is evidence of bone healing and regression of symptoms.
Goel A., Bhatjiwale M., Desai K. Basilar invagination: a study based on 190 surgically treated cases. J Neurosurg. 1998;88:962-968.
Goel A., Laheri V.K. Plate and screw fixation for atlanto-axial dislocation. Technical report. Acta Neurochir (Wien). 1994;129:47-53.
Goel A., Sharma P. Craniovertebral realignment for basilar invagination and atlantoaxial dislocation secondary to rheumatoid arthritis. Neurol India. 2004;52(3):338-341.
Goel A., Shah A. Reversal of longstanding musculoskeletal changes in basilar invagination after surgical decompression and stabilization. J Neurosurg Spine. 2009;10(3):220-227.
Goel A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004;1(3):281-286.
Please go to expertconsult.com to view the complete list of references.
1. Goel A., Desai K., Muzumdar D. Atlantoaxial fixation using plate and screw method: a report of 160 treated patients. Neurosurgery. 2002;51:1351-1357.
2. Goel A., Laheri V.K. Plate and screw fixation for atlanto-axial dislocation. Technical report. Acta Neurochir (Wien). 1994;129:47-53.
3. Gallie W.E. Fractures and dislocations of cervical spine. AMJ Surg. 1939;46:495-499.
4. Brooks A.L., Jenkins E.B. Atlantoaxial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978;60A:279-284.
5. Dickman C.A., Sonntag V.K., Papadopoulos S.M., Hadley M.N. The interior spinous method of posterior atlantoaxial arthrodesis. J Neurosurg. 1991;74:190-198.
6. Jeanneret B., Magerl F. Primary posterior fusions C1-2 in odontoid fractures: indications, technique and results of transarticular screw fixation. J Spinal Disord. 1992;5:464-475.
7. Kuroki H., Rengachary S.S., Goel V.K., et al. Biomechanical comparision of two stabilization techniques of the atlantoaxial joints: transarticular screw fixation versus screw and rod fixation. Neurosurgery. 2005;56:151-159.
8. Cacciola F., Phalke U., Goel A. Vertebral artery in relationship to C1-C2 vertebrae: an anatomical study. Neurol India. 2004;52(2):178-184.
9. Gupta S., Goel A. Quantitative anatomy of the lateral masses of the atlas and axis vertebrae. Neurol India. 2000;48:120-125.
10. Goel A. Double insurance atlantoaxial fixation. Surg Neurol. 2007;67(2):135-139.
11. Goel A. Atlantoaxial joint jamming as a treatment for atlantoaxial dislocation: a preliminary report. Technical note. J Neurosurg Spine. 2007;7(1):90-94.
12. Goel A., Kulkarni A.G. Screw implantation in spinous process for occipitoaxial fixation. J Clin Neurosci. 2004;11(7):735-737.
13. Goel A., Shah A. Reversal of longstanding musculoskeletal changes in basilar invagination after surgical decompression and stabilization. J Neurosurg Spine. 2009;10(3):220-227.
14. David K.M., Thorogood P.V., Stevens J.M., Crockard H.A. The dysmorphic cervical spine in Klippel-Feil syndrome: interpretations from developmental biology. Neurosurg Focus. 1999;6(6):E1.
15. Gunderson C.H., Greenspan R.H., Glaser G.H., Lubs H.A. The Klippel-Feil syndrome: genetic and clinical re-evaluation of cervical fusion. Medicine. 1967;46:491-512.
16. Menezes A.H. Primary craniovertebral anomalies and hindbrain herniation syndrome (Chiari I): database analysis. Pediatr Neurosurg. 1995;23:260-269.
17. Virchow R. Beitrage zur Physischen Anthropologie der Deutschen, mit Besonderer Berucksichtigung der Friesen. Berlin: Abhandlungen de Koniglichen Akademie der Wissenschaften; 1876.
18. Von Torklus D., Gehle W. The Upper Cervical Spine: Regional Anatomy, Pathology, and Traumatology. A Systematic Radiological Atlas and Textbook. New York: Grune & Stratton; 1972. 1–98
19. Grawitz P. Beitrag zur Lehre von der basilaren Impression des Schadels. Arch Path Anat Physiol. 1880;80:449.
20. Kothari M., Goel A. Transatlantic odonto-occipital listhesis: the so-called basilar invagination. Neurol India. 2007;55:6-7.
21. Goel A. Progressive basilar invagination after transoral odontoidectomy: treatment by facet distraction and craniovertebral realignment. Spine. 2005;30:E551-E555.
22. Goel A., Bhatjiwale M., Desai K. Basilar invagination: a study based on 190 surgically treated cases. J Neurosurg. 1998;88:962-968.
23. Goel A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004;1(3):281-286.
24. Goel A., Sharma P. Craniovertebral junction realignment for the treatment of basilar invagination with syringomyelia: preliminary report of 12 cases. Neurol Med Chir (Tokyo). 2005;45(10):512-518.
25. Chamberlain W.E. Basilar impression (platybasia). A bizarre developmental anomaly of the occipital bone and upper cervical spine with striking and misleading neurologic manifestations. Yale J Biol Med. 1939;11:487-496.
26. McRae D.L. Bony abnormalities in the region of foramen magnum: correlation of anatomic and neurologic findings. Acta Radiol. 1953;40:335-354.
27. Thiebaut F., Wackenheim A., Vrousos C. New median sagittal pneumostratigraphical findings concering the posterior fossa. J Radiol Electrol. 1961;42:1-7.
28. Goel A., Shah A., Rajan S. Vertical and mobile atlanto-axial dislocation. Clinical article. J Neurosurg Spine. 2009;11(1):9-14.
29. Bharucha E.P., Dastur H.M. Craniovertebral anomalies. A report on 40 cases. Brain. 1964;87:469-480.
30. Driesen W. Findings at operation in the central nervous system in basilar impressions and related abnormalities of the atlanto-occipital region. Acta Neurochir (Ger). 1960;9:9-68.
31. Williams B. A critical appraisal of posterior fossa surgery for communicating syringomyelia. Brain. 1978;101:223-250.
32. Klaus E. Rontgendiagnostik der platybasic und basilaren impression. Fortscher Rontgenstr. 1957;86:460-469.
33. Spillane J.D., Pallis C.H., Jones A.M. Developmental abnormalities in the region of the foramen magnum. Brain. 1957;80:11-47.
34. Virchow R. Untersuchungen Fiber die Entwicklung des Schadelgrundes. Berlin: Reimer; 1857.
35. Mahajan P.V., Bharucha B.A. Evaluation of short neck: new neck length percentiles and linear correlations with height and sitting height. Indian Pediatr. 1994;31:1193-1203.
36. Goel A., Achawal S. Surgical treatment for Arnold Chiari malformation associated with atlantoaxial dislocation. Br J Neurosurg. 1995;9:67-72.
37. Fischer E.G. Posterior fossa decompression for Chiari 1 deformity, including resection of the cerebellar tonsils. Childs Nerv Syst. 1995;11:625-629.
38. Goel A. Is syringomyelia pathology or a natural protective phenomenon? J Postgrad Med. 2001;47:87-88.
39. Goel A., Desai K.I. Surgery for syringomyelia: an analysis based on 163 surgical cases. Acta Neurochir (Wien). 2000;142:293-302.
40. Logue V., Edwards M.R. Syringomyelia and its surgical treatment—an analysis of 75 patients. J Neurol Neurosurg Psychiatry. 1981;44:273-284.
41. Levy W.J., Mason L., Hahn J.F. Chiari malformation presenting in adults: a surgical experience in 127 cases. Neurosurgery. 1983;12:377-390.
42. Di Lorenzo N., Fortuna A., Guidetti B. Craniovertebral junction malformations. Clinicoradiological findings, long-term results, and surgical indications in 63 cases. J Neurosurg. 1982;56:603-608.
43. Goel A. Basilar invagination, Chiari malformation, syringomyelia: a review. Neurol India. 2009;57(3):235-246.
44. Goel A., Cacciola F., Muzumdar D.P. Trigeminal neurinoma associated with Chiari malformation and syringomyelia. J Clin Neurosci. 2005;12(5):608-610.
45. Goel A., Muzumdar D., Dange N. Syringomyelia in infants secondary to mobile congenital atlantoaxial dislocation. Paediatr Neurosurg. 2007;43(1):15-18.
46. Kothari M., Goel A. Maternalizing the meninges: a pregnant Arabic legacy. Neurol India. 2006;54(4):345-346.
47. Kothari M., Goel A. “Aqualisation” of neuraxis: wondrous neuraqua CSF. Neurol India. 2008;56(1):1-3.
48. Ghanayem A.J., Leventhal M., Bohlman H.H. Osteoarthrosis of the atlantoaxial joints. Long-term follow-up after treatment with arthrodesis. J Bone Joint Surg Am. 1996;78:1300-1307.
49. Isono M., Ishii K., Kamida T., et al. Retro-odontoid soft tissue mass associated with atlantoaxial subluxation in an elderly patient: a case report. Surg Neurol. 2001;55:223-227.
50. Lagares A., Arrese I., Pascual B., et al. Pannus resolution after occipitocervical fusion in a non-rheumatoid atlanto-axial instability. Eur Spine J. 2006;15:366-369.
51. Goel A., Shah A., Rajan S. Craniovertebral instability secondary to degenerative osteoarthritis of the atlantoaxial joints: analysis of the management of 108 cases. J Neurosurg Spine. 2010;12(6):592-601.
52. Finn M., Fassett D.R., Apfelbaum R.I. Surgical treatment of nonrheumatoid atlantoaxial degenerative arthritis producing pain and myelopathy. Spine. 2007;32:3067-3073.
53. Menezes A.H., Van Gilder J.C., Clark C.R. Odontoid upward migration in rheumatoid arthritis: an analysis of 45 patients with “cranial settling.”. J Neurosurg. 1985;63:500-509.
54. Cai C.Y., Palmer C.A., Paramore C.G. Exuberant transverse ligament degeneration causing high cervical myelopathy. J Spinal Disord. 2001;14:84-88.
55. Birch B.D., Khandji A.G., McCormick P.C. Atlantoaxial degenerative articular cysts. J Neurosurg. 1996;85:810-816.
56. Fransen P., Pizzolato G.P., Otten P., et al. Synovial cyst and degeneration of the transverse ligament: an unusual cause of high cervical myelopathy. Case report. J Neurosurg. 1997;86:1027-1030.
57. Kaufmann A.M., Halliday W.C., West M., et al. Periodontoid synovial cyst causing cervico-medullary compression. Can J Neurol Sci. 1996;23:227-230.
58. Okamoto K., Doita M., Yoshikawa M., et al. Synovial cyst at the C1-C2 junction in a patient with atlantoaxial subluxation. J Spinal Disord Tech. 2004;17:535-538.
59. Ranawat C.S., O’Leary P., Pellicci P., et al. Cervical spine fusion in rheumatoid arthritis. J Bone Joint Surg Am. 1979;61:1003-1010.
60. Yamaguchi I., Shibuya S., Arima N., et al. Remarkable reduction or disappearance of retroodontoid pseudotumors after occipitocervical fusion. Report of three cases. J Neurosurg Spine. 2006;5:156-160.
61. Nguyen H.V., Ludwig S.C., Silber J., et al. Rheumatoid arthritis of the cervical spine. Spine. 2004;4:329-334.
62. Casey A.T., Crockard H.A., Geddes J.F., Stevens J. Vertical translocation: the enigma of the disappearing atlantodens interval in patients with myelopathy and rheumatoid arthritis. Part I. Clinical, radiological, and neuropathological features. J Neurosurg. 1997;87:856-862.
63. Kawaida H., Sakou T., Morizono Y. Vertical settling in rheumatoid arthritis: diagnostic value of Ranawat and Redlund-Johnell methods. Clin Orthop. 1989;239:128-135.
64. Grob D., Schutz U., Plotz G. Occipitocervical fusion in patients with rheumatoid arthritis. Clin Orthop. 1999;366:46-53.
65. Grob D., Wursch R., Grauer W., et al. Atlantoaxial fusion and retrodental pannus in rheumatoid arthritis. Spine. 1997;22:1580-1583.
66. Goel A., Pareikh S., Sharma P. Atlantoaxial joint distraction for treatment of basilar invagination secondary to rheumatoid arthritis. Neurol India. 2005;53(2):238-240.
67. Goel A., Sharma P. Craniovertebral realignment for basilar invagination and atlantoaxial dislocation secondary to rheumatoid arthritis. Neurol India. 2004;52(3):338-341.