Chapter 8 Cosmeceutical Vitamins: Vitamin C
INTRODUCTION
Vitamin C is a naturally occurring antioxidant incorporated into cosmeceuticals for the purpose of preventing and treating sun-damaged skin. Most plants and animals have the capacity to synthesize vitamin C. In humans, however, vitamin C cannot be synthesized because of loss of the ability to produce L-glucono-gamma-lactone oxidase, the enzyme necessary for its production. Vitamin C must instead be obtained from dietary sources such as citrus fruits and leafy green vegetables (Fig. 8.1). Interestingly, oral supplementation with vitamin C produces only a limited increase in skin concentration. This is because even with ingestion of massive doses, the absorption of vitamin C is limited by active transport mechanisms in the gut. Therefore, vitamin C has become a popular topically applied cosmeceutical.
VITAMIN C: EFFECTS ON COLLAGEN AND ELASTIN SYNTHESIS
Vitamin C is essential for collagen biosynthesis. Ascorbate serves as a cofactor for prolyl and lysyl hydroxylase, the enzymes responsible for stabilizing and cross-linking collagen. Ascorbate can also stimulate collagen synthesis directly by activating its transcription and stabilizing procollagen mRNA. Scurvy serves as prototype for the physiologic changes that occur when vitamin C is lacking and collagen biosynthesis is impaired.
PHOTOPROTECTION BY VITAMIN C
In addition to topical vitamin C, some have advocated that oral supplementation may be useful for photoprotection and even skin cancer prevention. In mice, dietary supplementation with vitamin C reduced the incidence of UV light-induced skin neoplasms although similar effects have not been documented in humans. Patients taking vitamin C supplements demonstrated a significant rise in plasma and skin vitamin C content but the vitamins failed to confer any protective effect against sunburn threshold. In contrast, two studies have reported protection against UV-induced erythema following supplementation with both vitamin C and vitamin E. Thus, the benefits of oral supplementation may be enhanced by combination therapy. Further studies elucidating the role of vitamin supplements for photoprotection are clearly warranted.
DELIVERY AND METABOLISM OF L-ASCORBIC ACID AND DERIVATIVES
• Magnesium ascorbyl phosphate
In vitro studies utilizing human fibroblasts demonstrated that MAP is equivalent to ascorbic acid in its ability to stimulate collagen synthesis. These findings were confirmed by additional studies that demonstrated enhanced collagen synthesis and cell growth of cultured fibroblasts treated with MAP. Finally, in vitro studies demonstrated that MAP phosphate regulates type I collagen production.
CLINICAL STUDIES REGARDING TOPICAL VITAMIN C
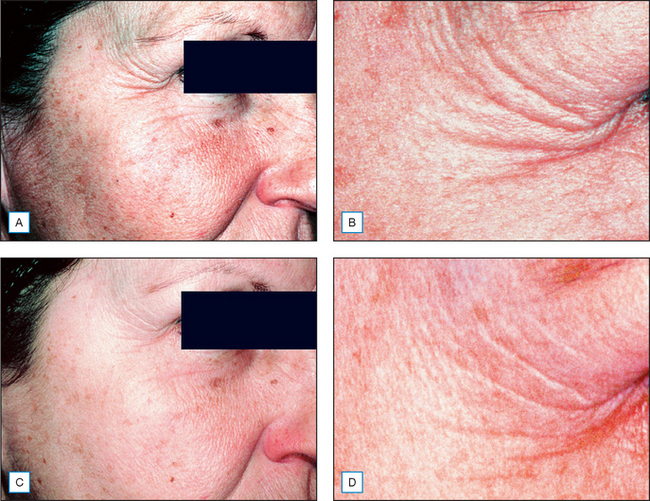
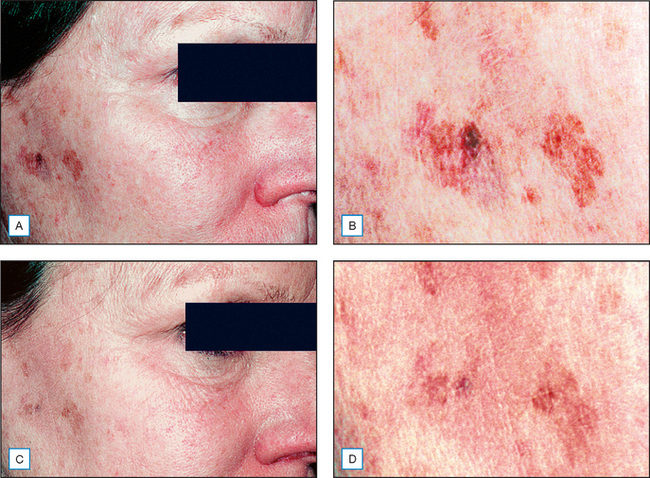
Clinical studies have investigated the cosmeceutical effect of products containing L-ascorbic acid. A 3-month, double-blind, randomized, vehicle-controlled study was performed on 19 patients aged between 36 and 72 years with moderately photodamaged facial skin. Patients applied topical ascorbic acid 10% (Cellex-C high-potency serum, Cellex-C International, Toronto, Ontario) or vehicle serum to half the face for 3 months. Optical profilometry image analysis demonstrated a statistically significant improvement in the vitamin C-treated side when compared to control. Clinical assessment showed significant improvement in fine wrinkling, tactile roughness, coarse rhytides, skin laxity/tone, sallowness/yellowing, and overall features on the side treated with active. Photographic assessment showed a 57.9% improvement in the vitamin C-treated group compared to control. The patients shown in Figures 8.2 and 8.3 demonstrate the type of clinical improvement that can be expected with continued use of topical L-ascorbic acid. The patient in Figure 8.2 shows vastly improved periorbital wrinkles while the patient in Figure 8.3 demonstrates a significant lightening of actinically induced mottled hyperpigmentation.
Fitzpatrick and Rostan reported a double blind, half face study of 10 patients treated with a new formulation containing 10% L-ascorbic acid and 7% tetrahexyldecyl ascorbate in an anhydrous polysilicone gel base. The inactive polysilicone gel base served as a control on the opposite side. Clinical evaluations were performed at 4, 8, and 12 weeks and punch biopsies were performed. There was overall improvement on the vitamin C-treated side that was statistically significant when compared to vehicle at 12 weeks. The vitamin C-treated side showed a decrease in photoaging score on the cheeks and perioral area. The periorbital areas improved on both sides, which the authors contribute to improved hydration. Skin biopsies after vitamin C treatment showed an increase in grenz zone collagen and increased staining for mRNA for type I collagen.
An innovative use for topical L-ascorbic was described by Alster and West who evaluated its efficacy for treating post-CO2 laser resurfacing erythema. Split face studies showed a significant decrease in post-CO2 laser resurfacing erythema by the eighth postoperative week in patients treated with an aqueous solution containing topical 10% L-ascorbic acid, 2% zinc sulphate, and 0.5% tyrosine. Interestingly, the same formulation in a cream base did not improve post-laser erythema.
Alster TS, West TB. Effect of topical vitamin C on postoperative carbon dioxide laser resurfacing erythema. Dermatologic Surgery. 1998;24:331–334.
Austria R, Semenzato A, Bettero A. Stability of vitamin C derivatives in solution and topical formulations. Journal of Pharmaceutical and Biomedical Analysis. 1997;15:795–801.
Carcamo JM, Pedraza A, Borquez-Ojeda O, Golde DS. Vitamin C suppresses TNF alpha-induced NF kappa B activation by inhibiting I Kappa B alpha phosphorylation. Biochemistry. 2002;41:12995–30002.
Darr D, Combs S, Dunston S, Manning T, Pinnell S. Topical vitamin C protects porcine skin from ultraviolet radiation-induced damage. British Journal of Dermatology. 1992;127:247–253.
Dunham WB, Zuckerkandl E, Reynolds R, et al. Effects of intake of L-ascorbic acid (vitamin C) on the incidence of dermal neoplasms induced in mice by ultraviolet light. Proceedings of the National Academy of Sciences USA. 1982;79:7532–7536.
Eberlein-Konig B, Placzek M, Przybilla B. Protective effect against sunburn of combined systemic ascorbic acid (vitamin C) and d–alpha-tocopherol (vitamin C). Journal of the American Academy of Dermatology. 1998;38:45–48.
Fisher GJ, Kang S, Varani J, et al. Mechanisms of photoaging and chronological skin aging. Archives of Dermatology. 2002;138:1462–1470.
Fitzpatrick RE, Rostan EF. Double-blind, half-face study comparing topical vitamin C and vehicle for rejuvenation of photodamage. Dermatologic Surgery. 2002;28:231–236.
Haywood R, Wardman P, Sanders R, Linge C. Sunscreens inadequately protect against ultraviolet A-induced free radicals in skin: implications for skin aging and melanoma? Journal of Investigative Dermatology. 2003;121:862–868.
Humbert PG, Haftek M, Creidi P, et al. Topical ascorbic acid on photoaged skin. Clinical, topographical and ultrastructural evaluation: double-blind study vs. placebo. Experimental Dermatology. 2003;12:237–244.
Kameyama K, Sakai C, Kondoh S, et al. Inhibitory effect of magnesium L-ascorbyl-2-phosphate (VC-PMG) on melanogenesis in vitro and in vivo. Journal of the American Academy of Dermatology. 1996;34:29–33.
Lin JY, Selim MA, Shea CR, et al. UV photoprotection by combination topical antioxidants vitamin C and vitamin E. Journal of the American Academy of Dermatology. 2003;48:866–867.
Lind FH, Lind JY, Gupta RD, et al. Ferulic acid stabilizes a solution of vitamins C and E and doubles its photoprotection of skin. Journal of Investigative Dermatology. 2005;125:826–832.
McCardle F, Thodes LE, Parslew R, et al. UVR-induced oxidative stress in human skin in vivo: effects of oral vitamin C supplementation. Free Radical Biology and Medicine. 2002;33:1355–1362.
Perricone NV. Topical vitamin C ester (ascorbyl palmitate). Journal of Geriatric Dermatology. 1997;5:162–170.
Pinnell SR. Cutaneous photodamage, oxidative stress and topical antioxidant protection. Journal of the American Academy of Dermatology. 2003;48:1–19.
Pinnell SR, Yang HS, Omar M, et al. Topical L-ascorbic acid percutaneous absorption studies. Dermatologic Surgery. 2001;27:137–142.
Shindo Y, Witt E, Hans D, et al. Enzymic and nonenzymic antioxidants in epidermis and dermis of human skin. Journal of Investigative Dermatology. 1994;102:122–124.
Tournas JA, Fu-Hsiung L, Burch JA, et al. Ubiquinone, idebenone and kinetin provide ineffective photoprotection to skin when compared to a topical antioxidant combination of vitamins C and E with ferulic acid. Journal of Investigative Dermatology. 2006;126:1185–1187.