CHAPTER 27 Coronoid Process and Monteggia Fractures
THE CORONOID
As this fracture often occurs in conjunction with radial head fractures and dislocation; it is also discussed in the chapter on complex instability (see Chapter 29).
MECHANISM OF INJURY
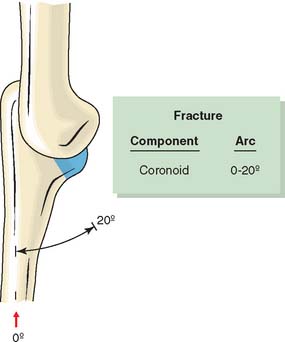
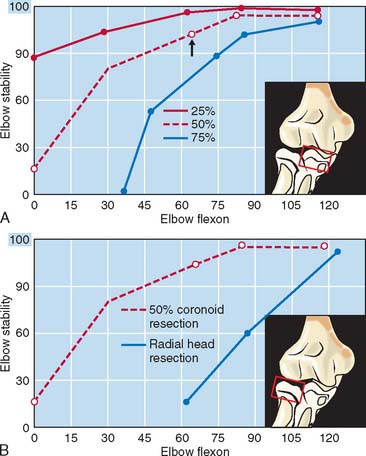
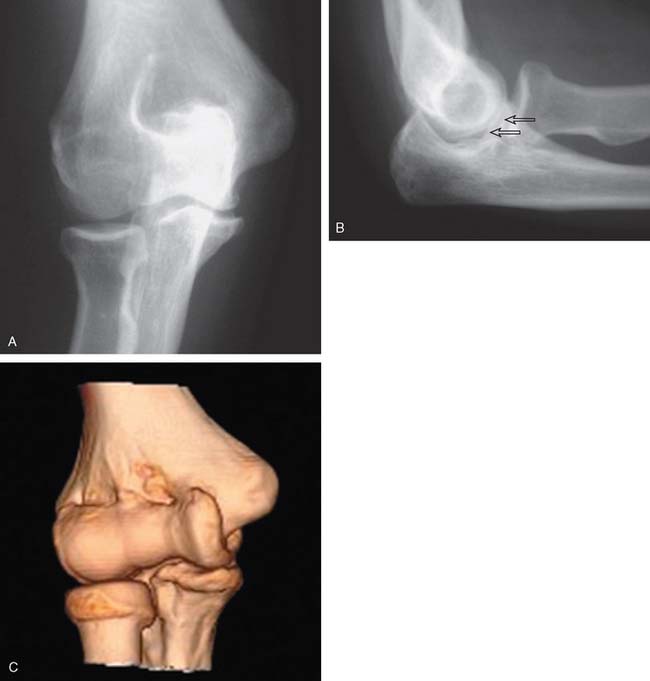
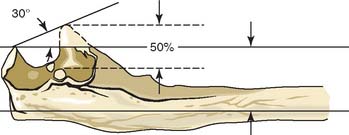
Isolated coronoid fractures are uncommon and usually occur in association with elbow dislocation.49,59 One recent review of 120 complex elbow injuries identified 21% with coronoid and radial head fractures, 19% with olecranon and radial head fracture and 33% with radial head, olecranon and coronoid fracture.20 One group identified three of eight isolated coronoid fractures.23 Theoretically, the coronoid is fractured with the elbow in 0 to 20 degrees of flexion during an axial load (Fig. 27-1).1 This is a mechanism similar to that in elbow dislocation. With flexion past 30 degrees, radial head fractures occur. The combination of coronoid and radial head fracture has important implications for treatment, as discussed in Chapter 29. Of particular note is the fact that fractures involving more than 50% of the coronoid (Regan/Morrey type II) are associated with marked elbow instability, especially if the radial head has been resected (Fig. 27-2).12,13,36
INCIDENCE
Fractures of the coronoid process are uncommon. This may occur with a comminuted olecranon or proximal ulnar fracture (Fig. 27-3). The injury has also been reported in 2% to 10% of patients with dislocation of the elbow. Our review of 293 acute radial head fractures documented 33 (11%) concurrent coronoid fractures (see Chapter 24).64 Since the initial series of 35 patients,49 a few case reports19,61 and small series have appeared.23,31,56
CLASSIFICATION
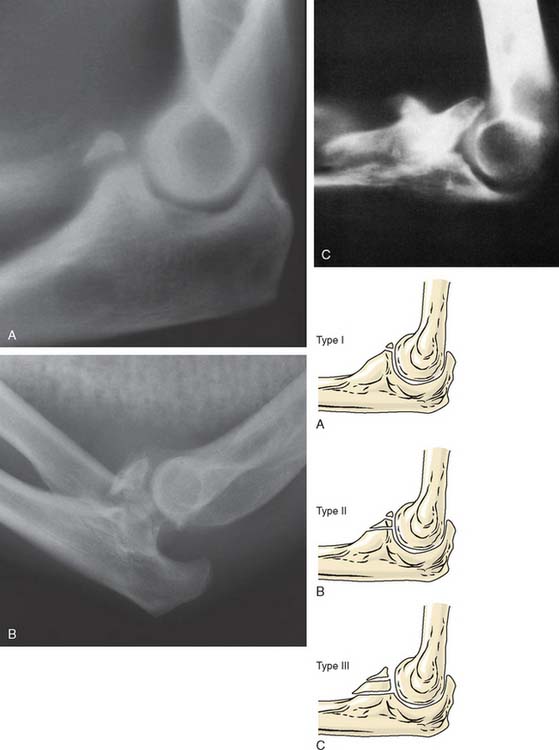
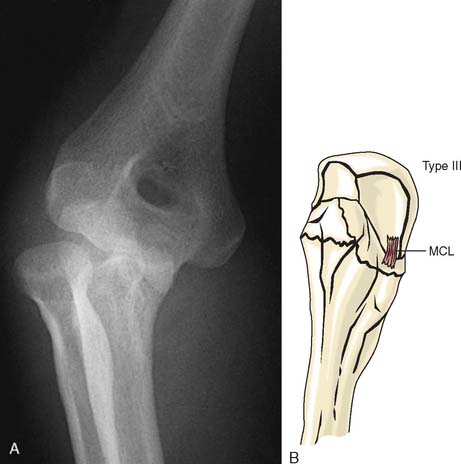
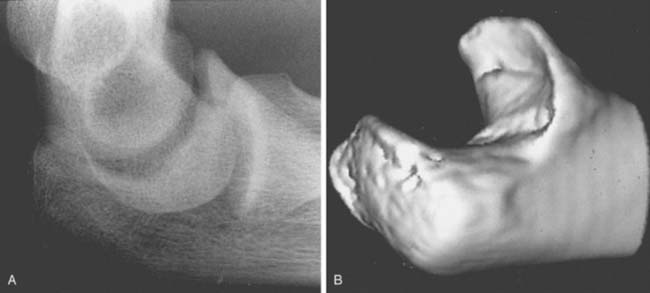
Review of Mayo records resulted in a simple classification of coronoid fractures as well as a rationale for treatment (Fig. 27-4). Type I is a fracture of the tip of the coronoid process caused by a shearing force as the coronoid process subluxates or dislocates over the trochlea. A type II injury involves a single or comminuted fragment constituting about half of the coronoid. A type III fracture involves more than half of the coronoid process. The type II or III fracture may be comminuted, and all three may be associated with dislocation of the elbow or with other injuries. Comminution in the sagittal plane, often involving the medial portion of the coronoid and sometimes even involving the sublime tubercle, has been documented58 (Fig. 27-5). Subtle medial coronoid fractures have also been documented. A hint of such an injury is the appearance of the so-called double crescent sign (Fig. 27-6).
ASSOCIATION INJURIES
With type I fractures, or any coronoid fracture, one must assume that the elbow has dislocated. Even if dislocation did not occur, some injury to the ligament is present, even if only a strain. Furthermore, 35% of the patients with type I, 56% of the patients with type II, and 80% of the patients with type III coronoid fractures had other identified injuries.49 In fact, today an isolated injury is considered a rarity and other pathology must be sought if it is not obvious.
Our current management philosophy is governed by our clinical experience and by basic investigational data (see Chapter 3).26,31,37,46 Simply put, first and foremost, a stable ulnohumeral joint must be attained and maintained. This means
TREATMENT
Authors’ Preference
Type I
The patient with type I fracture is treated according to the concurrent pathology. The fracture itself indicates that the elbow has dislocated and should be managed on that basis. One recent report has implicated the fragment as a source of catching or impingement, both responding to arthroscopic excision.29 It does not need to be fixed acutely.
Type II
Type II fractures should be treated with early motion unless the elbow is unstable. Typically involving more than 50% of the coracoid, screw fixation is effective if the fragment is not comminuted. If comminuted, a suture or a buttress plate are both effective options, and a distraction device can be used to provide the initial stability while the soft tissue heals. Fixation of the smaller fragments alone may not stabilize the joint but should be considered if technically feasible. As a useful clinical tool, we have observed that determining the rotational stability is assisted by a line from the tip of the olecranon through the residual coronoid. If this is parallel to the long axis of the ulna, a type II or a 50% fracture has occurred and the joint is potentially unstable (Fig. 27-7).
Type III
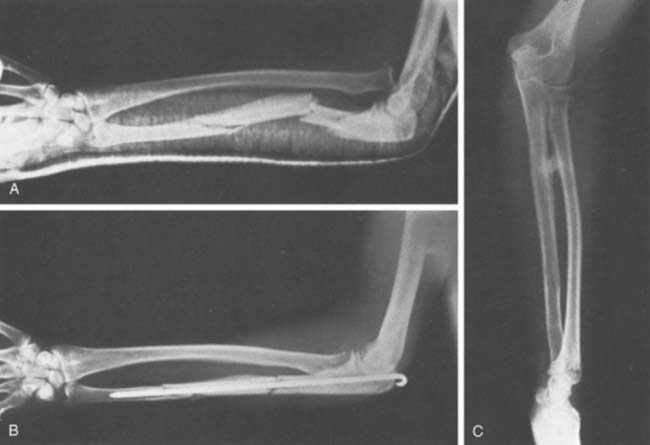
Type III fractures are always associated with elbow instability. If the fracture is comminuted and is not amenable to fixation, the suture or buttress plate options are employed and an external fixation device is mandatory. Failure to stabilize the elbow in type III fractures results in a painful subluxation of the ulnohumeral joint, usually with marked limitation of motion (Fig. 27-8). Hence, open reduction and rigid fixation, with or without the distraction device, remains the treatment of choice.
Note: The most important point is that the acute injury must be properly managed. Outcomes of acute management are orders of magnitude better than those of delayed reconstruction.23,42,52,56,67
Technique
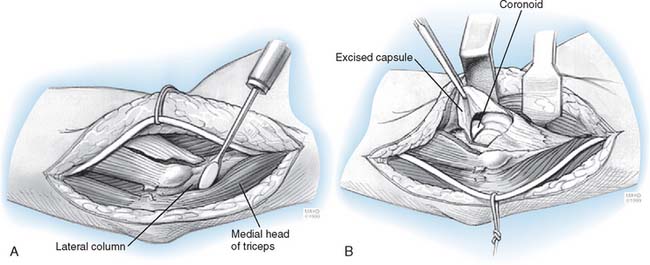
If the radial head is fractured or the elbow is grossly unstable, exposure and fixation of the coronoid is facilitated. We still usually use a straight posterior skin incision. Kocher’s interval is used if the radial head is fractured. If the fracture is an isolated one, a medial approach is used (see Chapter 7). This is mandatory if a sagittal component is present and if the medial collateral ligament is involved.
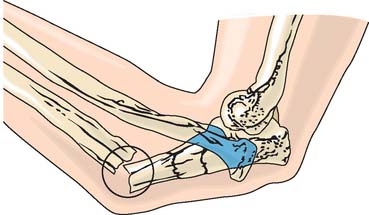
With the use of the posterior incision, the ulnar nerve is exposed but not transferred. The flexor-pronator origin is released with a 1-cm cuff of tendon left on the medial epicondyle (Fig. 27-9). The brachialis muscle is elevated from the capsule, and the joint entered. Fixation is ideally accomplished with one or two compression screws (Fig. 27-10). With comminuted fractures, a heavy No. 5 nonabsorbable suture may be placed through the brachialis tendon, and then through the fracture, and is secured through drill holes in the ulna through the base of the fracture (Fig. 27-11). A buttress plate is also effective (Fig. 27-12).
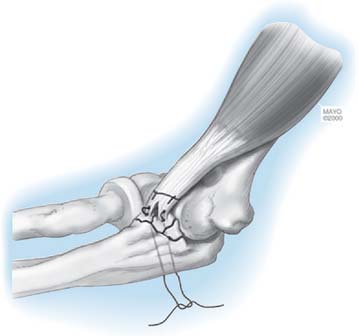
FIGURE 27-11 A suture through the brachialis tendon may be used to secure badly comminuted fracture fragments.
Reconstruction
An absent coronoid may be reconstructed with a well-fashioned bone graft from the ilium. Moritomo and colleagues35 have also described reconstruction with the osteotomized portion of the olecranon. But in general, reconstruction is unreliable. Using an osteochondral graft is successful in only about 50% of cases. More complex reconstruction has also been assessed42 with better outcomes being realized if the coracoid, radial head, and collateral ligaments are all addressed at the time of the injury.42,53,54
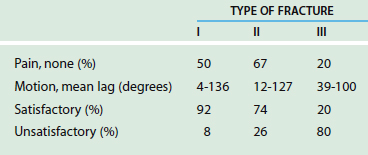
RESULTS
The results of 35 patients with acute coronoid fractures treated at Mayo are shown in Table 27-1. Using an elbow performance index, it is obvious that the chance of a satisfactory result directly correlates with the severity of the injury, as reflected by the coronoid fracture type. Pain is uncommon in type I and typical in type III injury. Our impression is that the results have improved over the last decade owing to (1) a better understanding of the implications of associated injury, (2) more aggressive exposure, and (3) improved design of internal and external fixation systems. Hence, the reports by both Ring et al55 and Pugh et al46 on 80% satisfactory outcomes following the above-mentioned principles when employed for acute fracture management.
Stress Fracture
Although reported for the olecranon,30,68 stress fracture has not been reported for the coronoid. We have, however, documented one instance occurring in a young 17-year-old female gymnast (Fig. 27-13). Symptoms resolved and full activity returned with cessation of activity for 3 months.
MONTEGGIA FRACTURE
Giovanni Battista Monteggia of Milan first described the injury that bears his name in 1814,33 the same year that Colles described his fracture. Monteggia initially reported on a fracture of the ulna associated with anterior dislocation of the radial head, which is today recognized as the most common of the Monteggia lesions, a term coined by Bado4 that includes all ulnar fractures associated with dislocations of the radiocapitellar articulation. These lesions are uncommon (7% of ulnar fractures, 0.7% of elbow injuries5) but are difficult to manage properly.
CLASSIFICATION
Depending on the type of dislocation of the radial head (anterior, posterior, and lateral), three distinct types of injuries were recognized early. Bado4 subsequently proposed a classification that encompasses the full spectrum of these injuries and has become universally accepted.
Type I
Type I injury is an anterior dislocation of the radial head associated with a fracture of the ulnar diaphysis at any level with anterior angulation (Fig. 27-14). This is the most common type of lesion (55% to 78% of Monteggia fractures, depending on the series) and is most common in children.
Type II
Type II injury is a posterior or posterolateral dislocation of the radial head associated with a fracture of the ulnar diaphysis with posterior angulation (Fig. 27-15). Usually it is more proximal. The lesion occurs most commonly in adults, with a frequency of about 10% to 15% of cases.
Type III
Type III injury is a lateral or anterolateral dislocation of the radial head associated with a fracture of the ulnar metaphysis (Fig. 27-16). Athough it is more common in children, it occurs with a frequency of 6.7% to 20% percent of cases.
Type IV
Type IV fracture, the rarest type (5% of cases), consists of an anterior dislocation of the radial head associated with a fracture of the proximal third of the radius and a fracture of the ulna at the same level (Fig. 27-17).
Equivalents
Bado also described equivalents to type I and II injury (according to him, types III and IV have no equivalents). Unfortunately, these so-called equivalents may have added uncertainty to our thinking, because the scheme attempts to account for virtually all other proximal ulna-radial fracture dislocations. With expanded classifications of olecranon, coronoid fractures and a better understanding of “complex instability,” the reliability of the so-called variants has become questionable.
MECHANISM OF INJURY
The greatest controversy concerns the type I lesion. A direct blow to the posterior aspect of the ulna seems to be the probable mechanism in most cases. However, a fall on the outstretched hand with the forearm in pronation may be the most common mechanism. Evans16 postulated that with such a fall, in which the hand is fixed to the ground by the weight of the body, the full pronation of the forearm is exaggerated by external rotation of the arm on the hand, and an oblique fracture of the ulna occurs. At the same time, the radius, forced into extreme pronation, crosses the ulna at the junction of the middle and proximal thirds. This contact acts as a fulcrum, forcing the proximal radius anteriorly to dislocate its head or to fracture, or, exceptionally, to do both (type IV). Evans carried out cadaver experiments that produced Monteggia type I or equivalent lesions in 17 of 18 attempts, confirming his hypothesis. Tompkins,65 on the other hand, postulated that with a fall on the outstretched hand, the radial head is dislocated by a violent reflex contraction of the biceps; this causes all the weight to be borne by the ulna, and, because of the longitudinal compressive force combined with the pull of the interosseous membrane and the simultaneous contracting brachialis, the ulna fractures and angulates anteriorly. Thus, the mechanism is one of hyperextension. This theory, if correct, would have implications for treatment, because flexion of 100 to 110 degrees would seem to be necessary after reduction to avoid redislocation of the radial head. It is likely that all three mechanisms (direct blow to the ulna, hyperpronation, and hyperextension) could cause a type I Monteggia fracture.
Type II injuries occur more often among middle-aged women, in whom ligamentous attachments of the proximal ulna are stronger than the ulna itself.45 This explains the mechanism of injury, which, similar to that in a posterior elbow dislocation, was confirmed by Penrose in cadaver experiments. Bado believed that these injuries are caused by a direct and supination rotational force,4 but that this has not been proved.
The mechanism of injury in type III fractures is a direct blow on the inner side of the elbow with or without rotation.4
RADIOLOGIC FINDINGS
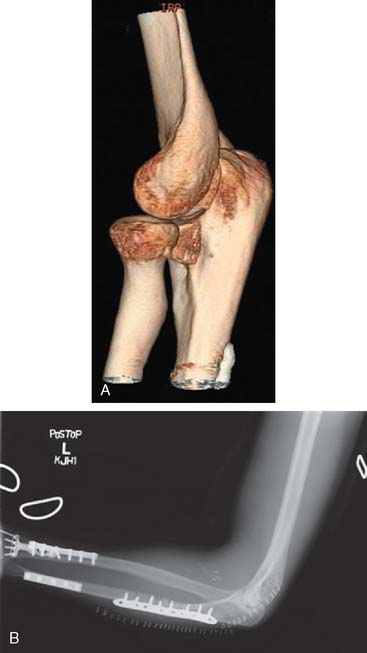
Adequate imaging is essential. Plane radiographs in two planes, including the elbow and wrist joints, are essential. The ulnar fracture is easy to recognize, but the dislocation of the radial head may be missed. This must be avoided, because it directly influences treatment and outcome. This occurs (1) as a result of poor-quality views, (2) particularly if the displacement is mild, (3) if the dislocation has been reduced inadvertently by a previous examiner or at the time of positioning the patient for the x-ray examination,2 or (4) if true biplanar views are not obtained. The Campbell Clinic experience in 1940 revealed that 52% of injuries were not diagnosed until 4 weeks after injury62; this incidence had decreased to 24 percent when Boyd and Boals8 reported on an expanded series of 159 lesions in 1965. Mobley and Janes32 reported that 5 of 15 patients (33%) had old lesions, and Reckling and Cordell48 found that 4 of 25 (16%) had missed lesions. Today, a CT study, especially with three-dimensional reconstruction, readily describes the full extent of the osseous injury and eliminated prior concerns (Fig. 27-18).
TREATMENT
HISTORICAL PERSPECTIVE
Watson-Jones anticipated an unfavorable outcome from this injury, causing permanent disability in 95%. In spite of contrary opinions,4,16 Speed and Boyd62 in 1940 concluded that closed treatment is unsatisfactory and advocated open reduction and internal fixation of the ulna and reconstruction of the annular ligament. In 1969, Boyd and Boals8 recommended open reduction and internal fixation of the ulna with a compression plate or an intramedullary nail, but they suggested that closed reduction of the radial head was usually adequate and open reduction usually unnecessary. If a fracture of the radial head was present, they suggested excision. They found the Boyd7 approach to the ulna and proximal third of the radius satisfactory and obtained excellent or good results in 77% of acute lesions.
As early as 1951, Penrose44 advised open reduction and internal fixation of the ulnar fracture combined with partial or total radial head excision (if the radial head was fractured) for type II injuries. Pavel43 and others,10,47 however, reported poor results after early radial head excisions for these injuries.
Bado4 suggested closed treatment for type II injuries with manipulation by gentle traction and pronation to reduce the dislocation. If the ulnar fracture is not reduced, he advised intramedullary nailing. He also mentioned that results of treatment are less satisfactory with this type of injury.
Reckling, in a study reported in 196848 and expanded in 1982,47 showed that the results of treatment of Monteggia lesions in adults were uniformly worse than those in children and that the best results were obtained with open anatomic reduction of the ulnar fracture, internal fixation, and complete closed reduction of the radial head dislocation. Yet, only 9 of 40 adult patients obtained excellent results.
Type III injuries are almost exclusively found in children. Bryan,10 however, reported three such injuries in adults, two treated surgically with good results and one by closed means with a poor result.
RECENT EXPERIENCE
Surprisingly and unfortunately, more recent reports continue to yield disappointing outcomes. One large study of 67 fractures reported only 54% satisfactory results at 1 to 14 years.51 The best results were in types I and III, with poorer outcomes after types II and IV fractures. In contrast, others have found the worse results after type I injury. A study from Israel described 41 patients—14 children and 27 adults—and emphasized that the type I fracture particularly requires careful monitoring and attention to the radial head.18 The principles of early recognition of proximal radioulnar dissociation and open reduction and internal fixation of the ulnar fracture in the adult are well accepted.55 The key is accurate linear, angular, and rotational alignment of the ulna. This is essential to avoid the major problem of radial head malalignment and instability.
COMPLICATIONS
Complications with this fracture remain all too com-mon. One comprehensive study documented 43% complications and 46% unsatisfactory results after 67 fractures.51
Radial neuropathy, particularly that involving the posterior interosseous branch, has been reported rather frequently.9,10,24,32,63 Causes of the deficit are direct trauma, compression of the nerve in the arcade of Frohse, or, most commonly, stretching of the nerve by a laterally dislocated radial head (the nerve lesion that is most common with type III Monteggia lesions). Its incidence has been as high as 20% of acute lesions. The prognosis is usually good, with complete recovery by 6 to 8 weeks.24 Exploration of the posterior interosseous nerve is advisable when no evidence of recovery is present by 8 to 10 weeks. Tardy permanent plasy of the radial nerve after a Monteggia fracture is uncommon28 and typically occurs after an old unreduced lesion with long-standing dislocation of the radial head. Improvement has occurred after exploration of the radial nerve and excision of the radial head, which compresses the nerve during movements of pronation and supination.
Median24 and ulnar10,32 nerve palsies are uncommon with Monteggia lesions.
UNION AND STABILITY
Gross malunion of the ulna is seldom seen today in the adult, but recurrent dislocation or subluxation of the head of the radius is a common problem. This is usually the result of minor imperfections in the reduction of the ulna. In this age group, a properly performed ulnar osteotomy may be successful in allowing radial head reduction and hence restoring function.22
Ectopic bone formation is common and can be extensive (Fig. 27-19) or present as a single cross-union (Fig. 27-20). The Boyd approach has also been implicated in cross-union in some instances.
Nonunion of the ulna most commonly is related to infection but is also the result of inadequate internal fixation.2 Compression plating, properly executed, produces the lowest rate of nonunion. We have found external fixation useful in the treatment of one infected ununited Monteggia fracture.
REFRACTURE
The incidence of refracture or fracture through a screw hole after forearm fracture is well recognized to occur from 2% to 28%.2,21,34,57 The fracture occurs at the fracture or screw hole with equal frequency.
AUTHORS’ PREFERRED METHOD OF TREATMENT OF MONTEGGIA LESIONS
Principles of treatment of Monteggia lesions in adults are as follows.
Accurate Reduction of the Ulnar Fracture and Maintenance of the Reduction
This essential step is best achieved by rigid, anatomic plating, supplemented by cancellous bone graft if there is significant comminution (see Fig. 27-19). In type IV injuries, if not comminuted, compression plating of the radial and ulnar shaft fractures is the treatment of choice.
1 Amis A.A., Miller J.H. The mechanisms of elbow fractures: An investigation using impact tests in vitro. Injury. 1995;26:163.
2 Anderson L.D. Fractures of the shaft of the radius and ulna. In: Rockwood C.A., Green D.P., editors. Fractures. Philadelphia: J. B. Lippincott Co., 1975.
3 Austin R. Tardy palsy of radial nerve from a Monteggia fracture. Injury. 1976;7:202.
4 Bado J.L. The Monteggia lesion. Clin. Orthop. Relat. Res. 1967;50:71.
5 Beck C., Dabezies E.J. Monteggia fracture-dislocation. Orthopedics. 1984;7:329.
6 Bohler L. The Treatment of Fractures. Vienna: Wilhelm Mandrich, 1929.
7 Boyd H.B. Surgical exposure of the ulna and proximal third of the radius through one incision. Surg. Gynecol. Obstet. 1940;71:86.
8 Boyd H.B., Boals J.C. The Monteggia lesion: A review of 159 cases. Clin. Orthop. 1969;66:94.
9 Bruce H.E., Harvey J.P., Wilson J.C. Monteggia fractures. J. Bone Joint Surg. 1974;56A:1563.
10 Bryan R.S. Monteggia fracture of the forearm. J. Trauma. 1971;11:992.
11 Burghele H., Serban N. Fractures of the olecranon: Treatment by external fixation. Ital. J. Orthop. Traumatol. 1982;8:159.
12 Cheng S., An K.-N., Morrey B.F., O’Driscoll S.W. Biomechanical of the coronoid in complex elbow fracture-dislocations. J. Shoulder Elbow Surg. 1998;793:304.
13 Closkey R.F., Goode J.R., Kirschenbaum D., Cody R.P. The role of the coronoid process in elbow instability: A biomechanical analysis of axial loading. J. Bone Joint Surg. 2000;82A:1749.
14 Cobb T.K., Morrey B.F. Use of distraction arthroplasty in unstable fracture dislocations of the elbow. Clin. Orthop. Relat. Res. 1995;312:201.
15 Conn J., Wade P.A. Injuries of the elbow: A ten-year review. J. Trauma. 1961;1:248.
16 Evans E.M. Pronation injuries of the forearm with special reference to the anterior Monteggia fracture. J. Bone Joint Surg. 1949;31B:578.
17 Fiolle D.J. Note sur les fractures de folecrane par projectiles de guerre. Marseille Med. 1918;55:241.
18 Givon U., Pritsch M., Levy O., Yosepovich A., Amit Y., Horoszowski H. Monteggia and equivalent lesions: A study of 41 cases. Clin. Orthop. Relat. Res. 1997;337:208.
19 Hanks G.A., Kottmeier S.A. Isolated fracture of the coronoid process of the ulna: A case report and review of the literature. J. Orthop. Trauma. 1990;4:193.
20 Heim U. Combined fractures of the radius and the ulna at the elbow level in the adult. Analysis of 120 cases after more than 1 year. Revue de Chirurgie Orthop et Reparatrice de l Appareil Moteur. 1998;84:142.
21 Hidaka S., Gustilo R.B. Refracture of bones of the forearm after plate removal. J. Bone Joint Surg. 1984;66A:1241.
22 Inoue G., Shionoya K. Corrective ulnar osteotomy for malunited anterior Monteggia lesions in children: 12 patients followed for 1-12 years. Acta Orthop. Scand. 1998;69:73.
23 Jeon I.H., Oh C.W., Kyung H.S., Park B.C., Kim P.T., Ihn J.C. Functional outcome after operative treatment of eight type III coronoid process fractures. J. Trauma. 2005;59:418.
24 Jessing P. Monteggia lesions and their complicating nerve damage. Acta Orthop. Scand. 1975;46:601.
25 Joshi R.P. The Hastings experience of the Attenborough springs and Rush nail for fixation of olecranon fractures. Injury. 1997;29:455.
26 Kamineni S., Hirahara H., Neale P., O’Driscoll S.W., An K.-N., Morrey B.F. Effectiveness of the lateral unilateral dynamic external fixator after elbow ligament injury. J. Bone Joint Surg. 2007;89A:1802.
27 Kozin S.H., Berglund L.J., Cooney W.P., Morrey B.F., An K-N. Biomechanical analysis of tension band fixation for olecranon fracture treatment. J. Shoulder Elbow Surg. 1996;5:442.
28 Lichter R.L., Jacobsen T. Tardy palsy of the posterior interosseous nerve with a Monteggia fracture. J. Bone Joint Surg. 1975;57A:124.
29 Liu S.H., Henry M., Bowen R. Complications of type I coronoid fractures in competitive athletes: Report of two cases and review of the literature. J. Shoulder Elbow Surg. 1996;5:223.
30 Maffulli N., Chan D., Aldridge M.J. Overuse injuries of the olecranon in young gymnasts. J. Bone Joint Surg. 1992;74B:305.
31 McKee M.D., Bowden S.H., King G.J., Patterson S.D., Jupiter J.B., Bamberger H.B., Paksima N. Management of recurrent, complex instability of the elbow with a hinged external fixator. J. Bone Joint Surg. 1998;80B:1031.
32 Mobley J.E., Janes J.M. Monteggia fractures. Proc. Staff Meet. Mayo Clin. 1955;30:497.
33 Monteggia G.B.. Instituzioni Chirurgiche, Vol. 5. Maspero, Milan, 1814.
34 Moore T.M., Klein J.P., Patzakis M.J., Harvey J.B. Results of compression plating of closed Galeazzi fractures. J. Bone Joint Surg. 1985;67A:1015.
35 Moritomo H., Tada K., Yoshida T., Kawatsu N. Reconstruction of the coronoid for chronic dislocation of the elbow: Use of a graft from the olecranon in two cases. J. Bone Joint Surg. 1998;80B:490.
36 Morrey B.F. Fractures and dislocations of the elbow. In: Gustilo R.B., editor. Fractures and Dislocations. Chicago: Year Book Medical Publishers, 1992.
37 Morrey B.F. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. J. Bone Joint Surg. 1995;77A:316.
38 Muller M.E., Allgower M., Schneider R., Willenegger H. Manual of Internal Fixation: Techniques Recommended by the AO Group, 2nd ed. New York: Springer-Verlag, 1979.
39 Murphy D.F., Green W.B., Dameron T.B. Displaced olecranon fractures in adults: Clinical evaluation. Clin. Orthop. Relat. Res. 1987;224:215.
40 Murphy D.F., Green W.B., Gilbert J.A., Dameron T.B. Displaced olecranon fractures in adults: Biomechanical analysis of fixation methods. Clin. Orthop. Relat. Res. 1987;224:210.
41 O’Donoghue D.H., Sell L.S. Persistent olecranon epiphysis in adults. J. Bone Joint Surg. 1942;24:677.
42 Papandrea R.F., Morrey B.F., O’Driscoll S.W. Reconstruction for persistent instability of the elbow after coronoid fracture-dislocation. J. Shoulder Elbow Surg. 2007;16:68. (Epub 2006, Oct. 25).
43 Pavel A., Pitman J.M., Lance E.M., Wade P.A. The posterior Monteggia fracture: A clinical study. J. Trauma. 1965;5:185.
44 Penrose J.H. The Monteggia fractures with posterior dislocation of the radial head. J. Bone Joint Surg. 1951;33B:65.
45 Perruelo N.N., Platigorsky H. Fractura de olecranon-olecranectomia. Acta Ortoped. Traumatol. Iberica. 1955;3:12.
46 Pugh D.M., Wild L.M., Schemitsch E.H., King G.J., McKee M.D. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J. Bone Joint Surg. 2004;86A:1122.
47 Reckling F.W. Unstable fracture-dislocation of the forearm (Monteggia and Galeazzi lesions). J. Bone Joint Surg. 1982;64A:857.
48 Reckling F.W., Cordell L.B. Unstable fracture-dislocations of the forearm: The Monteggia and Galeazzi lesions. Arch. Surg. 1968;96:999.
49 Regan W., Morrey B.F. Fractures of the coronoid process of the ulna. J. Bone Joint Surg. 1989;71A:1348.
50 Rettig A.C., Waugh T.R., Evanski P.M. Fracture of the olecranon: A problem of management. J. Trauma. 1979;19:23.
51 Reynders P., De Groote W., Rondia J., Govaerts K., Stoffelen D., Broos P.L. Monteggia lesions in adults: A multicenter Bota study. Acta Orthop. Belgica. 1996;62(suppl 1):78.
52 Ring D., Hannouche D., Jupiter J.B. Surgical treatment of persistent dislocation or subluxation of the ulnohumeral joint after fracture-dislocation of the elbow. J. Hand Surg. 2004;29A:470.
53 Ring D., Jupiter J.B. Reconstruction of posttraumatic elbow instability. Clin. Orthop. Relat. Res. 2000;370:44.
54 Ring D., Jupiter J.B., Sanders R.W., Mast J., Simpson N.S. Transolecranon fracture-dislocation of the elbow. J. Orthop. Trauma. 1997;11:545.
55 Ring D., Jupiter J.B., Waters P.M. Monteggia fractures in children and adults. J. A. A. O. S. 1998;6:215.
56 Ring D., Jupiter J.B., Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J. Bone Joint Surg. 2002;84A:547.
57 Rosson J.W., Shearer J.R. Refracture after the removal of plates from the forearm: An avoidable complication. J. Bone Joint Surg. 1991;73B:415.
58 Sanchez-Sotelo J., O’Driscoll S.W., Morrey B.F. Anteromedial fracture of the coronoid process of the ulna. J. Shoulder Elbow Surg. 2006;15:e5.
59 Scharplatz D., Allgower M. Fracture dislocation of the elbow. Injury. 1975;7:143.
60 Schmickal T., Wentzensen A. Treatment of complex elbow injuries by joint spanning articulated fixator. Unfallchirurg. 2000;103:191.
61 Selesnick F.H., Dolitsky B., Haskell S.S. Fracture of the coronoid process requiring open reduction with internal fixation. J. Bone Joint Surg. 1984;66A:1304.
62 Speed J.S., Boyd H.B. Treatment of fractures of the ulna with dislocation of head of radius (Monteggia fracture). J.A.M.A. 1940;115:1699.
63 Spinner M., Freundlich B.D., Teicher J. Posterior interosseous nerve palsy as a complication of Monteggia fractures in children. Clin. Orthop. 1968;58:141.
64 Terada N., Yamada H., Seki T., Urabe T., Takayama S. The importance of reducing small fractures of the coronoid process in the treatment of unstable elbow dislocation. J. Shoulder Elbow Surg. 2000;9:344.
65 Tompkins D.G. The anterior Monteggia fracture: Observations on etiology and treatment. J. Bone Joint Surg. 1971;53A:1109.
66 van Riet R.P., Morrey B.F., O’Driscoll S.W., van Glabbeek F. Associated injuries complicating radial head fractures: A demographic study. Clin. Orthop. Relat. Res. 2005;441:351.
67 van Riet R.P., Morrey B.F., O’Driscoll S.W. Use of osteochondral bone graft in coronoid fractures. J. Shoulder Elbow Surg. 2005;14:519.
68 Wilkerson R.D., Johns J.C. Non-union of an olecranon stress fracture in an adolescent gymnast: A case report. Am. J. Sports Med. 1990;18:432.
69 Yamamoto K., Yanase Y., Tomihara M. Posterior interosseous nerve palsy as complication of Monteggia fractures. Arch. Jpn. Chir. 1977;46:46.