Coronary circulation and the myocardial conduction system
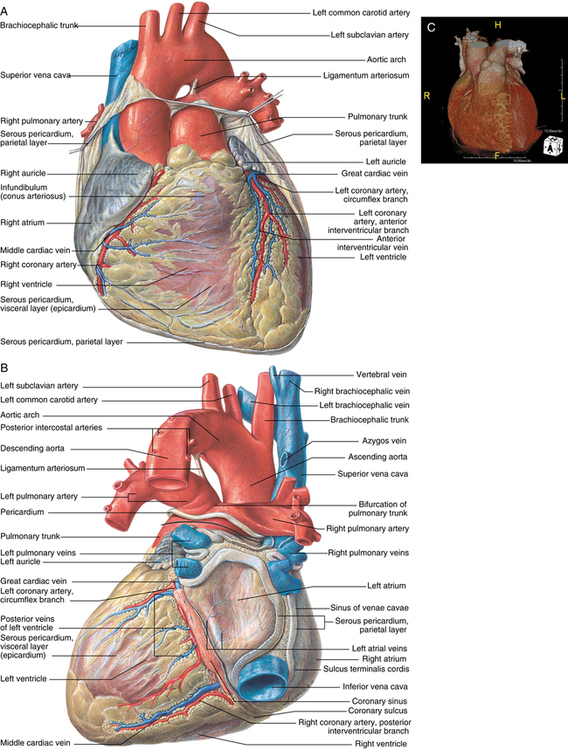
Coronary circulation
The right and left main coronary arteries arise from ostia (small openings) located behind the right and left aortic valve cusps toward the more cephalad portion of the sinus of Valsalva (Figure 52-1). The third aortic cusp is named the posterior or noncoronary cusp. The left main coronary artery travels anteriorly and leftward from the left coronary sinus and, after a 2-mm to 10-mm course between the pulmonary trunk and the left atrium, divides into the left anterior descending (LAD) and left circumflex arteries. Occasionally, a diagonal branch is also present.
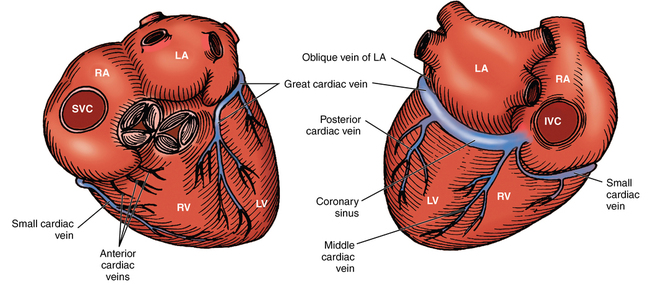
The coronary venous system consists of three primary systems: (1) the coronary sinus, (2) the anterior right ventricular veins, and (3) the thebesian veins (Figure 52-2). The coronary sinus is located in the posterior AV groove and receives blood from the great, middle, and small cardiac veins; the posterior veins of the left ventricle; and the left oblique atrial vein (oblique vein of Marshall). The coronary sinus drains blood primarily from the left ventricle and opens into the right atrium. The two to three anterior right ventricular veins originate in and drain blood from the right ventricular wall. These veins enter the right atrium directly or enter into a small collecting vein at the base of the right atrium. The thebesian veins are tiny venous outlets that drain directly into the cardiac chambers, primarily the right atrium and right ventricle.
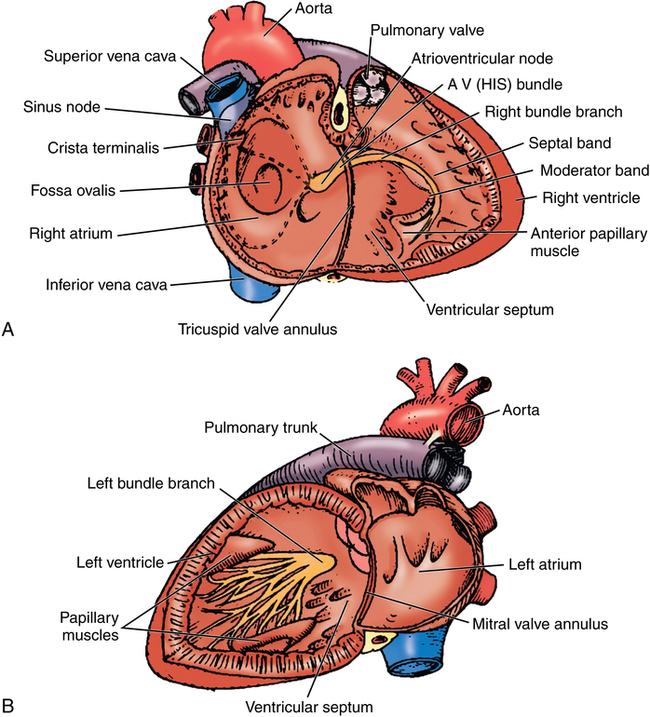
Myocardial conduction system
The SA node is a horseshoe-shaped structure located in the upper part of the sulcus terminalis of the right atrium (Figure 52-3). It extends through the atrial wall from epicardium to endocardium. SA nodal fibers have a higher intrinsic rate of depolarization than do any other cardiac muscle fibers and act as the pacemaker of the heart (see Chapter 33). Three internodal pathways facilitate conduction of impulses between the SA and AV nodes: the anterior (Bachmann bundle), middle, and posterior internodal tracts. The AV node lies in the medial floor of the right atrium at the base of the atrial septum above the orifice of the coronary sinus. The bundle of His begins at the anterior aspect of the AV node and penetrates through the central fibrous body. Here, the bundle of His divides into the left and right branch bundles. The division straddles the upper border of the muscular ventricular septum, and the bundles run superficially down either side of the septum. About midway to the apex, the left bundle divides into the anterior superior and posterior inferior fascicles. These fascicles continue to the base of the papillary muscles of the left ventricle, where they form plexuses of Purkinje fibers that distribute to all portions of the left ventricular myocardium. The right branch bundle continues to the anterior papillary muscle of the right ventricle, where it forms a plexus of Purkinje fibers that distribute to all portions of the right ventricular myocardium.