7 Cornea / External Disease
Anatomy / Physiology
Precorneal Tear Film
Layers
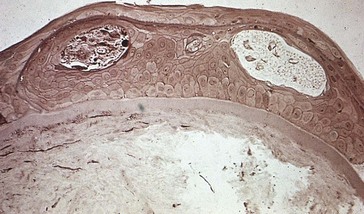
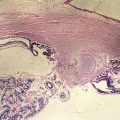
Cornea (Figure 7-1)
Average measurements
Epithelium
50 µm thick (5% of corneal thickness); hydrophobic (hydrophilic molecules penetrate poorly)
Stroma
480 µm thick centrally, 900 µm peripherally; 78% water by weight
Descemet’s membrane
3 (birth) to 12 µm (adults) thick; PAS-positive basement membrane
Endothelium
Conjunctival Disorders
Inflammation
Follicles
Gray-white round elevations with avascular center and vessels at periphery
Generally most prominent in inferior fornix (except in trachoma)
Papillae
Small to large elevations with central vascular tuft and pale avascular valleys
Nonspecific reaction to conjunctival inflammation (edema and leakage of fluid from vessels)
Degenerations
Concretions (Lithiasis)
Small, round, yellow-white deposits in palpebral conjunctiva
May erode through conjunctiva and abrade ocular surface causing foreign body sensation
Conjunctivochalasis
Redundant, loose, nonedematous inferior bulbar conjunctiva interposed between globe and lower eyelid
Pingueculum
Small nodule composed of abnormal subepithelial collagen; may calcify
Located at limbus, nasal more common than temporal; does not involve cornea
Allergy
Allergic Conjunctivitis
20% of the US population has allergies
90% of patients with systemic allergies will have ocular symptoms
Atopic Keratoconjunctivitis (AKC)
Atopy
hereditary allergic hypersensitivity (10–20% of population)
Types I < IV hypersensitivity reactions
Onset usually between ages 30 and 50 years
Clinical diagnosis (atopic skin disease [eczema], hay fever, asthma)
Superior Limbic Keratoconjunctivitis (SLK)
Recurrent inflammation of superior bulbar and palpebral conjunctiva; unknown etiology
Associated with CL wear and thyroid dysfunction (50%)
Female preponderance (70%), onset usually between ages 30 and 55 years
Recurrent episodes; lasts 1–10 years, eventually resolves permanently
Infectious Conjunctivitis
May be hyperacute, acute, or chronic
Usually viral in adults and bacterial in children
Findings
DDx of conjunctivitis with preauricular lymphadenopathy
EKC, HSV, Gonococcus, Chlamydia, Parinaud’s oculoglandular syndrome, Newcastle’s disease
Viral
Adenovirus
Epidemic keratoconjunctivitis (EKC)
Bacterial
Hyperacute (<24 hours)
Copious purulent discharge, marked conjunctival injection and chemosis
Chlamydial
Inclusion Conjunctivitis (TRIC – Trachoma Inclusion Conjunctivitis)
Chlamydia trachomatis serovars D to K
Trachoma
Bilateral keratoconjunctivitis; leading cause of preventable blindness
Chlamydia trachomatis serovars A to C
Classification
Other Conjunctivitis
Staphylococcal Disease
Blepharitis, conjunctivitis, keratitis (SPK, marginal infiltrates), phlyctenule
Tumors
Cystic Tumors
Squamous Tumors
Squamous Papilloma
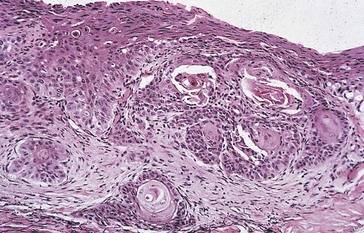
Conjunctival Intraepithelial Neoplasia (CIN)
Replacement of conjunctival epithelium by atypical dysplastic squamous cells
Usually transluscent or gelatinous appearance; <10% exhibit leukoplakia (keratinization)
Carcinoma in situ
Usually begins at limbus and spreads onto cornea
Associated with HPV subtype 16 and 18 (check HIV in young patient), and actinic exposure
Squamous Cell Carcinoma
Malignant cells have broken through epithelial basement membrane
Most common malignant epithelial tumor of conjunctiva; rarely metastasizes
Most common in Africa and Middle East
Mucoepidermoid Carcinoma
Rare, aggresive variant of squamous cell carcinoma with malignant goblet cells
Typically occurs in individuals >60 years old
Very aggressive, can invade globe through sclera
Melanocytic Tumors
Racial Melanosis
Light brown, flat, perilimbal pigmentation; increased melanin in basal epithelium
Nevus
Congenital nests of benign nevus cells along basal epithelial and / or substantia propria
50% have epithelial inclusion cysts
Often enlarges or becomes more pigmented during puberty or pregnancy
Types (classified by location)
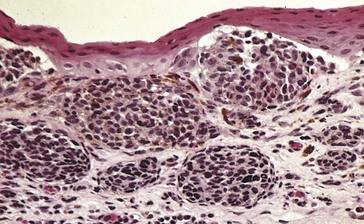
Primary Acquired Melanosis (PAM, Acquired Melanosis Oculi)
Unilateral, flat, diffuse, patchy, brown pigmentation; waxes and wanes
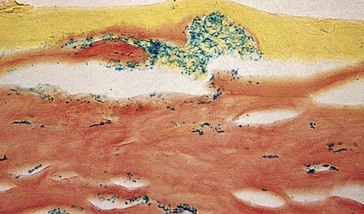
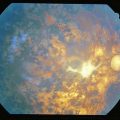
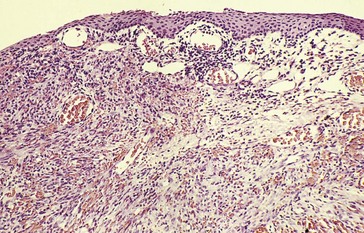
Proliferation of intraepithelial melanocytes; no cysts (Figure 7-8)
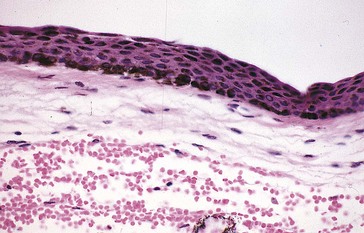
Figure 7-8 PAM with pigmentation throughout the epithelium.
(From Yanoff M, Fine BS: Ocular Pathology, 5th edn, St Louis, Mosby, 2002.)
Analogous to lentigo maligna of skin
Occurs in middle-aged to elderly whites
20–30% risk of malignant transformation, nodular thickening is indication for excisional biopsy
Secondary Acquired Conjunctival Melanosis
Addison’s disease, radiation, pregnancy, topical epinephrine
Malignant Melanoma
Rare, variably pigmented, elevated mass most commonly on bulbar conjunctiva
Arises from PAM (67%) or preexisting nevi (25%), or de novo
Pathology
intraepithelial pagetoid spread; need to bleach specimen to determine amount of atypia (Figure 7-9), stain with S-100 and HMB-45
Vascular Tumors
Kaposi’s Sarcoma
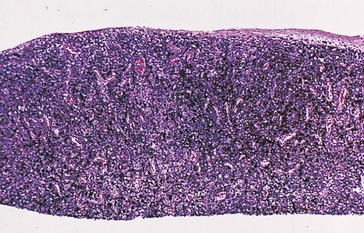
Lymphoid Tumors
(See Ch. 6, Orbit / Lids / Adnexa)
Smooth, flat, fleshy, salmon-colored mass; single or multiple
Occurs in substantia propria; overlying epithelium is smooth; can be bilateral
20% associated with systemic disease (but systemic lymphoma rarely presents in conjunctiva)
Requires systemic workup, including CT scan, bone scan, SPEP, medical consultation
Other Tumors
Benign Hereditary Intraepithelial Dyskeratosis (BHID) (AD)
Originally seen in triracial families in Halifax County, North Carolina (Haliwa Indians)
Corneal Disorders
Trauma
Abrasion
Epithelial defect, most commonly traumatic (e.g. fingernail, plant branch)
Increased risk of infection, especially in contact lens wearer
Foreign Body (FB)
Often metal (usually associated with adjacent rust ring), glass, or organic material
Laceration
Partial- or full-thickness cut in cornea
Burns
Alkali
denatures but does not precipitate proteins, also saponifies fat; therefore penetrates deeply
Radiation
Grading systems
Treatment
Ocular Surface Disease
Causes tear film disturbance and dry eye
Due to deficiency in tear film component(s)
Keratoconjunctivitis Sicca
Xerophthalmia
Epithelial keratinization due to vitamin A deficiency
Incidence 5 million new cases / year; affects 20-40 million children worldwide
Stevens-Johnson Syndrome
Young people; 25% recurrence, 10–33% mortality
Other findings
Ocular Cicatricial Pemphigoid
Bullous disease of mucous membranes resulting in scarring
Usually women age >60 years old
Other findings
Lipid Deficiency
Meibomian gland disease (blepharitis, meibomitis, acne rosacea) (see Ch. 6, Orbit / Lids / Adnexa)
Inflammation
Interstitial Keratitis
Etiology
Can be initiated by minor corneal trauma in patients with congenital syphilis
Cogan’s Syndrome
Ocular inflammation (usually IK) with Meniere’s-like vestibular dysfunction
Thygeson’s Superficial Punctate Keratopathy
Associated with HLA-DR3; 90% bilateral; spontaneous remissions and exacerbations for years
Degenerations
White Limbal Girdle of Vogt
Small, white, fleck and needle-like deposits at temporal and nasal limbus
Pathology: subepithelial elastotic degeneration of collagen (sometimes with calcium particles)
Corneal Arcus
Furrow Degeneration
Thin area peripheral to arcus senilis, more apparent than real; nonprogressive; asymptomatic
Crocodile Shagreen
Mosaic, polygonal, hazy, gray opacities separated by clear zones; ‘cracked-ice’ appearance
Polymorphic Amyloid Degeneration
Bilateral, symmetric, small stellate flecks or filaments in deep stroma
Slowly progressive; usually seen in patients >50 years old; asymptomatic
Spheroidal Degeneration (Labrador Keratopathy, Actinic Keratopathy, Lipid Droplet Degeneration, Bietti’s Hyaline Degeneration, Keratinoid Degeneration)
Depositions
Ochronosis (Alkaptonuria) (AR)
Melanin-like pigment (alkapton; peripheral epithelium and superficial stroma)
Tyrosinemia Type II (Richner-Hanhart Syndrome) (AR)
Deposits in epithelium and subepithelial space due to tyrosine aminotransferase deficiency
Refractile branching linear opacities, may have dendritic pattern
Triad of painful hyperkeratotic skin lesions (on palms and soles), keratitis, and mental retardation
Wilson’s Disease (Hepatolenticular Degeneration) (AR)
Increased copper levels due to deficiency in ceruloplasmin
Ulcers
Peripheral Corneal Ulcers
Mooren’s Ulcer
Chronic, very painful, progressive ulceration
Typically begins nasally or temporally and spreads circumferentially (up to 360°)
Type II hypersensitivity reaction
Associated with hepatitis C, Crohn’s disease, and hydradenitis
Terrien’s Marginal Degeneration
Painless, progressive, bilateral, trough-like stromal thinning; starts superiorly
Marginal Keratolysis / Peripheral Ulcerative Keratitis (PUK)
Ulceration is typically peripheral and unilateral, can be central and bilateral
Due to elevated collagenase; melting stops when epithelium heals
Associated with dry eyes (Sjögren’s) and sytemic disease:
Microbial Keratitis (Infectious Ulcer)
Bacterial
Penetration of intact epithelium
Neisseria, Corynebacterium diphtheriae, Shigella, Haemophilus aegyptus, Listeria monocytogenes
Through epithelial defect
any organism; most commonly Staphylococcus, Streptococcus, and Pseudomonas
Risk factors
corneal trauma or surgery, contact lens wear, epithelial ulceration, dry eye, lid abnormalities
Treatment
Crystalline Keratopathy
Often caused by Streptoccus viridans, also Candida
Associated with chronic topical steroid use (post corneal graft)
Branching, cracked-glass appearance without epithelial defect
Herpes Simplex (HSV)
Often asymptomatic primary infection before age 5 years, 3- to 5-day incubation period
Generally unilateral but can be bilateral (i.e. immunocompromised host)
Seropositivity to HSV is 25% by age 4 years and 100% by age 60 years
Recurrent HSV
due to reactivation of latent virus in trigeminal (Gasserian) ganglion; 4 presentations:
Diagnosis
Treatment
Complications
Major clinical study
Herpetic Eye Disease Study (HEDS)
Herpes Zoster Ophthalmicus (HZO)
Herpes zoster involvement of first branch of trigeminal nerve CN 5 (V1)
May occur without rash (zoster sine herpete)
Most common single dermatome is CN 5: ophthalmic (V1) > maxillary (V2) > mandibular (V3)
3 branches of ophthalmic division: frontal nerve > nasociliary nerve > lacrimal nerve
Findings
Treatment
Complications
occur in 50%; most common is postherpetic neuralgia
| Lesion | HSV Dendrite | HZV Pseudodendrite |
|---|---|---|
| Appearance | Delicate, fine, lacy ulcer | Coarse, ropy, elevated, ’painted-on’ lesion |
| Smaller, less branching than HSV dendrite | ||
| Terminal bulbs | Blunt ends (no terminal bulbs) | |
| Epithelial cells slough | Epithelial cells are swollen and heaped-up | |
| Staining | Base with fluorescein | Poor with fluorescein and rose bengal |
| Edges with rose bengal | ||
| Treatment | Do not use steroids | Good response to steroids |
Note: Active viral replication in epithelial lesions occurs in both HSV and HZV
Other causes of pseudodendrite: Acanthamoeba, tyrosinemia II, epithelial healing ridge
Fungi
Types
Acanthamoeba
22 species; exists as trophozoite or cyst
90% initially misdiagnosed as HSV
Treatment
débridement if infection limited to epithelium (may be curative), topical agents
Epstein-Barr Virus (EBV)
Diagnosis
Ectasias
Keratoconus
90% bilateral; onset typically around puberty
Associations
Keratoglobus
Rare, sporadic, globular corneal deformity
Associated with connective tissue disorders, Leber’s congenital amaurosis
Dystrophies
Inherited genetic disorders (usually defective enzyme or structural protein)
AD except macular, type 3 lattice, gelatinous, and nystagmus-associated form of CHED, which are AR
Anterior
Anterior Basement Membrane (Cogan’s Microcystic; Map-Dot-Fingerprint) (AD)
Most common anterior corneal dystrophy
Usually bilateral, can be asymmetric; primarily affects middle-aged women
Symptoms more common in those >30 years old
Findings
irregular and often loose epithelium with characteristic appearance (map, dot, fingerprint):
Pathology
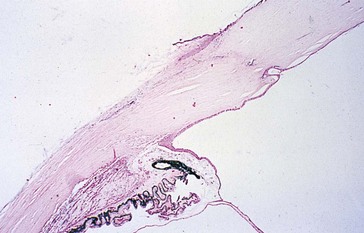
epithelial reduplication with excess subepithelial and intraepithelial production of basement membrane material and collagen (due to poor epithelial adhesion to basement membrane) (Figure 7-11)
Stromal
Macular (AR)
Mapped to chromosome 16q22; error in synthesis of keratan sulfate
Most severe but least common of the 3 classic stromal dystrophies
Granular (AD)
Mapped to chromosome 5q31 (BIGH3)
Deposits present in 1st decade of life, can remain asymptomatic for decades
Lattice
Mapped to chromosome 5q31 (BIGH3)
Deposits present in 1st decade of life
Types
Avellino’s
Mapped to chromosome 5q31 (BIGH3)
Central Crystalline (Schnyder’s) (AD)
Slowly progressive, rarely reduces vision enough to require corneal transplantation
Fleck (Francois-Neetans’) (AD)
Congenital, nonprogressive, asymmetric or unilateral
Endothelial
Fuchs’ (AD)
Early onset (mapped to chromosome 1p32-34) or late onset (mapped to chromosomes 13 and 18 (TCF4)
Variable penetrance, may be sporadic
Most common in postmenopausal women
Symptoms
blurred vision (initially, only in morning; later, all day); may have pain (ruptured bullae)
Miscellaneous
Descemetocele
Extreme focal thinning of cornea in which only Descemet’s membrane remains
Bullous Keratopathy
Corneal edema with epithelial bullae, thickened stroma, but no guttata
Due to loss or dysfunction of endothelial cells
Exposure Keratopathy
Desiccation of corneal epithelium due to CN 7 lesion (failure to close eyelids)
Contact Lens-related Problems
Giant papillary conjunctivitis (GPC)
sensitivity to CL material, deposits on CL, or mechanical irritation
Superior limbic keratoconjunctivitis (SLK)
may be due to hypersensitivity or toxic reaction to thimerosal
Corneal Transplant Failure
Findings
Epithelial Downgrowth
Surface epithelium grows through wound into eye, covering anterior segment structures
Appears as advancing line on corneal endothelium
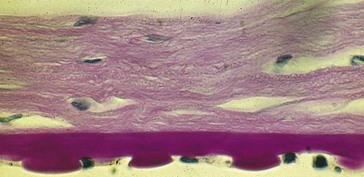
Pathology
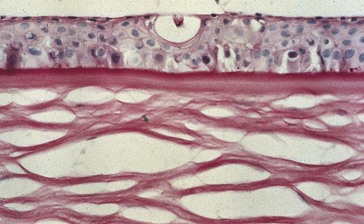
multilayered nonkeratinized squamous epithelium; PAS stains conjunctival goblet cells (differentiates between corneal and conjunctival epithelium) (Figure 7-16)
Fibrous Ingrowth
Fibrous proliferation through wound into AC
Limbal Stem Cell Deficiency
Graft-Versus-Host Disease (GVHD)
Ominous complication of bone marrow transplant (BMT)
Occurs primarily in allogeneic grafts
50% develop acute GVHD (50% mortality); 20–40% develop chronic GVHD
Multiple Endocrine Neoplasia (MEN)
MEN 2a (Sipple’s syndrome) (AD)
Scleral Disorders
Scleritis
More common in females; onset age 30–60 years
Etiology
50% associated with systemic disease
Classification
Diagnosis
Takayasu’s Disease
Narrowing of large branches of aorta
Diminished pulsations in upper extremities
Decreased blood pressure in upper extremities, increased BP in lower extremities
Relapsing Polychondritis
Discoloration
Surgery
Penetrating Keratoplasty (PK; PKP)
Full-thickness corneal graft / transplant
Donor screening
Tissue preservation
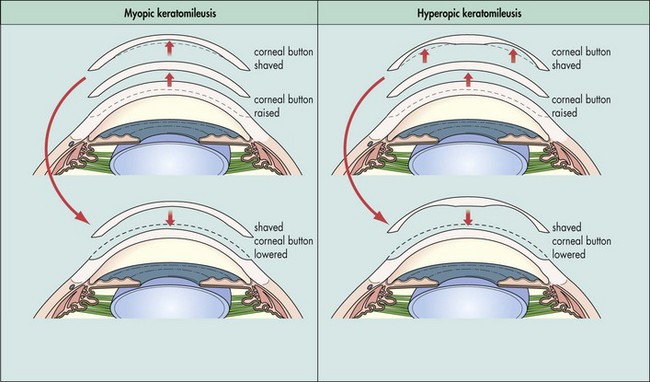
Keratomileusis
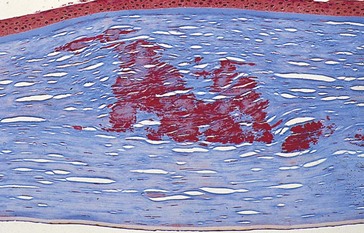
Lamellar section is removed, frozen, shaped on a cryolathe, then replaced in stromal bed to correct myopia or hyperopia. Donor lenticule can be used instead (Figure 7-17)
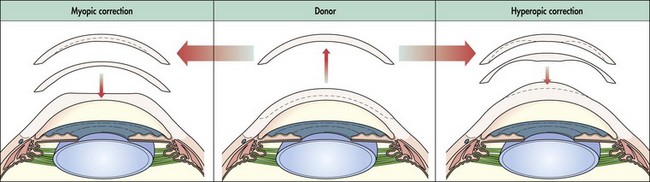
Epikeratophakia (Epikeratoplasty)
Epithelium is removed and a lathed donor lenticule is placed to correct myopia or hyperopia (Figure 7-18)
Astigmatic Keratotomy (AK)
Various nomograms exist (i.e. Lindstrom ARC-T)
Do not make arcuate incisions >90° (decreased efficacy, increased instability)
When combined with RK, do not cross incisions (creates wound gape and instability)
Radial Keratotomy (RK)
Deep radial corneal incisions to correct low to moderate myopia
Effect dependent on number of incisions, depth of incisions, size of optical zone, patient age
Photorefractive Keratectomy (PRK)
Laser ablation of corneal surface to correct myopia, hyperopia, and astigmatism
Excimer (excited dimer) laser
argon-fluoride (wavelength = 193 nm; far ultraviolet), energy = 64 eV
Functions as a ‘cold’ laser (breaks molecular bonds to ablate tissue; no thermal damage)
Each pulse removes approximately 0.25 µm of corneal tissue
Depth of ablation is related to diameter of optical zone and amount of intended correction
Disadvantages of PRK
involves visual axis, risk of haze / scarring, regression, requires removal of epithelium
Complications
Treatment of complications
Laser in Situ Keratomileusis (LASIK)
Advantages of LASIK
more rapid healing, less discomfort, less risk of haze, less postoperative medications
Complications
Treatment of complications
Laser-Assisted Epithelial Keratomileusis (LASEK)
Phototherapeutic Keratectomy (PTK)
Use of excimer laser to ablate corneal pathology limited to anterior  of cornea
of cornea
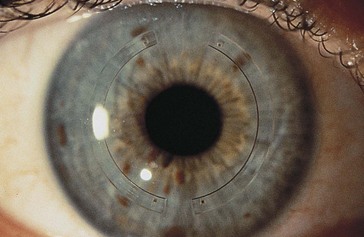
Intrastromal Corneal Ring Segments (Intacs)
Ring segment implants placed into peripheral corneal channels outside the visual axis to correct low to moderate myopia. Implants flatten the cornea without cutting or removing tissue from the central optical zone. Also used to reshape corneas with keratoconus or post-LASIK ectasia (Figure 7-19)
Review questions (Answers start on page 365)
American Academy of Ophthalmology. External Disease and Cornea, vol 8. San Francisco: AAO; 2012.
Arffa RC. Grayson’s Diseases of the Cornea, 4th edn. St Louis: Mosby; 1998.
Brightbill FS, McDonnell PJ, McGhee CNJ. Corneal Surgery Theory, Technique and Tissue, 4th edn. St Louis: Mosby; 2008.
Kaufman HE, Barron BA, McDonald MB. The Cornea, 2nd edn. Philadelphia: Butterworth-Heinemann; 1997.
Krachmer JH, Mannis MJ, Holland EJ. Cornea, 3rd edn. St Louis: Mosby; 2011.
Krachmer JH, Palay DA. Cornea Color Atlas, 2nd edn. St Louis: Mosby; 2006.
Leibowitz HM, Waring GO. Corneal Disorders: Clinical Diagnosis and Management, 2nd edn. Philadelphia: Saunders WB; 1998.
Foster CS, Azar DT, Dohlman CH. 4th edn. 2005. Lippincott Williams & Wilkins.



 OF CORNEA: lagophthalmos / exposure
OF CORNEA: lagophthalmos / exposure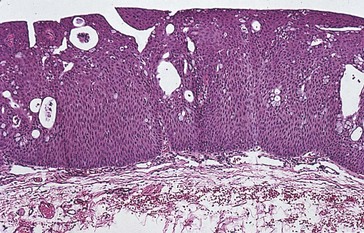

 of limbus; good prognosis, some scarring
of limbus; good prognosis, some scarring to
to  of limbus; guarded prognosis
of limbus; guarded prognosis of limbus; poor prognosis, risk of perforation
of limbus; poor prognosis, risk of perforation of cornea; normal aging, nocturnal exposure
of cornea; normal aging, nocturnal exposure