Chapter 23 Cor Pulmonale
2 What are the subtypes of cor pulmonale?
Cor pulmonale can be acute or chronic.
 In acute cor pulmonale the afterload to the right ventricle can rise in a matter of minutes (e.g., massive pulmonary embolism) giving very little room for compensation. The result will be acute right ventricular dilatation and failure, its severity depending primarily on the degree of acute PA hypertension.
In acute cor pulmonale the afterload to the right ventricle can rise in a matter of minutes (e.g., massive pulmonary embolism) giving very little room for compensation. The result will be acute right ventricular dilatation and failure, its severity depending primarily on the degree of acute PA hypertension.
 In chronic cor pulmonale, an increase of right ventricular afterload in the face of slowly developing PA hypertension (e.g., hypoxemia in chronic obstructive pulmonary disease [COPD]) generates a compensatory response of the right ventricle (see later) that will preserve the stroke volume until either the afterload increases excessively or the myocardium fails because of ischemia or other pathologic condition.
In chronic cor pulmonale, an increase of right ventricular afterload in the face of slowly developing PA hypertension (e.g., hypoxemia in chronic obstructive pulmonary disease [COPD]) generates a compensatory response of the right ventricle (see later) that will preserve the stroke volume until either the afterload increases excessively or the myocardium fails because of ischemia or other pathologic condition.
3 What is the pathophysiology of right ventricular failure?
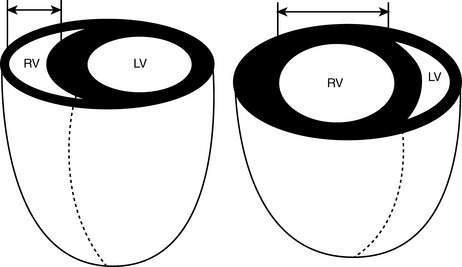
Under normal conditions, the pulmonary circulation is a low-resistance circuit, and the right ventricle generates the same stroke volume as the left ventricle with end-systolic pressures that are just 20% to 25% of those in the left ventricle. The low pressure within the thin free wall of the right ventricle also allows myocardial perfusion to occur both in systole and in diastole. Because of its structure, similar to that of veins rather than arteries, the right ventricle accommodates well additional volume but not higher pressure. When pressure overload occurs acutely, the right ventricle can only dilate and, if the pressure is sufficiently elevated, fail. Chronically, in response to increased systolic workload the free wall of the right ventricle hypertrophies and becomes similar to the left ventricle. Laplace’s law helps explaining the evolution from hypertrophy to dilatation and failure (Fig. 23-1): In a thin-wall chamber, an increase in intraluminal pressure increases wall stress unless thickness increases or the internal radius decreases. As the right ventricle hypertrophies, myocardial perfusion becomes limited to diastole, making its myocardium more susceptible to ischemia, and thus leading to dilatation and failure.
4 What are the causes of cor pulmonale?
Any process that results in pulmonary hypertension can cause cor pulmonale. Pulmonary hypertension is defined as mean PA pressures > 20 mm Hg at rest or > 30 mm Hg with exercise. The most frequent cause of pulmonary hypertension and cor pulmonale is COPD, due to chronic hypoxemia. In COPD the degree of hypertension is generally moderate, and oxygen supplementation may be effective in relieving some of the pressure load to the right ventricle and delaying failure. Additional causes of cor pulmonale include chronic pulmonary thromboembolic disease, left-sided cardiac abnormalities, untreated obstructive sleep apnea (OSA), interstitial lung diseases, and primary pulmonary hypertension. A comprehensive classification of the diseases of the lung associated with PA hypertension and cor pulmonale is shown in Table 23-1.
Table 23-1 Classification of cor pulmonale according to causative factor
| Category | Example |
|---|---|
| Diseases affecting the air passages of the lung and alveoli | COPD Cystic fibrosis Infiltrative or granulomatous defects Idiopathic pulmonary fibrosis Sarcoidosis Pneumoconiosis Scleroderma Mixed connective tissue disease Systemic lupus erythematosus Rheumatoid arthritis Polymyositis Eosinophilic granulomatosis Radiation Malignant infiltration |
| Diseases affecting thoracic cage movement | Kyphoscoliosis Thoracoplasty Neuromuscular weakness Sleep apnea syndrome Idiopathic hypoventilation |
| Diseases affecting the pulmonary vasculature | Primary disease of the arterial wall Primary pulmonary hypertension Pulmonary arteritis Toxin-induced pulmonary hypertension Chronic liver disease Peripheral pulmonary stenosis |
| Thrombotic disorders | Sickle cell diseases Pulmonary microthrombi |
| Embolic disorders | Thromboembolism Tumor embolism Other embolic processes (amniotic fluid, air, fat) Schistosomiasis and other parasitic infections |
| Pressure on PAs | Mediastinal tumors Aneurysms Granulomata Fibrosis |
Modified from Rubin LJ, ed: Pulmonary Heart Disease. Boston, 1984, Martinus Nijhoff, p 4.
7 What are the signs and symptoms of cor pulmonale?
Symptoms of cor pulmonale include the following:
9 What are the electrocardiographic (ECG) findings associated with right ventricular hypertrophy?
 Right axis deviation: QRS negative in lead I, positive in aVR
Right axis deviation: QRS negative in lead I, positive in aVR
 Tall R waves in the right precordial leads, deep S waves in the left precordial leads
Tall R waves in the right precordial leads, deep S waves in the left precordial leads
 Right atrial enlargement: P pulmonale, large P wave, in II and V1
Right atrial enlargement: P pulmonale, large P wave, in II and V1
 ST-segment changes in the opposite direction of the QRS (i.e., wide QRS-ST angle)
ST-segment changes in the opposite direction of the QRS (i.e., wide QRS-ST angle)
 Right bundle branch block: wide QRS (> 1.12 seconds); RSR′ in V1 and V2
Right bundle branch block: wide QRS (> 1.12 seconds); RSR′ in V1 and V2
11 What tests can help determine the diagnosis of cor pulmonale?
Laboratory investigations to detect the underlying cause of cor pulmonale may include the following:
 Arterial blood gas analysis with acid-base status.
Arterial blood gas analysis with acid-base status.
 Hematocrit to detect polycythemia.
Hematocrit to detect polycythemia.
 Coagulation studies to diagnose hypercoagulability, including serum levels of proteins S and C, antithrombin III, factor V Leyden, homocysteine, anticardiolipin antibodies.
Coagulation studies to diagnose hypercoagulability, including serum levels of proteins S and C, antithrombin III, factor V Leyden, homocysteine, anticardiolipin antibodies.
 Antinuclear antibody level for connective tissue diseases, such as scleroderma.
Antinuclear antibody level for connective tissue diseases, such as scleroderma.
 Brain natriuretic peptide may be elevated to compensate right-sided heart failure by diuresis, natriuresis, and vasodilation.
Brain natriuretic peptide may be elevated to compensate right-sided heart failure by diuresis, natriuresis, and vasodilation.
Radiographic findings include the following:
 Enlargement of the central PAs (right PA > 16 mm, left PA > 18 mm) with oligemic peripheral lung fields (Westermark sign)
Enlargement of the central PAs (right PA > 16 mm, left PA > 18 mm) with oligemic peripheral lung fields (Westermark sign) Enlargement of the right ventricle, presenting as an increased width of the cardiac silhouette in the posteroanterior view and increased retrosternal space in the lateral view
Enlargement of the right ventricle, presenting as an increased width of the cardiac silhouette in the posteroanterior view and increased retrosternal space in the lateral view Computed tomography and computed tomographic angiography
Computed tomography and computed tomographic angiography
 Dilation of the main PA diameter (≥ 29 mm has a reported sensitivity of 84% and a specificity of 75% for diagnosing pulmonary hypertension).
Dilation of the main PA diameter (≥ 29 mm has a reported sensitivity of 84% and a specificity of 75% for diagnosing pulmonary hypertension). Ultrafast, ECG-gated computed tomography (CT)
Ultrafast, ECG-gated computed tomography (CT)
 Ultrafast, ECG-gated CT has been evaluated to study right ventricular function: it may estimate ejection fraction and wall mass with high accuracy.
Ultrafast, ECG-gated CT has been evaluated to study right ventricular function: it may estimate ejection fraction and wall mass with high accuracy. Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA)
Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA)
Echocardiographic findings include the following:
 Transthoracic and transesophageal two-dimensional echocardiography (TTE and TEE, respectively) can be used to evaluate ventricular size and function, valvular dysfunction, and pulmonary hypertension.
Transthoracic and transesophageal two-dimensional echocardiography (TTE and TEE, respectively) can be used to evaluate ventricular size and function, valvular dysfunction, and pulmonary hypertension.
 Paradoxical leftward motion and flattening of the interventricular septum during both systole and diastole.
Paradoxical leftward motion and flattening of the interventricular septum during both systole and diastole. In severe cases, the interventricular septum may bulge into the left ventricle during the entire cardiac cycle, resulting in reduced left ventricular filling and output.
In severe cases, the interventricular septum may bulge into the left ventricle during the entire cardiac cycle, resulting in reduced left ventricular filling and output. Doppler echocardiography is used to estimate PA pressure noninvasively.
Doppler echocardiography is used to estimate PA pressure noninvasively.
 The pressure difference between the right ventricle and right atrium can be calculated from the tricuspid valve regurgitant jet usually present in pulmonary hypertension.
The pressure difference between the right ventricle and right atrium can be calculated from the tricuspid valve regurgitant jet usually present in pulmonary hypertension.12 What are the indications for use of echocardiography in the evaluation of cor pulmonale?
Indications for TEE and diagnosis of pulmonary hypertension include the following:
Class I: Conditions for which evidence and/or general agreement of an effective treatment exist
Class II: Conditions for which conflicting evidence and/or a divergence of opinion exist about the usefulness or efficacy of a procedure or treatment
Class III: Conditions for which evidence and/or general agreement exist that the treatment is not effective and in some cases may be harmful
13 Discuss nonpharmacologic treatment options for patients with cor pulmonale
 Lifestyle modifications. Although data are not available, it seems sensible that promoting a healthy lifestyle that includes moderate aerobic exercise and weight reduction should be beneficial. Strenuous activity should be avoided, and supplemental oxygen may be beneficial during even graded exercise, such as walking.
Lifestyle modifications. Although data are not available, it seems sensible that promoting a healthy lifestyle that includes moderate aerobic exercise and weight reduction should be beneficial. Strenuous activity should be avoided, and supplemental oxygen may be beneficial during even graded exercise, such as walking.
 Oxygen therapy is considered a mainstay of treatment for patients with COPD. Large controlled trials demonstrate that long-term administration of oxygen improves survival in patients with hypoxemia and COPD. Oxygen therapy decreases pulmonary vascular resistance by diminishing pulmonary vasoconstriction and improves right ventricular stroke volume and cardiac output.
Oxygen therapy is considered a mainstay of treatment for patients with COPD. Large controlled trials demonstrate that long-term administration of oxygen improves survival in patients with hypoxemia and COPD. Oxygen therapy decreases pulmonary vascular resistance by diminishing pulmonary vasoconstriction and improves right ventricular stroke volume and cardiac output.
 Phlebotomy may provide symptomatic relief of dyspnea to patients with pronounced polycythemia (hematocrit > 60%). Although less frequently used than in the past, phlebotomy can be considered in patients with polycythemia with acute decompensation.
Phlebotomy may provide symptomatic relief of dyspnea to patients with pronounced polycythemia (hematocrit > 60%). Although less frequently used than in the past, phlebotomy can be considered in patients with polycythemia with acute decompensation.
 Noninvasive ventilation (NIV) is the first line of ventilatory support during exacerbation of COPD, and it is standard therapy for advanced OSA. It is reasonable to infer that by correcting hypoxemia and acidosis, NIV will also decrease PA pressure, ease the forward flow of the right ventricle, and improve stroke volume and cardiac output when right ventricle failure is present. However, no data exist on the outcome benefit of NIV in acute cor pulmonale.
Noninvasive ventilation (NIV) is the first line of ventilatory support during exacerbation of COPD, and it is standard therapy for advanced OSA. It is reasonable to infer that by correcting hypoxemia and acidosis, NIV will also decrease PA pressure, ease the forward flow of the right ventricle, and improve stroke volume and cardiac output when right ventricle failure is present. However, no data exist on the outcome benefit of NIV in acute cor pulmonale.
14 What are the pharmacologic therapies for patients with cor pulmonale?
 Diuretics are indicated to manage right ventricle failure and volume overload. No evidence exists of benefit of long-term diuretic therapy in compensated cor pulmonale.
Diuretics are indicated to manage right ventricle failure and volume overload. No evidence exists of benefit of long-term diuretic therapy in compensated cor pulmonale.
 Vasodilators are a mainstay of pharmacologic therapy of pulmonary hypertension. Vasodilators improve cardiac output by decreasing the afterload to the right ventricle, and their efficacy in cor pulmonale depends on their relative selectivity for the pulmonary circulation. Systemic hypotension, syncope, and myocardial infarction are all possible complications of vasodilator therapy. They are discussed in detail later.
Vasodilators are a mainstay of pharmacologic therapy of pulmonary hypertension. Vasodilators improve cardiac output by decreasing the afterload to the right ventricle, and their efficacy in cor pulmonale depends on their relative selectivity for the pulmonary circulation. Systemic hypotension, syncope, and myocardial infarction are all possible complications of vasodilator therapy. They are discussed in detail later.
 Anticoagulation with warfarin (Coumadin) is indicated for those patients with cor pulmonale resulting from thromboocclusive pulmonary disease. In addition, and in the absence of the customary contraindications, it has been recommended for pulmonary hypertension associated with a variety of other diseases, such as collagen diseases, human immunodeficiency virus, and congenital left-to-right shunts.
Anticoagulation with warfarin (Coumadin) is indicated for those patients with cor pulmonale resulting from thromboocclusive pulmonary disease. In addition, and in the absence of the customary contraindications, it has been recommended for pulmonary hypertension associated with a variety of other diseases, such as collagen diseases, human immunodeficiency virus, and congenital left-to-right shunts.
15 Discuss the different classes of vasodilators used in the treatment of cor pulmonale
Long-term treatment of cor pulmonale includes the following:
 Calcium channel blockers (nifedipine, diltiazem, amlodipine) have been used both in the short term as a test of pulmonary vascular responsiveness and in the long term as therapy.
Calcium channel blockers (nifedipine, diltiazem, amlodipine) have been used both in the short term as a test of pulmonary vascular responsiveness and in the long term as therapy.
 Prostacyclins improve hemodynamics, symptoms, and outcome of patients with pulmonary hypertension of diverse etiology. Epoprostenol is administered as a continuous intravenous infusion through indwelling central venous access, and its use is limited to centers with the experience and structure to safely provide this treatment. Iloprost is a prostacyclin analogue that can be administered by inhalation. However, it requires a special nebulizer and six to nine administrations per day. Data on the long-term effect of iloprost therapy are still scarce.
Prostacyclins improve hemodynamics, symptoms, and outcome of patients with pulmonary hypertension of diverse etiology. Epoprostenol is administered as a continuous intravenous infusion through indwelling central venous access, and its use is limited to centers with the experience and structure to safely provide this treatment. Iloprost is a prostacyclin analogue that can be administered by inhalation. However, it requires a special nebulizer and six to nine administrations per day. Data on the long-term effect of iloprost therapy are still scarce.
 Endothelin-receptor antagonists such as bosentan have shown significant improvements in symptoms and short-term composite outcomes. One advantage of bosentan is its oral administration. Disadvantages come from its common side effects, including headache, flushing, elevation of liver enzyme levels, dependent edema, and anemia, which may lead to discontinuation of treatment.
Endothelin-receptor antagonists such as bosentan have shown significant improvements in symptoms and short-term composite outcomes. One advantage of bosentan is its oral administration. Disadvantages come from its common side effects, including headache, flushing, elevation of liver enzyme levels, dependent edema, and anemia, which may lead to discontinuation of treatment.
 Phosphodiesterase inhibitors such as sildenafil improve exercise capacity but do not prevent clinical worsening over time. In many cases, the starting dose of sildenafil is 20 mg 3 times a day, but in many cases, a dose of 80 mg 3 times a day is needed, with significant systemic side effects.
Phosphodiesterase inhibitors such as sildenafil improve exercise capacity but do not prevent clinical worsening over time. In many cases, the starting dose of sildenafil is 20 mg 3 times a day, but in many cases, a dose of 80 mg 3 times a day is needed, with significant systemic side effects.
Vasodilators for acute cor pulmonale include the following:
 Bridge treatment while other options are worked out and
Bridge treatment while other options are worked out and
 Test of reactivity of the pulmonary circulation for chronic vasodilator therapy with other drugs.
Test of reactivity of the pulmonary circulation for chronic vasodilator therapy with other drugs.
Inotropes with vasodilatory properties include the following:
 Dobutamine is the prototype of these agents. Dobutamine is a catecholamine with β1 and β2 adrenergic vascular effects. Dobutamine enhances myocardial contractility and decreases vascular resistance, thus increasing stroke volume and decreasing pulmonary and systemic pressure. The balance of these actions determines the effectiveness of the drug in each individual patient. Ideally, it will decrease PA pressure and increase cardiac output enough to maintain an adequate systemic blood pressure. Its effect is limited by systemic hypotension and tachycardia. An advantage of this drug is that, like all catecholamines, it has a short half-life, and its effect regresses rapidly on discontinuation.
Dobutamine is the prototype of these agents. Dobutamine is a catecholamine with β1 and β2 adrenergic vascular effects. Dobutamine enhances myocardial contractility and decreases vascular resistance, thus increasing stroke volume and decreasing pulmonary and systemic pressure. The balance of these actions determines the effectiveness of the drug in each individual patient. Ideally, it will decrease PA pressure and increase cardiac output enough to maintain an adequate systemic blood pressure. Its effect is limited by systemic hypotension and tachycardia. An advantage of this drug is that, like all catecholamines, it has a short half-life, and its effect regresses rapidly on discontinuation.
 Milrinone is a phosphodiesterase inhibitor (different class from sildenafil) with hemodynamic actions similar to dobutamine, but longer-lived and possibly more effective (i.e., more inotropy and less arrhythmia). Given its different mechanism of action, milrinone can be added in the short term to catecholamines, such as dobutamine or norepinephrine, and further potentiate their inotropic effect.
Milrinone is a phosphodiesterase inhibitor (different class from sildenafil) with hemodynamic actions similar to dobutamine, but longer-lived and possibly more effective (i.e., more inotropy and less arrhythmia). Given its different mechanism of action, milrinone can be added in the short term to catecholamines, such as dobutamine or norepinephrine, and further potentiate their inotropic effect.
17 Discuss the considerations for ventilator management of patients with cor pulmonale
 Maintain adequate PaO2 and PaCO2 to optimize PA vasodilation.
Maintain adequate PaO2 and PaCO2 to optimize PA vasodilation.
 Avoid excessive intrathoracic pressures, which may decrease venous return and increase afterload to the right ventricle, and consequent decreased filling and output of the left ventricle.
Avoid excessive intrathoracic pressures, which may decrease venous return and increase afterload to the right ventricle, and consequent decreased filling and output of the left ventricle.
 Limit intrathoracic pressure by controlling the level of mean airway pressure, which can be increased by increasing end-inspiratory pressure, end-expiratory pressure (PEEP, auto-PEEP), and inspiratory time. Careful administration of PEEP in patients with acute respiratory failure may be beneficial when it results in alveolar recruitment and consequent relief of hypoxemia.
Limit intrathoracic pressure by controlling the level of mean airway pressure, which can be increased by increasing end-inspiratory pressure, end-expiratory pressure (PEEP, auto-PEEP), and inspiratory time. Careful administration of PEEP in patients with acute respiratory failure may be beneficial when it results in alveolar recruitment and consequent relief of hypoxemia.
1 American College of Cardiology Foundation: 2003 Guideline Update for the Clinical Application of Echocardiography: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Washington: DC; 2003.
2 Bogaart H.J., Abe K., Noordergraf A.V., et al. The right ventricle under pressure. Cellular and molecular mechanisms of right-heart failure in pulmonary hypertension. Chest. 2009;135:794–804.
3 Criner G.J. Effects of long-term oxygen therapy on mortality and morbidity. Respir Care. 2000;45:105–118.
4 Gordon C., Collard C.D., Pan W. Intraoperative management of pulmonary hypertension and associated right heart failure. Curr Opin Anaesthesiol. 2010;23:49–56.
5 Haddad F., Couture P., Tousignant C., et al. The right ventricle in cardiac surgery, a perioperative perspective: I. Anatomy, physiology, and assessment. Anesth Analg. 2009;108:407–421.
6 Han M.K., McLaughlin V.V., Criner G.J., et al. Pulmonary diseases and the heart. Circulation. 2007;916:2992–3005.
7 Inglessis I., Shin J.T., Lepore J.J., et al. Hemodynamic effects of inhaled nitric oxide in right ventricular myocardial infarction and septic shock. J Am Coll Cardiol. 2004;44:793–798.
8 McLaughlin V.V., McGoon M.D. Pulmonary arterial hypertension. Circulation. 2006;114:1417–1431.
9 Metha S., Hill N.S. Noninvasive ventilation. Am J Respir Crit Care Med. 2001;163:540–577.
10 Minai O.A., Chaouat A., Adnot S. Pulmonary hypertension in COPD: epidemiology, significance, and management: pulmonary vascular disease: the global perspective. Chest. 2010;137:39S–51S.
11 Oswald-Mammosser M., Weitzenblum E., Quoix E., et al. Prognostic factors in COPD patients receiving long-term oxygen therapy. Importance of pulmonary artery pressure. Chest. 1995;107:1193–1198.
12 Piazza G., Goldhaber S.Z. Chronic thromboembolic pulmonary hypertension. N Engl J Med. 2011;364:351–360.
13 Scharf S.M., Iqbal M., Keller C., et al. Hemodynamic characterization of patients with severe emphysema. Am J Respir Crit Care Med. 2002;166:314–322.
14 Simonneau G., Robbins I.M., Beghetti M., et al. Updated classification of pulmonary hypertension. J Am Coll Cardiol. 2009;54:S43–S54.
15 Stobierska-Dzierzek B., Awad H., Michler R.E. The evolving management of acute right-sided heart failure in cardiac transplant recipients. J Am Coll Cardiol. 2001;38:923–931.
16 Vizza C.D., Lynch J.P., Ochoa L.L., et al. Right and left ventricular dysfunction in patients with severe pulmonary disease. Chest. 1998;113:576–583.