Congenital Optic Nerve Head Abnormalities
Optic Disc Coloboma
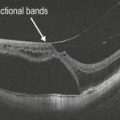
Optic disc colobomas are uncommon congenital defects that develop as a result of defective closure of the fetal fissure (Fig. 6.3.1). Colobomas can be associated with peripapillary retinal detachments or schisis. In posterior segment colobomas, histological and OCT studies show that a tissue called the intercalary membrane overlies the area affected by the defect. OCT allows a qualitative assessment of the vitreous in eyes with optic disc colobomas, documenting the degree of vitreous condensation and adhesion in the area of the optic disc, especially with the three-dimensional reconstruction. OCT can potentially reveal retinal breaks on the optic disc margin. Retinal detachments and schisis associated with the optic disc colobomas can also be visualized on OCT scanning.
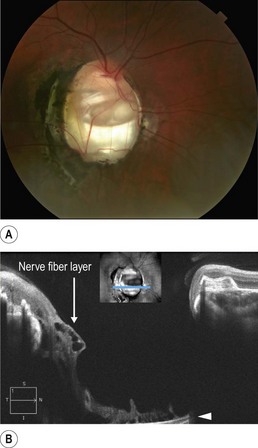
Figure 6.3.1 Color photograph of an optic disc coloboma of the right eye. There is minimal retinal involvement with pigmentation and scarring temporal to the disc. A line scan shows a deep cavitary depression within the optic nerve that is significantly more exaggerated than what is seen in normal optic nerve cupping. There are associated hyporeflective cystic changes within the nerve fiber layer (arrow). There is shadowing due to overhanging of the nasal optic nerve rim with loss of the underlying OCT signal (arrowhead). The blue line (inset) shows the position of the B-scan.
Optic Disc Pit
Optic disc pit is a rare congenital anomaly of the optic nerve head (Fig. 6.3.2). Associated maculopathy has been reported to eventually develop in over 90% of affected eyes. OCT line scans through the affected regions show both subretinal fluid and schisis of the outer retinal layers, extending from the temporal margin of the disc to the nasal aspect of the fovea, and overlying a central neurosensory retinal detachment. Lamellar macular holes or even full-thickness macular holes can develop.
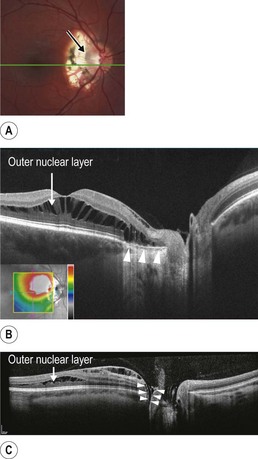
Figure 6.3.2 (A) Color photograph of an optic nerve pit (arrow) previously treated with focal laser photocoagulation temporal to the optic disc. (B) Line scan shows intraretinal schisis of the outer nuclear layer (arrow). Chorioretinal atrophy, as a result of the prior laser treatment, can be seen (arrowheads). This OCT scan does not go through the optic nerve pit. (C) Line scan through an optic disc pit showing intraretinal schisis of the outer nuclear layer (arrow). The optic nerve pit can be seen in cross section (arrowheads).
Optic Nerve Head Drusen
ONH drusen are not an unusual congenital and developmental abnormalities (Fig. 6.3.3). Drusen exhibit shadowing on the OCT B-scan. Optical coherence tomography is valuable in the diagnosis of ONH drusen, and in the differential diagnosis with ONH edema. The retinal nerve fiber layer (RNFL) thickness and the peripapillary total retinal thickness are significantly greater in eyes with ONH edema than in eyes with ONH drusen. A recent study suggests that EDI may be more efficient than regular OCT scanning in detecting ONH drusen.
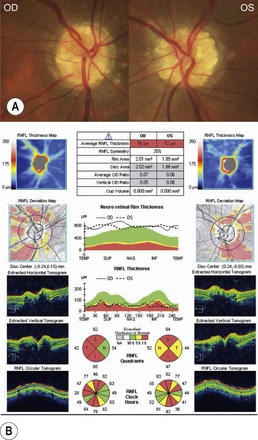
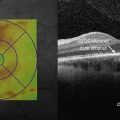
Figure 6.3.3 Color photograph of a patient with bilateral optic nerve head drusen. Note the elevated calcified deposits in the ONH of both right eye (RE) and left eye (LE). The retinal vessels that emerge from the ONH have normal appearance. ONH and RNFL analysis shows reduction in the average RNFL thickness in both eyes, and altered values of RNFL thickness measurement in fundus quadrants. The B-scan across the ONH reveals elevation and shadowing typical of ONH drusen.
Megalopapilla
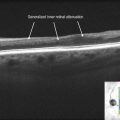
Megalopapilla is a congenital malformation characterized by an abnormally large optic disc, with no pathological significance (Fig. 6.3.4). The RNFL thickness is normal in megalopapilla, which is an essential feature in the differential diagnosis with glaucomatous optic neuropathy. Normative data from normal eyes indicate that the RNFL is thicker in superior and inferior fundus quadrants, while it is thinner in nasal and temporal quadrants. The same features are observed in eyes with megalopapilla.

Figure 6.3.4 Color photograph of a patient with bilateral megalopapilla shows enlarged optic disc area with increased cup-to-disc ratio. The cups are round and notching of the neuroretinal rim is not observed. SD-OCT shows increased optic disc area, 4.24 mm2 and 2.75 mm2 as measured by Heidelgerg Retina Tomograph (Heidelberg Engineering GmbH, Heidelberg, Germany). Despite the increased cup-to-disc ratio and clinical diffuse absence of neuroretinal rim tissue in both eyes, the OCT showed normal RNFL thickness in the left eye (LE) and sectorial RNFL thinning only in the inferior sector in the right eye (RE). Of note, the normative data in the OCT software is valid for disc areas between 1.2 mm2 and 2.8 mm2, which might be related to the warning message in the right eye. (Image courtesy of Dr Patricia Cerqueira, Sao Paulo University.)