Chapter 23 Congenital Aneurysms of the Sinuses of Valsalva
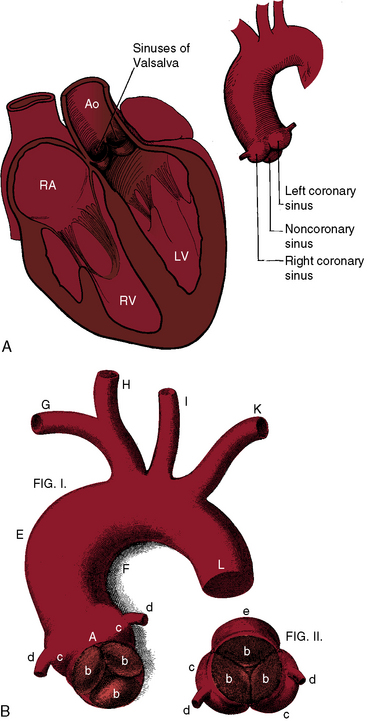
Antonio Maria Valsalva, anatomist and pathologist, was born in 1666 in the historic Emilia-Romagna region of northern Italy. The sinuses that bear Valsalva’s name consist of three small outpouchings in the wall of the aorta immediately above the attachments of each aortic cusp (Figure 23-1). In 1839, James Hope1 published an account of a ruptured congenital aneurysm of a sinus of Valsalva, “a case of aneurysmal pouch of the aorta bursting into the right ventricle.” A year later, John Thurnam2 expanded Hope’s report by adding examples of unruptured aortic sinus aneurysms and by naming the sinuses according to their relationship to the coronary arteries as the right coronary sinus, the left coronary sinus, and the noncoronary sinus (see Figure 23-1). These designations appeared in Quain’s Elements of Anatomy3 and remain in use today.4
Aneurysms of the sinuses of Valsalva account for 1% of congenital anomalies of the heart and circulation.5 The aneurysms tend to be single, although exceptionally, more than one sinus is involved.6,7 An aneurysm may arise from each sinus of a bicuspid aortic valve,6,8 from each sinus of a trileaflet aortic valve,7 and rarely, from a quadricuspid aortic valve.9
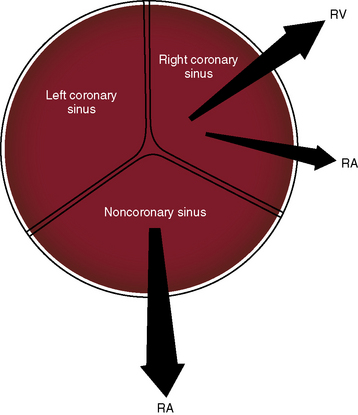
The anatomic relationship of the sinuses of Valsalva to adjacent structures determines the site into which a given congenital aneurysm ruptures.4 Ninety percent to 95% originate in the right or noncoronary sinus and project into the right ventricle or right atrium, and less than 5% originate in the left coronary sinus (Figure 23-2).4,10,11 Those that arise in the noncoronary sinus almost always rupture into the right atrium (see Figure 23-2), and those that arise in the right coronary sinus rupture into the right ventricle or occasionally into the right atrium (see Figure 23-2).4 Rarely, rupture is into the pulmonary artery,10,12 left ventricle,4 left atrium,4 or pericardial space.4,13 Also rarely, a sinus aneurysm dissects into the interventricular septum, where it remains unruptured or perforates and ruptures into the left or right ventricle.5,14–16 A congenital etiology is questionable when an aneurysm originates in the left coronary sinus and ruptures into the left side of heart.4
A sinus of Valsalva aneurysm can cause aortic regurgitation by interfering with aortic leaflet coaptation, can enter the right atrium and cause tricuspid regurgitation,17 or can enter the right ventricular outflow tract and cause subpulmonary obstruction. A congenital aortic sinus aneurysm that is the site of infective endocarditis can be difficult to distinguish from aortic valve infective endocarditis that caused the aortic sinus to perforate.4,18–20 A large unruptured aneurysm can compress the superior vena cava, the right atrium, the right ventricle,21 or a coronary artery.
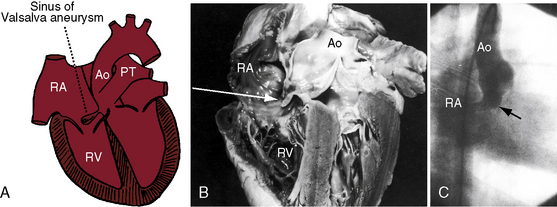
A congenital sinus of Valsalva aneurysm begins as a blind pouch or diverticulum at a localized site in an aortic sinus and then protrudes as a finger-like or nipple-like projection that ruptures at its tip (Figure 23-3).4,22,23 The fundamental histologic fault responsible for a coronary sinus aneurysm is discontinuity of the elastic layer in the aortic media at the juncture between the ascending aorta and aortic valve annulus, which sets the stage for avulsion and aneurysm formation.23,24 The histologic fault is present at birth, but with rare exception, the aneurysm is not.18,25,26 Marfan syndrome is associated with dilation of the ascending aorta and the sinuses of Valsalva, but dissection or rupture is in the ascending aorta, not in the sinuses.27 An aorticocameral communication is a tortuous channel that originates the ascending aorta above the left sinus of Valsalva and terminates in the right atrium without involving the aortic sinuses.28
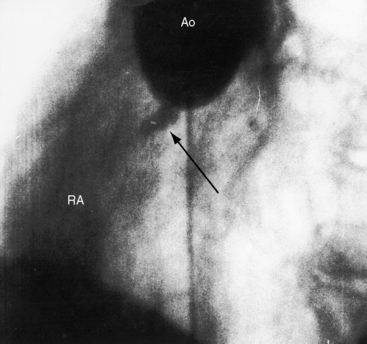
The physiologic consequences of rupture depend on three factors: 1, the amount of blood flowing through the rupture; 2, the rapidity with which the rupture develops; and 3, the chamber that receives the rupture. Irrespective of the right-sided receiving site, shunted blood must flow through the pulmonary circulation, the left atrium, and the left ventricle before returning to the aorta. When the right atrium receives the rupture, all four cardiac chambers are volume overloaded. A sudden large rupture provokes congestive failure because the heart cannot adapt rapidly to the acute hemodynamic burden. Conversely, small insidious perforations initially go unnoticed (Figure 23-4). Deformity of aortic cusps caused by a ruptured or unruptured aneurysm causes regurgitation through the valve (Figure 23-5), and rupture of a sinus aneurysm into the left ventricle causes regurgitation through the rupture.29 Aneurysms that originate in the right sinus of Valsalva are typically associated with a supracristal ventricular septal defect (see Figure 23-5).4,23,30–32
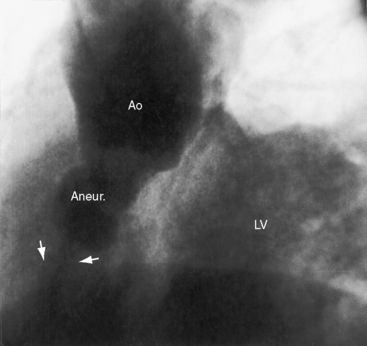
Figure 23-5 Aortogram from a 31-year-old woman with an asymptomatic restrictive ventricular septal defect and mild to moderate aortic regurgitation. Sudden dyspnea, orthopnea, and a coarse continuous murmur were caused by rupture of an aneurysm (Aneur., arrows) of the right sinus of Valsalva into the right ventricle. The left ventricle (LV) visualized because of aortic regurgitation. The echocardiogram is shown in Figure 23-14. (Ao = aorta.)
Unruptured congenital sinus of Valsalva aneurysms were recognized by Thurnam (see previous).2 Before the advent of echocardiography, approximately 20% of unruptured aneurysms were chance findings at necropsy or at cardiac surgery.33 However, occult unruptured congenital aortic sinus aneurysms are now readily imaged, even in older adults (see Figure 23-17).28,34 An unruptured aneurysm can compress a proximal coronary artery or can dissect into the ventricular septum and cause complete heart block.34 Protrusion of an aneurysm into the left ventricle is occasionally responsible for aortic regurgitation (see previous),29 less commonly for obstruction to left ventricular outflow.
History
Ruptured aortic sinus aneurysms typically announce themselves in young males after puberty but before age 30 years. The male:female ratio is as high as 4:1.22 Rupture rarely occurs in infancy or early childhood25,26,35 or as late as the seventh decade36,37 and rarely occurs during pregnancy.38 The average age of rupture was 34 years in one large series, with an age range of 11 years to 67 years.36 An unruptured congenital aneurysm of the right coronary sinus was an incidental necropsy finding in a 82-year-old man,33 and an 85-year-old man came to attention because an occult unruptured aortic sinus aneurysm in the right ventricular outflow tract caused a to-and-fro murmur (see Figure 23-17). Death from congestive heart failure typically occurs within a year after rupture.36 Sudden death follows perforation into the pericardium, and syncope and sudden death are occasional sequelae of complete heart block caused by a ruptured15 or unruptured34 aneurysm that dissects into the base of the ventricular septum.15,39 Conversely, long survival sometimes follows a small slowly progressive perforation (see Figure 23-4). One such individual lived for 30 years, and another lived for 17 years;40 a 65-year-old man died of gastric carcinoma 10 years after rupture,37 and rupture in infancy was followed by surgical repair 15 years later. Small perforations come to attention because of a continuous murmur (see Figure 23-4),41 because of a diastolic murmur caused by aortic regurgitation, because of infective endocarditis,4,19 or during a diagnostic study for ventricular septal defect.42 A large unruptured saccular aneurysm filled with laminated thrombus came to light because of a prominent paracardiac density on a routine chest x-ray, and another unruptured aneurysm announced itself with cerebral and retinal emboli.43 Compression of a coronary artery by an unruptured aneurysm is a rare cause of angina pectoris or myocardial infarction (see previous). In 1957, a 27-year-old soldier with a large acute rupture underwent the first successful surgical repair with a polyvinyl prosthesis shaped as a golf tee. Three decades later, the patient had dramatic reperforation (see second case history subsequent).44
Congenital sinus of Valsalva aneurysms come to attention because of the acute development of a large perforation, gradual progression of a small perforation, or an asymptomatic or symptomatic unruptured aneurysm. An large acute rupture is announced by the dramatic onset of severe retrosternal or upper abdominal pain and intractable dyspnea.31,36 The rupture often but not necessarily follows physical stress. The acute symptoms last for hours or days, sometimes subsiding gradually, leaving the patient’s condition temporarily improved, but congestive heart failure appears and progresses relentlessly. The following case histories are illustrative.
The first history describes a 45-year-old truck driver whose work included strenuous lifting of 50-lb to 100-lb sacks of plaster.31 He was in good health until 3 weeks before an alarming experience. While carrying a 100-lb sack, he suddenly became “out of breath” and fell to the floor. A raw sensation radiated from the epigastrium to the base of the neck. Despite severe weakness and shortness of breath, he carried 20 more sacks before consulting a doctor. When seen by the authors, he was relatively asymptomatic.
The initial pain is believed to be related to the rupture itself. Occasionally, the aneurysm compresses a coronary artery, so symptoms of myocardial ischemia or infarction coexist.45 Rupture may be announced by acute dyspnea rather than pain, or mild chest pain may occur for weeks before the onset of dyspnea and tightness in the upper abdomen. If a patient with a ventricular septal defect suddenly develops chest pain, dyspnea, and a continuous murmur, the reason is likely to be rupture of a coexisting aortic sinus aneurysm (see Figure 23-5; see previous).
Small insidious perforations that initially progress gradually go unnoticed (see Figures 23-4 and 23-16). Mild dyspnea without pain sometimes precedes congestive heart failure by months or years.17 Patients sometines present during a relatively asymptomatic interval with a continuous murmur mistaken for patent ductus arteriosus.
Congenital aortic sinus aneurysms usually go unrecognized until they rupture.33 However, unruptured aneurysms can manifest themselves with a to-and-fro murmur from flow in and out of the intact aneurysmal pouch (see Figure 23-17), with the murmur of tricuspid regurgitation, with a midsystolic murmur of right ventricular outflow obstruction, with the pain of myocardial ischemia from coronary artery compression, with aortic regurgitation–caused malapposition of aortic cusps,29 with superior vena caval obstruction,21 with a paracardiac mass in the chest x-ray, with systemic emboli,43 with complete heart block, with syncope, or with sudden death.15
Physical appearance
Because rupture rarely occurs before puberty (see previous), growth and development are seldom affected by the catabolic effects of congestive heart failure. Aneurysm of the noncoronary sinus of Valsalva has been reported with the Klippel-Feil syndrome, which is characterized by short neck, low posterior hairline, and restricted mobility of the upper spine caused by congenital fusion of any two cervical vertebrae.46 Giant aneurysms of the left and noncoronary sinuses have been reported with Noonan’s syndrome, characterized by hypertelorism, down-slanting eyes, webbed neck, short stature, and chest deformity.47
Arterial pulse
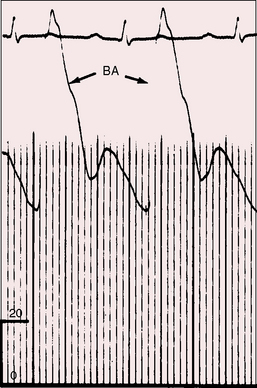
All gradations of an aortic runoff are reflected in the arterial pulse, irrespective of which chamber or side of the heart receives a ruptured sinus of Valsalva aneurysm (Figure 23-6). The pulse pressure may not be wide immediately after perforation because the left ventricle has not had time to adapt to the increase in volume and because left ventricular end diastolic pressure is elevated.48 If survival permits, the arterial pulse becomes bounding with a rapid rise, a rapid fall, a wide pulse pressure, and a bisferiens configuration. Carotid pulses are visible, Quincke pulses appear in the fingertips, and pistol shot sounds and Duroziez’s murmur are heard over the femoral arteries. When an aneurysm penetrates the base of the ventricular septum and causes complete heart block, the arterial pulse is slow.
Jugular venous pulse
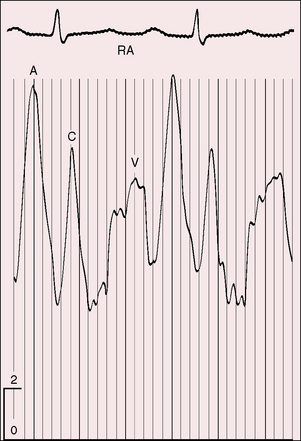
The height and waveform of the jugular venous pulse depend on the size and rapidity of the rupture and on the presence and degree of right ventricular failure. A small insidious rupture leaves the jugular venous pulse normal, irrespective of which chamber receives the rupture. A large sudden rupture into the right atrium or right ventricle is accompanied by congestive heart failure, an elevated mean jugular venous pressure, and tall A and V waves (Figure 23-7). When an aortic sinus aneurysm projects into the right atrium and causes tricuspid regurgitation (see previous), the V wave is selectively elevated. When an aneurysm causes obstruction of the superior vena cava, the mean jugular venous pressure is elevated, but the wave forms disappear. When an aneurysm results in obstruction to right ventricular outflow, the A wave selectively increases. Complete heart block is accompanied by the distinctive jugular pulse described in Chapter 4.
Auscultation
A hallmark of acute rupture of an aortic sinus aneurysm into the right side of the heart is the sudden appearance of a continuous murmur in a previously healthy individual, usually a young male.36 In a patient known to have a ventricular septal defect, the sudden appearance of a continuous murmur is a feature of rupture of a coexisting aortic sinus aneurysm (see Figure 23-5).30,36
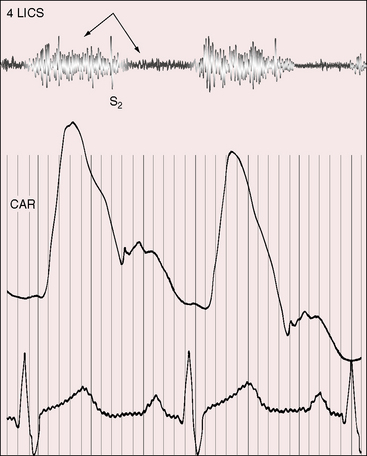
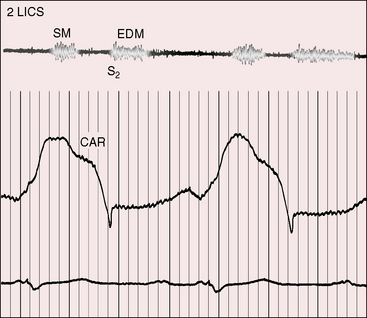
When the right atrium receives the rupture, the continuous murmur is maximal along the right or left sternal border, or over the lower sternum (Figure 23-8). When the rupture enters the body of the right ventricle, the continuous murmur is maximal at the mid to lower left sternal border (Figure 23-9), and rupture into the outflow tract of the right ventricle results in a continuous murmur at the upper left sternal edge. The systolic component of continuous murmurs tends to be louder at higher thoracic sites, and the diastolic component tends to be louder at lower thoracic sites.
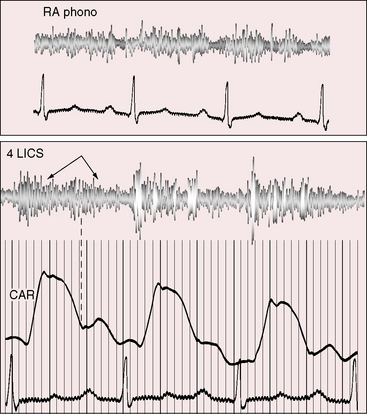
Figure 23-8 Right atrial intracardiac phonocardiogram (RA phono) with simultaneous thoracic wall phonocardiogram at the fourth left intercostal space (4 LICS) in the 17-year-old boy with rupture of an aneurysm of the noncoronary sinus of Valsalva into the right atrium (see Figures 23-6 and 23-7). The continuous murmur within the right atrium and on the thoracic wall (4LICS) exhibits systolic or diastolic accentuation from beat to beat but does not peak around the second heart sound. (CAR = carotid pulse).
The quality, loudness, and configuration of the continuous murmur accompanying a sudden large rupture were well stated in early reports. Hope described “a very loud, superficial sawing murmur prolonged continuously over the first and second heart sounds (probably weaker during the period of repose).”1 Thurnam called attention to “a superficial, harsh murmur and a peculiarly intense sawing or blowing sound accompanied by an equally marked or purring tremor heard over the varicose orifice and in the circulation beyond it; this sound is continuous but is loudest during systole, less loud during diastole.”2 These descriptions carry an important message: namely, that the continuous murmur of a ruptured aortic sinus aneurysm does not peak around the second heart sound, in contrast to the continuous murmur of patent ductus arteriosus (Figures 23-9 and 23-10). Either the systolic or the diastolic portion of the murmur tends to be louder. Intensity may diminish around the second heart sound only to increase in diastole, creating a to-and-fro cadence. From time to time, the continuous murmur exhibits either systolic or diastolic accentuation (see Figure 23-9). An aneurysm may be compressed by right ventricular contraction, by impeding systolic flow, and by accounting for diastolic accentuation of the continuous murmur. Rupture directly into the left ventricle results in an early diastolic murmur of aortic regurgitation and in a short midsystolic murmur from augmented flow into the aorta (see Figure 23-10). An unruptured aneurysm may cause an isolated diastolic murmur of aortic regurgitation by compromising aortic cusp coaptation (see previous).29
Variations in murmur patterns are better understood with examination of intracardiac phonocardiograms recorded at sites in and around the rupture (see Figure 23-8). Continuous murmurs are recovered from within the aneurysm itself. The systolic component might be more prominent in the proximal aortic portion of the aneurysm, and the diastolic component may be more prominent in the distal right atrial or right ventricular portion.
Tricuspid regurgitation,17 mitral regurgitation, and ventricular septal defect30 result in holosystolic murmurs. Short midsystolic murmurs are generated by rapid ejection across the aortic and pulmonary valves. An aneurysm may protrude into the right ventricular outflow tract and cause a longer midsystolic murmur or may compromise aortic cusp coaptation and cause the murmur of aortic regurgitation. However, these systolic and diastolic murmurs tend to be obscured by the louder continuous murmur through the rupture.
Unperforated aortic sinus aneurysms can be accompanied by prominent murmurs in both phases of the cardiac cycle as blood flows into and out of the unruptured aneurysmal pouch. These to-and-fro murmurs are auscultatory counterparts of the phasic expansion and relaxation of unruptured aneurysms imaged with two-dimensional echocardiography (see Figure 23-17) and with signals recorded with pulsed Doppler echocardiography.34 An unperforated aneurysm that obstructs the right ventricular outflow tract results in a midsystolic murmur across the obstruction, and an unperforated aneurysm that projects into the right atrium can result in the murmur of tricuspid regurgitation. An unruptured aneurysm that protrudes into the left ventricular outflow tract or into the base of the ventricular septum can cause murmurs of aortic regurgitation29 and aortic stenosis.14
Electrocardiogram
Small, slowly progressive aortic sinus ruptures are accompanied by normal electrocardiograms. The rhythm is normal sinus even when a large rupture is into the right atrium. The PR interval tends to be prolonged (Figure 23-11). The QRS axis is normal or rightward, and occasionally leftward. Atrioventricular conduction defects, including complete heart block,49 right or left bundle branch block, and bifascicular block, occur when a ruptured or unruptured aneurysm penetrates the base of the ventricular septum and injures the atrioventricular node or His bundle.49 A right atrial P wave abnormality is generated when the right atrium receives the rupture, or when an aortic sinus aneurysm causes tricuspid regurgitation. Increased flow through the left atrium accounts for a left atrial P wave abnormality.
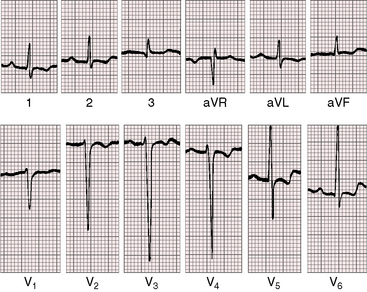
Figure 23-11 Electrocardiogram from the 17-year-old boy with an aneurysm of the noncoronary sinus of Valsalva that ruptured into the right atrium (see Figures 23-6, 23-7, and 23-8). The PR interval is prolonged. The QRS axis is normal. Left ventricular hypertrophy is characterized by deep S waves in leads V2-4 and prominent R waves and ST segment/T wave abnormalities in leads V5-6.
Rupture into the right atrium or right ventricle results in volume overload of both ventricles, but the electrocardiogram usually shows left ventricular hypertrophy by voltage criteria and ST segment/T wave abnormalities (see Figure 23-11).36 Right ventricular hypertrophy may coexist, but does not occur alone,36 except with aneurysms that cause right ventricular outflow obstruction. An aneurysm that compresses a proximal coronary artery results in electrocardiographic changes of myocardial ischemia or infarction.45
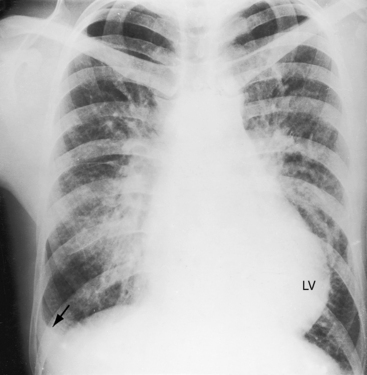
X-ray
Because most patients with ruptured congenital aortic sinus aneurysms are otherwise healthy, previous x-rays are often available for comparison. Small insidious perforations leave the x-ray unchanged. Large acute ruptures are followed by pulmonary venous congestion because of the steep rise in end diastolic pressure in an unprepared left ventricle (Figure 23-12). Increased pulmonary arterial blood flow results in enlargement of the pulmonary trunk (Figure 23-13).42,50 Moderate left atrial enlargement is seen in the lateral projection; and in the anteroposterior view, a right atrial convexity appears at the right lower cardiac border and a moderately dilated left ventricle occupies the apex (see Figure 23-13).42,50 When an aortic sinus aneurysm ruptures into the right side of the heart, volume overload of both ventricles and congestive heart failure account for the radiologic picture (see Figure 23-12).42 Rupture is into the left ventricle causes pulmonary venous congestion without increased pulmonary arterial blood flow, and with a selective increase in left ventricular size. Rarely, calcium is seen in the aneurysm. Also rarely, an aneurysm of the left aortic sinus presents as a localized convex radiologic prominence immediately below the pulmonary trunk, or a large saccular aneurysm of the right aortic sinus presents as a prominent right paracardiac density.
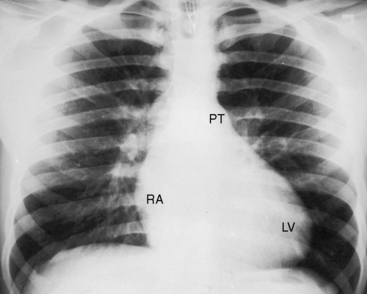
Figure 23-13 X-ray from the 17-year-old boy with a noncoronary sinus of Valsalva aneurysm that ruptured into the right atrium (see Figures 23-6, 23-7, and 23-8). Increased venous vascularity is evident in the inner third of the lung fields. The pulmonary trunk (PT) is moderately dilated. An enlarged right atrium (RA) occupies the right lower cardiac border, and a dilated left ventricle (LV) occupies the apex.
Echocardiogram
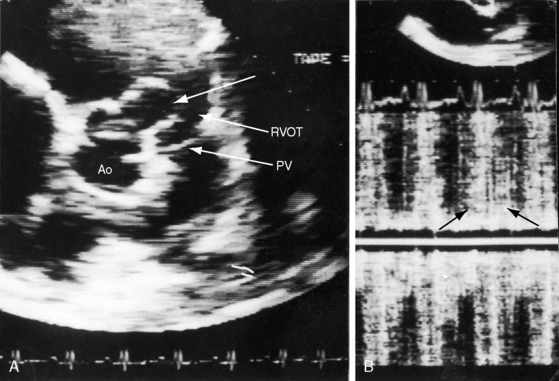
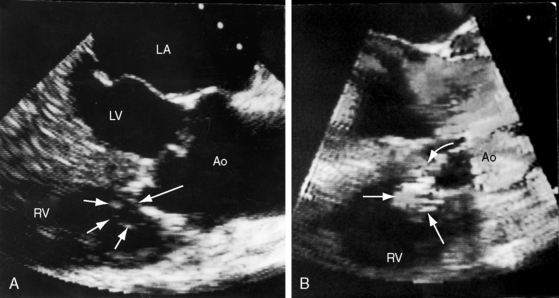
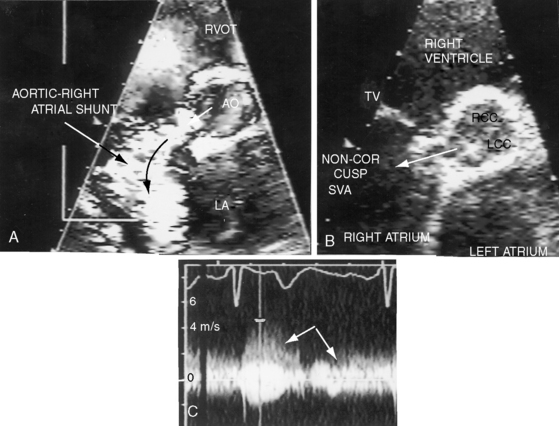
Echocardiography with color flow imaging and Doppler interrogation establish the diagnosis of a ruptured or unruptured sinus of Valsalva aneurysm (Figures 23-14 through 23-18) and establish the presence of associated abnormalities that are either intrinsic features of the aneurysm or that are in addition to the aneurysm.51,52 Echocardiography identifies insidious asymptomatic ruptures manifested only by a continuous murmur (see Figures 23-4 and 23-16). Two-dimensional imaging identifies the aneurysmal sac (see Figures 23-14, 23-15, and 23-18A, B), the aortic sinus of origin (see Figures 23-14, 23-15, and 23-18B), the two normal sinuses, and a normal aorta above the aneurysm. Color flow imaging identifies flow into the recipient chamber (see Figures 23-16B, and 23-18A). Pulsed Doppler (see Figure 23-15) and continuous wave Doppler (see Figure 32-18C) define the flow patterns in the ruptured aneurysm. A large unruptured aortic sinus aneurysm (see Figure 23-17) is characterized by phasic expansion and relaxation and by to-and-fro pulsed Doppler signals at the site of origin from the aorta but has no evidence of rupture.11 Doppler interrogation establishes the presence and degree of subpulmonary obstruction when an aneurysm protrudes into the right ventricular outflow tract (see Figure 23-16). The presence and degree of aortic regurgitation are established, a coexisting ventricular septal defect is identified and characterized, and the physiologic consequences of rupture into the right atrium, right ventricle, or left ventricle are determined. Real-time imaging identifies ischemic regional left ventricular wall motion abnormalities that result from compression of a coronary artery by an aortic sinus aneurysm.
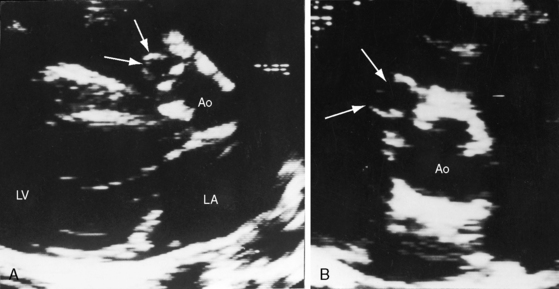
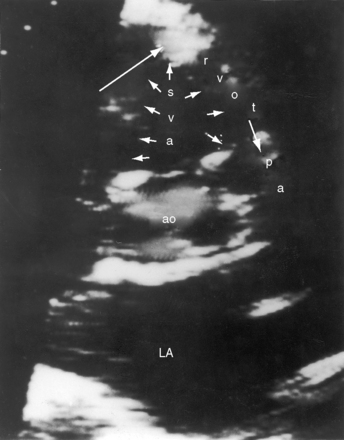
Figure 23-14 A, Parasternal long-axis and, B, short-axis echocardiograms from a 31-year-old woman with a restrictive perimembranous ventricular septal defect and mild aortic regurgitation. An aneurysm (paired arrows) of the right sinus of Valsalva ruptured into the right ventricle near the attachment of the septal tricuspid leaflet. The aortogram is shown in Figure 23-5. (Ao = aorta; LA = left atrium; LV = left ventricle.)
1 Hope J. A treatise on the diseases of the heart and great vessels: comprising a new view of the physiology of the heart’s action, according to which the physical signs are explained. London: J. Churchill & Sons; 1839.
2 Thurnam J. On aneurysms, and especially spontaneous varicose aneurysms of the ascending aorta. Trans R Med Chir Soc (Glasgow). 1840;23:323.
3 Walmsley T.. The heart. Quain’s elements of anatomy, Vol. 4. New York: Longmans, Green & Company. 1929. Part 3
4 Sakakibara S., Konno S. Congenital aneurysm of the sinus of Valsalva. Anatomy and classification. Am Heart J. 1962;63:405-424.
5 Wells T., Byrd B., Neirste D., Fleurelus C. Images in cardiovascular medicine. Sinus of valsalva aneurysm with rupture into the interventricular septum and left ventricular cavity. Circulation. 1999;100:1843-1844.
6 Chamsi-Pasha H., Musgrove C., Morton R. Echocardiographic diagnosis of multiple congenital aneurysms of the sinus of Valsalva. Br Heart J. 1988;59:724-726.
7 Pomerance A., Davies M.J. Congenital aneurysms of all three sinuses of valsalva. J Pathol Bacteriol. 1965;89:607-610.
8 Peszek-Przybyla E., Radwan K., Gruszka A., Krejca M., Buszman P., Sosnowski M. Sinus of Valsalva aneurysm. Cardiology Journal. 2009;16:455-457.
9 Pitta S.R., Kondur A., Afonso L. Quadricuspid aortic valve associated with unruptured sinus of Valsalva aneurysm. Eur J Echocardiogr. 2008;9:575-576.
10 Heilman K.J.3rd, Groves B.M., Campbell D., Blount S.G.Jr. Rupture of left sinus of Valsalva aneurysm into the pulmonary artery. J Am Coll Cardiol. 1985;5:1005-1007.
11 Zannis K., Tzvetkov B., Deux J.-F., Kirsch E.W.M. Unruptured congenital aneurisms of the right and left sinuses of Valsalva. Eur Heart J. 2007;28:1565.
12 Scagliotti D., Fisher E.A., Deal B.J., Gordon D., Chomka E.V., Brundage B.H. Congenital aneurysm of the left sinus of Valsalva with an aortopulmonary tunnel. J Am Coll Cardiol. 1986;7:443-445.
13 Watanabe M., Aoki M., Fujiwara T. Rare type of congenital aneurysm of the right sinus of Valsalva protruding superiorly into the pericardial space. General Thoracic & Cardiovascular Surgery. 2009;57:151-152.
14 Hands M.E., Lloyd B.L., Hung J. Cross-sectional echocardiographic diagnosis of unruptured right sinus of Valsalva aneurysm dissecting into the interventricular septum. Int J Cardiol. 1985;9:380-383.
15 Onat A., Ersanli O., Kanuni A., Aykan T.B. Congenital aortic sinus aneurysms with particular reference to dissection of the interventricular septum. Am Heart J. 1966;72:158-164.
16 Raffa H., Mosieri J., Sorefan A.A., Kayali M.T. Sinus of Valsalva aneurysm eroding into the interventricular septum. Ann Thorac Surg. 1991;51:996-998.
17 Taylor F.H., Sanger P.W., Robicsek F., Ibrahim K. Herniation of ruptured sinus valsalva aneurysm through the tricuspid orifice: case report. Am Surg. 1965;31:171-174.
18 Bardy G.H., Valenstein P., Stack R.S., Baker J.T., Kisslo J.A. Two-dimensional echocardiographic identification of sinus of Valsalva-right heart fistula due to infective endocarditis. Am Heart J. 1982;103:1068-1071.
19 Datta B.N., Berry J.N., Khattri H.N. Infected aneurysm of sinus of Valsalva. Report of a case with involvement of all three sinuses. Br Heart J. 1971;33:323-325.
20 Jick H., Kasarjian P.J., Barsky M. Rupture of aneurysm of aortic sinus of Valsalva associated with acute bacterial endocarditis. Circulation. 1959;19:745-749.
21 Okita Y., Miki S., Kusuhara K., et al. A giant aneurysm of the non-coronary sinus of Valsalva. Thorac Cardiovasc Surg. 1987;35:316-317.
22 Perloff J.K. Sinus of Valsalva-right heart communications due to congenital aortic sinus defects. Am Heart J. 1960;59:318-321.
23 Angelini P. Aortic sinus aneurysm and associated defects: can we extrapolate a morphogenetic theory from pathologic findings? Tex Heart Inst J. 2005;32:560-562.
24 Edwards J.E., Burchell H.B. Specimen exhibiting the essential lesion in aneurysm of the aortic sinus. Proc Staff Meet Mayo Clin. 1956;31:407-412.
25 Ainger L.E., Pate J.W. Rupture of a sinus of Valsalva aneurysm in an infant. Surgical correction. Am J Cardiol. 1963;11:547-551.
26 Perry L.W., Martin G.R., Galioto F.M.Jr., Midgley F.M. Rupture of congenital sinus of Valsalva aneurysm in a newborn. Am J Cardiol. 1991;68:1255-1256.
27 Milewicz D.M., Dietz H.C., Miller D.C. Treatment of aortic disease in patients with Marfan syndrome. Circulation. 2005;111:e150-e157.
28 Tsai Y.C., Wang J.N., Yang Y.J., Wu J.M. Aortico-cameral communication from left sinus Valsalva aneurysm to right atrium via a tortuous tunnel with aneurysmal dilatation. Pediatr Cardiol. 2002;23:108-109.
29 London S.B., London R.E. Production of aortic regurgitation by unperforated aneurysm of the sinus of Valsalva. Circulation. 1961;24:1403-1406.
30 Sakakibara S., Konno S. Congenital aneurysm of the sinus of Valsalva associated with ventricular septal defect. Anatomical aspects. Am Heart J. 1968;75:595-603.
31 Szweda J.A., Drake E.H. Ruptured congenital aneurysms of the sinuses of Valsalva: a report of two cases treated surgically. Circulation. 1962;25:559.
32 Ishii M., Masuoka H., Emi Y., Mori T., Ito M., Nakano T. Ruptured aneurysm of the sinus of valsalva coexisting with a ventricular septal defect and single coronary artery. Circ J. 2003;67:470-472.
33 Fishbein M.C., Obma R., Roberts W.C. Unruptured sinus of Valsalva aneurysm. Am J Cardiol. 1975;35:918-922.
34 Dev V., Shrivastava S. Echocardiographic diagnosis of unruptured aneurysm of the sinus of Valsalva dissecting into the ventricular septum. Am J Cardiol. 1990;66:502-503.
35 Gleason M.M., Hardy C., Chin A.J., Pigott J.D. Ruptured sinus of Valsalva aneurysm in childhood. Am Heart J. 1987;114:1235-1238.
36 Sakakibara S., Konno S. Congenital aneurysms of sinus of Valsalva. A clinical study. Am Heart J. 1962;63:708-719.
37 Sorensen E.W., Kolsaker L. Ruptured aneurysm of sinus of Valsalva. Report of two cases. Acta Med Scand. 1962;172:369-374.
38 Cripps T., Pumphrey C.W., Parker D.J. Rupture of the sinus of Valsalva during pregnancy. Br Heart J. 1987;57:490-491.
39 Krieger O.J., Lee E.B., Lee N.K. Congenital aneurysm of the noncoronary sinus of Valsalva leading to complete heart block: case report. Ann Intern Med. 1956;45:525-534.
40 Jones A.M., Langley F.A. Aortic sinus aneurysms. Br Heart J. 1949;11:325-341.
41 Peters P., Juziuk E., Gunther S. Doppler color flow mapping detection of ruptured sinus of Valsalva aneurysm. J Am Soc Echocardiogr. 1989;2:195-197.
42 Guo D.W., Cheng T.O., Lin M.L., Gu Z.Q. Aneurysm of the sinus of Valsalva: a roentgenologic study of 105 Chinese patients. Am Heart J. 1987;114:1169-1177.
43 Wortham D.C., Gorman P.D., Hull R.W., Vernalis M.N., Gaither N.S. Unruptured sinus of Valsalva aneurysm presenting with embolization. Am Heart J. 1993;125:896-898.
44 Hemp J.R., Young J.N., Harrell J.E.Jr., Woodworth G.R. Late recurrent rupture of a sinus of Valsalva aneurysm. Am J Cardiol. 1989;63:761-762.
45 Chipps H.D. Aneurysm of the sinus of Valsalva causing coronary occlusion. Arch Pathol. 1941;31:627-630.
46 Kawano Y., Tamura A., Kadota J. Klippel-Feil syndrome accompanied by an aneurysm of the non-coronary sinus of Valsalva. Intern Med. 2006;45:1191-1192.
47 Purnell R., Williams I., Von Oppell U., Wood A. Giant aneurysms of the sinuses of Valsalva and aortic regurgitation in a patient with Noonan’s syndrome. Eur J Cardiothorac Surg. 2005;28:346-348.
48 Morganroth J., Perloff J.K., Zeldis S.M., Dunkman W.B. Acute severe aortic regurgitation. Pathophysiology, clinical recognition, and management. Ann Intern Med. 1977;87:223-232.
49 Ahmad R.A., Sturman S., Watson R.D. Unruptured aneurysm of the sinus of Valsalva presenting with isolated heart block: echocardiographic diagnosis and successful surgical repair. Br Heart J. 1989;61:375-377.
50 Davidsen H.G., Petersen O., Thomsen G. Roentgenologic findings in five cases of congenital aneurysm of the aortic sinuses (sinuses of Valsalva). Acta Radiol. 1958;49:205-217.
51 Chiang C.W., Lin F.C., Fang B.R., Kuo C.T., Lee Y.S., Chang C.H. Doppler and two-dimensional echocardiographic features of sinus of Valsalva aneurysm. Am Heart J. 1988;116:1283-1288.
52 Sahasakul Y., Panchavinnin P., Chaithiraphan S., Sakiyalak P. Echocardiographic diagnosis of a ruptured aneurysm of the sinus of Valsalva: operation without catheterisation in seven patients. Br Heart J. 1990;64:195-198.