Agenesis of GB: Congenital absence of GB
 Ectopic GB: Ectopically positioned GB has been reported in nearly every possible position in abdomen and pelvis
Ectopic GB: Ectopically positioned GB has been reported in nearly every possible position in abdomen and pelvis

 near the gallbladder (GB) fundus. This is considered a normal variant given its high prevalence.
near the gallbladder (GB) fundus. This is considered a normal variant given its high prevalence.
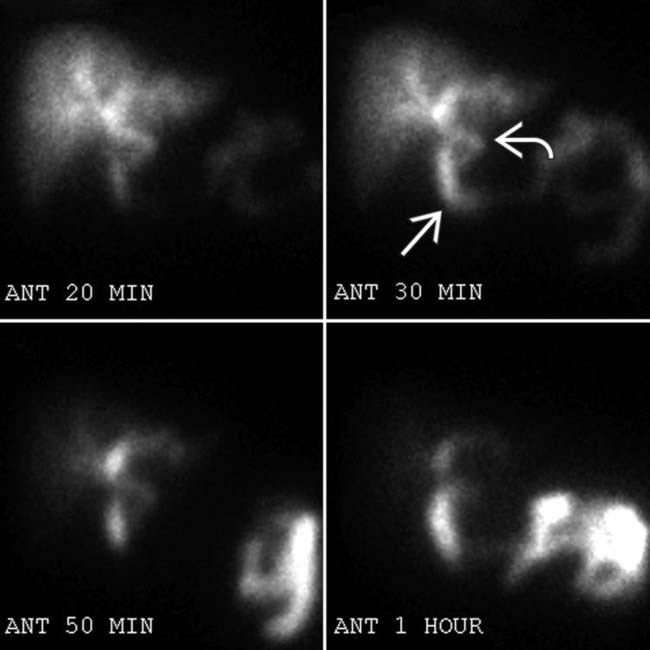
 and proximal small bowel
and proximal small bowel  , but no GB activity. The patient had no operative history and multiple imaging studies confirmed GB agenesis.
, but no GB activity. The patient had no operative history and multiple imaging studies confirmed GB agenesis.TERMINOLOGY
Synonyms
Definitions
• Spectrum of congenital malformations of gallbladder (GB) shape, morphology, number, or position
 Duplicated GB: Duplicated GBs with separate cystic ducts for each moiety
Duplicated GB: Duplicated GBs with separate cystic ducts for each moiety
 Multiseptate GB: Single GB with “honeycomb” appearance due to innumerable internal septations, likely due to incomplete vacuolization of developing GB bud
Multiseptate GB: Single GB with “honeycomb” appearance due to innumerable internal septations, likely due to incomplete vacuolization of developing GB bud
 Congenital diverticulum: Usually a true diverticulum (containing all layers of GB wall) that can be located anywhere in GB
Congenital diverticulum: Usually a true diverticulum (containing all layers of GB wall) that can be located anywhere in GB
 Ectopic GB: Ectopically positioned GB has been reported in nearly every possible position in abdomen and pelvis
Ectopic GB: Ectopically positioned GB has been reported in nearly every possible position in abdomen and pelvis
 Duplicated GB: Duplicated GBs with separate cystic ducts for each moiety
Duplicated GB: Duplicated GBs with separate cystic ducts for each moiety
 Multiseptate GB: Single GB with “honeycomb” appearance due to innumerable internal septations, likely due to incomplete vacuolization of developing GB bud
Multiseptate GB: Single GB with “honeycomb” appearance due to innumerable internal septations, likely due to incomplete vacuolization of developing GB bud Congenital diverticulum: Usually a true diverticulum (containing all layers of GB wall) that can be located anywhere in GB
Congenital diverticulum: Usually a true diverticulum (containing all layers of GB wall) that can be located anywhere in GB
 Ectopic GB: Ectopically positioned GB has been reported in nearly every possible position in abdomen and pelvis
Ectopic GB: Ectopically positioned GB has been reported in nearly every possible position in abdomen and pelvis
IMAGING
CT Findings
• GB agenesis: Absence of GB in patient with no history of prior cholecystectomy; should exclude prior history of cholecystectomy or ectopic position of GB before arriving at this diagnosis
• Bilobed GB: External contour of GB may be normal and division between duplicated GB cavities may be imperceptible
• Duplicated GB: External contour of GB may or may not be normal; separate cystic ducts and cystic arteries leading to 2 separate GBs in close contiguity
PATHOLOGY
General Features
• Normal embryology
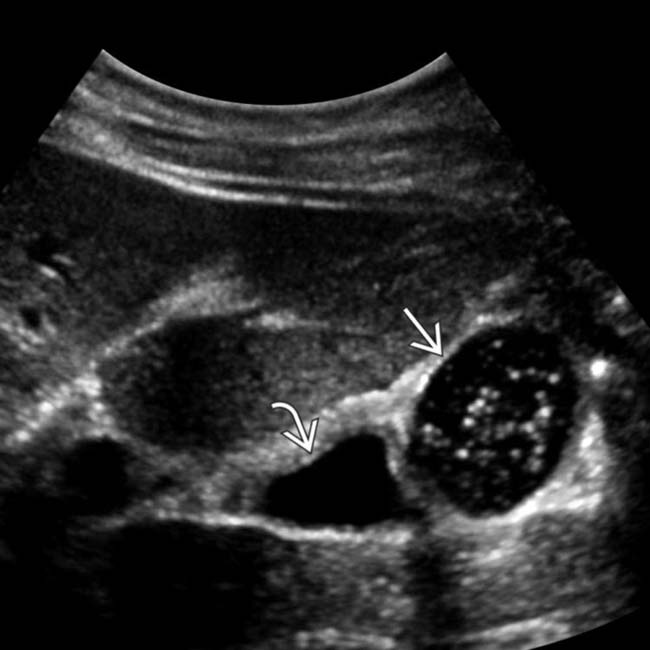
 and the other containing sludge
and the other containing sludge  .
.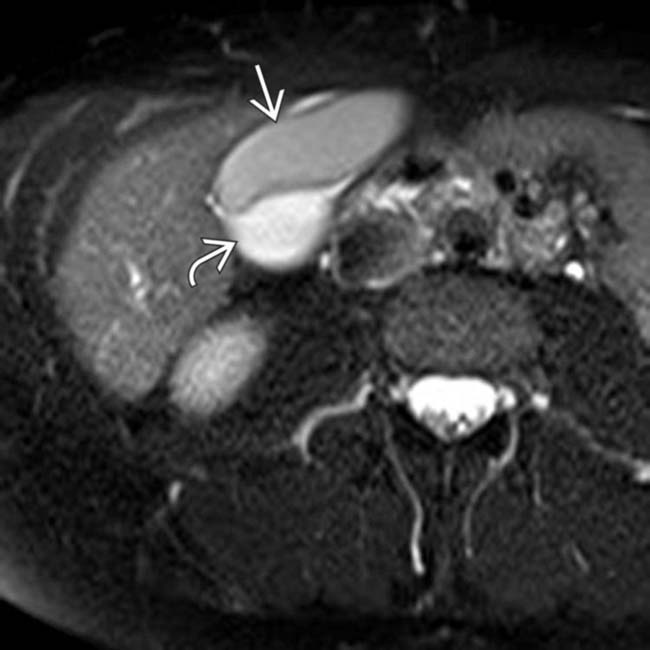
 , and the other showing intermediate to high T2 signal
, and the other showing intermediate to high T2 signal  . Two separate cystic ducts were seen on MRCP (not shown), allowing the diagnosis of a duplicated GB (rather than a bilobed GB).
. Two separate cystic ducts were seen on MRCP (not shown), allowing the diagnosis of a duplicated GB (rather than a bilobed GB).
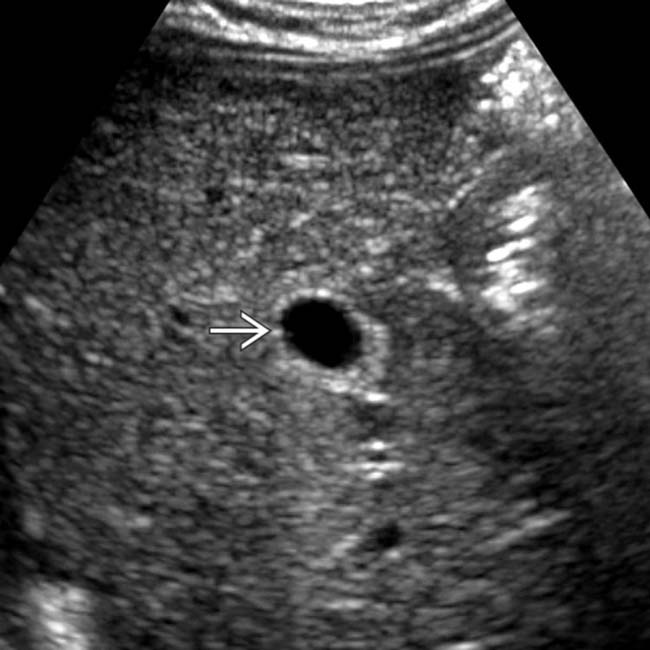
 within both lobes of a bilobed GB.
within both lobes of a bilobed GB.
 . Both lobes of a bilobed GB share a common cystic duct. Persistent abdominal pain and leukocytosis prompted cholecystostomy drainage of the more superficial GB. Both lumina were successfully decompressed.
. Both lobes of a bilobed GB share a common cystic duct. Persistent abdominal pain and leukocytosis prompted cholecystostomy drainage of the more superficial GB. Both lumina were successfully decompressed.









 .
.























































 . As an isolated finding this is not clinically significant, although the location of the GB may make cholecystectomy exceedingly difficult.
. As an isolated finding this is not clinically significant, although the location of the GB may make cholecystectomy exceedingly difficult.
 adjacent to the GB. The configuration of the “cyst” is characteristic of GB duplication. Both the GB and the “cyst” are partially opacified via separate cystic ducts on a follow-up Eovist enhanced MRCP.
adjacent to the GB. The configuration of the “cyst” is characteristic of GB duplication. Both the GB and the “cyst” are partially opacified via separate cystic ducts on a follow-up Eovist enhanced MRCP.


