Chapter 10 Condylar Fractures in Children
Introduction
The age of occurrence depends on the anatomical location. The average age for lateral condylar injuries is around 6 years.1,2 The less common medial condylar injuries occur in the age range 8–12 years.2,3 T-condylar fractures are more common in adolescents but occur in children in the age range 5–12 years (average 8.8 years).4 Fractures involving the entire distal humeral physis may be misdiagnosed as lateral condylar fractures. They should be suspected in a child below 1 year of age but can occur from birth to 6 years.5–7 They have an association with child abuse.
Epicondylar fractures are often associated with dislocations of the elbow and have a peak incidence in the 6- to 12-years age group.8–11
Lateral condylar fractures
Background/aetiology
Fractures of the lateral condyle in children represent 15% of all paediatric elbow fractures and are the second most common childhood elbow injury after supracondylar fractures (70%).12
These fractures constitute 75% of distal humeral physeal fractures.12 It is noted that fractures that exit in the trochlear notch will lead to an element of elbow instability with subluxation of the radius and ulna with the lateral condylar fragment.
Dislocation in association with a lateral condylar fracture has been reported by Rasool.13 He described 14 cases with a posteromedial dislocation and lateral condylar fracture, five of which also had a fracture of the medial epicondyle. He stressed the importance of looking for a lateral condylar fracture in children with a dislocation of the elbow.
Classification
Anatomical location
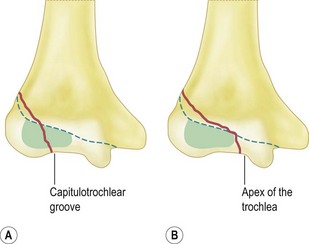
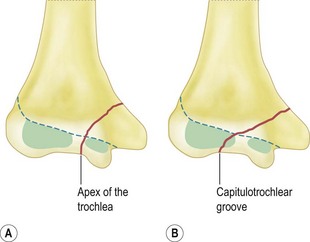
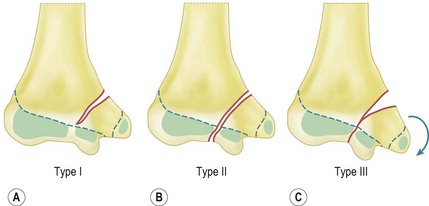
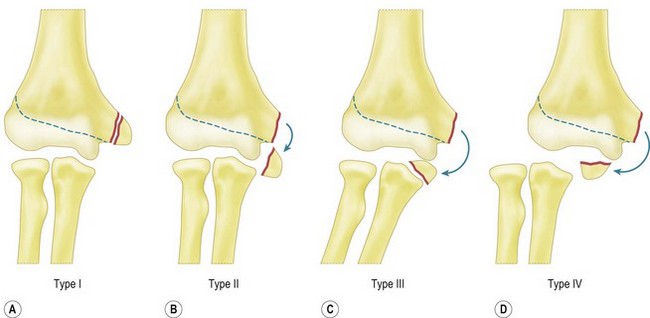
Milch15 described type I and II lateral condylar fractures (Fig. 10.1). In both types, the fracture line begins at the posterolateral aspect of the lateral condyle in the metaphysis:
Staging
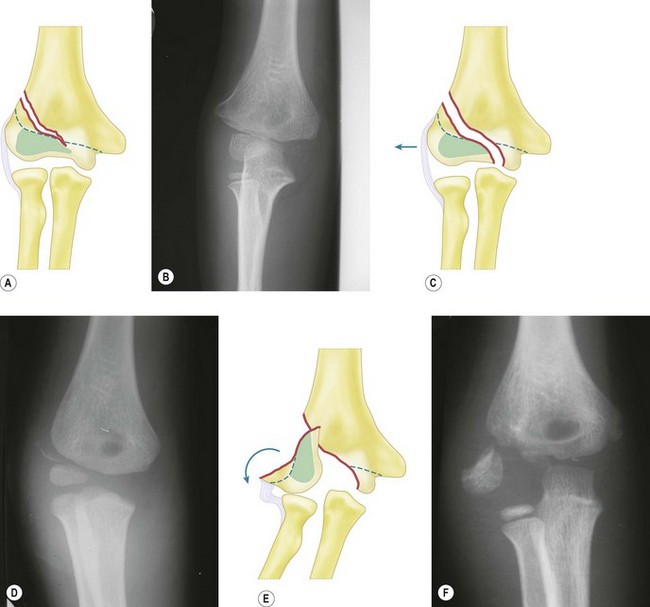
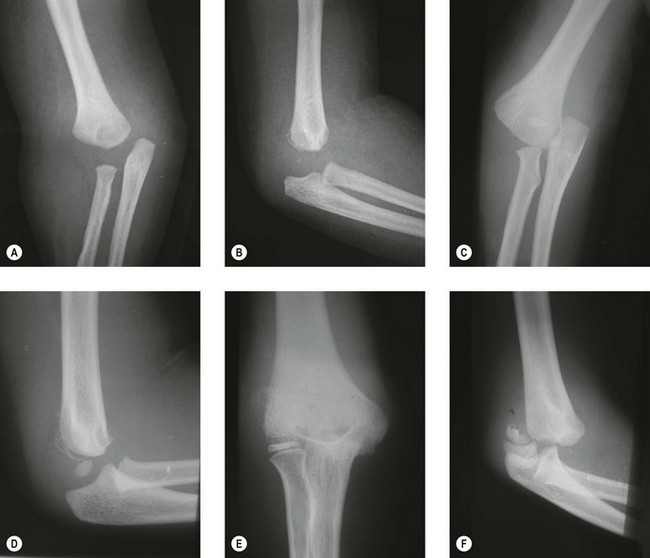
Jakob et al16 described three stages of displacement (Fig. 10.2):
Badelon et al17 modified this classification into four stages. In stage I the fracture line is seen on only one X-ray view and displaced less than 2 mm. In stage II the fracture line is seen on both the anteroposterior (AP) and lateral views but remains displaced less than 2 mm. Stages III and IV are the equivalent of Jakob stage II and stage III, respectively. The addition of the extra stage was to distinguish which fractures were unstable and more likely to displace and thus identify which should be fixed. They determined that stage I could be treated conservatively by plaster immobilization but stages II, III and IV required open reduction and internal fixation.
We use the thee-stage classification of Jakob et al in this text.
Mechanism of injury
Two mechanisms of injury are proposed:
Presentation, investigation and treatment options
Clinical features
In stage I displacement there may be no or minimal swelling and only local tenderness over the lateral condyle, this sign being key to the diagnosis. This can be confirmed by eliciting pain when passively flexing the wrist. In an undisplaced fracture not appreciated on X-ray, the presence of lateral ecchymosis may be the only clinical sign and should alert the clinician to the possible presence of this fracture.19 In addition, swelling is localized to the lateral side of the elbow only.
Investigations
Radiographs
The metaphyseal fragment is often small and minimally displaced, with displacement best appreciated on the lateral view. Badelon et al17 found that if the fracture could only be appreciated on one view then it was stable, but if seen on both views there was more likelihood that the articular hinge was disrupted, making the fracture unstable. The relationship of the proximal ulna and radius to the humerus must be studied since lateral subluxation of the distal radius and ulna imply a Milch II fracture with disruption of the articular hinge.
Finnbogason et al20 reviewed 112 undisplaced and minimally displaced fractures and classified them as stable fractures, fractures with an undefinable risk and high-risk fractures. Stable fractures had no gap or a minimal gap that did not extend all the way to the epiphyseal cartilage (65 cases, none of which had lateral displacement). Fractures with an undefinable risk showed the fracture line extending all the way to the epiphyseal cartilage (displacement occurred in 6 (17%) of 35 fractures). High-risk fractures had a fracture gap that was almost as equally separated laterally and medially. Five (42%) of 12 of these fractures displaced.
Oblique radiographs may improve the diagnosis and Song et al21 found that the internal oblique view was significantly more accurate in demonstrating the fracture gap and fracture pattern than the AP and lateral views. They concluded that classifications should be based on the greatest displacement seen on at least three views, namely AP, lateral and internal oblique.
Arthrogram (Fig. 10.3)
Arthrograms have been shown to increase the accuracy of diagnosis. Yates and Sullivan22 showed that the initial diagnosis on plain radiographs was altered in 7 of 36 (19%) children with elbow injuries.
CT scan
Chapman et al23 showed that multi-detector computed tomography, which can be done in children without using sedation, was highly reproducible in characterizing lateral condylar fractures and frequently demonstrated disruption of the articular surface. It may lead to a change in treatment for children with fracture displacement near the threshold of 2 mm.
MRI
Kamegaya et al24 performed MRI on 12 patients with fractures of less than 2 mm displacement as seen on plain radiographs. Fractures that passed through the articular surface into the joint were deemed unstable. One of five fractures that had 1 mm displacement was found to be unstable and four of seven with 2 mm displacement were found to be unstable. This study suggests that MRI is a useful and accurate method of assessing fracture stability and enables the identification of fractures that would be better treated by pin fixation rather than cast immobilization.
Treatment
Plaster immobilization
Immobilization is appropriate for 30–40% of lateral condylar fractures.17,26 Badelon et al17 stated that in cases where the fracture is seen in only one view and displaced less than 2 mm (i.e. stable fracture) immobilization is adequate. Speed and Macey27 showed uniformly good results using this method and had no abnormalities of growth or premature fusion. Some authors have recommended placing the forearm in supination to decrease the muscle pull of the extensors and reduce the risk of displacement on the distal fragment.
Late displacement is the concern with simple immobilization. Beaty and Kassar28 had two cases of late displacement out of 24 stage I fractures. Their criteria for plaster immobilization was displacement of less than 2 mm on three X-ray views (AP, lateral and internal oblique).
Closed reduction and pinning for stage II
Mintzer et al29 reported good results after percutaneous pin fixation in 12 fractures with displacement of less than 2 mm. Joint congruity was checked with an arthrogram.
Open reduction and internal fixation
This is the most widely recommended treatment for stage II and stage III fractures because of the propensity for late displacement and the potential for late complications. The key is to have accurate reduction; Hardacre et al1 showed poor results when the reduction was inadequate.
With open reduction, care must be taken to avoid dissection at the posterior aspect of the fragment as this is the site of the fragment’s blood supply. The reduction must be adequate and this is done by direct visualization. Mohan et al30 reported the use of a posterolateral approach that is more cosmetic and provides excellent exposure with minimal dissection. They had no complications in 20 patients.
Methods of fixation
Most authors recommend smooth pins as these do not affect the growth plate. At least two K-wires should be used and can be inserted parallel or crossed. If there is an adequate metaphyseal fragment then one wire can be passed through this fragment. Pins can be buried under the skin or left protruding. There is controversy as to how long the pins need to be left in situ and, although some authors recommend 6 weeks, it has been shown that 3 weeks is sufficient.31
Although smooth pins are preferred Sharma et al32 used partially threaded cancellous screws.
Outcome
Badelon et al17 and Speed and Macey27 reported excellent results in patients with undisplaced fractures.
Bast et al33 reported union rates of 98% following non-operative treatment for undisplaced or minimally displaced fractures.
Ippolito et al34 evaluated 49 individuals at a follow-up of 18–45 years. Twenty fractures with displacement of 2–10 mm without tilting had been treated non-operatively and 36 with displacement and tilting had been treated surgically. All patients had a good result.
Treatment
Stage I fractures
These are treated in an above-elbow backslab with the forearm in pronation and the elbow flexed to 90°. The pronation creates a compressive force on the lateral condyle.35 A check X-ray is performed in the backslab at 1 week and the backslab left on for a total of 3 weeks. Active mobilization is then undertaken without physiotherapy.
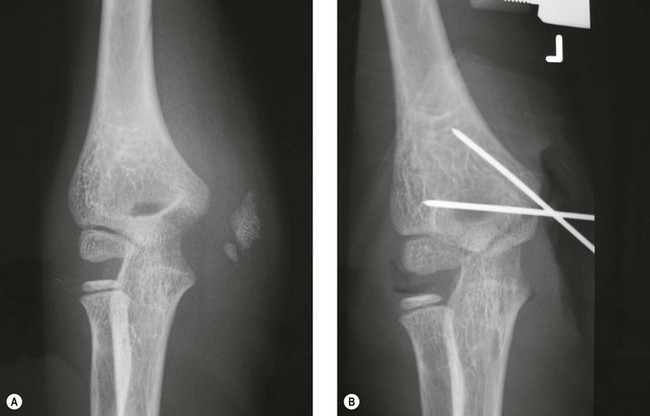
Stage II and III fractures
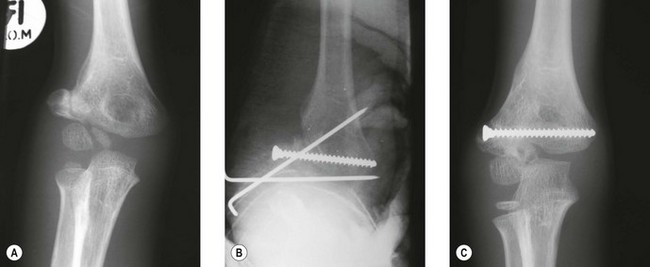
Stage II and III fractures require open reduction and internal fixation. The proximal limb of the Kocher J incision is used and the fracture exposed by opening the fascia between brachioradialis and ECRL. The reduction may be difficult to hold but is assisted with the use of small fragment reduction forceps. It is checked by direct visualization of the anterior aspect of the joint. This is exposed by cutting the synovial attachment to the distal fragment. K-wires (1.6 mm) crossing at the lateral edge of the metaphysis are angulated from each other by approximately 60° (Fig. 10.4). The wires are left protruding through the skin and the end is bent to a right angle. A backslab is applied for 3 weeks with the elbow flexed at 90° and the forearm in neutral rotation. The plaster and wires are removed in the outpatient clinic without anaesthesia.
Complications
Lateral spur formation/lateral condylar overgrowth with cubitus varus
This is seen in 40–50% of patients with loss of carrying angle.27,36,37 De Jager and Hoffman26 reviewed 60 patients following lateral condylar fractures and found an average of 4 mm of lateral condylar overgrowth and an average of 3° loss of the carrying angle. It occurs in those treated operatively or non-operatively and can lead to clinical cubitus varus depending on the pre-morbid carrying angle. It is rarely of cosmetic or functional significance. It is important, however, to warn parents that this deformity may occur.
Delayed union
Delayed union (failure of union within 12 weeks) may occur even when the fracture has been adequately reduced. Reasons include poor vascular supply to the fragment38 or synovial fluid passing between the fracture fragments.1 The fragments remain reduced and eventually unite.
Non-union
Non-union is defined as no union by 12 weeks.38 It occurs with stage II or III fractures that are untreated, present late or are inadequately reduced.
The management of non-unions is controversial. Jakob et al16 and Dhillon et al39 reported that patients who were treated after 3 weeks had the same results as patients who had no treatment at all. Complications included loss of motion, delayed union and non-union, deformity and avascular necrosis.
Other authors have reported success with operative treatment prior to closure of the growth plate.1,38,40 Shimada et al41 reported good results at an average of 11 years follow-up. The average time between injury and surgery was 5 years (5 months to 10 years). One poor result was due to avascular necrosis.
The main concern with late surgery is the risk of avascular necrosis. Speed and Macey27 reported a high incidence of ‘epiphyseal changes’ in patients treated with late surgery. Yang et al,42 however, reported low rates of avascular necrosis and good results by approaching the non-union through an olecranon osteotomy, thus not disrupting the soft tissue attachment to the fragment.
Some patients who are seen years after their fracture (Fig. 10.5) may never have sought treatment at the time of the injury. They present with cubitus valgus. In addition, tardy ulnar nerve palsy may be noted, although this does not normally occur until an average of 22 years after the injury.43 When present, motor loss is usually followed by sensory changes. Papandrea and Waters44 recommended that late presentations were treated by a two-stage procedure. The first stage involved fixation and bone grafting of the non-union with anterior transposition of the ulnar nerve. At a later stage an osteotomy was advised. Milch15 described a transverse osteotomy and, more recently, Tien et al45 has advocated a dome osteotomy with fixation of the non-union through a posterior approach. This is thought to be associated with a reduced rate of complication.
Avascular necrosis
This can involve either the entire lateral condyle or result in a fishtail deformity.
Entire lateral condyle
This is usually iatrogenic and results from disturbance of the extra-osseous blood supply to the fragment. The blood enters via vessels that pierce the condyle in the posterior non-articular area.46 It may occur at the time of surgery for an acute fracture where there has been overzealous stripping of the soft tissue, but is more common in late surgery or surgery for non-unions. Some authors have advocated a transolecranon approach to avoid damaging the blood supply when treating non-unions.42
Fishtail deformity
The so-called fishtail deformity occurs with damage to the intra-osseous end arteries that supply the lateral part of the medial crista of the trochlea. It may also occur in undisplaced supracondylar fractures, medial condylar fractures, fractures of the entire distal humeral physis46 and from persistence of a gap between the lateral and medial ossification centres.47–49
Personal view
Non-union
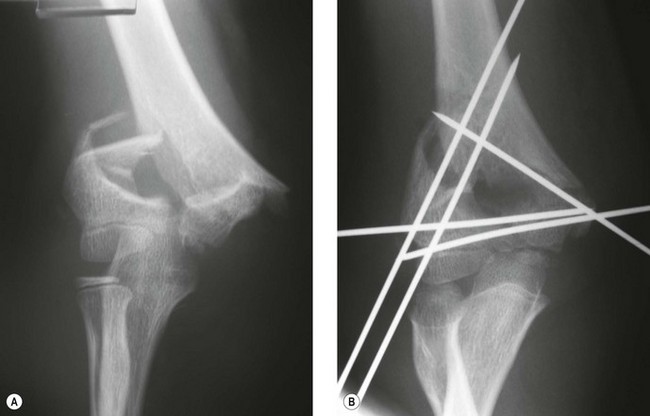
In stage II, the fragment has moved upwards and is tilted laterally and forward. The fragment is mobilized, reduced and held with an oblique K-wire passing through the epiphysis (left out the skin) and with a horizontal 3.5 mm cancellous screw (preferably partially threaded) through the metaphyseal fragment to provide compression (Fig. 10.6). The K-wire is removed at 3 weeks and the elbow mobilized actively. Physiotherapy is not usually necessary.
In stage III, the fragment is rotated. It is mobilized and reduced into a position that allows a functional reduction, i.e. the reduction that yields the best range of movement intraoperatively.40 In addition, in stage III, bone graft may be required. The postoperative management is the same as for stage II.
Medial condylar fractures
Introduction
These fractures are rare and account for less than 1% of fractures of the distal humerus.12 However, as they are intra-articular fractures they require accurate reduction to avoid later complications.
Background/aetiology
Infants may sustain this injury but more commonly they occur in the age range of 8–14 years.50 The fracture line extends from the metaphysis of the medial condyle and exits between the ossification centres of the lateral and medial condyle (apex of the trochlea) or through the lateral condylar epiphysis (capitulotrochlear groove). The fragment includes the medial epicondyle and the attached flexor muscles. These muscles cause the fragment to rotate so that the articular surface of the fragment faces posteriorly and laterally.
In younger children there is an association with child abuse,51,52 but the fracture also occurs with greenstick fractures of the olecranon and true posterolateral dislocations of the elbow.51,53
Classification
Salter–Harris14
This fracture is most likely a Salter–Harris II injury since untreated fractures result in non-union with cubitus varus rather than physeal arrest, which is more likely to occur with a Salter–Harris IV injury.54 However, the paucity of reported cases has meant that this has yet to be conclusively determined.
Anatomical location
Displacement of the fracture
This has been divided into three types by Kilfoyle55 (Fig. 10.8):
Mechanism of Injury
Two mechanisms of injury have been described. With a fall on the point of the flexed elbow, the semilunar notch of the olecranon impacts against the trochlear notch and initiates the fracture.52,56–58 The second mechanism involves a fall onto the outstretched arm, resulting in an avulsion injury secondary to valgus strain.3,59
Presentation, investigations and treatment
Radiology
X-rays
In the younger child before ossification of the trochlea, it may be difficult to differentiate this fracture from a medial epicondyle fracture.3,60,61 One must have a high index of suspicion, especially if there is a metaphyseal fragment with the medial epicondyle. To differentiate the two the following must be observed:
Outcome
As type III fractures occur in older children and are more severe, the results in these patients are less satisfactory than in younger patients, who tend to sustain type I or type II injuries.3,56,60
Complications
Leet et al62 reported a 33% incidence of complications (21 fractures), which included non-unions, avascular necrosis and loss of reduction. In addition ulnar nerve injury has been reported,59 but is uncommon. It is more likely to occur iatrogenically as the result of injury at the time of surgery.
Delayed or non-union
This is usually the result of an unrecognized displaced fracture treated conservatively with immobilization. It may also occur following surgery if fixation is inadequate.55,59
T-condylar fractures
Introduction
This is a rare injury in the skeletally immature child. In our unit we see one in every 150 displaced supracondylar fractures.4
Background/aetiology
The average age at presentation is 8.8 years. In these children, the largely cartilaginous distal humerus is more elastic and the articular surface may remain intact.4,63 Displacement is in the osseous supracondylar area.
Classification
Presentation, investigation and treatment
Radiology
X-rays
The key to diagnosis is the vertical fracture line extending into the apex of the trochlea on the AP radiograph. This may not always be clear on the preoperative X-ray but is normally obvious on a traction view taken intraoperatively.4,65 If, despite this, the diagnosis remains in doubt an arthrogram should be performed.
Under the age of 4 years, the distal end of the humerus is largely cartilaginous and only the capitellum is ossified. What appears to be an isolated lateral condylar fracture may have an intercondylar extension without a Thurston-Holland metaphyseal fragment visible on the X-ray to indicate an associated fracture of the medial condyle. For this age group Beghin et al65 recommended varus and valgus stress views in preference to arthrograms in children with isolated displaced condylar fractures in order to exclude a T-condylar extension.
Treatment
As these are intra-articular fractures they require accurate restoration of the articular surface.63,65–67 They are prone to stiffness and require early motion if possible. The treatment options include:
Closed reduction and percutaneous fixation
Mulder and Hoffman4 employed smooth wires and Kanellopoulus and Yiannakopoulos68 utilized threaded K-wires to effect compression of the intra-articular fracture fragments. Mulder and Hoffman4 found that in skeletally immature patients under the age of 12 years the articular cartilage remains intact and its elasticity protects the articular surface from disrupting.
Open reduction and fixation
When closed reduction cannot be achieved, open reduction and fixation of the fracture with multiple K-wires should be undertaken. Some authors utilize compression screws to hold the articular fragments together and then fix the restored articular fragment to the shaft with K-wires.64 The wires are removed at 3 weeks and if there is evidence of union on X-ray mobilization is commenced.
Papavasiliou and Bestlikas63 reported on a posterior triceps splitting approach in six cases of children under the age of 14 years. Re69 in 15 cases, where they used either a posteromedial triceps sparing approach70 or an olecranon osteotomy, found that patients had significantly better extension with a triceps-sparing approach. They also found that the use of continuous passive motion (CPM) resulted in restoration of motion earlier, with greater flexion, than when CPM was not used.
In the adolescent fixation with plates provides rigid fixation allowing early mobilization (see adult fractures, Ch. 16).
Outcome
In a review of three series,63,66,67 29 of 30 fractures were treated surgically and all but one had a good or very good outcome at follow-up. Mulder and Hoffman4 reported good and excellent results in eight of nine patients followed up for an average of 3.5 years (2–5 years).
Complications
Stiffness
This is the most common complication. Although there is normally a greater loss of extension than flexion, it is not usually functionally significant.63,66,67
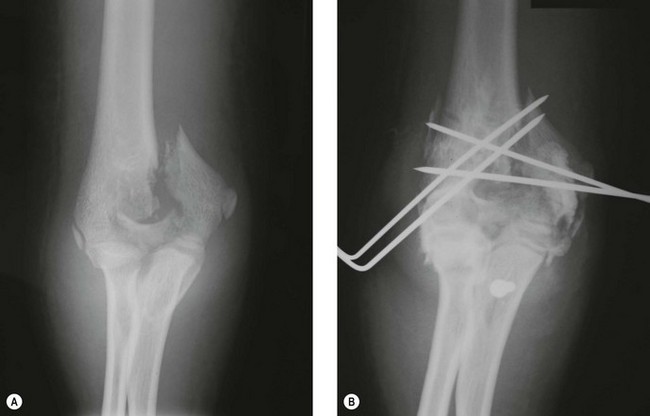
Personal view
In the skeletally immature child, our experience is that the articular cartilage remains intact, and we have had good results with closed reduction and pinning.4 We utilize two K-wires – one from each side – to hold the intra-articular split and then two lateral and one medial wire to hold the reduced fragments to the humeral shaft (as for supracondylar fractures) (Fig. 10.10). The wires are removed at 3 weeks and active mobilization started.
Fracture of the entire distal humeral physis
Introduction
This fracture was originally thought to be rare but was most likely often overlooked.5,7,72–75 Its importance lies in the difficulty of differentiating it from a fracture of the lateral condyle.
It is also important as it has an association with child abuse and thus the physician must have a high index of suspicion when seeing an infant with this fracture (Fig. 10.12).5,7,72 It accounts for 5% of all elbow fractures in our unit.12
Background/aetiology
Mechanism of injury
The most likely mechanism of injury is a rotatory force on the elbow, as would occur in birth injury or child abuse cases. Hyperextension injury is unlikely in the newborn and young infant as they often have a residual flexion contracture of the elbow secondary to intrauterine positioning which prevents hyperextension. Bright76 has shown that physes are more likely to fracture with bending or tension forces, although falls are also a common cause.75
Classification
DeLee et al5 classified this injury into three groups according to age (Fig. 10.13):
Presentation, investigations and treatment
The newborn may present with a pseudoparalysis. The clinical signs may be minimal, with slight swelling and crepitus.77 The swelling will be present on both sides of the elbow (medial and lateral).
As there is an association with child abuse, particularly in children under 1 year, other injuries should be excluded (Fig. 10.12).5,7
Radiology
Differential diagnosis
This fracture is most commonly confused with a fracture of the lateral condyle.
In stage III lateral condylar fractures the relationship between the radial head and the capitellum (Storen’s line) is disrupted. In EDHP fractures Storen’s line remains intact irrespective of the posteromedial displacement (Fig. 10.14).5
In stage II lateral condylar fractures the relationship between the radial head and capitellum may be maintained. However, an increase in Baumann’s angle (due to lateral tilt of the condyle) and anterior tilt of the capitellum is diagnostic. In EDHP fractures posterior translation of the capitellum is present (Fig. 10.15).81
DeLee et al5 reported posteromedial translation in all cases of EDHP fractures; however, Mackerdhuj et al81 found it to be present in only 30%, the rest being posterior.
In a prospective study using the above parameters, Mackerdhuj et al81 were able to differentiate between stage II lateral condylar fractures and EDHP fractures in 19 of 20 cases. Only one case required an arthrogram (Fig. 10.16).
Treatment
Manipulation and percutaneous pinning
For fractures that are unstable and displaced, manipulation and percutaneous pinning may be performed.7 If, however, there is significant swelling over the medial aspect of the joint, identification of the epicondyle can be difficult and there is risk to the ulnar nerve.71 A small medial incision reduces the risk and enables the safe insertion of the medial pin.
Open reduction and pinning
Some authors have advocated open reduction and pinning. Mizuno et al74 recommended this because of his poor results with closed reduction.
Fractures of the medial epicondyle
Background/aetiology
These are relatively common fractures, with an incidence of between 9% and 14% of fractures of the elbow.12,82 They are more common in boys and occur in the age range of 6–14 years (average 10 years).9,11,82 This is similar to the age distribution of medial condylar fractures. They are commonly associated with elbow dislocations, with a reported incidence of 50%.9,11,82
It begins to ossify at between 4 and 6 years of age and fuses when the child is approximately 15 years old. During its ossification it may appear fragmented, simulating a fracture.83
Attachments
Medial collateral ligament
The medial collateral ligament originates from the medial epicondyle and consist of three bands: anterior, posterior and transverse. The anterior band is the main stabilizer against valgus forces and is taut in extension. The posterior band is taut in flexion.84
Capsule
As the capsule is attached up to the physeal line in young children, a fracture line involving the medial epicondyle may be intra-articular. As growth occurs the epicondyle migrates proximally and becomes extra-articular. The fracture usually involves the apophysis only but may also include a small metaphyseal fragment or may even split the apophysis.83
Mechanism of injury
There are three mechanisms of injury:
Direct blow
This is an uncommon cause, but when it occurs there may be marked bruising and fragmentation of the fracture fragment.18,85
Avulsion
The common flexor origin muscles produce a significant force on the medial epicondyle with a fall on the outstretched arm where the elbow is extended and goes into valgus. The addition of extension of the wrist further tightens and increases the forces in the flexor muscles. Evidence that these forces avulse the medial epicondyle emanates from the associated injuries, which are also common with a valgus force, i.e. radial neck fractures and greenstick fractures of the olecranon.55 Further evidence that suggests this is the cause of some epicondylar fracture is the high incidence of this injury in wrestlers near skeletal maturity.86
Dislocation of the elbow
In dislocations of the elbow it is the ulnar collateral ligament that produces the avulsion force. With spontaneous reduction of the dislocation or subluxation the epicondylar fracture fragment may be trapped in the joint without an apparent dislocation. Testimony to spontaneous reduction is the presence of calcification in the lateral collateral ligament and periosteum with this fracture.82,87 Patrick88 theorized that the incarceration may occur without a dislocation but with extreme valgus whereby the vacuum created caused the fragment to be sucked into the joint. Approximately 50% of children with an elbow dislocation will have a medial epicondyle fracture and in approximately 7–15% the medial epicondyle will become incarcerated between the joint surfaces.9,11,82
Presentation, investigations and treatment
Clinical features and radiology
Displaced fractures (Fig. 10.19)
Displaced fractures are more evident clinically and easily appreciated on X-ray.
Some authors test the elbow for valgus instability.84,90 This is performed with the patient supine, the arm abducted 90°, the shoulder externally rotated 90° and the elbow flexed at least 15° to unlock the olecranon. On the AP view, if the medial side opens more than 2 mm compared to the resting state the elbow is regarded as unstable. This is called the valgus gravity stress test.
Incarceration without dislocation (Fig. 10.20)
Examination reveals a block to movement and the fragment usually lies in the trochlear notch. On X-ray, if the fragment is level with the joint incarceration must be excluded.58 The elbow joint will not be fully reduced.
Radiology
Differential diagnosis60,61
If there is any doubt about the diagnosis, an arthrogram is indicated.
Treatment
Controversy arises when there is displacement of greater than 5 mm (type II). Most authors recommend conservative treatment.48,82,91–93 Smith91 in a classic paper disputed the misconception that this was a severe injury and reported that conservatively treated patients did well.
Surgical treatment is advised by Woods and Tullos90 in the throwing athlete or in athletes who requires a stable elbow (e.g. gymnasts, tennis players, wrestlers) when there is a positive valgus gravity stress test. Hines et al10 recommended open reduction and fixation when the epicondyle is displaced greater than 2 mm. Lee et al11 found no cases of late instability in type II fractures and advised conservative treatment in all cases.
Reports show similar results for non-operative and operative treatment.8–11
Incarcerated fragment
Roberts94 described a method for manipulating the fragment out of the joint. Under sedation or anaesthesia, a valgus stress is applied to the flexed elbow while supinating the forearm. This unlocks the radial head, takes the median nerve away and relaxes the pronator origin. The wrist and fingers are simultaneously extended. This method may work if done within 24 h of the fracture. It has been reported to work in 87% of cases of type IV injury and 66% of cases of type III injury.11
If there is ulnar nerve involvement, manipulation should not be undertaken and open reduction performed.87
Even if the incarceration has been discovered late, surgery has been shown to give good results. Fowles et al92 reported that patients regained 80% of their movement when operated on at an average of 14 weeks post injury. Even when not extracted, the functional loss may not be severe.95 Rosenthal reported an 8-year follow-up where the fragment had united to the ulna with a prominence but only minor loss of motion.95
Complications
Nerve injury
A careful neurological examination of the arm, with particular reference to the median and ulnar nerves, is essential. The median nerve may be entrapped within the joint after reduction of an elbow dislocation, and any patient presenting with symptoms and signs of median nerve dysfunction in this situation should be explored immediately.44
The overall incidence of ulnar nerve complications following medial epicondylar fractures is 10–16%.82 The majority are neuropraxias, which recover with time. In the presence of complete ulnar nerve palsy, however, the nerve should be explored. Late dysfunction of the ulnar nerve due to entrapment by scar tissues has been shown not to occur.86,89
With incarcerated medial epicondylar fractures the incidence of ulnar nerve pathology is 50%.82 In the presence of ulnar nerve symptoms and signs, and an incarcerated fragment with or without dislocation, a manipulation should not be performed as it may further compromise ulnar nerve function.88 In this situation an open exploration of the joint should be performed. The prognosis for nerve recovery is worse when there is a delay in the diagnosis of an incarcerated fragment.
Non-union
Although up to 50% of fractures fail to unite, it is usually of no consequence to the majority of patients.11
Fractures of the lateral epicondylar epiphysis
Introduction
This is an extremely rare injury; it is important to recognize and appreciate that the fragment may become incarcerated in the joint.96
Background/aetiology
This apophysis ossifies in the second decade (10–11 years). Ossification begins distally at the level of the condylar physis and proceeds proximally. It has either a triangular shape or appears as a sliver of bone.97
Mechanism of Injury and displacement
Displacement
Displacement is dependent on the location of the fracture.98 If the fracture line starts between the origins of the common extensors and the extensor carpi radialis longus, displacement is minimal. If it starts in the area of origin of the extensor carpi radialis longus then displacement may be marked.
1 Hardacre JA, Nahigian SH, Froimson AI, et al. Fractures of the lateral condyle of the humerus in children. J Bone Joint Surg Am. 1971;53:1083-1095.
2 Landin LA, Danielson LG. Elbow fractures in children: an epidemiological analysis of 589 cases. Acta Orthop Scand. 1986;57:309-312.
3 Fowles JV, Kassan MT. Displaced fractures of the medial humeral condyle in children. J Bone Joint Surg Am. 1980;62:1159-1163.
4 Mulder MJ, Hoffman EB. Displaced T-condylar fractures of the distal humerus in children. SA Orthop J. 2007;6(2):18-24.
5 DeLee JC, Wilkins KE, Rogers LF, et al. Fracture-separation of the distal humeral epiphysis. J Bone Joint Surg Am. 1980;67:46-51.
6 Moucha CS, Mason DE. Distal humeral epiphyseal separation. Am J Orthop. 2003;32:497-500.
7 de Jager LT, Hoffman EB. Fracture separation of the distal humeral epiphysis. J Bone Joint Surg Br. 1991;73:143-146.
8 Papavasiliou VA. Fracture-separation of the medial epicondylar epiphysis of the elbow joint. Clin Orthop. 1982;171:172-174.
9 Wilson NI, Ingram R, Rumaszewski I, et al. Treatment of fractures of the medial epicondyle of the humerus. Injury. 1988;19:342-344.
10 Hines RF, Herndon WA, Evans JP. Operative treatment of medial epicondylar fractures in children. Clin Orthop. 1987;221:170-174.
11 Lee AS, Knudsen CJ, Hoffman EB. Fractures of the medial epicondyle of the humerus. Presented at South African Orthopaedic Congress 1993, Bloemfontein;.
12 Hoffman EB. Incidence of fractures at Red Cross Children’s Hospital, Cape Town. Personal communication.
13 Rasool MN. Elbow dislocation with lateral condyle fracture in children. SA Orthop J. 2006;5(3):72-78.
14 Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am. 1963;45:587-632.
15 Milch H. Fractures and fracture dislocations of the humeral condyles. J Trauma. 1964;4:592-607.
16 Jakob R, Fowles JV, Rang M, Kassab MT. Observations concerning the lateral humeral condyles in children. J Bone Joint Surg Br. 1975;40:430-436.
17 Badelon O, Bensahel H, Mazda K, et al. Lateral humeral condylar fractures in children: a report of 47 cases. J Pediatr Orthop. 1988;8:31-34.
18 Stimson LA. A practical treatise on fractures and dislocations. Philadelphia, PA: Lea Brothers; 1900.
19 Meyer NJ, Lyon RM. Lateral ecchymosis as a clinical sign of lateral condylar fractures. Am J Orthop. 2003;32:260-261.
20 Finnbogason T, Karlsson G, Lindberg L, et al. Nondisplaced and minimally displaced fractures of the lateral humeral condyle in children: a prospective radiographic investigation of fracture stability. J Pediatr Orthop. 1995;15:422-425.
21 Song KS, Kang CH, Min BW, et al. Internal oblique radiographs for diagnosis of nondisplaced and minimally displaced lateral condylar fractures of the humerus in children. J Bone Joint Surg Am. 2007;89:58-63.
22 Yates C, Sullivan JA. Arthrographic diagnosis of elbow injuries in children. J Pediatr Orthop. 1987;7:54-60.
23 Chapman VM, Grottkau BE, Albright M, et al. Multidetector computer tomography of pediatric lateral condylar fractures. J Comput Assist Tomogr. 2005;29:842-846.
24 Kamegaya M, Shinohara Y, Kurokawa M, et al. Assessment of stability in children’s minimally displaced lateral humeral condylar fractures by magnetic resonance imaging. J Pediatr Orthop. 1999;19:570-572.
25 Davidson RS, Markowitz RI, Dormans J, et al. Ultrasonographic evaluation of the elbow in infants and young children after suspected trauma. J Bone Joint Surg Am. 1994;76:1804-1813.
26 de Jager LT, Hoffman EB. Fractures of the lateral condyle in children. Presented at the South African Orthopaedic Congress 1988, Bloemfontein.
27 Speed JS, Macey HB. Fracture of the humeral condyles in children. J Bone Joint Surg. 1933;15:903-919.
28 Beaty JH, Kassar JR. The elbow: physeal fractures, apophyseal injuries of the distal humerus, osteonecrosis of the trochlear and T-condylar fractures. In: Beaty JH, Kassar JR, editors. Rockwood and Wilkins fractures in children. 6th edn. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:592-659.
29 Mintzer CM, Water OM, Brown DJ. Percutaneous pinning in the treatment of displaced lateral condylar fractures. J Pediatr Orthop. 1994;14:462-465.
30 Mohan N, Hunter JB, Colton CL. The posterolateral approach to the distal humerus for open reduction and internal fixation of fractures of the humerus in children. J Bone Joint Surg Br. 2000;82:642-645.
31 Thomas DP, Howard AW, Cole WG, et al. Three weeks of Kirschner wire fixation for displaced lateral condylar fractures of the humerus in children. J Pediatr Orthop. 2001;21:565-569.
32 Sharma JC, Arora A, Mathur NC, et al. Lateral condylar fractures of the humerus in children: fixation with partially threaded 4.0-mm AO cancellous screw. J Trauma. 1995;39:1129-1133.
33 Bast SC, Hoffer MM, Aval S. Nonoperative treatment for minimally and nondisplaced lateral humeral condylar fractures in children. J Pediatr Orthop. 1998;18:448-450.
34 Ippolito E, Tudisco C, Frasetti P, et al. Fracture of the humeral condyles in children: 49 cases evaluated after 18–45 years. Acta Orthop Scand. 1996;67:173-178.
35 Abraham E, Powers T, Witt P, Ray D. Experimental hyperextension supracondylar fractures in monkeys. Clin Orthop. 1982;172:309-318.
36 Foster DE, Sullivan JA, Gross RH. Lateral humeral condylar fractures in children. J Pediatr Orthop. 1985;5:16-22.
37 Herring JA. Lateral condylar fracture of the elbow. J Pediatr Orthop. 1986;6:724-727.
38 Flynn JC, Richards JF. Non-union of minimally displaced fractures of the lateral condyle of the humerus in children. J Bone Joint Surg Am. 1971;53:1096-1101.
39 Dhillon KS, Sengupta S, Singh BJ. Delayed management of fractures of the lateral humeral condyle in children. Acta Orthop Scand. 1988;59:419-424.
40 Roye DPJr, Bini SA, Infosino A. Late surgical treatment of lateral condylar fractures in children. J Pediatr Orthop. 1991;11:195-199.
41 Shimada K, Masada K, Tada K, et al. Osteosynthesis for the treatment of non-union of the lateral humeral condyle in children. J Bone Joint Surg Am. 1997;79:234-240.
42 Yang WE, Shih CH, Lee ZL, et al. Anatomic reduction of old displaced condylar fractures of the humerus in children via a posterior approach with olecranon osteotomy. J Trauma. 2008;64:1281-1289.
43 Gay JR, Love JG. Diagnosis and treatment of tardy paralysis of the ulnar nerve. J Bone Joint Surg. 1947;29:1087-1097.
44 Papandrea R, Waters PM. Posttraumatic reconstruction of the elbow in the pediatric patient. Clin Orthop. 2000;370:115-126.
45 Tien UC, Chen JC, Fu YC, et al. Supracondylar dome osteotomy for cubitus valgus deformity associated with a lateral condylar non union in children: surgical technique. J Bone Joint Surg Am. 2006;88(Supp 1):191-201.
46 Haraldsson S. On osteochondrosis deformans juvenalis capituli humeri including investigation of intra osseous vasculature in distal humerus. Acta Orthop Scand. 1959;38:1-232.
47 Wadsworth TG. Premature epiphyseal fusion after injury of the capitellum. J Bone Joint Surg Br. 1964;46:46-49.
48 Wilson JN. Fracture of the external condyle of the humerus in children. Br J Surg. 1936;18:299-316.
49 Nwakama AC, Peterson HA, Shaughnessy WJ. Fishtail deformity following fracture of the distal humerus in children: historical review, case presentations, discussion of etiology and thoughts on treatment. J Pediatr Orthop B. 2000;9:309-318.
50 Papavasiliou V, Nenopoulos S, Venturis T. Fractures of the medial condyle in childhood. J Pediatr Orthop. 1987;7:421-423.
51 Bensahel H, Cuskonyi Z, Badelon O, et al. Fractures of the medial humerus in children. J Pediatr Orthop. 1986;6:430-433.
52 De Boeck H, Cateleyn PP, Opdecam P. Fracture of the medial humeral condyle. J Bone Joint Surg Am. 1987;69:1442-1444.
53 Saraf SK, Tuli SM. Concomitant medial condyle fracture of the humerus in a childhood posterolateral dislocation of the elbow. J Orthop Trauma. 1989;3:352-354.
54 Wilkins KE. Fractures and dislocations of the elbow region. Part II. Fractures involving the medial condylar physis. In: Rockwood CAJr, King RE, editors. Fractures in children. 3rd edn. Philadelphia, PA: Lippincott; 1991:658-669.
55 Kilfoyle RM. Fractures of the medial condyle and epicondyle of the elbow in children. Clin Orthop. 1965;41:43-50.
56 Chacha PB. Fractures of the medial condyle of the humerus with rotational displacement: report of two cases. J Bone Joint Surg Am. 1970;52:1453-1458.
57 Potter CM. Fracture-dislocation of the trochlear. J Bone Joint Surg Br. 1954;36:250-253.
58 Harrison RB, Keats TE, Frankel CJ, et al. Radiographic clues to fractures of the unossified medial humeral condyle in young children. Skeletal Radiol. 1984;11:209-212.
59 El Ghawabi MH. Fracture of the medial condyle of the humerus. J Bone Joint Surg Am. 1975;57:677-680.
60 Fahey JJ, O’Brien E. Fracture-separation of the medial humeral condyle in a child confused with fracture of the medial epicondyle. J Bone Joint Surg Am. 1971;53:1102-1104.
61 Cothay DM. Injury to the lower medial epiphysis of the humerus before development of the ossific center: report of a case. J Bone Joint Surg Br. 1967;49:766-767.
62 Leet AI, Young C, Hoffer MM. Medial condyle fractures of the humerus in children. J Pediatr Orthop. 2002;22:2-7.
63 Papavasiliou VA, Beslikas TA. T-condylar fractures of the distal humeral condyles in childhood: an analysis of six cases. J Pediatr Orthop. 1986;6:300-303.
64 Toniolo RM, Wilkins KE. Fractures and dislocations of the elbow region. Part VI. T-condylar fractures. In: Rockwood CAJr, Wilkins KE, Beaty JH, editors. Fractures in children. 4th edn. Philadelphia, PA: Lippincott Raven; 1996:830-844.
65 Beghin JL, Bucholz RW, Wenger DR. Intercondylar fractures of the humerus in young children. J Bone Joint Surg Am. 1982;64:1083-1086.
66 Jarvis JG, D’Astous JL. The pediatric T supracondylar fracture. J Pediatr Orthop. 1984;4:687-699.
67 Kasser JR, Richards K, Millis M. The triceps dividing approach to open reduction of complex distal humerus fractures in adolescents: a cybex evaluation of triceps function and motion. J Pediatr Orthop. 1990;10:93-96.
68 Kanellopoulos AD, Yiannakopoulos CK. Closed reduction and percutaneous stabilization of pediatric T-condylar fractures of the humerus. J Pediatr Orthop. 2004;24:13-16.
69 Re PR, Waters PM, Hresko TY. T-condylar fractures of the distal humerus in children and adolescents. J Paediatr Orthop. 1999;19:313-318.
70 Bryan RS, Morrey BF. Extensive posterior exposure of the elbow: a triceps sparing approach. Clin Orthop. 1982;166:188-192.
71 Rasool MN. Ulna nerve injury after K-wire fixation of supracondylar humerus fractures in children. J Pediatr Orthop. 1998;18:686-690.
72 Akbarnia BA, Silberstein MJ, Rende RJ, et al. Arthrography in the diagnosis of fractures of the distal end of the humerus in infants. J Bone Joint Surg Am. 1986;68:599-602.
73 Holda ME, Manoli A, LaMont RL. Epiphyseal separation of the distal end of the humerus with medial displacement. J Bone Joint Surg Am. 1980;62:52-57.
74 Mizuno K, Hirohata K, Kashiwagi D. Fracture-separation of the distal humeral epiphysis in young children. J Bone Joint Surg Am. 1979;61:570-573.
75 Abe M, Ishizu T, Nagaoka T, et al. Epiphyseal separation of the distal end of the humeral epiphysis: a follow-up note. J Pediatr Orthop. 1995;15:426-434.
76 Bright RW. Epiphyseal-plate cartilage: a biomechanical and histological analysis of failure modes. J Bone Joint Surg Am. 1974;56:688-703.
77 Siffert RS. Displacement of distal humeral epiphysis in newborn infant. J Bone Joint Surg Am. 1963;45:165-169.
78 Dias JJ, Lamont AC, Jones JM. Ultrasonic diagnosis of neonatal separation of the distal humeral epiphysis. J Bone Joint Surg Br. 1988;70:825-828.
79 Barrett WP, Almquist EA, Staheli LT. Fracture separation of the distal humeral physis in the newborn. J Pediatr Orthop. 1984;4:617-619.
80 Hansen PE, Barnes DA, Tullos HS. Case report: arthrographic diagnosis of an injury pattern in the distal humerus of an infant. J Pediatr Orthop. 1982;2:569-572.
81 Mackerdhuj P, White CD, Hoffman EB. Differentiating between stage II lateral condylar fractures and entire distal humeral physeal injuries of the elbow in children. Presented at the South African Orthopaedic Congress, Cape Town; 2008.
82 Bede WB, Lefebure AR, Rosmon MA. Fractures of the medial humeral epicondyle in children. Can J Surg. 1975;18:137-142.
83 Silberstein JJ, Brodeur AE, Graviss ER, et al. Some vagaries of the medial epicondyle. J Bone Joint Surg Am. 1981;62:524-528.
84 Schwab GH, Bennett JB, Woods GW, et al. Biomechanics of elbow instability: the role of the medial collateral ligament. Clin Orthop. 1980;146:42-52.
85 Watson-Jones R. Primary nerve lesions in inquiries of the elbow and wrist. J Bone Joint Surg. 1930;12:121-140.
86 Ogawa K, Ui M. Fracture-separation of the medial humeral epicondyle caused by arm wrestling. J Trauma. 1996;41:494-497.
87 Fowles JV, Slimane N, Kassab MT. Elbow dislocation with avulsion of the medial humeral condyle. J Bone Joint Surg Br. 1990;72:102-104.
88 Patrick J. Fracture of the medial epicondyle with displacement into the elbow joint. J Bone Joint Surg. 1946;28:143-147.
89 Watson Jones R. Fractures of the elbow. 5th edn. Wilson JN, editor. Watson Jones fractures and joint injuries. vol. II. Edinburgh: Churchill Livingstone; 1976.
90 Woods GM, Tullos HB. Elbow stability and medial epicondyle fracture. Am J Sports Med. 1977;5:23-30.
91 Smith FM. Medial epicondyle injuries. J Am Med Assoc. 1950;142:396-402.
92 Fowles JV, Kassab MT, Moua T. Untreated intra-articular entrapment of the medial humeral epicondyle. J Bone Joint Surg Br. 1984;60:562-565.
93 Dias JJ, Johnson GV, Hoskinson J, et al. Management of severely displaced medial epicondyle fractures. J Orthop Trauma. 1987;1:59-62.
94 Roberts NW. Displacement of the internal epicondyle into the joint. Lancet. 1934;2:78-79.
95 Rosendahl B. Displacement of the medial epicondyle into the elbow joint: the final result in a case where the fragment had not been removed. Acta Orthop Scand. 1959;28:212-219.
96 McLeod GG, Gray AJ, Turner MD. Elbow dislocation with intra-articular entrapment of the lateral epicondyle. J R Coll Surg Edinb. 1993;38:112-113.
97 Silberstein JJ, Brodeur AE, Graviss ER. Some vagaries of the lateral epicondyle. J Bone Joint Surg Am. 1982;64:444-448.
98 Hasner E, Husby J. Fracture of the epicondyle and condyle of the humerus. Acta Chir Scand. 1951;101:195-205.