Chapter 27 Computer-Assisted Navigation for Anterior Cruciate Ligament Reconstruction
Computer-assisted navigation for anterior cruciate ligament (ACL) reconstruction can increase precision in tunnel placement and also provide valuable outcome information such as rotational stability.1–8 This is accomplished by registering anatomical landmarks and tracking the location of instruments and the tibia and femur in three-dimensional (3D) space on what is essentially a 3D map in the computer. Values such as the location of instruments and measures of impingement and isometry, as well as the location of the femoral and tibial tunnels, are calculated and shown to the operating surgeon in real time. Computer-assisted navigation has been demonstrated to improve accuracy and decrease laxity of the ACL reconstructed joint.5
Rationale
Computer assistance for precision navigation has been increasingly common in everyday applications such as the global positioning system (GPS) for drivers and sailors and has spread into surgical applications such as total knee replacement, pedicle screw placement, stereotactic brain surgery, and otolaryngology. In orthopaedic surgery, computer-assisted navigation has repeatedly been demonstrated to improve accuracy of total knee replacement components, not only in reducing outliers but also in correcting consistent repeated errors made by experienced surgeons.9,10 Similarly, improved accuracy in the placement of total hip components has also been demonstrated.11 Clinical outcomes have been shown to be comparable between navigated and nonnavigated groups.2,5
Need for Precision in Tunnel Placement
Clinical outcomes in ACL reconstructed patients are significantly related to accurate tunnel placement. Although there may not be a clear consensus on where tunnels should be placed, ample evidence exists that certain tunnel positions will result in mechanical problems with the graft and/or produce inappropriate kinematics. Multiple authors have indicated that incorrect tunnel placement can result in pain, laxity, synovitis, loss of range of motion, graft impingement, and graft failure.12–23 In longer-term follow-up, errors in tunnel placement result in an increased risk of arthritis.18 Although shorter-term studies may not demonstrate substantial differences, there remains a significant risk of arthritis following ACL reconstruction, and this is likely to related in part to tunnel placement.
Current Accuracy without Navigation
Clinically, accuracy of ACL reconstruction techniques can be assessed by the number of revision ACL reconstructions performed each year. Recent reports suggest that approximately 10% to 20% of all cases are revised.24,25 The vast majority of the failures are related to technical errors, specifically tunnel placement.24–26 The most common error is excessive anterior femoral tunnel placement, which can decrease rotational stability and may result in a graft that is lax in extension and tight in flexion.22,24 Among experienced surgeons, it has been noted that the tibial tunnel can be placed too far posterior in order to avoid notch impingement.2–4 This can result in posterior cruciate ligament (PCL) impingement with the knee in flexion and subsequent loss of knee flexion or strain on the graft. In addition, the graft will tend to be more vertically oriented and contribute less rotational stability.24
Several studies have been performed under various conditions to assess the accuracy of ACL tunnel placement. The Pittsburgh group evaluated tunnel placement by two experienced ACL surgeons in 20 foam knee models using standard arthroscopic guides. Actual tibial tunnel placement was a mean of 4.9 mm from the ideal tunnel site. Actual femoral tunnel placement was a mean of 4.2 mm from the ideal tunnel site. These differences were believed to be significant.6
Another study from the same group demonstrated the variability of tunnel placement by surgeons with 100 to 3500 cases of experience. Two fellows and two experienced surgeons each drilled 10 tunnels in foam knees. Tibial placement by experienced surgeon 1 varied by 2 mm; experienced surgeon 2, 3.4 mm; fellow 1, 2.1 mm; and fellow 2, 2.4 mm. On the femoral side, variability was less for experienced surgeons: experienced surgeon 1, 2.3 mm; experienced surgeon 2, 3.0 mm; fellow 1, 4.5 mm; and fellow 2, 4.1 mm. Clearly, substantial variability was observed.27
Surgeon accuracy in tunnel placement has also been evaluated in cadavers.28 In an advanced arthroscopy course, instructors placed tunnels in 24 specimens. The tunnel placement was then evaluated. Fifty percent (12/24) of the femoral tunnels and 25% (6/24) of the tibial tunnels were “unacceptable.” Similar results have been anecdotally noted by instructors at other training courses.
Evaluation of tunnel placement in vivo has also been performed in several centers. Harner recently reported on a series of 30 patients in which the tibial guide pin placement was evaluated by the use of intraoperative fluoroscopy.29 Tibial pins were placed using standard arthroscopic landmarks: namely, 7 mm anterior to the PCL, the medial tibial eminence, the anterior horn of the lateral meniscus, and the center of the visualized ACL tibial footprint. After reviewing the pin placement, Harner believed that it was necessary to reposition the pin 43% of the time. Typically, the tendency was for the experienced ACL surgeon to place the tibial tunnel too posterior (13/14 cases). In addition, repositioning of the pin was as frequent in the last 10 cases (5/10) as in the first 10 cases (5/10).
Similar results were found for a series of 24 patients in which tunnel position was evaluated postoperatively by radiographs.30 Two experienced ACL surgeons performed ACL reconstructions and recorded their perceptions of femoral and tibial tunnel placement. These were then correlated with actual tunnel placement by a blinded observer. The femoral tunnel demonstrated excellent (perfect) correlation coefficient (R2 = 1) on the anteroposterior (AP) radiograph (medial-lateral placement) between perceived and actual position. Good correlation (R2 = 0.55) was found for the lateral radiograph (AP position). However, the ability of the surgeons to describe medial-lateral tibial tunnel position was poor (R2 = 0.14), and the true AP position of the tibial tunnel had no correlation (R2 = 0.07, P = 0.36) to the surgeons’ perception. The authors concluded that four tunnels (12.5%) “were in very different positions than that expected by the surgeon.”
Other authors have noted that radiographic analysis of tunnel placement demonstrated too-posterior placement of the tibial tunnel and a relatively vertically oriented (the 11- or 1-o’clock position) femoral tunnel using standard arthroscopic instrumentation.2,4
Techniques of Computer-Assisted Navigation
Essential elements of computer-assisted navigation for ACL reconstruction include the ability to register and accurately track the relative positions of the tibia and femur as well as the intraarticular landmarks that guide correct tunnel placement. This can be accomplished by several methods, but most current solutions involve markers on rigid bodies attached to the tibia and femur with pins or screws. These are tracked intraoperatively by use of a binocular infrared camera attached to a computer that can calculate the relative position of the femur and tibia to less than 1 mm and less than 1 degree of precision1 (Fig. 27-1). Some systems require the use of preoperative computed tomography (CT) scans or intraoperative fluoroscopy (Brainlab, Westchester, IL). Other systems are “image-free,” such as the Orthopilot (Aesculap, Center Valley, PA) and do not require the use of preoperative or intraoperative radiographic imaging.
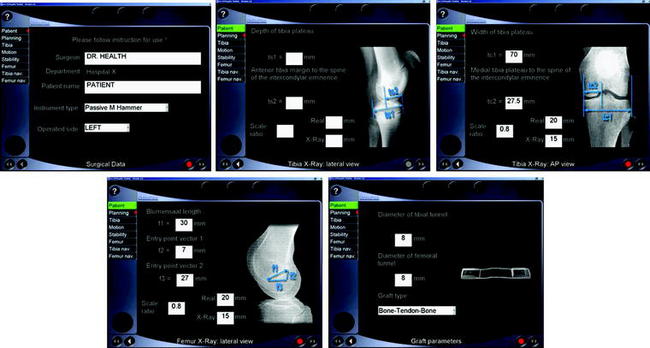
The navigation camera and display screen are set up opposite to the operative side of the patient, positioned opposite the knee and next to the arthroscopy tower or screen (Fig. 27-2). The initial data screens are filled in with the basic demographic data such as the name of the patient and physician (Fig. 27-3). This is followed by the optional input of preoperative radiographic information if desired by the surgeon. Clinically in the author’s practice, this has not been found to be necessary to obtain accurate and precise results. This part of the setup may be completed by ancillary personnel prior to the initiation of the case.
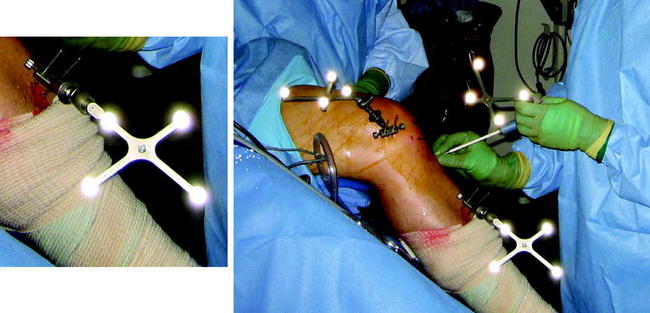
The trackers for ACL reconstruction are then attached by either two Kirschner wires (K wires) (Fig. 27-4) or a screw to the tibia and femur. The Orthopilot system uses trackers that can be attached by K wire fixation to bone, unlike other systems that use a significantly larger screw, which could be a potential stress riser. The K wires are placed percutaneously through small stab incisions on the anterior tibia and medial epicondyle of the femur. This minimizes morbidity associated with the placement of the trackers. We do not recommend the placement of the femoral tracker through the quadriceps mechanism because this can cause pain and potentially quadriceps weakening.
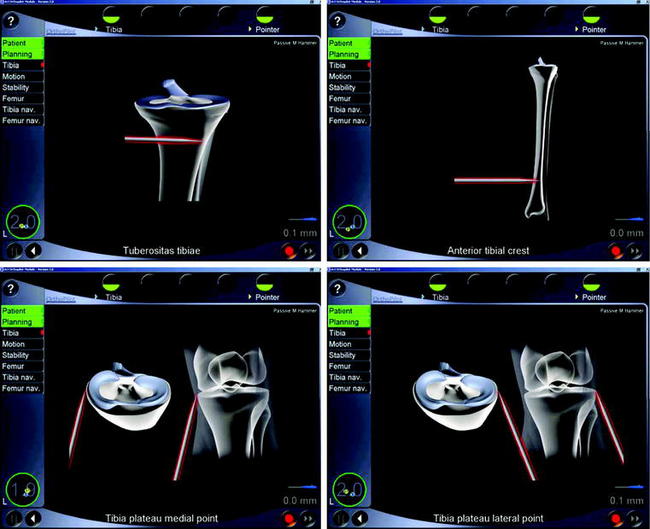
Following attachment of the trackers to the femur and tibia, tibial extraarticular landmarks are registered, including the tibial tubercle, the anterior tibial crest, and the medial and lateral borders of the tibia (Fig. 27-5). This is performed by palpating the identified landmarks using a pointer with attached reflective markers and clicking a foot pedal that serves as a mouse button. This step is followed by kinematic evaluation of knee motion by recording the relative positions of the femur and tibia in full extension and flexion. Acquisition of landmarks and kinematic testing takes approximately 90 seconds.
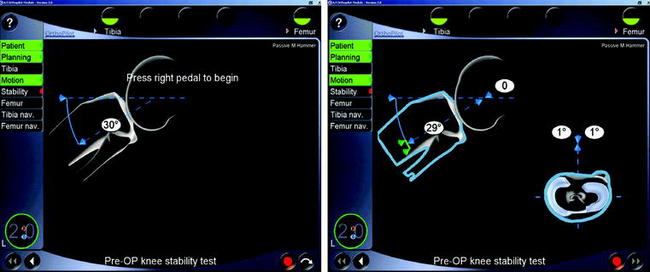
The relative motion of the femur and tibia is then assessed by the surgeon in a chosen degree of flexion, usually 30 degrees. Absolute anterior and posterior translation in millimeters is recorded. In addition, the arc of internal and external rotation is recorded (Fig. 27-6). This is a measurement that cannot be accurately obtained without this system. The values are then written to a permanent file. Of note, any screen can be recorded to the computer memory at any step in the program.
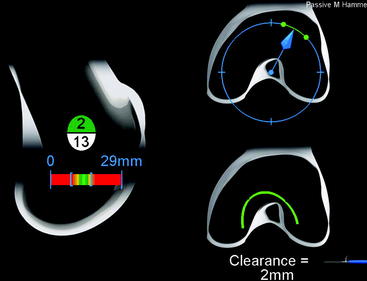
At this point, the arthroscope is introduced into the knee, and the usual tibial intraarticular landmarks are identified and palpated with the pointer, similar to palpation with a probe. These include the PCL, the anterior horn of the lateral meniscus, and the medial tibial spine. Following this, the anterior margin of the intercondylar notch, the femoral ACL origin, and the posterior edge of the intercondylar notch are palpated. Of note, one of the most valuable pieces of information is a real-time measurement of the intercondylar notch length (Blumensaat’s line; Fig. 27-7). The average length is 30 mm; a measurement of 25 to 26 mm suggests that the true over-the-top position has not been reached and the proposed position is not correct. At our institution, this has been particularly useful in providing additional feedback for residents in training.
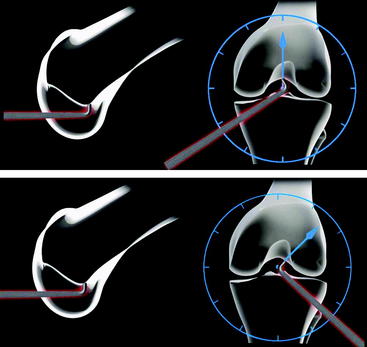
Fig. 27-7 Notch length. This is an excellent check of whether the true over-the-top position has been reached.
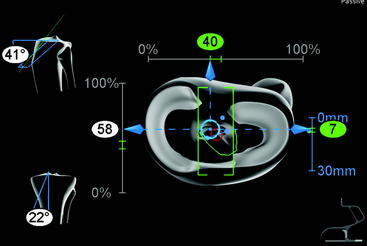
Following the acquisition of intraarticular landmarks, the tibial guide is placed as usual into the knee and placed in the proposed location for the tibial tunnel. The guide has reflective markers attached, permitting the precise identification of the location of the tibial guide pin with respect to the PCL, the intracondylar notch, and other intraarticular and extraarticular landmarks (Fig. 27-8). This allows the surgeon to choose the appropriate coronal and sagittal angles and distance from the PCL, as well as toavoid impingement on the roof or wall of the intercondylar notch.
Following selection and recording of the tibial tunnel, the proposed femoral tunnel location is evaluated by placing the pointer tip at the location of the femoral guide pin (Fig. 27-9). This tells the surgeon where the location of the proposed tunnel site is from the posterior femoral cortex and the location on the “clock face” (i.e., the position of the graft laterally). In addition, information is provided on the amount of isometry of the graft and where and by how many millimeters the graft will impinge on the intercondylar notch.
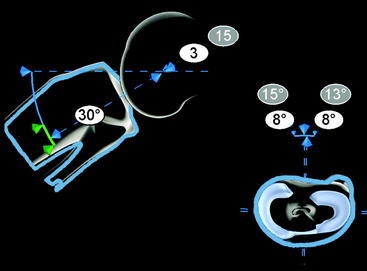
Finally, after securing the graft, the final measurements of AP translation and internal and external rotation are obtained (Fig. 27-10).
Results
The results of computer-assisted navigation for ACL reconstruction have demonstrated consistent improvements in tunnel placement and clinically measured laxity. The improvements have been observed in both relatively inexperienced surgeons and surgeons who have conducted multiple ACL reconstructions. In the laboratory setting, DiGioa demonstrated improved accuracy in tunnel placement in foam knees when compared with standard manual instrumentation. This was shown first with experienced surgeons and then with novices.6
Koh reported that navigation improved the accuracy of tibial tunnel placement.2 Forty-two navigated knees demonstrated a more anatomical, slightly more anterior tibial tunnel without impingement compared with nonnavigated knees. The variability of tunnel placement was extremely low in both the navigated and nonnavigated knee groups. After an initial learning curve, minimal extra time was needed for the navigated knees.
Eichorn reported substantially better accuracy both for inexperienced surgeons (fellows)3 and for his own4 tunnel placement. Inexperienced surgeons demonstrated extremely low variability and accurate femoral and tibial tunnel placement using navigation.3 Navigated ACL reconstructions performed by a very experienced surgeon demonstrated improved tunnel placement on the lateral wall (the 10-o’clock versus the 10:30 position) and a more accurate anterior placement of the tibial tunnel (more anterior without impingement).4
A French group recently published results of navigated ACL reconstructions in patients randomized to either navigated or nonnavigated knees.5 Twenty-two nonnavigated and 26 navigated knees were compared. Nineteen of the 22 nonnavigated knees had a portion of the tibial tunnel placed anterior to the roof of the notch versus none of the navigated knees. The variability of laxity was substantially less, and less than 2 mm of laxity was seen in 96.7% of navigated knees versus 83% of nonnavigated knees. The initial additional time for use of the system was 25 minutes but with experience decreased to less than 10 minutes.
Discussion
ACL reconstructions performed with computer-assisted navigation have demonstrated improved accuracy in tunnel placement and improved measurements of clinically assessed laxity in patients when compared with nonnavigated knees.1–6 Following an initial learning curve of a few cases, the additional time required for this increased precision is minimal. At this time, a moderate cost is associated with the initial acquisition of the machine; however, most of the navigation systems can be used for other procedures such as joint replacement. In addition, the high cost of revision surgery may be avoided if tunnel position is more accurate. The benefits of navigation have been demonstrated both for relatively less experienced and more experienced surgeons. Less experienced surgeons typically will have less variable results in addition to improved accuracy with navigation.3 More experienced surgeons, who are often quite consistent in tunnel placement, will typically shift tunnel placement to a more anatomical position.2,4,5
1 Koh JL. Computer-assisted navigation and anterior cruciate ligament reconstruction: accuracy and outcomes. Orthopaedics. 2005;10:s1283-s1287.
2 Koh JL, Koo S. Leonard J, Kodali P. ACL tunnel placement: A radiographic comparison between navigated versus manual ACL reconstruction. Orthopedics. 2006;10:S122-S124.
3 Eichhorn J. Three years of experience with computer navigation-assisted positioning of drilling tunnels in anterior cruciate ligament replacement (SS-67). Arthroscopy. 2004;20:31-32.
4 Eichhorn J. Three years of experience with computer-assisted navigation in anterior cruciate ligament replacement. http://www.aclstudygroup.com/Powerpoint-pdf02/Eichhorn.pdf.
5 Plaweski S, Cazal J, Rosell P, Merloz P. Anterior cruciate ligament reconstruction using navigation: A comparative study on 60 patients. Am J Sports Med. 2006;94:542-552.
6 Picard F, DiGioia AM, Moody J, et al. Accuracy in tunnel placement for ACL reconstruction. Comp Aid Surg. 2001;6:279-289.
7 Klos TV, Habets RJ, Banks AZ, et al. Computer assistance in arthroscopic anterior cruciate ligament reconstruction. Clin Orthop. 1998;354:65-69.
8 Degenhart M. Computer-navigated ACL reconstruction with the OrthoPilot. Surg Technol Int. 2004;12:245-251.
9 Stulberg SD, Loan P, Sarin V. Computer-assisted navigation in total knee replacement: Results of an initial experience in thirty-five patients. J Bone Joint Surg Am. 2002;84:S90-S98.
10 Berry DJ. Computer-assisted knee arthroplasty is better than a conventional jig-based technique in terms of component alignment. J Bone Joint Surg Am. 2004;86:2573.
11 Parratte S, Argenson JNA. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty. A prospective, randomized, controlled study. J Bone Joint Surg Am. 2007;89:494-499.
12 Aglietti P, Buzzi R, Giron F, et al. Arthroscopic-assisted anterior cruciate ligament reconstruction with the central third patellar tendon. A 5–8-year follow-up. Knee Surg Sports Traumatol Arthrosc. 1997;5:138-144.
13 Howell SM, Clark JA, Farley TE. Serial magnetic resonance study assessing the effects of impingement on the MR image of the patellar tendon graft. Arthroscopy. 1992;8:350-358.
14 Howell SM, Clark J. Tibial tunnel placement in anterior cruciate ligament reconstructions and graft impingement. Clin Orthop. 1992;283:187-195.
15 Howell SM, Taylor MA. Failure of reconstruction of the anterior cruciate ligament due to impingement by the intercondylar roof. J Bone Joint Surg. 1993;75A:1044-1055.
16 Howell SM, Wallace MP, Hull ML, Deutsch ML. Evaluation of the single-incision arthroscopic technique for anterior cruciate ligament replacement. A study of tibial tunnel placement, intraoperative graft tension, and stability. Am J Sports Med. 1999;27:284-293.
17 Ikeda H, Muneta T, Niga S, et al. The long-term effects of tibial drill hole position on the outcome of anterior cruciate ligament reconstruction. Arthroscopy. 1999;15:287-291.
18 Jarvela T, Paakkala T, Jarvela K, et al. Graft placement after the anterior cruciate ligament reconstruction: A new method to evaluate the femoral and tibial placements of the graft. Knee. 2001;8:219-227.
19 Khalfayan EE, Sharkey PF, Alexander AH, Bruckner JD, Bynum EB. The relationship between tunnel placement and clinical results after anterior cruciate ligament reconstruction. Am J Sports Med. 1996;3:335-341.
20 Romano VM, Graf BK, Keene JS, Lange RH. Anterior cruciate ligament reconstruction. The effect of tibial tunnel placement on range of motion. Am J Sports Med. 1993;3:415-418.
21 Muneta T, Yamamoto H, Ishibashi T, et al. The effects of tibial tunnel placement and roofplasty on reconstructed anterior cruciate ligament knees. Arthroscopy. 1995;1:57-62.
22 Sommer C, Friederich NF, Muller W. Improperly placed anterior cruciate ligament grafts: correlation between radiological parameters and clinical results. Knee Surg Sports Traumatol Arthrosc. 2000;8:207-213.
23 Yaru NC, Daniel DM, Penner D. The effect of tibial attachment site on graft impingement in an anterior cruciate ligament reconstruction. Am J Sports Med. 1992;2:217-220.
24 Allen CA, Giffin JR, Harner CD. Revision anterior cruciate ligament reconstruction. Orthop Clin N Am. 2003;34:79-98.
25 AOSSM institutes multi-center revision ACL study. Matava MJ, Boden BP, editors. AOSSM Sports Medicine Update. 2005;5. March-April
26 Getelman MH, Friedman MJ. Revision anterior cruciate ligament surgery. J Am Acad Orthop Surg. 1999;7:189-198.
27 Burkart A, Debski RE, McMahon PJ, et al. Precision of ACL tunnel placement using traditional and robotic techniques. Comput Aided Surg. 2001;6:270-278.
28 Kohn D, Beusche T, Caris J. Drill hole position in endoscopic anterior cruciate ligament reconstruction. Results on an advanced arthroscopy course. Knee Surg Sports Traumatol Arthrosc. 1998;6:S13-S15.
29 Cha PS, West RV, Harner CD. The results of using intraoperative fluoroscopy for ideal tibial tunnel position during anterior cruciate ligament reconstruction. 11th ESSKA Congress. May 8, 2004.
30 Sudhahar TA, Glasgow MM, Donell ST. Comparison of expected vs. actual tunnel position in anterior cruciate ligament reconstruction. Knee. 2004;11:15-18.