Chapter 152 Complex Lumbosacropelvic Fixation Techniques
Anatomic and Biomechanical Considerations
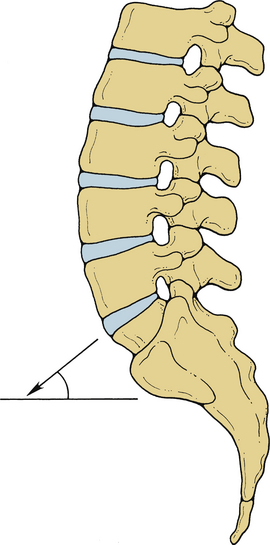
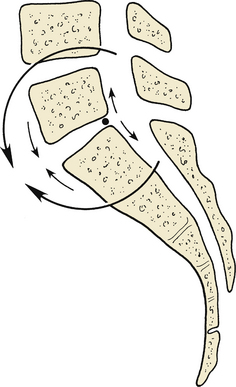
The LSJ is a unique spinal level in several respects.1 In the sagittal or flexion-extension axis, it has the largest range of motion of any thoracic or lumbar level, averaging 17 degrees of total movement. In the axial plane and during rotation and lateral (coronal plane) bending, the LSJ has the most limited range of motion of any spinal level, averaging 1 degree of rotation and 3 degrees of bending, respectively.2 Because of the normal lordotic curvature of the lumbar spine, the slope of the lumbosacral intervertebral disc (L5-S1) is usually the steepest of any disc, with respect to the true horizontal. The summation of spinal load vectors results in exposure of the lumbosacral disc to the largest loads encountered throughout the spine. The large loads carried and the angular position of the disc at the LSJ produce unique load-bearing characteristics, including the highest level of translational shear force in the entire spine (Fig. 152-1).1,3,4
Sacrum
The sacrum is formed from five fused vertebrae in which the specially adapted and large transverse processes merge into thick lateral masses, the alae. The sacral spinal canal has four pairs of dorsal and ventral foramina. The subdural and subarachnoid spaces terminate as the thecal sac tapers at the caudal margin of S2. The filum terminale internum is an extension of the pia arachnoid of the conus medullaris, extending from the tip of the conus to the end of the subdural space. At the termination of the subdural space, the thecal sac tapers to invest the filum terminale internum and form the filum terminale externum. The filum terminale externum extends to the end of the sacral canal and attaches to the rostral portion of the coccyx.
Sacroiliac Joint
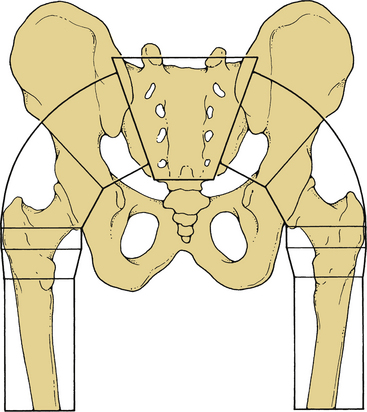
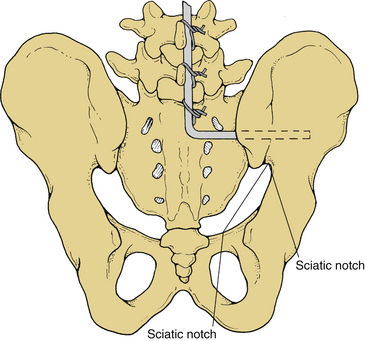
The SIJ is formed by the interdigitating surfaces of the sacral alae and the iliac bones. It is predominantly a fibrocartilaginous amphiarthrodial (no synovial capsule) joint. There is a small diarthrodial (synovial capsule present) portion located at the ventral aspect of the SIJ. The interdigitation and matching contours of the iliac and sacral alar surfaces create an interlocking mechanism to help stabilize the joint. The wedgelike shape of the sacrum helps stabilize the SIJ and serves to transfer loads from the spine to the pelvis (Fig. 152-2).
The SIJ is essentially an immobile joint that functions as a shock absorber for the spine. In studies on fresh cadavers, there was minimal motion in pediatric specimens, and none in adults.5 Another cadaveric study has demonstrated that in adults older than 50 years of age, autofusion of the joint is observed in 75% of specimens.6
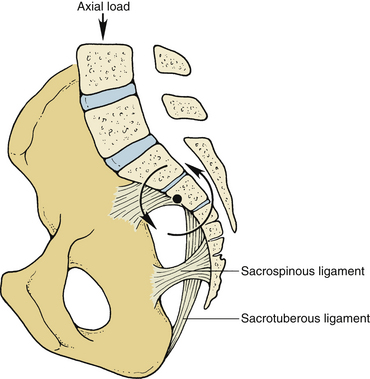
The major biomechanical function of the pelvis is that of transferring loads from the SIJ to the hip joints. The stable transfer of these loads is dependent on the ligaments connecting the lumbar vertebrae and the sacrum to the pelvis. The ligamentous structures spanning the SIJ include the interosseous, dorsal, and ventral sacroiliac ligaments (Fig. 152-3). The interosseous, sacroiliac, and dorsal sacroiliac complex provides the major stabilization for the SIJ.
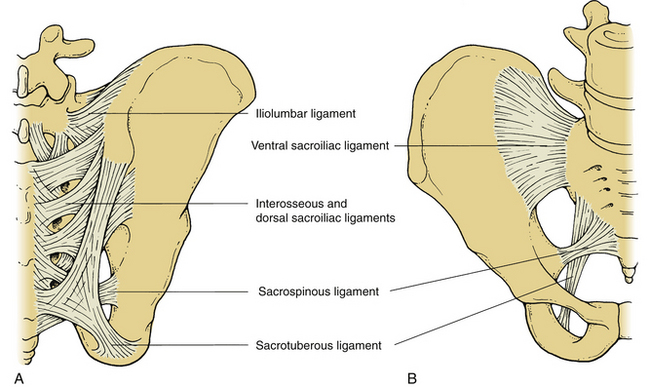
FIGURE 152-3 Dorsal (A) and ventral (B) views of the major ligamentous attachments of the sacroiliac joint.
The force vector of axial load from the spine is located ventral to the SIJ. This causes a ventral rotational tendency of the sacrum at the level of the SIJ. The center point of this rotational vector is located near the center of the S2 vertebral body (Fig. 152-4). The sacrospinous and sacrotuberous ligaments pass from the lower sacrum to the ischial bones. The position of these ligaments creates a long moment arm through which they are able to resist sacral rotation and are thereby able to maintain the lordotic lumbosacral posture despite the gravitational sagittal plane vector.
Muscular Interactions
In the resection of sacral tumors, stability of the sacropelvic region can be jeopardized because portions of the sacrum and possibly the SIJ are removed. Resection of the caudal portion of the sacrum up to the S1-2 interspace and removal of up to one third of the SIJ can be performed with only a 30% loss of weight-bearing capacity. The lower half of the S1 body and up to one half of the SIJ can be resected with a 50% loss of weight-bearing stability.7 Preservation of 50% of weight-bearing capacity is adequate for early ambulation in the postoperative period, and further stabilization is not likely to be necessary. In general, in cases of tumor or other destructive lesions of the sacral (e.g., infection), the bilateral alae should be evaluated. If one ala or more than 50% of bilateral alae are destroyed, the patient will require lumbopelvic fixation.
Indications for Lumbosacralpelvic Fixation
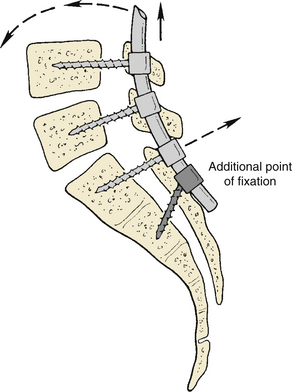
In short-segment cases and in the absence of osteopenia, sacral fixation with a single pair of bone screws is adequate. In longer-segment cases (e.g., scoliosis, postsacrectomy reconstruction, and multisegmental lumbosacral fusion) or with osteoporotic bone, more substantial segmental fixation is required to achieve rigidity. In addition, when high-grade lumbosacral spondylolistheses (grades III and above) are reduced, standard sacral screws may be inadequate and lead to loosening or sacral fracture. Rigidity is a crucial element in these constructs because fusion rates are directly related to use of rigid instrumentation, and better outcomes clearly correlate with the acquisition of a solid fusion.8–15 If a long instrumentation construct is placed, the sacral attachment is usually subjected to large cantilevered forces that may lead to screw pull-out (Fig. 152-5). Additional points of sacral or sacropelvic fixation may prevent complications in such cases.
The SIJ is autofused in many adults older than 50 years of age. Long-term follow-up study of patients with instrumentation constructs crossing the SIJ has demonstrated no adverse effects relating to the presence of the implants.16 Therefore, if it is necessary for additional security of fixation in the lumbosacropelvic region, placement of instrumentation across the SIJ is a rational approach for providing spinal stability.
Lumbosacral Pivot Point
In a study of the biomechanics of sacropelvic fixation, McCord et al. described the concept of the lumbosacral pivot point.17 This is the axis of rotation at the lumbosacral junction. During flexion, the portions of L5 and the sacrum that are ventral to this pivot move toward one another. Likewise, the portions of L5 and the sacrum located dorsal to this pivot point will move apart during flexion (Fig. 152-6). Anatomically, the lumbosacral pivot point is marked by the intersection of the middle osteoligamentous column and the lumbosacral (L5-S1) disc. In constructs that cross the SIJ, only those devices that pass ventral to this point provide a significant biomechanical advantage regarding rigidity of fixation.
Complex Techniques of Sacral Fixation
Many lumbosacral fusions can be adequately immobilized with placement of bone screws into the sacral pedicles. These screws, however, obtain their thread purchase in the broad cancellous channel of the sacral pedicle. Therefore, bone screws in the sacral pedicles are subject to failure because of the relative porosity of the sacrum, the manner in which stress tends to be concentrated at the termini of a fusion construct, and the large flexion moments to which these constructs are subjected.18,19 Sacral screws may fail by pull-out or by fracture.18 In cases in which it is believed that the use of a single pair of bone screws may not be adequate for stabilization, the use of more complex techniques is warranted.
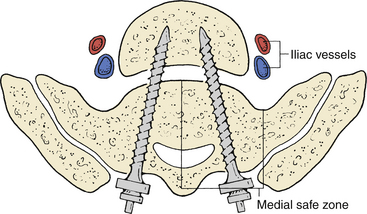
With regard to injuring structures ventral to the sacrum, cadaveric studies have shown that the widest margin of safety is found at the medial safe zone (Fig. 152-7).20 Therefore, placing the screws in a medial or toed-in direction is preferred at the S1 or promontory level. Some authors have advocated bicortical purchase of sacral screws to enhance pull-out resistance, which affords some pull-out strength advantage, although this involves additional risk.20–25 Zindrick et al. found that bicortical purchase with a 6.5-mm diameter screw resulted in an increase in pull-out strength of about 30%.25 Penetrating an excessive distance beyond the ventral cortex carries the risks of neurologic deficit, chronic pain from lumbosacral trunk injury, sympathetic chain injury, peritonitis, sepsis, and hemorrhage,20,24 although these risks are minimal if the screw penetrates 1 cm or less.
Fixation with Sublaminar Devices
The addition of sublaminar devices such as hooks, wires, or cables at the sacrum is a simple means of enhancing fixation. It should be borne in mind that the sacral laminae are often quite thin and may not provide substantial strength to hold such devices. All of these devices, including hooks, are tension-band fixators. Dorsally placed tension-band constructs provide limitation of flexion but do not provide substantial torsional stability or resistance to extension. With fusions at the LSJ, it has been shown that fixation with sublaminar devices alone does not improve the fusion rate when this rate is compared with that of noninstrumented fusions.26 Therefore, sublaminar devices should be used at the LSJ only in conjunction with other devices.
Although the bony thickness at the sacral lamina is meager, the bone stock is usually quite substantial at the nearby dorsal foramina. Thus, the dorsal foramina are excellent sites to place hooks for the purpose of enhancing construct strength. When added to a sacral pedicle screw construct, this technique has been shown to significantly increase rigidity.27
Fixation with Screws
A number of simple techniques use bone screws to enhance sacral fixation. Screws provide rigid three-dimensional stabilization and can be used for short-segment fixation at the LSJ. Shorter constructs provide a major advantage because immobilization of long segments of the spine increases the load, not only at the immediately adjacent segment but also at more distal segments.28
Directing screws medially (pedicular) or laterally (alar) and then rigidly attaching them to the rod or plate greatly enhances pull-out resistance. Studies are in conflict regarding which of these two methods is better, but both offer a substantial biomechanical advantage over a straight sagittal-plane trajectory.25,29 Oblique trajectories dramatically increase the cross-sectional area of bone that resists screw dislodgement via the cantilevered forces applied by the spine in flexion. If the longitudinal members are then linked with cross-members, a triangulation effect is created. This enhances both the rigidity of the construct and its pull-out resistance.25,30,31 Torsional stability is particularly enhanced by cross-fixation of the rods.30,32,33
Perhaps the easiest method for enhancing sacral fixation with screws is the placement of an additional pair of laterally directed bone screws into the sacral alae below the S1 level. This method provides a biomechanical advantage over a single pair of pedicle screws.13,17 These screws are easily added to a construct without the need for preplanning or special devices, and fluoroscopy is not required. For this method, a type of screw whose attachment site to the rod is somewhat narrow is optimal. Screws with a broad attachment site may be difficult to place sufficiently close together for the optimal trajectory of the screws to be attained (Fig. 152-8).
The placement of screws into the S2 and even the S3 levels has been advocated to enhance the security of sacral fixation. Biomechanical testing has demonstrated that these screw placement sites do not add sufficiently to the security of fixation to warrant their use.17,25 The thickness of the sacrum in the sagittal plane diminishes at the lower sacral levels. Therefore, inadvertent penetration of the ventral surface of the sacrum with such screws is more likely, and injury to the anatomic structures immediately adjacent to the ventral cortical surface may occur. However, such S2 alar screws can be used as more substantial anchor points if they are used as S2 sacroiliac screws, in which the screw transverses the SIJ and functions as an iliac screw in terms of longer length and iliac purchase.
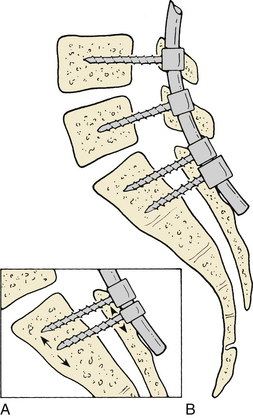
The pedicular transvertebral screw fixation technique has been described for treatment of lumbosacral spondylolisthesis.34 This technique involves placement of a long screw through the pedicle of S1, passing through the rostral end plate of S1 and into the caudal end plate of the L5 vertebral body. When combined with screws in the L4 pedicles, this provides a unique biomechanical construct. It appears to be a simple method for stabilizing high-grade spondylolisthesis. The simplicity of this technique is attractive, and the clinical results appear to be encouraging (Fig. 152-9).
Along with placement of screws spanning from vertebra to sacrum, fibular bone struts can be applied in a similar manner. Placement of fibular grafts to act as dowels can be performed from a dorsal or ventral approach.35–39
The procedure has been reported in use with autografts, allografts, and even with vascularized autografts.36,37,40,41 Transvertebral fibular dowels should always be augmented with screw fixation.
Along with screw placement, sacral fixation can be supplemented by insertion of the rods directly into the lateral sacral bony masses. Jackson has described a method whereby screws are directed through the S1 pedicle, and cortical purchase is obtained in the vertebral end plate of S1 as well. The rods are then passed into the lateral sacrum toward the SIJ and affixed rigidly to the screws.
Devices for Sacral Fixation with Multiple Screws
A number of devices especially designed for sacral and sacropelvic fixation have been marketed. The two basic types are those that cross the SIJ and those that affix directly to the sacrum only. The sacral fixation devices are generally platelike structures that are secured to the sacrum with screws. Asher and Strippgen described one early example of these.42 It is called the Isola plate because of its butterfly shape (and is named after a species of Rocky Mountain butterfly). This design contained holes for the passage of multiple sacral screws. The position of the holes dictated placement of the screws, and anthropometric sacral measurements taken in male and female cadavers served as the basis for spacing of the holes.
Fixation across the Sacroiliac Joint
The most commonly used method for sacropelvic attachment is the Galveston technique or a variation of it. The procedure was originally described by Allen and Ferguson for the treatment of scoliosis.43,44 It is accomplished by inserting angled rods into the iliac bones and passing them into the hard cortical bone above the sciatic notch (Fig. 152-10). This technique is useful for providing extremely rigid fixation in difficult cases, such as reconstruction after tumor resection or patients with lumbosacral agenesis.45
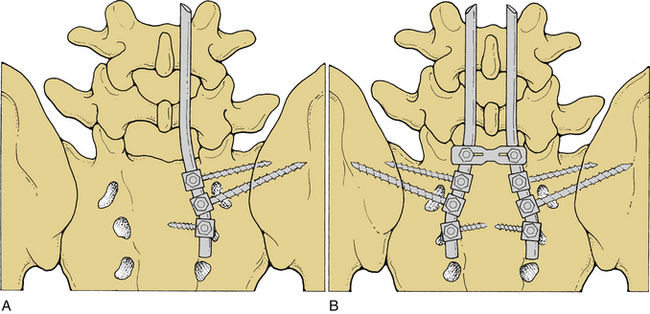
Placing Galveston rods into the ilium can be cumbersome and technically difficult. Therefore, specialized screws for iliac insertion have been developed (Isola iliac screws, DePuy AcroMed, Raynham, MA). Iliac screws are placed by using fluoroscopy, and the rods are then either directly attached or joined to the screw by a connector fitting. These devices markedly enhance the rigidity of lumbosacral instrumentation constructs. The increases in rigidity are similar for both the iliac screws and the Galveston rods.17 Multiple studies have confirmed that iliac fixation provides the most effective means to supplement sacral screws.46,47
Bicortical Iliac Screw Fixation
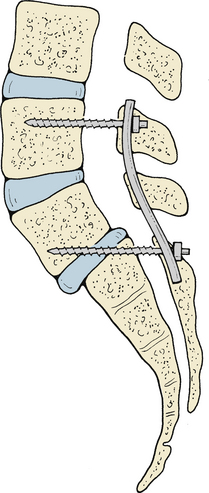
A simple method of sacropelvic fixation is the placement of long, variable-angle bone screws obliquely through the iliac bones (Fig. 152-11). When combined with additional sites of fixation at the sacrum, this technique creates a tripod effect for load sharing. This method has not been studied for its biomechanical characteristics, but early clinical results appear satisfactory.48
Complications of Complex Lumbopelvic Fixation
The majority of complications associated with complex instrumentation constructs are similar to those of any other spine fixation procedures. Infection remains a common adverse sequela of these operations, occurring in 3% to 5% of cases, even in experienced hands.49 Problems such as blood loss, neurologic deficits, and poor bone quality should be managed with the same measures as would be used in any other implant case.
Revision Surgery
Revision surgery of instrumentation constructs should address the reason for the failure. If there is a fractured implant, more fixation points should be included to improve load sharing. If screw pull-out is observed, the use of larger-diameter or longer screws provides greater thread purchase. If the pull-out appears to be largely due to poor bone quality, pressurized injection of polymethylmethacrylate may improve screw pull-out resistance.25
In cases of Galveston rod failure, additional fixation points can usually be secured. These rods tend to loosen by pull-out because they do not have purchase into the deep portion of the iliac bones. Further fixation should be attempted by placement of screws into the sacral pedicles or alae and attachment to the rod. Also, rigid cross-members should be added if these are not already present in the construct.
Postoperatively, patients who have undergone revision surgery should be placed in thoracolumbosacral orthoses. The addition of a hip extension device to these orthoses has traditionally been recommended. However, it has been shown that spinal motion is not reduced by the addition of this cumbersome and uncomfortable attachment.50
In a few cases, such stability has been accomplished by attaching ventral allograft bone struts to transpelvic plates at the lower end and to the remaining lumbar vertebrae above.51 Pelvic rim stabilization with transverse plates and stabilization with oblique allograft struts from the dorsal iliac wings to the telescoped lumbar vertebrae have also been attempted with some success.52 Graft positioning oblique to the primary ventral rotational force vector in the upright posture is the main clinical and theoretical impediment to the success of these techniques.
McCord D.H., Cunningham B.W., Shono Y., et al. Biomechanical analysis of lumbosacral fixation. Spine (Phila Pa 1976). 1992;17:S235-S243.
Pintar F.A., Maiman D.J., Yoganandan N., et al. Rotational stability of a spinal pedicle screw/rod system. J Spinal Disord. 1995;8:49-55.
Ruland C.M., McAfee P.C., Warden K.E., et al. Triangulation of pedicular instrumentation. A biomechanical analysis. Spine (Phila Pa 1976). 1991;16:S270-S276.
Tomita K., Tsuchiya H. Total sacrectomy and reconstruction for huge sacral tumors. Spine (Phila Pa 1976). 1990;15:1223-1227.
White A.A., Panjabi M.M. Clinical biomechanics of the spine. Philadelphia: Lippincott-Raven; 1990.
Zindrick M.R., Wiltse L.L., Widell E.H., et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;203:99-112.
1. Farfan H.F., Kirkaldy-Willis W.H. The present status of spinal fusion in the treatment of lumbar intervertebral joint disorders. Clin Orthop Relat Res. 1981;158:198-214.
2. White A.A., Panjabi M.M. Clinical biomechanics of the spine. Philadelphia: Lippincott-Raven; 1990.
3. Colombini D., Occhipinti E., Grieco A., et al. Estimation of lumbar disc areas by means of anthropometric parameters. Spine (Phila Pa 1976). 1989;14:51-55.
4. Dietrich M., Kurowski P. The importance of mechanical factors in the etiology of spondylolysis. A model analysis of loads and stresses in human lumbar spine. Spine (Phila Pa 1976). 1985;10:532-542.
5. White A.A., Panjabi M.M. Clinical instability of the spine. In: Evarts C.M., Burton R.I., Cofield R.H., et al, editors. Surgery of the musculoskeletal system. New York: Churchill Livingstone; 1990:2151-2173.
6. Brooke R. The sacroiliac joint. J Anat. 1924;58:297-301.
7. White A.A., Panjabi M.M. The problem of clinical instability in the human spine: a systematic approach. In: White A.A., Panjabi M.M., editors. Clinical biomechanics of the spine. Philadelphia: Lippincott-Raven; 1990:277-378.
8. Balderston R.A., Winter R.B., Moe J.H., et al. Fusion to the sacrum for nonparalytic scoliosis in the adult. Spine (Phila Pa 1976). 1986;11:824-829.
9. Hanley E.N.Jr., Levy J.A. Surgical treatment of isthmic lumbosacral spondylolisthesis. Analysis of variables influencing results. Spine (Phila Pa 1976). 1989;14:48-50.
10. Kim S.S., Denis F., Lonstein J.E., et al. Factors affecting fusion rate in adult spondylolisthesis. Spine (Phila Pa 1976). 1990;15:979-984.
11. Kornblatt M.D., Casey M.P., Jacobs R.R. Internal fixation in lumbosacral spine fusion. A biomechanical and clinical study. Clin Orthop Relat Res. 1986;203:141-150.
12. Lorenz M., Zindrick M., Schwaegler P., et al. A comparison of single-level fusions with and without hardware. Spine (Phila Pa 1976). 1991;16:S455-S458.
13. Louis R. Fusion of the lumbar and sacral spine by internal fixation with screw plates. Clin Orthop Relat Res. 1986;203:18-33.
14. Nagel D.A., Kramers P.C., Rahn B.A., et al. A paradigm of delayed union and nonunion in the lumbosacral joint. A study of motion and bone grafting of the lumbosacral spine in sheep. Spine (Phila Pa 1976). 1991;16:553-559.
15. Zdeblick T.A. A prospective randomized study of lumbar fusion: preliminary results. Spine (Phila Pa 1976). 1993;18:983-991.
16. Kostuik J.P., Errico T.J., Gleason T.F. Luque instrumentation in degenerative conditions of the lumbar spine. Spine (Phila Pa 1976). 1990;15:318-321.
17. McCord D.H., Cunningham B.W., Shono Y., et al. Biomechanical analysis of lumbosacral fixation. Spine (Phila Pa 1976). 1992;17:S235-S243.
18. Devlin V.J., Boachie-Adjei O., Bradford D.S., et al. Treatment of adult spinal deformity with fusion to the sacrum using CD instrumentation. J Spinal Disord. 1991;4:1-14.
19. Pashman R.S., Hu S.S., Schendel M.J., et al. Sacral screw loads in lumbosacral fixation for spinal deformity. Spine (Phila Pa 1976). 1993;18:2465-2470.
20. Mirkovic S., Abitbol J.J., Steinman J., et al. Anatomic consideration for sacral screw placement. Spine (Phila Pa 1976). 1991;16:S289-S294.
21. Camp J.F., Caudle R., Ashmun R.D., et al. Immediate complications of Cotrel-Dubousset instrumentation to the sacro-pelvis. A clinical and biomechanical study. Spine (Phila Pa 1976). 1990;15:932-941.
22. Esses S.I., Botsford D.J., Huler R.J., et al. Surgical anatomy of the sacrum. A guide for rational screw fixation. Spine (Phila Pa 1976). 1991;16:S283-S288.
23. Krag M.H., Van Hal M.E., Beynnon B.D. Placement of transpedicular vertebral screws close to anterior vertebral cortex. Description of methods. Spine (Phila Pa 1976). 1989;14:879-883.
24. Licht N.J., Rowe D.E., Ross L.M. Pitfalls of pedicle screw fixation in the sacrum. A cadaver model. Spine (Phila Pa 1976). 1992;17:892-896.
25. Zindrick M.R., Wiltse L.L., Widell E.H., et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;203:99-112.
26. Ogilive J.W., Bradford D.S. Sublaminar fixation in lumbosacral fusions. Clin Orthop Relat Res. 1991;269:157-161.
27. Stovall D.O.Jr., Goodrich J.A., Lundy D., et al. Sacral fixation technique in lumbosacral fusion. Spine (Phila Pa 1976). 1997;22:32-37.
28. Nagata H., Schendel M.J., Transfeldt E.E., et al. The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine (Phila Pa 1976). 1993;18:2471-2479.
29. Carlson G.D., Abitbol J.J., Anderson D.R., et al. Screw fixation in the human sacrum. An in vitro study of the biomechanics of fixation. Spine (Phila Pa 1976). 1992;17:S196-S203.
30. Carson W.L., Duffield R.C., Arendt M., et al. Internal forces and moments in transpedicular spine instrumentation. The effect of pedicle screw angle and transfixation: the 4R-4bar linkage concept. Spine (Phila Pa 1976). 1990;15:893-901.
31. Ruland C.M., McAfee P.C., Warden K.E., et al. Triangulation of pedicular instrumentation. A biomechanical analysis. Spine (Phila Pa 1976). 1991;16:S270-S276.
32. Asher M., Carson W., Heining C., et al. A modular spinal rod linkage system to provide rotational stability. Spine (Phila Pa 1976). 1988;13:272-277.
33. Pintar F.A., Maiman D.J., Yoganandan N., et al. Rotational stability of a spinal pedicle screw/rod system. J Spinal Disord. 1995;8:49-55.
34. Abdu W.A., Wilber R.G., Emery S.E. Pedicular transvertebral screw fixation of the lumbosacral spine in spondylolisthesis. A new technique for stabilization. Spine (Phila Pa 1976). 1994;19:710-715.
35. Heller J.G., Ghanayem A.J., McAfee P., Bohlman H.H. Iatrogenic lumbar spondylolisthesis: treatment by anterior fibular and iliac arthrodesis. J Spinal Disord. 2000;13:309-318.
36. Majd M.E., Holt R.T. Anterior fibular strut grafting for the treatment of pseudoarthrosis in spondylolisthesis. Am J Orthop. 2000;29:99-105.
37. Smith J.A., Deviren V., Berven S., et al. Clinical outcome of trans-sacral interbody fusion after partial reduction for high-grade l5-s1 spondylolisthesis. Spine (Phila Pa 1976). 2001;26:2227-2234.
38. Smith M.D., Bohlman H.H. Spondylolisthesis treated by a single-stage operation combining decompression with in situ posterolateral and anterior fusion. An analysis of eleven patients who had long-term follow-up. J Bone Joint Surg [Am]. 1990;72:415-421.
39. Whitecloud T.S.3rd, Butler J.C. Anterior lumbar fusion utilizing transvertebral fibular graft. Spine (Phila Pa 1976). 1988;13:370-374.
40. Esses S.I., Natout N., Kip P. Posterior interbody arthrodesis with a fibular strut graft in spondylolisthesis. J Bone Joint Surg [Am]. 1995;77:172-176.
41. Meyers A.M., Noonan K.J., Mih A.D., Idler R. Salvage reconstruction with vascularized fibular strut graft fusion using posterior approach in the treatment of severe spondylolisthesis. Spine (Phila Pa 1976). 2001;26:1820-1824.
42. Asher M.A., Strippgen W.E. Anthropometric studies of the human sacrum relating to dorsal transsacral implant designs. Clin Orthop Relat Res. 1986;203:58-62.
43. Allen B.L.Jr., Ferguson R.L. The Galveston technique for L rod instrumentation of the scoliotic spine. Spine (Phila Pa 1976). 1982;7:276-284.
44. Allen B.L.Jr., Ferguson R.L. The Galveston technique of pelvic fixation with L-rod instrumentation of the spine. Spine (Phila Pa 1976). 1984;9:388-394.
45. Dumont C.E., Damsin J.P., Forin V., et al. Lumbosacral agenesis. Three cases of reconstruction using Cotrel-Dubousset or L-rod instrumentation. Spine (Phila Pa 1976). 1993;18:1229-1235.
46. Cunningham B.W., Lewis S.J., Long J., et al. Biomechanical evaluation of lumbosacral reconstruction techniques for spondylolisthesis: an in vitro porcine model. Spine (Phila Pa 1976). 2002;27:2321-2327.
47. Lebwohl N.H., Cunningham B.W., Dmitriev A., et al. Biomechanical comparison of lumbosacral fixation techniques in a calf spine model. Spine (Phila Pa 1976). 2002;27:2312-2320.
48. Baldwin N.G., Benzel E.C. Sacral fixation using iliac instrumentation and a variable angle screw device. J Neurosurg. 1994;81:313-316.
49. Cahill D.W. Infections of the spine. Contemp Neurosurg. 1993;15:1-8.
50. Axelsson P., Johnsson R., Stromqvist B. Lumbar orthosis with unilateral hip immobilization. Effect on intervertebral mobility determined by roentgen stereophotogrammetric analysis. Spine (Phila Pa 1976). 1993;18:876-879.
51. Shikata J., Yamamuro T., Kotoura Y., et al. Total sacrectomy and reconstruction for primary tumors. Report of two cases. J Bone Joint Surg [Am]. 1988;70:122-125.
52. Tomita K., Tsuchiya H. Total sacrectomy and reconstruction for huge sacral tumors. Spine (Phila Pa 1976). 1990;15:1223-1227.