CHAPTER 16 COMMON PREHOSPITAL COMPLICATIONS AND PITFALLS IN THE TRAUMA PATIENT
The evolution of prehospital care in this country has an interesting and continually evolving record. Although there is recorded history of wagons and carts being used to transport the sick and injured as early as 900 ACE, the term “ambulance” was not used until introduced by Queen Isabella of Spain in the early 15th century. Even at that time, it referred more to military field hospitals and tents for the wounded than to a means of transporting wounded and dead from battlefields. Not until the time of Baron Larrey would the term “ambulance” take up its more current meaning of “a specially equipped motor vehicle, airplane, or ship for carrying sick or injured people, usually to a hospital.”1
One of the prime factors identified as contributing to the continued reduction in battlefield casualties from 8% in World War I to less than 2% in the Vietnam War was reducing the time from injury to initiation of medical care. On this backdrop, the mid-1960s and early 1970s sought to improve prehospital care, education, equipment, and processes. The early 1960s called for an extension of basic and advanced first aid training to greater numbers of the lay population, and preparation of nationally accepted texts, training aids, and courses of instruction for rescue squad personnel, policemen, firefighters, and ambulance attendants.2 Ambulance services in the 1960s was very piecemeal and adequate at best. In a few major cities, there were specially equipped ambulances prepared to care for the injured and sick, and trained professional prehospital personnel were available. However, approximately 50% of the country’s ambulance services at that time were provided by over 12,000 morticians mainly because their vehicles were able to accommodate transportation of patients on gurneys or stretchers.
In the mid-1960s, the National Traffic and Motor Safety Act and the Highway Safety Act3 provided for the establishment of national standards for used motor vehicles, motor vehicle inspections, and emergency services. Communications were also problematic. At a time when the United States had just placed a man on the moon, it was easier in most instances to communicate with that extraterrestrial individual than it was for prehospital providers to communicate with the emergency department where they were headed.
Over the next several decades, the education and provision of specifically equipped vehicles progressed until the mid-1980s when Injury in America: a Continuing Public Health Problem was published.4 Although the report found that there had been significant progress in the credentialing and education of prehospital care providers, more than 2.5 million Americans died from injuries in the 1966–1985 period. This prompted the expenditure of more federal dollars to study the continuing public health problem, as the report noted and called for the institution of more systems of communication and transportation of the injured to facilities specially equipped for managing critically injured patients.
In 1992, the Model of Trauma Care Systems Plan, developed by Health Resources and Services Administration under the Authority of the Trauma Systems Planning and Development Act of 1990,5 marked the next major step in the evolution of health policy related to trauma care. This plan emphasized the need for a fully inclusive trauma care system that involved not only trauma centers, but also all health care facilities according to availability of trauma resources, including prehospital providers. As a result, the numbers of dedicated trauma centers and state trauma systems developed, although at a still less-than-adequate pace. Trauma centers were charged with becoming resource facilities for emergency medical response agencies. Educational programs such as Prehospital Trauma Life Support (PHTLS), Basic Trauma Life Support (BTLS), and others were developed with states being empowered to license and credential prehospital providers at various levels.
INCIDENCE
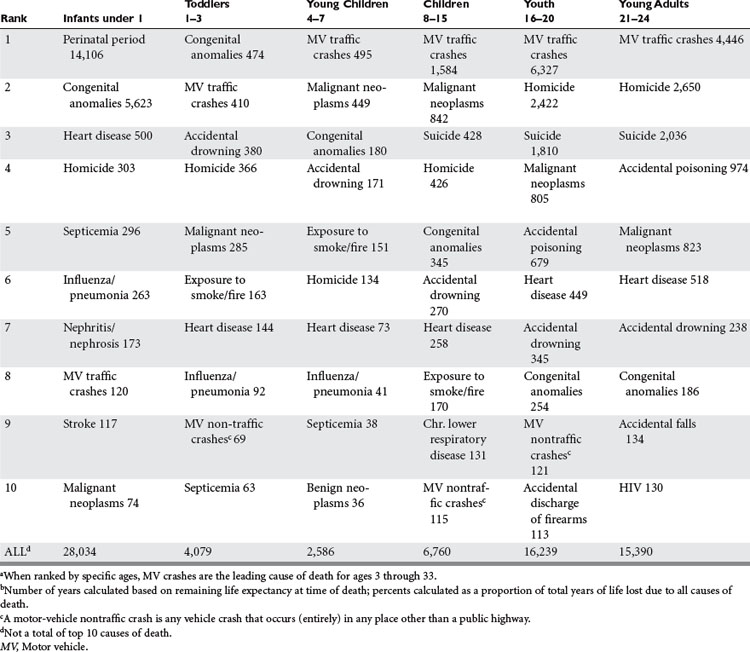
According to the National Highway Traffic Safety Administration, the leading cause of death in the United States in 2002 for people aged 4–34 is overwhelmingly motor vehicle traffic crashes (Table 1). In terms of years of life lost, motor vehicle crashes ranks third, after malignant neoplasms and heart disease, at 5% of total years of life lost for the entire population.
The foundation of Advanced Trauma Life Support® of the American College of Surgeons6 stresses an ABC (airway, breathing, and circulation) approach. Much of the emphasis on prehospital care and subsequent care involves appropriate management of the airway, providing for ventilation by breathing for the patient, and control of circulation consisting of hemorrhage control and restoration of intravascular volume. Not surprisingly, the most common prehospital complications occur in these three areas.
AIRWAY
Ensuring that the trauma victim has a patent airway is the highest management priority.7 If manual maneuvers (clearing the airway of foreign bodies, jaw thrust, or chin lift) or basic adjuncts (oropharyngeal or nasopharyngeal airways) are not adequate to maintain the airway, then alternate, more invasive methods are required.
BREATHING
A tension pneumothorax is a life-threatening situation as a result of an injury to the lung causing a pneumothorax that results in air leaking into the pleural space, causing increased pressure that results in difficult ventilation and decreased venous return. Typically it is recognized by a variety of signs and symptoms, including tachypnea, dyspnea, decreased breath sounds or unilateral absence of breath sounds, air hunger, respiratory distress, tachycardia, hypotension, tracheal deviation, neck vein distention, and cyanosis (late). Hyperresonant percussion tone and absent breath sounds are typical of a significant pneumothorax. While there are many signs and symptoms that are associated with a tension pneumothorax, some may be difficult to recognize in the prehospital setting, and some may not be present in all situations. In a patient who has required intubation and positive pressure ventilation, a minimal lung injury may develop into a clinically significant tension pneumothorax, and should be anticipated if a patient in this type of setting suddenly deteriorates.
CIRCULATION
One of the most common prehospital complications related to circulation is the failure to detect and address ongoing hemorrhage. Control of external hemorrhage is best controlled by applying direct pressure to the bleeding site. Common areas that are missed that are sources of external hemorrhage include the posterior scalp, axillae, perineum, and posterior trunk. Bulky dressings, particularly applied to the scalp, may be dangerous for a number of reasons. First, they can hide posterior scalp hemorrhage from view of the providers while providing a false sense of security that the bleeding has been controlled. Failure to recognize signs and symptoms of intrathoracic, intra-abdominal and pelvic bleeding is another potential prehospital complication related to circulatory insufficiency.
Prehospital intravenous fluid therapy is an area of continued controversy. A thorough discussion of the types and amount of fluid to be administered in the prehospital setting is beyond the scope of this chapter. In general, there are very few complications in the prehospital setting related to fluid excess. There is also evidence that subsets of patients—particularly trauma patients who have suffered penetrating trauma—may do better with no prehospital fluid or limited prehospital fluid than those who receive prehospital fluid.8 There is general agreement among providers of trauma care that extra time spent in the field trying to obtain intravenous access is detrimental to efforts to get the patient to definitive care and attempts to obtain access should be limited in most situations.9 In the case of significant intracavitary bleeding, fluid cannot be administered in adequate amounts in the prehospital setting to restore effective intravascular volume. Therefore, efforts should be directed toward expeditious transfer to definitive care.
Other causes of circulatory insufficiency must be kept in mind. Pericardial tamponade manifested by Beck’s triad of hypotension, jugular venous distension, and muffled heart tones may be difficult to discern in the frenetic prehospital setting. A temporizing measure for this rare prehospital occurrence it pericardiocentesis. Complications related to this procedure are significant and include, but are not limited to, inadvertent ventricular laceration/puncture, laceration of the coronary arteries or vein, injury to the thoracic or upper abdominal great vessels, pneumothorax, or injury to the upper abdominal viscera. Prehospital attempts at pericardiocentesis are discouraged except by the most experienced providers and then in only the most dire of circumstances. Restoration of intravascular volume may temporarily offset the negative circulatory effects of pericardial tamponade, but, again, rapid transport to definitive care is the best approach in this situation.
DISABILITY
The major goal during the resuscitation of patients with traumatic neurologic injury is to avoid or minimize secondary brain injury and spinal cord damage. Avoiding hypoxemia and shock are also major priorities. Management of ventilation and maintenance of cerebral perfusion pressure can and should be addressed, altered, and optimized in the prehospital setting. Maintaining adequate perfusion and oxygenation in order to prevent secondary brain injury makes a positive difference in morbidity and mortality from TBI. The ABCs are important in the management of TBI in order to prevent secondary brain injury. The goals should be to maintain systolic blood pressure greater than 90 mm Hg, oxygenation saturations of at least 95%, and provide ventilation to maintain ETCO2 of 30–35 mm Hg.10
Historically, prehospital intubation has been the highest priority for patients with TBI with an associated coma (GCS ≤8), but recent evidence has shown that prehospital intubation may worsen outcomes for patients with TBI.11 This has been somewhat controversial and has been refuted based on the variability of the expertise of prehospital providers, and the use of neuromuscular blockade agents (rapid-sequence intubation [RSI]) as an aid to intubation, which varies based on prehospital protocols. These results appear to be related to the expertise of the prehospital provider and the use of neuromuscular blockade agents (RSI). Intubation with pharmacologic agents is thought to lessen the “struggling” and difficulty in intubation. Without adequate sedation or paralytics, the intubation time may be prolonged, resulting in hypoxia, which may be the reason for the worsened outcomes, versus providers that have full pharmacologic agents available. Additionally, some prehospital providers have more expertise in intubation techniques, based on frequency of intubation. Therefore, it likely depends on the expertise and ease of intubation whether intubation is beneficial or harmful in the prehospital setting for patient outcomes with TBI.12 Using the BVM technique and maintaining adequate minute ventilation and oxygenation is preferred compared to a prehospital provider with less proficiency at endotracheal intubation and the potential for the patient to have significant (degree and duration) hypoxemia and/or hypercarbia while attempting to accomplish endotracheal intubation. The use of intravenous lidocaine (1 mg/kg) may blunt an increase in intracranial pressure (ICP) during intubation.
Controlled hyperventilation—mild therapeutic hyperventilation (ETCO2 of 25–30 mm Hg)—may be utilized in situations with acute neurologic deterioration with signs of herniation or obvious increase in ICP. Hyperventilation should be stopped if the signs of intracranial hypertension resolve (i.e., dilated pupil responds). Prophylactic hyperventilation should not be used in the prehospital management of TBI. Overaggressive hyperventilation produces cerebral vasoconstriction that in turn leads to a decrease in cerebral oxygen delivery. Routine prophylactic hyperventilation has been shown to worsen neurologic outcomes and should not be used.10
COMORBIDITIES
With advancement of age of the general population, the use of anticoagulants (warfarin, clopidogrel, aspirin) is becoming more common. Failure to recognize the patient who is fully medically anticoagulated may lead to a delay in recognizing significant intracranial, intrathoracic, or intra-abdominal bleeding. Alternatively, recognition of the medically anticoagulated state can lead to a higher index of suspicion on the part of prehospital providers as to the potential for significant injury, despite what might otherwise be considered minor trauma.
1 Ortiz JM. U.S. Army Medical Department Journal. October–December 1998:17-25.
2 National Research Council. Accidental Death and Disability: The Neglected Disease of Modern Society. Washington, DC: National Academy Press, 1996.
3 Highway Safety Act 1966 (PL 89–564), September 9, 1966
4 National Research Council. Injury in America: A Continuing Public Health Problem. Washington, DC: National Academy Press, 1985.
5 Trauma Systems Planning and Development Act of 1990 (PL 101–590), November 16, 1990
6 American College of Surgeons. Advanced Trauma Life Support Program for Physicians. Chicago: American College of Surgeons Committee on Trauma, 1993.
7 Prehospital Trauma Life Support Committee of the National Association of Emergency Medical Technicians in cooperation with the Committee on Trauma of the American College of Surgeons PHTLS—Basic and Advanced Prehospital Trauma Life Support. 5 ed. St. Louis, MO: Mosby; 2003.
8 Bickell WH, Wall MJ, Pepe PE, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med. 1994;331:1105-1109.
9 Sampalis JS, Tammim H, Davis R, et al. Ineffectiveness of on-site intravenous lines: is prehospital time the culprit? J Trauma. 1997;43:608-615.
10 Vincent J-L, Bené J. Primer on medical management of severe brain injury. Crit Care Med. 2005;33(6):1392-1399.
11 Davis DP, Hoyt DB, Ochs M, et al. The effect of paramedic rapid sequence intubation on outcome in patients with severe traumatic brain injury. J Trauma. 2003;54(3):444-453.
12 Cascio AN. Letter to the editor. J Trauma. 2004;56(2):454.