chapter 11
Common Neck, Arm and Upper Back Problems
Neck and arm pain and sensory disturbance with or without weakness in the arm are very common complaints. This chapter will discuss the more frequently encountered peripheral nervous system (lower motor neuron)1 problems and the non-neurological conditions seen in everyday clinical practice. It will emphasise those features that help differentiate one problem from another. The chapter will be divided into three sections reflecting the regions of complaints most often seen in clinical practice:
Essentially there are only four neurological symptoms that can develop in a limb:
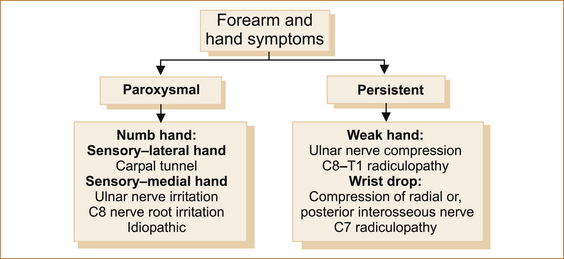
When a patient presents complaining of problems in the arm, for example, the important thing to establish is whether the symptoms relate to a non-neurological or a neurological problem and whether, if the latter, it is a peripheral (‘lower motor neuron’) or central (‘upper motor neuron’) problem. Remember the peripheral nervous system in the upper limb consists of the anterior horn cell in the spinal cord, the motor and sensory nerve roots, brachial plexus, peripheral nerves, neuromuscular junctions and muscle. A central nervous system problem is anything above the level of the anterior horn cell, i.e. in the spinal cord, brainstem, deep cerebral hemisphere or cortex (see Figure 1.1). The pattern of weakness and sensory disturbance together with the reflexes will help determine whether the problem is central or peripheral. Finally, it is important to establish whether the symptoms are intermittent or persistent as different conditions present with either paroxysmal or persistent symptoms. Pain in the arm is only occasionally related to the nervous system but, when it is, it almost invariably indicates a problem in the peripheral nervous system as central causes of pain are very rare.
Symptoms arising from peripheral nerve lesions can arise as a result of three mechanisms:
• direct trauma, in which case the neurological symptoms will be present from the moment of trauma
• compression of the nerve (referred to as entrapment syndromes), in which case the symptoms will be persistent and, as the compression worsens, the severity of the symptoms (in terms of intensity and the extent of involvement of the muscles or area of sensation supplied by the particular nerve or nerve root) will increase
• irritation, which is also seen with entrapment syndromes, where the symptoms are initially intermittent and often provoked by certain activities; with repeated and prolonged irritation damage may result in persistent weakness and/or sensory loss.
NECK PAIN
Acute spasm of the neck muscles
The most common form is torticollis, often referred to as a ‘wry neck’. It is a self-limiting condition, resolving within days. More severe and disabling but very rare forms of congenital and acquired spasmodic torticollis occur [1] but are beyond the scope of this book.
Non-specific neck pain
The aetiology of this entity is uncertain but it is often encountered in patients with psychological problems such as anxiety or depression [2].
Whiplash
• Within the hours to first day or up to a few days after whiplash injury the patient complains of neck pain and stiffness, with or without a decreased a range of motion of the neck. Tenderness on palpation of the neck muscles and even the spinal processes is common. The pain may radiate into the shoulders or down the spine to the thoracic region.
• Headache frequently occurs together with insomnia, complaints of poor memory and difficulty concentrating [3].
• A small percentage of patients will develop non-specific and diffuse arm pain with or without subjective weakness and/or sensory symptoms in the arm that are clearly beyond the distribution of a single nerve or nerve root and are not related to nerve root compression. The pain and neurological symptoms in the arm, unlike cervical nerve root compression, are often aggravated by movement of both the arm and the neck while nerve root compression may be aggravated by movement of the neck but not the arm.
• Imaging is usually normal although in older patients degenerative disease may be seen and is often incorrectly invoked as the cause of the symptoms.
• The duration of symptoms varies from a few weeks to months or even years (the late whiplash syndrome, a controversial entity [4]), although 90–95% of patients experience only pain that settles within weeks.
The aetiology of whiplash is unknown and, curiously, it is not seen at all in Lithuania where there is little awareness of the syndrome and no accident compensation scheme [5, 6].
Cervical radiculopathy
Cervical radiculopathy arising from the 3rd and 4th cervical nerve roots is very rare. Unilateral pain in the suboccipital region, extending to the back of the ear, and in the dorsal or lateral aspect of the neck occurs with radiculopathy of the 3rd cervical nerve root. C4 radiculopathy results in unilateral pain that may radiate to the posterior neck and trapezius region and to the anterior chest but does not typically radiate into the upper extremity [7]. Neither is associated with any discernible weakness although neurological symptoms may occur with sensory symptoms in the distribution of the C3 or C4 nerve root and, in the very rare occurrence when a radiculopathy is associated with spinal cord compression, an upper motor neuron pattern of weakness in all four or just the lower limbs with or without sensory symptoms and a possible sensory level may result. The term ‘sensory level’ refers to the level within the central nervous system that the spinothalamic dermatomal sensory loss extends up to on the trunk or in the limbs.
PROBLEMS AROUND THE SHOULDER AND UPPER ARM
Pain with or without focal neurological symptoms in the shoulder and upper arm
• nerve root compression of the 4th, 5th and 6th cervical nerve roots
• suprascapular nerve entrapment syndrome
Figure 11.1 lists the common causes of pain in the region of the shoulder.
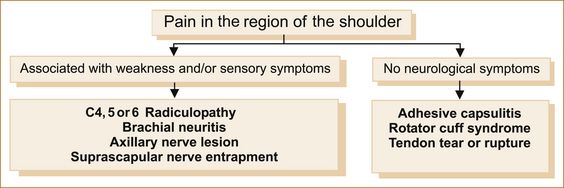
FIGURE 11.1 Painful conditions affecting the shoulder region
NEUROLOGICAL CAUSES
Radicular pain: Pain from nerve root compression, if associated with weakness and/or sensory disturbance in the distribution of the nerve root, is readily diagnosed. However, pain may occur in the absence of or precede neurological symptoms by days or even weeks. Although radicular pain may affect the upper (C4–C5) arm, it is more common in the lower (C6–8) arm.
Numbness and/or localised shoulder pain not influenced by movement of the shoulder suggests a possible C5 nerve root problem. Where neurological symptoms and signs develop, the numbness is located over the top of the shoulder along its mid-portion and extends laterally to the upper arm but not into the forearm. There may be weakness of the supraspinatus, infraspinatus and deltoid muscles [7].
Brachial neuritis or neuralgic amyotrophy: The diagnosis should be suspected when severe shoulder pain aggravated by movement of the shoulder is associated with weakness and sensory disturbance in the arm. Van Alfen et al [10] have described the clinical details in a large series of patients. As there is no ‘gold standard’ diagnostic test for brachial neuritis, the clinical features of neuralgic amyotrophy are likely to evolve.
SYMPTOMS: The classic symptoms begin with the subacute onset over weeks of increasingly severe constant unilateral pain predominantly in the shoulder girdle; less commonly, the pain may come on rapidly. Rarely, bilateral cases occur but one side is usually affected for some hours or up to 2 days before the other side is involved [11]. This constant pain persists on average for approximately 3–4 weeks but may last as little as a few days or up to 60 days or more. In many patients it may be followed by a movement-evoked severe stabbing pain that can persist for months. In a small proportion of cases the pain can radiate from the shoulder to the arm, the cervical spine or neck down into the arm, the scapular or dorsal region to the chest wall and/or arm, or be confined to a lower plexus distribution (e.g. medial arm and/or hand, axilla).
The shoulder pain is aggravated by movement of the shoulder, not the neck, but here there are neurological symptoms such as weakness and sensory disturbance in the arm that indicate a neurological cause for the pain. Although local heat to the shoulder region occasionally provides some relief from the pain, this is non-specific and cannot be used in diagnosis. Individual nerves can be affected in brachial neuritis, in particular the suprascapular, axillary, musculocutaneous, long thoracic and radial nerves [11].
Progressive weakness developing over days may commence within 24 hours after the onset of the pain or may be delayed for up to 4 weeks [11]. Although any part of the plexus can be involved, the upper brachial plexus is more commonly affected in males whereas the middle and lower brachial plexus is more commonly affected in females. Wasting may occur with prolonged symptoms. Recovery can take months or even years. Sensory involvement is common and sensory symptoms can be very diffuse and non-localising.
Recurrence is rare but can occur and familial cases, termed hereditary neuralgic amyotrophy, have been described. Hereditary neuropathy with pressure palsy can also cause neuralgic amyotrophy and is related to a defect in the peripheral myelin protein 22 and is regarded as a distinct disorder [12].
Axillary nerve lesion: Axillary nerve lesions are usually related to traumatic dislocation of the shoulder joint as a result of either a sporting injury or secondary to a tonic–clonic seizure. Less commonly they occur with a fracture of the neck of the humerus or following shoulder surgery. As with all single nerve (mononeuritis) lesions, some are idiopathic (unknown cause).
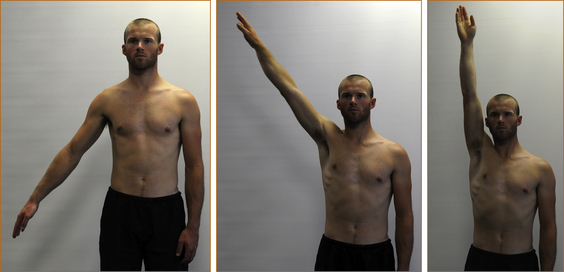
EXAMINATION: There is weakness of shoulder abduction beyond the first 30° (the initial 30° is supplied by the supraspinatus muscle) due to weakness of the deltoid muscle (see Figure 11.2). There may be a small patch of numbness over the lower aspect of the deltoid muscle. When the lesion relates to dislocation, there is often pain in the shoulder aggravated by movement of the shoulder. The presence of pain and weakness with a history of trauma to the shoulder is a strong pointer to the diagnosis. The prognosis for recovery is variable [13].
Suprascapular nerve entrapment: The suprascapular nerve arises from the junction of the 5th and 6th cervical nerve roots and traverses an oblique course across the supraspinatus fossa, relatively fixed on the floor of the fossa and tethered underneath the transverse scapular ligament, to the scapular notch and supplies the supraspinatus and infraspinatus muscles. Most often the suprascapular entrapment syndrome relates to local compression by the suprascapular ligament although it may be idiopathic in origin or due to rarer causes [14]. Although very rare, it is a diagnosis not to be missed as prompt treatment is more likely to result in resolution of the problem.
SYMPTOMS: The pain is deep and diffuse, localised to the posterior and lateral aspects of the shoulder and may be referred into the arm, neck or upper anterior chest wall. Certain scapular motions may be painful, causing the patient to restict shoulder movement. Adduction of the arm across the body tenses the nerve and may increase the pain. Occasionally, the patient may complain of burning, aching or crushing pain.
EXAMINATION: It is important to test the supraspinatus and infraspinatus muscles, looking for weakness confined to those muscles. Remember, pain may give the appearance of weakness with the patient not exerting a full effort as a result of the pain. The clue that the weakness relates to pain from the shoulder is that, in addition to the supraspinatus and infraspinatus appearing weak, the deltoid and subscapularis muscles will also appear weak. Severe suprascapular nerve entrapment results in atrophy and permanent weakness of the supraspinatus and infraspinatus muscles (see Figure 11.3).
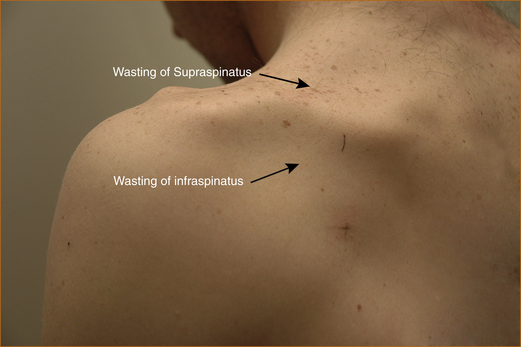
FIGURE 11.3 Suprascapular entrapment with marked wasting of the supraspinatus and infraspinatus muscles
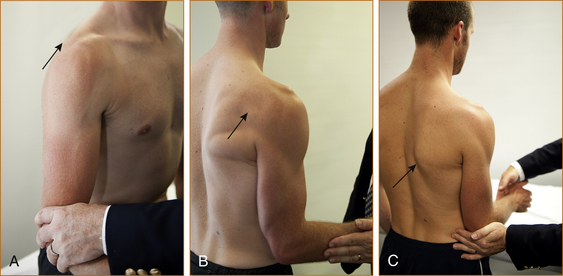
FIGURE 11.4 A Method of testing the supraspinatus. The arm is abducted approximately 20–30° away from the chest wall while the examiner pushes on the elbow, trying to force the arm back against the chest wall.
B Method of testing the infraspinatus. The elbow is kept next to the chest wall and the semi-flexed forearm is externally rotated against resistance.
C Method of testing the subscapularis. The arm is bent at a right angle at the elbow and the forearm is semi-pronated. The elbow is kept at the side and the patient is asked to rotate the forearm in towards the body while the examiner tries to prevent this by pushing the forearm in the opposite direction.
NON-NEUROLOGICAL CAUSES OF SHOULDER PAIN
Adhesive capsulitis: Adhesive capsulitis or the ‘frozen shoulder’ results in a gradual onset of pain and stiffness that leads to a restricted range of movement at the shoulder joint. It is usually seen in patients over the age of 40. A normal range of movement of the shoulder is incompatible with the diagnosis and X-rays are usually normal. The aetiology of this condition is unclear but it is not uncommon in the setting of a hemiplegia.
Rotator cuff syndrome: Probably the commonest cause of pain affecting the shoulder joint is non-neurological and is related to rotator cuff syndrome, also referred to as impingement syndrome. There are four tendons in the rotator cuff and these tendons are related individually to the following muscles: teres minor, subscapularis, infraspinatus and supraspinatus. The rotator cuff is compressed against the acromium causing bursitis, tendinitis and eventually a rotator cuff tear. Partial or complete tears or inflammation (tendinitis, tendinosis, calcific tendinitis) associated with rotator cuff injury occur in the region near where these tendon/muscle complexes attach to the humerus [17]. Other causes of pain in the shoulder joint include adhesive capsulitis and arthritis.
SYMPTOMS: Symptoms are generally those of pain, initially after and then during activity. The pain can often be relieved by rest. Patients over 40 years of age are more susceptible to rotator cuff tendinosis with overuse. In this age group the most prominent complaint is pain with overhead use and athletic activities. Night pain and an inability to lie on that side are also common [17]. Although the pain may radiate into the arm and the neck it is clearly related to movement of the shoulder and not the neck, indicating local shoulder pathology and not radicular pain. Pain in the shoulder between 60° and 180° of elevation is typical of a rotator cuff problem and is termed the painful arc syndrome (see Figure 11.5).
Painless weakness affecting the shoulder region and upper arm
CERVICAL NERVE ROOT COMPRESSION
Cervical nerve root compression more commonly affects the lower cervical nerve roots (C7–T1), but rarely compression of the C5 and/or C6 nerve root or an upper cord brachial plexus problem [28] can result in painless weakness in the shoulder and upper arm region [29, 30]. The weakness will affect all C5 and C6 innervated muscles around the shoulder: supraspinatus, infraspinatus, subscapularis, deltoid, biceps and brachialis. If C6 is the major component, brachioradialis will also be weak. In general, a radiculopathy is more likely to be associated with pain.
WINGING OF THE SCAPULA
Most patients with a mononeuritis of the long thoracic nerve to the serratus anterior muscle are not aware of the problem until someone points out that their shoulder blade is protruding (see Figure 11.6). Occasional patients notice difficulty reaching up to high places with the affected arm with or without mild shoulder pain [31]. Most patients recover spontaneously but this may take up to 2 years.
Painless numbness affecting the shoulder and upper arm
Sensation over the lower aspect of the neck, shoulder and upper arm is supplied via the 3rd to 5th cervical nerve roots. As degenerative disease predominantly affects the lower aspect of the cervical spine (C6, C7, C8 and T1), it is uncommon to see isolated sensory loss in the distribution of these nerve roots. If it does occur the sensory loss will be in a dermatome pattern as shown in Figures 1.12 and 1.13.
PROBLEMS IN THE FOREARMS AND HANDS
Numbness in the hand, forearm or both
CARPAL TUNNEL SYNDROME
Symptoms: Carpal tunnel syndrome presents in two ways.
1. In most patients the symptoms arise as a result of irritation and compression of the median nerve at the wrist by the flexor retinaculum of the carpal tunnel. Patients experience paraesthesia (numbness, pins and needles or tingling) or dysaesthesia (an unpleasant sensation). The sensory branches of the median nerve innervate the lateral 3½ digits, but many patients find it difficult to localise the sensory symptoms and often describe sensory disturbance well beyond the lateral 3½ digits [32]. The duration of altered sensation varies from a few minutes up to 30 minutes or rarely longer.
2. A second presentation is usually encountered in older patients who present with either persistent altered sensation within the median nerve distribution in the hand or marked wasting of the thenar eminence (the muscles at the base of the thumb), with little in the way of nocturnal sensory symptoms.
Some patients complain of pain in the hand and at times up the arm even as far as the shoulder [33]. If the pain occurs only when the patient is experiencing sensory symptoms, it is reasonable to accept that the pain may be related to CTS. On the other hand, if the patient experiences pain at times when there are no sensory symptoms, this pain is less likely to be related to CTS and the patient may have two conditions, e.g. arthritis or occupational overuse syndrome. Patients should be advised that this pain may not be due to CTS and therefore may not resolve with appropriate treatment of CTS. The presence of pain, swelling and tenderness is not typical of CTS and suggests that either the CTS is secondary to the development of rheumatoid arthritis or the patient is not suffering from CTS.
Examination: In young patients there is usually no wasting or sensory loss, and the only abnormalities that may be found are a positive Tinel’s and/or Phalen’s sign (see Figure 11.7A–C). Tinel’s sign2 is the precipitation of a fleeting pain or sensory symptoms radiating into the palm and fingers when the median nerve is tapped at the wrist. Phalen’s sign [35] is the presence of altered sensation in some or all of the lateral 3½ digits precipitated by forced flexion of the wrist. The wrist may need to be flexed for up to 60 seconds. Occasionally, patients with a negative Phalen’s sign may develop the sensory symptoms when the wrists are extended.

FIGURE 11.7 A Tinel’s sign. The median nerve is tapped using the tendon hammer several times from the proximal portion of the hand across the wrist for 2–3 cm.
B, C Phalen’s sign. The classic description is that the wrist is flexed (B) for up to 60 seconds and, if positive, the patient will experience transient altered sensation in the fingers and hand within the distribution of the median nerve. Some patients do not experience paraesthesia in the hands with wrist flexion but may with wrist extension (C).
The sensitivity of clinical examination by a neurologist for the diagnosis of this syndrome is 84% with a specificity of 72%. The sensitivity and specificity of Tinel’s sign were 0.60 and 0.67, respectively, and of Phalen’s sign were 0.75 and 0.47, respectively [36].
The electrophysiological diagnosis is discussed in Appendix H, ‘Nerve conduction studies and electromyography’.
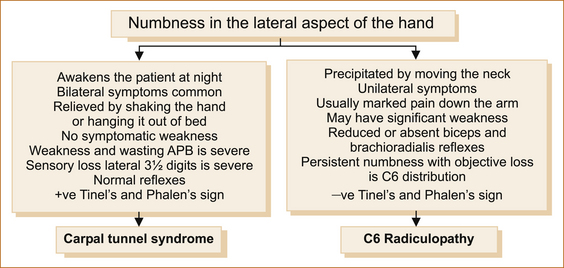
CARPAL TUNNEL SYNDROME VERSUS C6 RADICULOPATHY
Carpal tunnel syndrome is far more common than a C6 radiculopathy. Both may result in paraesthesia affecting the lateral aspect of the hand and both may result in pain in the hand and arm, although pain radiating down the arm is more in keeping with a C6 radiculopathy. Figure 11.8 highlights the difference between these two entities.
ULNAR NERVE LESIONS
Ulnar nerve lesions at the elbow present with unilateral symptoms (bilateral cases are extremely rare). Intermittent symptoms can occur if the patient leans the elbow on a desk or the arm of a chair. Isolated sensory symptoms may precede weakness for
months or even years but this is unusual. The more common presentation is the gradual onset of numbness and/or pins and needles affecting the medial 1½ digits and the medial aspect of the hand on both the palmar and dorsal surfaces. Pins and needles or numbness is the initial symptom in most patients with ongoing compression weakness and eventually wasting of the hypothenar eminence (base of the 4th and 5th digits) and the interossei and medial two lumbricals (the small muscles between the digits). An ulnar nerve lesion at the elbow is sometimes referred to
Weakness with or without numbness in the hand and forearm
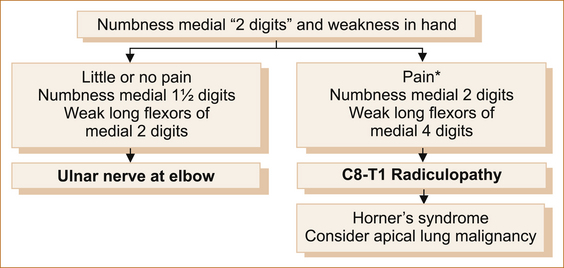
ULNAR NERVE LESION AT THE ELBOW VERSUS C8–T1 RADICULOPATHY
Both conditions can present with a gradual onset of weakness of the hand associated with altered sensation affecting the medial two digits and the medial aspect of the forearm, although often with ulnar nerve lesions the numbness is confined to the fingers and hand. The hand weakness is usually more marked with a radiculopathy as more muscles used to grip objects are affected. In neither will there be any change in the reflexes. Figure 11.9 lists the differences between these two entities. Figures 11.10 and 11.11 show how to test the long flexors of the distal phalanges of the medial four digits. Very rarely, the lower cord of the brachial plexus may be affected, e.g. with a tumour in the apex of the lung, and in this situation the sympathetic ganglion may also be affected resulting in an ipsilateral Horner’s syndrome.
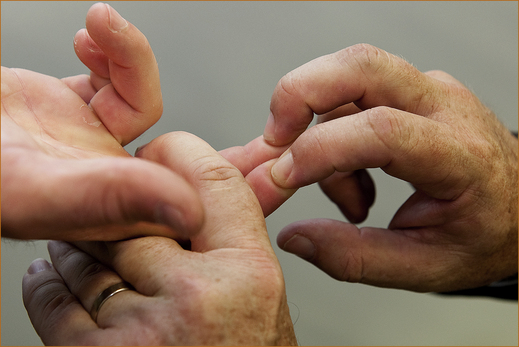
Examination: A careful examination of the pattern of weakness will differentiate these two entities. With an ulnar nerve lesion at the elbow there will be weakness of the abductor digiti minimi, the interossei, the medial two lumbricals and only the long flexors (bending the tips of the fingers at the distal interphalangeal joint) of the medial two digits (the medial aspect of the flexor digitorum profundus). Both the medial and lateral aspect of the flexor digitorum profundus is affected with C8–T1 radiculopathy. A nerve root or lower cord brachial plexus lesion will result in weakness of the long flexors of the medial four digits.
The fingers are prevented from flexing at the proximal phalangeal joint (supplied by the median nerve to the flexor digitorum superficialis) and the examiner asks the patient to bend the tips of their fingers while the examiner attempts to straighten them. The lateral two (Figure 11.10) are supplied by the median nerve and the medial two (Figure 11.11) by the ulnar nerve.
THORACIC OUTLET SYNDROME
The reason for discussing thoracic outlet syndrome (TOS) [48] is that it is frequently suspected by non-neurologists in patients with paraesthesia affecting the medial aspect of the forearm and hand in the absence of an ulnar nerve lesion [49]. Thoracic outlet syndrome is a controversial entity. It can occur in children and young adults [50, 51]. There are three types: arterial, venous and neurogenic. Neurogenic TOS is the commonest but in itself is exceedingly rare. It relates to brachial plexus compression, usually from scarred scalene muscles secondary to neck trauma. Compression can also occur with a cervical rib; however, the absence of a cervical rib on X-ray does not exclude the diagnosis as compression may be due to a fibrous band.
The most frequent neurological symptom is aching pain in the side or back of the neck extending across the shoulder and down the arm. Tingling and numbness are common in the forearm and hand in the ulnar (C8–T1) distribution. Paraesthaesia in the medial forearm and hand is a common complaint (90%), with the little finger involved four times as often as the thumb. One clue to the diagnosis is the precipitation of the paraesthesia with overhead activity or carrying heavy objects [52]. Objective sensory loss is uncommon and muscle weakness and wasting are late signs; once they develop the prognosis for recovery is poor. Sensory signs can occur without weakness and vice versa.
RADIAL NERVE PALSY (saturday night palsy)
The term ‘Saturday night palsy’ refers to the intoxicated patient who falls asleep in the chair and awakens with a wrist drop due to radial nerve compression in the radial groove of the humerus in the upper arm. The typical story is a patient awakening with a painless wrist drop with an inability to extend the wrist and fingers occasionally associated with mild sensory loss at the base of the first and second digits on the dorsal surface (see Figure 1.14).
• The patient will have weakness of the supinator (turning the forearm from the hand pointing to the ground to pointing to the ceiling), brachioradialis (flexing the elbow with the forearm semi-pronated) and the extensors of the wrist, fingers and thumb.
• The apparent weakness of the small muscles of the hand is due to the wrist drop. Strength in the adductor and abductor muscles of the fingers is normal when tested with the hand flat on a hard surface eliminating the wrist drop (see Figure 11.13F).
• The triceps reflex is preserved.
• The brachioradialis reflex is reduced or absent.
• The degree of weakness of wrist and finger extension is severe, resulting in the wrist drop.
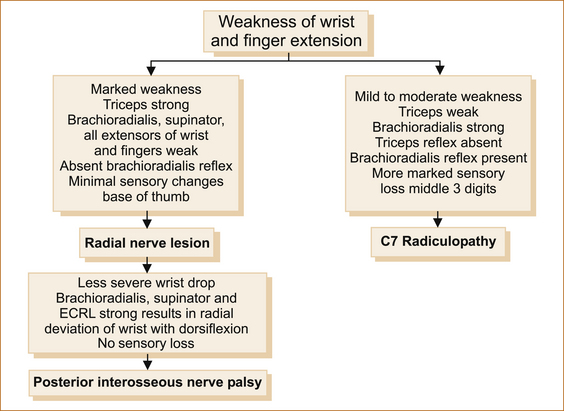
RADIAL NERVE PALSY VERSUS A C7 RADICULOPATHY
Patients with a C7 radiculopathy may also present with weakness of wrist and finger extension but it is usually less severe and radicular arm pain is more prominent. Figure 11.12 lists the differences between a C7 radiculopathy and a radial nerve lesion. Figure 11.13 shows how to determine on clinical examination if it is a radial nerve palsy and how to test finger abduction when the finger and wrist extension are very weak.







Figure 11.13 A Method of testing the triceps. Ask the patient to extend the elbow from 90° of flexion. It is important NOT to fully bend the elbow when testing the triceps as this will produce a false positive weakness of elbow extension (normal strength).
B Method of testing the biceps (arrow). The forearm is fully supinated and the patient is asked to bend the elbow (normal strength).
C Method of testing the brachioradialis. The arm is semi-pronated and flexed at the elbow, and the patient is asked to bend the arm at the elbow (weak).
D Method of testing the extensor muscles of the wrist. The patient is asked to extend the wrist and the back of the examiner’s hand is placed over the back of the patient’s hand and both exert a full effort (weak).
E Method of testing the extensor muscles of the fingers. The examiner places the metacarpophalangeal (MCP) joints across the patient’s 5th digit, and the patient’s MCP joints are placed across the examiner’s 5th digit so that both the patient and the examiner are using the same muscles to test finger extension. Both should push as hard as possible. If the strength is normal, neither the patient nor the examiner can overcome finger extension. A common method used by many is pushing down on the extended fingers with the ulnar border of the hand, but it is hard to be sure how hard the examiner should push (weak).
F1, F2 Method of testing finger abduction and adduction in the presence of wrist drop. A wrist drop can give the false impression of weakness of the ulnar innervated muscles that abduct and adduct the fingers. Ask the patient to place the palm on a firm surface so that the fingers are touching the surface and then test adduction and abduction. The strength will be normal with a radial nerve lesion.
RADIAL TUNNEL SYNDROME OR POSTERIOR INTEROSSEOUS NERVE ENTRAPMENT
Radial tunnel syndrome is an extremely rare cause of weakness affecting the extensor muscles of the wrist and hand. Once again, a delay in recognition is more likely to result in a poor outcome with treatment. It is due to a compressive neuropathy of the posterior interosseous nerve (a branch of the radial nerve). The posterior interosseous nerve is compressed in an aponeurotic (deep fascia attached to muscle) cleft in the supinator muscle.
Pain in the forearm
TENNIS ELBOW OR LATERAL EPICONDYLITIS
Although referred to as tennis elbow, this condition is not confined to tennis players. It produces pain and tenderness over the lateral aspect of the elbow, radiating into the proximal forearm extensor muscles. The pain is aggravated by the patient clenching the fist, e.g. while lifting heavy objects. There is no sensory disturbance or weakness, although the pain may limit the patient’s ability to exert a full effort giving the impression of weakness. It is an overuse injury involving the extensor radialis brevis muscle, which originates on the lateral epicondylar region of the distal humerus.
OCCUPATIONAL OVERUSE SYNDROME
Pain is the predominant symptom and is diffuse occurring in the hand, wrist, forearm, elbow, shoulder, scapular region and neck, clearly beyond the distribution of any single nerve or nerve root. There is also diffuse tenderness of muscles, joints and ligaments in the forearm and less commonly the upper arm [53].
FOREARM PAIN RELATED TO CERVICAL RADICULOPATHY
Relationship between symptoms and nerve root involvement: Sensory symptoms, if present, will be in the distribution of the nerve roots (see Figures 1.12 and 1.13).
The particular nerve root involved will influence the pattern of weakness.
• In the forearm pain occurs along the lateral border (radial side) of the forearm with C6 lesions.
• Pain involving the whole arm radiating into the 3rd digit suggests C7 (as the C7 nerve root supplies the periosteum of bone, the pain is more diffuse affecting the whole limb).
• Pain on the medial (ulnar side) indicates C8 nerve root pathology.
• Upper arm or shoulder pain may also occur with a C6, C7 or C8 radiculopathy. Suprascapular pain (C5 or C6), interscapular pain (C7 or C8) or scapular pain (C8).
Cervical radiculopathy may be acute or chronic:
• Acute cervical radiculopathy with significant pain is more common in younger patients and is usually the result of a tear in the annulus fibrosis and subsequent prolapse of the nucleus pulposus (jelly-like substance in the middle of the spinal disc) or the disc itself.
• Subacute radiculopathy occurs in patients with preexisting cervical spondylosis. These patients experience occasional neck pain and develop insidious symptoms, which are often polyradicular in nature.
• Chronic radiculopathies occur either spontaneously or when acute or subacute radiculopathies fail to respond to treatment. The gradual onset of wasting and weakness of the small muscles of the hand and forearm, sometimes associated with fasciculations is seen in the elderly and this sometimes leads to the suspicion of motor neuron disease.
Confirming the diagnosis of cervical nerve root compression:
• A plain X-ray of the cervical spine with anteroposterior, lateral and oblique views will often demonstrate narrowing of the disc space or degenerative changes causing the problem. It is important to request oblique views to see the foramen through which the nerve roots emerge.
• If the pain does not settle with conservative (non-surgical) treatment, an MRI scan can usually identify the underlying pathology.
• A plain CT scan (i.e. without myelography) only occasionally identifies the underlying pathology and is not recommended in this situation.
• When the main complaint is arm pain, surgery almost invariably relieves the pain. The weakness and sensory loss may take some months to resolve and in some cases never resolve.
COMPLEX REGIONAL PAIN SYNDROME
Symptoms can recur once or many times months or even years later.
A variety of terms have been used to describe this entity, including causalgia, shoulder–hand syndrome, reflex sympathetic dystrophy and Sudeck’s atrophy. The current nomenclature refers to complex regional pain syndrome (CRPS) types I and II, where the only difference between types I and II is the presence of a nerve lesion in type II with the
latter termed causlagia4 [Greek: kausos(heat) + algos (pain)]. Causalgia is burning pain, allodynia (pain evoked by innocuous stimulatio of the skin) and hyperpathia (an abnormal exaggerated response to a painful stimulus), usually in the hand or foot after partial injury of a nerve or one of its major branches. Pain is more severe in type II.
Clinical features: The problem may appear after a trivial injury and sometimes complicates minor surgery, e.g. for carpal tunnel. The essential clinical features include:
• persistent pain developing within days to weeks after the injury or surgery and pain that is not clearly confined to the distribution of a single nerve or nerve root
• initially increased temperature, then fluctuating between a sense of increased heat or coldness and subsequently persistent coldness
• swelling in the region of the pain
• changes in the colour of the skin, often described as mottled
Figure 11.14 lists the clinical features of some of the problems affecting the forearm and hands. It separates them into those that cause paroxysmal and those that cause persistent symptoms. Occasionally pain is absent and the patient presents with the other clinical features after an injury such as isolated coldness or altered sweating [54].
REFERENCES
1. Dauer, W.T., et al. Current concepts on the clinical features, aetiology and management of idiopathic cervical dystonia. Brain. 1998;121(Pt 4):547–560.
2. Linton, S.J. A review of psychological risk factors in back and neck pain. Spine. 2000;25(9):1148–1156.
3. Jansen, G.B., et al. Whiplash injuries: Diagnosis and early management. The Swedish Society of Medicine and the Whiplash Commission Medical Task Force. Eur Spine J. 2008;17(Suppl 3):S355–S417.
4. Radanov, B.P., Sturzenegger, M., Di Stefano, G. Long-term outcome after whiplash injury: A 2-year follow-up considering features of injury mechanism and somatic, radiologic, and psychosocial findings. Medicine (Baltimore). 1995;74(5):281–297.
5. Obelieniene, D., et al. Pain after whiplash: A prospective controlled inception cohort study. J Neurol Neurosurg Psychiatry. 1999;66(3):279–283.
6. Schrader, H., et al. Natural evolution of late whiplash syndrome outside the medicolegal context. Lancet. 1996;347(9010):1207–1211.
7. Harrop, J.S., et al. Neurological manifestations of cervical spondylosis: An overview of signs, symptoms, and pathophysiology. Neurosurgery. 2007;60(Supp1 1):S14–S20.
8. Stiell, I.G., et al. The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. 2003;349(26):2510–2518.
9. Hurwitz, E.L., et al. Treatment of neck pain: Noninvasive interventions. Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. J Manipulative Physiol Ther. 2009;32(2 Suppl):S141–S175.
10. van Alfen, N., van Engelen, B.G. The clinical spectrum of neuralgic amyotrophy in 246 cases. Brain. 2006;129(2):438–450.
11. Cruz-Martinez, A., Barrio, M., Arpa, J. Neuralgic amyotrophy: Variable expression in 40 patients. J Periph Nerv Syst. 2002;7(3):198–204.
12. Chance, P.F. Inherited focal, episodic neuropathies: Hereditary neuropathy with liability to pressure palsies and hereditary neuralgic amyotrophy. Neuromol Med. 2006;8(1–2):159–174.
13. Perlmutter, G.S. Axillary nerve injury. Clin Orthop Relat Res. 1999;368:28–36.
14. Post, M. Diagnosis and treatment of suprascapular nerve entrapment. Clin Orthop Relat Res. 1999;368:92–100.
15. Zoltan, J.D. Injury to the suprascapular nerve associated with anterior dislocation of the shoulder: Case report and review of the literature. J Trauma. 1979;19(3):203–206.
16. Solheim, L.F., Roaas, A. Compression of the suprascapular nerve after fracture of the scapular notch. Acta Orthop Scand. 1978;49(4):338–340.
17. Rodgers, J.A., Crosby, L.A. Rotator cuff disorders. Am Fam Physician. 1996;54(1):127–134.
18. Lewis, J.S. Rotator cuff tendinopathy/subacromial impingement syndrome: Is it time for a new method of assessment? Br J Sports Med. 2009;43(4):259–264.
19. Pajareya, K., et al. Effectiveness of physical therapy for patients with adhesive capsulitis: A randomized controlled trial. J Med Assoc Thai. 2004;87(5):473–480.
20. Hawkins, R.H., Dunlop, R. Nonoperative treatment of rotator cuff tears. Clin Orthop Relat Res. 1995;321:178–188.
21. Blair, B., et al. Efficacy of injections of corticosteroids for subacromial impingement syndrome. J Bone Joint Surg Am. 1996;78(11):1685–1689.
22. Yamakado, K. The targeting accuracy of subacromial injection to the shoulder: An arthrographic evaluation. Arthroscopy. 2002;18(8):887–891.
23. Watson, M. Major ruptures of the rotator cuff: The results of surgical repair in 89 patients. J Bone Joint Surg Br. 1985;67(4):618–624.
24. Stephens, M.B., Beutler, A.I., O’Connor, F.G. Musculoskeletal injections: A review of the evidence. Am Fam Physician. 2008;78(8):971–976.
25. Haahr, J.P., Andersen, J.H. Exercises may be as efficient as subacromial decompression in patients with subacromial stage II impingement: 4–8-years’ follow-up in a prospective, randomized study. Scand J Rheumatol. 2006;35(3):224–228.
26. Gartsman, G.M., O’Connor, P.D. Arthroscopic rotator cuff repair with and without arthroscopic subacromial decompression: A prospective, randomized study of one-year outcomes. J Shoulder Elbow Surg. 2004;13(4):424–426.
27. Codsi, M.J. The painful shoulder: When to inject and when to refer. Cleve Clin J Med. 2007;74(7):473–474. [477–478, 480–482 passim].
28. Schott, G.D. A chronic and painless form of idiopathic brachial plexus neuropathy. J Neurol Neurosurg Psychiatry. 1983;46(6):555–557.
29. Shimizu, S., et al. Radiculopathy at the C5/6 intervertebral foramen resulting in isolated atrophy of the deltoid: An aberrant innervation complicating diagnosis. Report of two cases. Eur Spine J. 2008;17(Suppl 2):S338–S341.
30. Yoss, R.E., et al. Significance of symptoms and signs in localization of involved root in cervical disk protrusion. Neurology. 1957;7(10):673–683.
31. Wiater, J.M., Flatow, E.L. Long thoracic nerve injury. Clin Orthop Relat Res. 1999;368:17–27.
32. Caliandro, P., et al. Distribution of paresthesias in carpal tunnel syndrome reflects the degree of nerve damage at wrist. Clin Neurophysiol. 2006;117(1):228–231.
33. Bland, J.D. Treatment of carpal tunnel syndrome. Muscle Nerve. 2007;36(2):167–171.
34. Tinel, J. Presse Medicale. 1915;47:388.
35. Phalen, G.S. The birth of a syndrome, or carpal tunnel revisited. J Hand Surg Am. 1981;6(2):109–110.
36. Katz, J.N., et al. The carpal tunnel syndrome: Diagnostic utility of the history and physical examination findings. Ann Intern Med. 1990;112(5):321–327.
37. O’Connor, D., Marshall, S., Massy-Westropp, N. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database Syst Rev. (1):2003. [CD003219].
38. Gerritsen, A.A., et al. Splinting vs surgery in the treatment of carpal tunnel syndrome: A randomized controlled trial. JAMA. 2002;288(10):1245–1251.
39. Marshall, S., Tardif, G., Ashworth, N. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev. (2):2007. [CD001554].
40. Wong, S.M., et al. Single vs two steroid injections for carpal tunnel syndrome: A randomised clinical trial. Int J Clin Pract. 2005;59(12):1417–1421.
41. Hui, A.C., et al. A randomized controlled trial of surgery vs steroid injection for carpal tunnel syndrome. Neurology. 2005;64(12):2074–2078.
42. Korthals-de Bos, I.B., et al. Surgery is more cost-effective than splinting for carpal tunnel syndrome in the Netherlands: Results of an economic evaluation alongside a randomized controlled trial. BMC Musculoskelet Disord. 2006;7:86.
43. Iida, J., et al. Carpal tunnel syndrome: Electrophysiological grading and surgical results by minimum incision open carpal tunnel release. Neurol Med Chir (Tokyo). 2008;48(12):554–559.
44. Bland, J.D. Do nerve conduction studies predict the outcome of carpal tunnel decompression? Muscle Nerve. 2001;24(7):935–940.
45. Herskovitz, S., Berger, A.R., Lipton, R.B. Low-dose, short-term oral prednisone in the treatment of carpal tunnel syndrome. Neurology. 1995;45(10):1923–1925.
46. Weber, R.A., Rude, M.J. Clinical outcomes of carpal tunnel release in patients 65 and older. J Hand Surg Am. 2005;30(1):75–80.
47. Leit, M.E., Weiser, R.W., Tomaino, M.M. Patient-reported outcome after carpal tunnel release for advanced disease: A prospective and longitudinal assessment in patients older than age 70. J Hand Surg Am. 2004;29(3):379–383.
48. Peet, R.M., et al. Thoracic-outlet syndrome: Evaluation of a therapeutic exercise program. Proc Staff Meet Mayo Clin. 1956;31(9):281–287.
49. Sanders, R.J., Hammond, S.L., Rao, N.M. Diagnosis of thoracic outlet syndrome. J Vasc Surg. 2007;46(3):601–604.
50. Maru, S., et al. Thoracic outlet syndrome in children and young adults. Eur J Vasc Endovasc Surg. 2009;38(5):560–564.
51. Gunther, T., et al. Late outcome of surgical treatment of the nonspecific neurogenic thoracic outlet syndrome. Neurol Res. 2009. [[vol]:[pages]].
52. Leffert, R.D., Perlmutter, G.S. Thoracic outlet syndrome: Results of 282 transaxillary first rib resections. Clin Orthop Relat Res. 1999;368:66–79.
53. Dennett, X., Fry, H.J. Overuse syndrome: A muscle biopsy study. Lancet. 1988;1(8591):905–908.
54. Slipman, C.W., Chow, D.W. Therapeutic spinal corticosteroid injections for the management of radiculopathies. Phys Med Rehabil Clin N Am. 2002;13(3):697–711.
55. Persson, L.C., Lilja, A. Pain, coping, emotional state and physical function in patients with chronic radicular neck pain. A comparison between patients treated with surgery, physiotherapy or neck collar – a blinded, prospective randomized study. Disabil Rehabil. 2001;23(8):325–335.
56. Fouyas, I.P., Statham, P.F., Sandercock, P.A. Cochrane review on the role of surgery in cervical spondylotic radiculomyelopathy. Spine (Phila Pa 1976). 2002;27(7):736–747.
57. Stanton-Hicks, M., et al. Reflex sympathetic dystrophy: Changing concepts and taxonomy. Pain. 1995;63(1):127–133.
58. Schott, G.D. Complex? Regional? Pain? Syndrome? Pract Neurol. 2007;7(3):145–157.
59. Veldman, P.H., et al. Signs and symptoms of reflex sympathetic dystrophy: Prospective study of 829 patients. Lancet. 1993;342(8878):1012–1016.
60. Cepeda, M.S., Carr, D.B., Lau, J. Local anesthetic sympathetic blockade for complex regional pain syndrome. Cochrane Database Syst Rev. (4):2005. [CD004598].
61. Mailis, A., Furlan, A. Sympathectomy for neuropathic pain. Cochrane Database Syst Rev. (2):2003. [CD002918].
62. Christensen, K., Jensen, E.M., Noer, I. The reflex dystrophy syndrome response to treatment with systemic corticosteroids. Acta Chir Scand. 1982;148(8):653–655.
63. Hannington-Kiff, J.G. Intravenous regional sympathetic block with guanethidine. Lancet. 1974;1(7865):1019–1020.
64. Bonelli, S., et al. Regional intravenous guanethidine vs stellate ganglion block in reflex sympathetic dystrophies: A randomized trial. Pain. 1983;16(3):297–307.
65. Robinson, J.N., Sandom, J., Chapman, P.T. Efficacy of pamidronate in complex regional pain syndrome type I. Pain Med. 2004;5(3):276–280.
66. Malik, V.K., et al. Intravenous regional phenoxybenzamine in the treatment of reflex sympathetic dystrophy. Anesthesiology. 1998;88(3):823–827.
67. Inchiosa, M.A., Jr., Kizelshteyn, G. Treatment of complex regional pain syndrome type I with oral phenoxybenzamine: Rationale and case reports. Pain Pract. 2008;8(2):125–132.
1See Chapters 1 and 3 for a discussion of upper versus lower motor neuron problems.
2Tinel described a tingling sensation when the proximal stump of an injured nerve was tapped [34].
4Diagnostic criteria for complex regional pain syndrome type I [57] (not all authors agree with this nomenclature [58]):
1. The presence of an initiating noxious event or a cause of immobilisation.
2. Continuing pain, allodynia or hyperalgesia with which the pain is disproportionate to any inciting event.
3. Evidence at some time of oedema, changes in skin blood flow or abnormal sudomotor activity in the region of the pain.
4. This diagnosis is excluded by the existence of a condition that otherwise would account for the degree of pain and dysfunction.