22 Common Fractures
Each age group has typical mechanisms of injury and common fractures. When evaluating newborns and infants with injuries, one should maintain a high index of suspicion for nonaccidental trauma because this is a leading cause of fracture in this age group (see Chapter 12). Injuries in toddlers and school-aged children most often result from falls. During adolescence, injuries become similar to those of adults and are often sustained in sports or through high-energy mechanisms, such as motor vehicle collisions.
Fracture Description
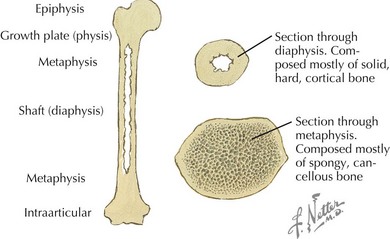
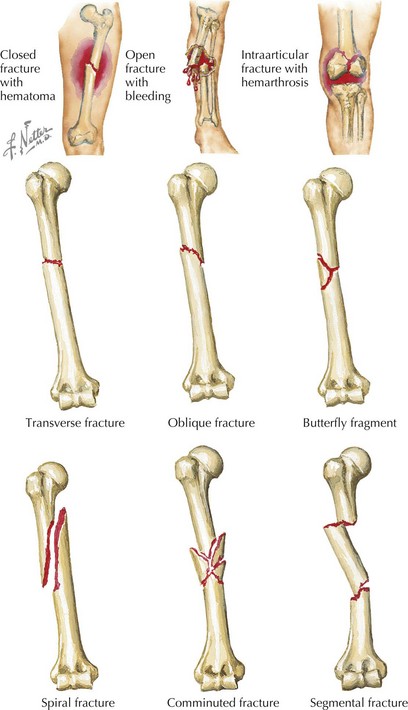
After a fracture has been identified, to effectively communicate with orthopedic consultants and other health care providers, it is important to use fracture nomenclature so that appropriate decisions can be made regarding management and treatment. Consultants should always be made aware of the patient’s neurovascular status. Radiographic interpretation of the fracture should include the type of image; anatomic location (Figure 22-1); whether it is complete or incomplete, open or closed, and intra- or extraarticular; and the presence of physeal (growth plate) disruption, displacement, angulation, shortening, or comminution (Figure 22-2).
Fractures that extend across the width of a bone are complete fractures, and those that do not extend all the way across are incomplete fractures. Incomplete fractures are more common in children than adults and are described in more detail below. Complete fractures can be further characterized according to their orientation as transverse fractures (those running at right angles to the long axis of the affected bone), oblique fractures (those that cross the shaft at an angle), and spiral fractures (fractures in which the break is helical). Any fracture that divides the bone into more than two separate segments is said to be comminuted (see Figure 22-2).
Perhaps the most important feature of a fracture is the distinction between an open and closed fracture (see Figure 22-2). In open fractures, the overlying skin is disrupted, and the fracture communicates with the outside environment, thus leading to increased risk of infection. Open fractures are an orthopedic emergency and necessitate operative repair.
Common Fracture Types in Children
Physeal Fractures
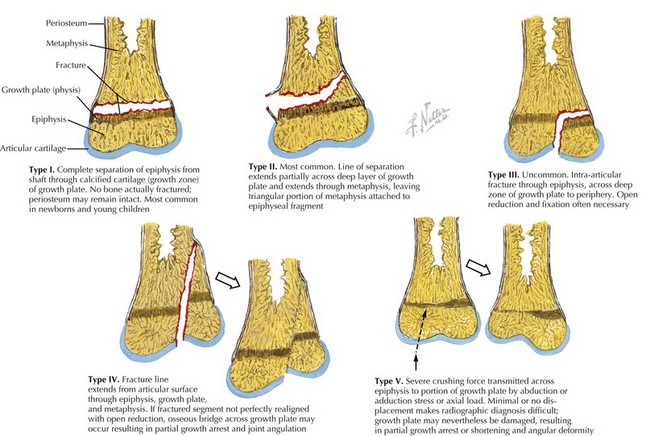
Fractures involving the physis occur frequently in children and account for up to 20% of all pediatric fractures. Although several classification systems for the description of physeal fractures exist, the Salter-Harris classification system is the most widely used. This classification system, based on the radiographic appearance of the fracture, describes the degree of involvement of the physis, epiphysis, metaphysis, and joint and has both prognostic and therapeutic implications (Figure 22-3).
Greenstick Fractures
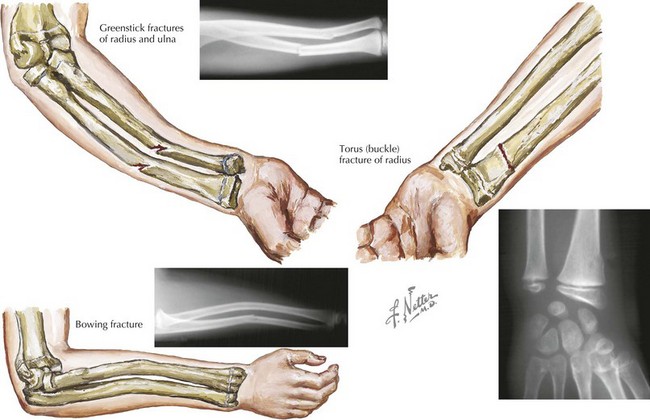
Greenstick fractures are the most common fracture pattern in children. They describe an incomplete fracture of cortex in which the fracture line does not extend completely through the width of the bone. Depending on the degree of angulation, reduction by an orthopedic surgeon may be necessary (Figure 22-4).
Torus Fractures
Torus, or buckle, fractures are common fractures in young children. They result from a compressive load resulting in metaphyseal compaction of trabecular bone and buckling of cortical bone. These fractures are often seen in the distal radius after a fall onto an outstretched hand. As the child matures, the stiffness of the metaphyseal region increases, and the incidence of torus fractures decreases. These fractures are stable and can be managed with simple immobilization for 3 to 4 weeks and orthopedic follow-up (see Figure 22-4).
Bowing Fractures
Bowing fractures represent a plastic deformity of the bone and are unique to children. These fractures occur when a longitudinal force exceeds the bone’s ability to recoil to its normal position and results in a bend in the bone without a fracture. These fractures most commonly involve the radius and ulna. Bowing fractures can sometimes be subtle, and comparison views of the contralateral arm may be necessary. If the deformity occurs in a child younger than 4 years or if the deformation is less than 20 degrees, the angulation usually corrects with growth. However, open reduction may be required for these fractures if they have bowing greater than 20 degrees and the patient is older than 6 years old (see Figure 22-4).
Fractures of the Upper Extremity
Clavicle Fractures
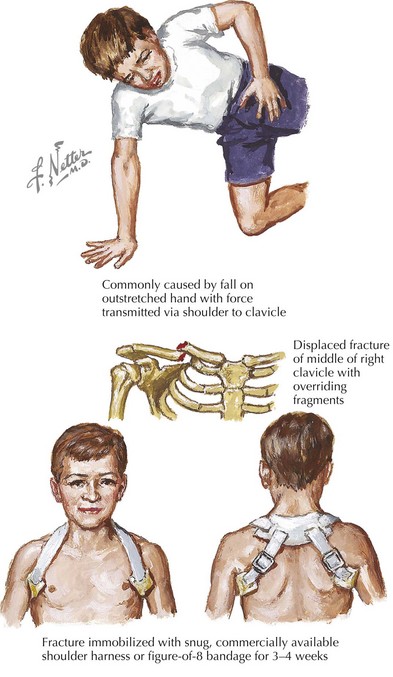
Most clavicle fractures heal well without complication, and management consists of immobilization in a figure-of-8 clavicle strap or sling and swathe. Patients with open fractures, neurovascular or respiratory compromise, significantly displaced midshaft fractures, or grossly unstable distal injuries need orthopedic consultation because closed reduction may be indicated. The vast majority of clavicle fractures heal quickly, usually within 3 to 6 weeks. A bony callus appears during the healing process but disappears with bone remodeling (Figure 22-5).
Fractures of the Humerus
Fractures of the humerus include supracondylar fractures (discussed in the Elbow Fractures section below), proximal humerus fractures, and midshaft fractures. The latter two fractures are relatively rare. Child abuse should be considered when a child younger than 3 years of age presents with a spiral fracture of the humerus.
Elbow Fractures
Anatomy of the Elbow
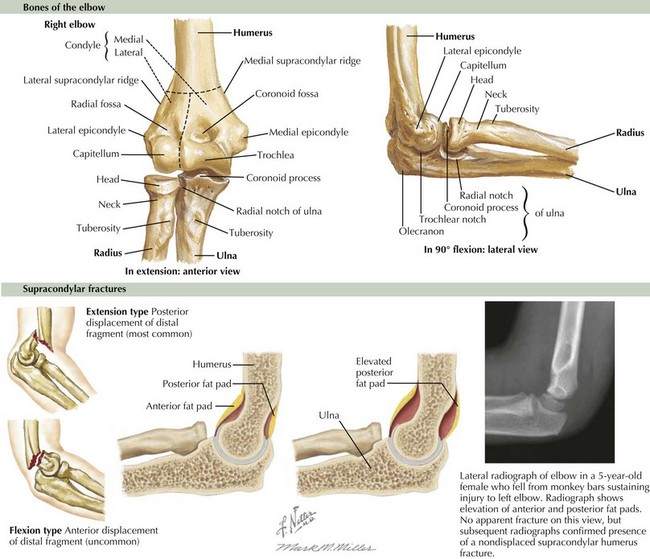
An adequate radiographic evaluation of the elbow consists of an anteroposterior view of the joint in extension and a lateral view with the elbow flexed at 90 degrees (Figure 22-6). When evaluating elbow radiography, it is important to look for abnormalities of the fat pads, the anterior humeral line, and the radiocapitellar line on lateral views of the elbow. There are two elbow fat pads that overly the joint capsule along the distal humerus, one anterior and another posterior. Of the two, only the anterior fat pad is normally visible on a lateral radiograph as a small lucency just anterior to the coronoid fossa. When there is fluid in the joint space, as with a hemarthrosis from a fracture, the fat pads are displaced upward and outward thereby accentuating the anterior fat pad and making the posterior fat pad visible. The posterior fat pad sits deep in the olecranon fossa and is not visible under normal circumstances (see Figure 22-6). The anterior humeral line is also used to identify occult elbow injury. It is drawn along the anterior cortex of the distal humerus on a true lateral view of the elbow and should normally intersect the middle third of the capitellum; displacement may be consistent with a supracondylar fracture. The radiocapitellar line is drawn down the radius and should bisect the capitellum. Failure to do so may suggest an occult radial neck fracture or radial head dislocation.
Supracondylar Fractures
Neurovascular injury is a common complication of supracondylar fractures. Although actual laceration of the brachial artery is rare, the vessel may be compressed or contused or undergo vasospasm at the fracture site, leading to distal ischemia. Patients are also at risk for developing a forearm compartment syndrome, which can lead to Volkmann’s ischemic contracture and a nonfunctional hand and wrist. Neurologic deficits, usually transient, are also common, and radial, medial, and ulnar nerve palsies have all been associated with supracondylar fractures (see Figure 22-6).
Forearm Fractures
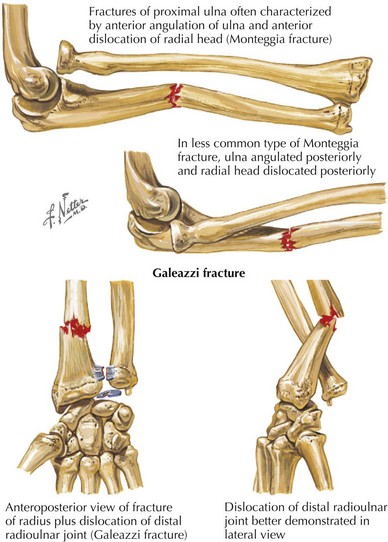
In general, isolated fractures of the ulna are rare. A fracture of the proximal ulna may be associated with concomitant dislocation of the radial head, know as a Monteggia fracture. A fracture at the distal third of the radius in association with distal radioulnar joint dislocation is called a Galeazzi fracture (Figure 22-7). These fractures require closed reduction. Most proximal radius fractures in young children involve the radial neck, usually resulting in Salter-Harris type I and type II radial neck fractures. Proximal radius fractures can occur in conjunction with elbow dislocations and are often associated with medial epicondyle, olecranon, and coronoid process fractures. Nondisplaced or minimally displaced fractures of radial head and neck can often be treated with splinting and orthopedic follow-up. Fractures with a high degree of angulation or displacement may need reduction or surgical repair.
Fractures of the Hand and Wrist
Fractures of the Phalanges
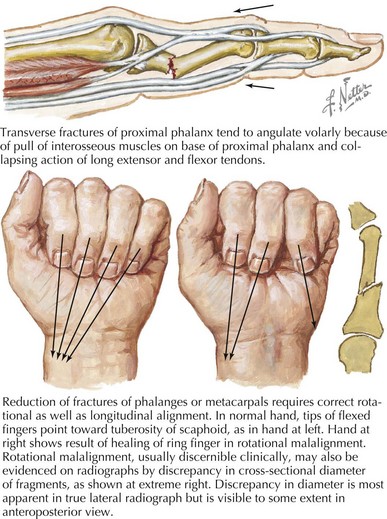
The different phalangeal fracture patterns in children include physeal, diaphyseal, and tuft fractures. Evaluation of the fractured digit should include assessment of the skin integrity, the nail bed, any gross deformity, tendon function, and rotational alignment. The most common fractures of the hand in pediatrics are distal phalanx fractures, or tuft fractures. These are usually crush injuries complicated by lacerations. These injuries are treated with wound care, nailbed repair, and finger splinting. Middle and proximal phalangeal fractures commonly occur at the physis and are usually Salter-Harris type II fractures. When evaluating patients with these fractures, it is important to assess for rotational deformity with the fingers flexed because any malrotation or angular deformity requires closed reduction to preserve hand function (Figure 22-8).
Fractures of the Pelvis and Lower Extremities
Fractures of the Pelvis
Pelvic fractures in children include pelvic ring fractures, avulsion fractures, and acetabular fractures. Pelvic ring fractures are rare in children and involve high-energy accidents. These are discussed in more detail in Chapter 8. Acetabular fractures are also rare in children and are often associated with hip dislocation. Avulsion fractures are described earlier in this chapter and in Chapter 25.
Fractures of the Femur
Femur fractures occur commonly in children. The majority of femur fractures result from low-energy events, such as falls from playground equipment or sports-related injuries. These occur primarily in children age 5 to 10 years old. Femur fractures in children younger than 2 years old should raise concern for nonaccidental trauma (see Chapter 12). Femur fractures can also result from high-energy events such as motor vehicle collisions.
Stress fractures of the femoral neck are becoming increasingly recognized in young athletes. See Chapter 25 for a discussion of these fractures.
Fractures of the Ankle and Foot
Distal Tibial and Fibular Fractures
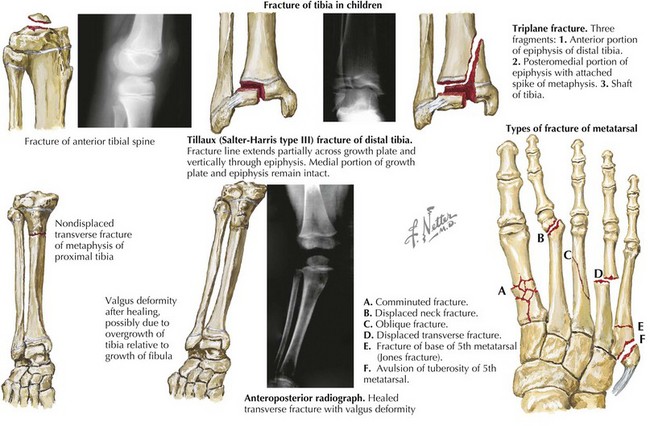
A Tillaux fracture is a Salter-Harris type III injury of the ankle that occurs as the medial distal tibial physis begins to close in adolescents who are nearing skeletal maturity, usually between the ages of 11 and 15 years. Forced external rotation of the foot leading to external rotation of the distal fibula causes the anterior tibiofibular ligament to avulse a piece of the anterolateral tibial epiphysis (Figure 22-9). This injury usually results from low-energy trauma such as in skateboard and baseball sliding injuries. Diagnostic work-up should begin with radiography, but after diagnosis has been made, a CT or MRI scan should be obtained to determine whether the fracture requires closed or open reduction.
Another fracture of the ankle unique to adolescent patients is the triplane fracture, a multiplanar fracture in which the fracture extends through the growth plate (transversely), epiphysis (sagittally), and distal tibial metaphysis (coronally) resulting in a Salter-Harris type IV fracture with three classically described fragments (see Figure 22-9). These fractures also occur in adolescents between the ages of 11 and 15 years before completion of the distal tibial physis closure. As with Tillaux fractures, the diagnostic workup should begin with radiography followed by CT or MRI to delineate the amount of displacement because many of these fractures require operative management.
Fractures of the Foot
Metatarsal and phalangeal fractures are common in children and account for the majority of fractures in children’s feet. Most metatarsal and phalangeal fractures present with pain and swelling, occasionally accompanied by deformity. These injuries should be evaluated radiographically, and most can be treated with bulky splints and crutches. The fifth metatarsal fracture is the most common midfoot fracture. Proximal avulsion fractures of the tuberosity at the base of the fifth metatarsal are very common. They are usually associated with lateral ankle strain and heal well with brief immobilization. It is important to distinguish these fractures from Jones fractures, which can look very similar. Jones fractures are transverse fractures of the fifth metatarsal. Although far less common than avulsion fractures, they are associated with greater morbidity. If unrecognized, they have a high rate of nonunion, which can require bone grafting and internal fixation (see Figure 22-9).
Eiff MP, Hatch RL. Boning up on common pediatric fractures. Contemp Pediatr. 2003;20:30-42.
Fleisher GR, Ludwig S, Henretig FM. Orthopedic trauma. In: Textbook of Pediatric Emergency Medicine. Philadelphia: Lippincott Williams & Wilkins; 2006:1525-1570.
Hart ES, Albright MB, Rebello GN, Grottkau BE. Broken bones: common pediatric fractures—part I. Ortho Nurs. 2006;25(4):251-256.
Hart ES, Grottkau BE, Rebello GN, Albright MB. Broken bones: common pediatric upper extremity fractures—part II. Ortho Nurs. 2006;25(5):311-323.
Hart ES, Luther B, Grottkau BE. Broken bones: common pediatric lower extremity fractures—part III. Ortho Nurs. 2006;25(6):390-407.
Jadhav SP, Swischuk LE. Commonly missed subtle skeletal injuries in children: a pictorial review. Emerg Radiol. 2008;15(6):391-398.
Nofsinger CC, Wolfe SW. Common pediatric hand fractures. Curr Opin Pediatr. 2002;14(1):42-45.
Shrader MW. Pediatric supracondylar fractures and pediatric physeal elbow fractures. Orthop Clin North Am. 2008;39(2):163-171.