Chapter 48 Combined Ventral-Dorsal Surgery
Disorders of the cervical spine can be considered for combined ventral and dorsal surgery in one setting. The indications for these cases may be small in number but when necessary can be technically demanding with associated significant morbidity.1,2 Traditionally, such operations were most appropriate for trauma patients having three-column instability, much like that seen in the thoracolumbar model described by Denis.3 With anterior and posterior ligamentous and osseous disruption, combined ventral and dorsal surgery may provide short- and long-term stability and prevent late kyphotic deformity.4,5
It is clear that a combined operation under a single anesthetic offers savings in blood loss, incidence of wound infections, hospital stay, and total cost.1,2 This chapter summarizes some indications for performing combined surgery, as well as the technical and complicating factors associated with such procedures.
Acute Cervical Spine Injury
Patients who suffer traumatic cervical spine injury will have plain radiographs taken or CT imaging performed. Although these methods can demonstrate osseous injury, ligamentous injury is not accurately depicted. Advanced imaging such as MRI should be considered in the patient who is stable and is being considered for a ventral, dorsal, or combined procedure.6
The three-column framework for managing spinal instability in the thoracolumbar spine can likewise be incorporated in acute cervical spine injury patients.3 Before the use of MRI, Cybulski et al. reviewed the factors that make three-column disruption more likely: (1) disruption of anterior and posterior longitudinal ligaments; (2) dislocation of facets; and (3) disruption of the posterior interspinous ligaments with sufficient force to cause shear dislocation of one vertebra on another.6
Although posterior tension band stabilization procedures can be performed on most reduced cervical fracture-dislocations, Cybulski et al. recommend consideration of circumferential surgery in cases of significant three-column instability. Distractive-flexion or compressive-flexion injuries corrected with posterior fusion were the most likely to need a ventral fusion. These injuries apply horizontal shearing forces that destabilize all three columns.6
In defining the most optimal procedure, most shortcomings arise from a lack of standardized nomenclature or a scoring system.7 Vaccaro et al. proposed a scoring system (subaxial injury classification, SLIC) based on three key features: (1) injury morphology as determined by mechanism of injury from existing imaging studies; (2) integrity of the discoligamentous soft tissue complex (DLC) based on anterior and posterior longitudinal ligamentous structures and the intervertebral disc, and (3) patient neurology (Table 48-1).8 An ideal classification system would be based on fracture pattern, suspected mechanism of injury, spinal alignment, neurologic injury, and prognosis of long-term stability.8 The Vaccaro classification was derived from literature review and surveys done with the Spine Trauma Study Group (STSG, founded in 2004, consisting of 50 surgeons from 12 countries dedicated to improving interpretation and management of traumatic spine conditions). The results demonstrated that DLC is the most difficult to objectify on the basis of low interrater and intrarater intraclass correlation coefficient (ICC). There was a high degree of validity, with 93.3% of raters agreeing on a treatment plan based on the SLIC algorithm.8
| Points | |
|---|---|
| Morphology | |
| No abnormality | 0 |
| Compression | 1 |
| Burst | +1–2 |
| Distraction (e.g., facet perch, hyperextension) | 3 |
| Rotation/translation (e.g., facet dislocation, unstable teardrop, advanced-stage flexion-compression injury | 4 |
| Discoligamentous complex | |
| Intact | 0 |
| Indeterminate (e.g., isolated interspinous widening, MRI signal change only) | 1 |
| Disrupted (e.g., widening of disc space, facet perch, dislocation) | 2 |
| Neurologic Status | |
| Intact | 0 |
| Root injury | 1 |
| Complete cord injury | 2 |
| Incomplete cord injury | 3 |
| Continuous cord compression in setting of neurologic deficit (neuromodifier) | +1 |
Data from Vaccaro AR, Hurlbert RJ, Fisher CG, et al: The sub-axial cervical spine injury classification system (SLIC): a novel approach to recognize the importance of morphology, neurology and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 32(23):2365–2374, 2007.
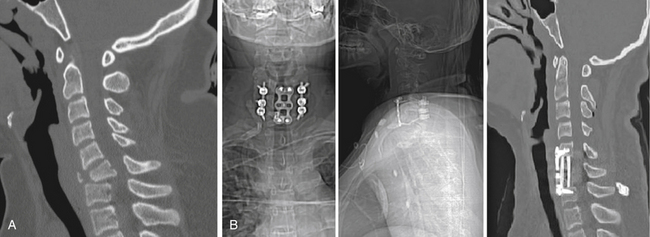
Dvorak et al.7 described an algorithm for deciding the choice of surgical approach on the basis of a systematic review of the literature, as well as opinions of 48 spine surgeons comprising the STSG. On the basis of the scoring system from the SLIC scale, algorithms were created by the STSG. Although many approaches described are for either ventral or dorsal approaches, some algorithms conclude with a combined approach. In distraction injuries with hyperextension injury with or without avulsion fractures, the fusion construct can be addressed ventrally. However, in cases of severe spondylosis, diffuse idiopathic skeletal hyperostosis, or ankylosing spondylitis, the adjacent level stiffness is best neutralized with an additional dorsal approach. For bilateral facet subluxations (perches facets without fracture) there is a higher incidence of kyphosis after posterior fusion alone speculating progressive disc space collapse as a cause for failure. End-plate compression fracture with facet fracture/dislocation almost always requires a combined approach. In those who have a ventral surgery alone, there may be early mechanical failure of the fusion. Severe ventral vertebral body fractures including teardrop fractures and burst-fracture dislocations have posterior element failure as a common feature (Fig. 48-1). These patients are candidates for a combined approach. In unilateral or bilateral facet fracture dislocations (no vertebral body fracture) a posterior approach is often used. However, if prereduction MRI demonstrates a disc fragment displaced into the spinal canal or the patient declines neurologically after closed reduction, a concomitant anterior discectomy, reduction, and fusion approach is recommended.7
Kyphotic Deformity
Cervical kyphosis can occur because of several conditions, including trauma, malignancy, inflammatory disease, infection, spondylosis, and iatrogenic processes. Postlaminectomy kyphosis, or “swan neck” deformity, occurs in approximately 20% of adult patients after multiple cervical laminectomy.9 Risk factors associated with postoperative kyphosis include preoperative loss of cervical lordosis, extent of laminectomy, facet capsule destruction, tumor, and radiation.9 In postlaminectomy kyphosis, a ventral decompression and fusion are associated with significant graft complications and instability. Graft complications can include dislodgement, pseudarthrosis, and acceleration of adjacent level degeneration.10 In advanced disease, further degeneration resulting in foraminal stenosis and subsequent radiculopathy; progressive spinal cord shift to the anterior portion of the spinal canal, resulting in myelopathy; as well as swallowing, breathing, and forward gaze difficulties can be present and are reasons for surgical intervention.11
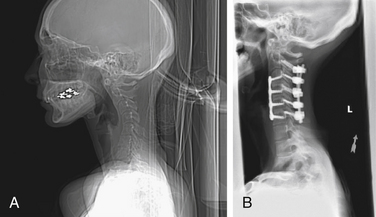
A combined approach has the potential for correction of severe postlaminectomy kyphotic deformity. Various methods of reduction exist. Beginning in a supine position, the patient is intubated, placed in prongs and traction, and positioned in an extended position. A lateral cervical radiograph confirms kyphotic correction. An anterior approach is begun with an anterior cervical discectomy and fusion. The patient is then turned to the prone position. Lateral cervical radiograph confirms stable alignment, and a dorsal fusion with placement of lateral mass screws and rods is performed (Fig. 48-2). Alternatively, Sin et al. describe a ventral-dorsal-ventral, or 540-degree fusion, for correction of nearly 90-degree cervical kyphosis secondary to C5-6 Pseudomonas discitis. In this case, the anterior approach was suboptimal due to scar and inability to reduce the deformity after partial C5-6 corpectomies because of dorsal element fusion from the remote infection. The wound was closed, and a dorsal approach with radical removal of the C5 lamina, posterior facets, and lateral masses was performed. This approach allowed for significant enough reduction posteriorly to proceed with fusion. Sin et al. then returned ventrally and completed the C5-6 corpectomies followed by graft placement and ventral plating.12
Combined ventral and dorsal approaches to correct cervical kyphosis have several advantages. The dorsal osteotomy works synergistically with the return to lordosis offered by ventral osteotomy and reconstruction by shortening the posterior column and lengthening the anterior column. There is also a reduction in stress forces, which reduces the risk of graft migration and pseudarthosis.13
Numerous studies exist on ventral or dorsal approaches for managing kyphotic deformity. However, few reports exist in the literature about combined cervical reconstruction of kyphotic sagittal plane deformity. Few studies demonstrate the amount of preoperative kyphosis, amount of deformity correction, and maintenance of correction. Nottmeier et al. reviewed the charts of patients who underwent 360-degree reconstruction over a 6-year period. Forty-one patients with average follow-up of 19 months had a mean sagittal angle correction of 22 degrees and a mean fusion rate of 97.5%. However, three patients had adjacent segment kyphosis, one of whom required extension of the fusion.11 Mummaneni et al. had a mean follow-up of 2.6 years in 27 patients. Mean Ishihara index values improved from −17.7 to +11.4, demonstrating a significant return to cervical lordosis. They had a 95% fusion rate. The complication rate was 33.3%, none of which were neurologic deficits after surgery. All patients had neuromonitoring (motor evoked potentials, somatosensory evoked potentials, and electromyogram).13 These studies suggest a role of combined approach for cervical kyphotic deformity with a potentially superior fusion rate. The adjacent segment kyphosis and complication rates will need further scrutiny.
Neoplasms
The differential diagnosis for intramedullary spinal tumors includes metastasis, astrocytoma, ependymoma, hemangioblastoma, ganglioglioma, and vascular malformations. Extremely rare cases of schwannoma, lymphoma, lipoma, primitive neuroectodermal tumors, and meningioma have been described.14
The goals of surgery include pain control, neurology preservation, and stable fusion construct, all while maximizing a safe tumor resection. Tumors that invade ventral and dorsal neural elements and cause kyphotic deformity are considered for a combined approach. Patients with a life expectancy greater than 2 years, including those with breast carcinoma and myeloma, should be carefully evaluated for a combined approach that provides multiple areas of stabilization when circumferential tumor destruction has occurred.2
Large cervical neurofibromas extending around the spinal cord can be challenging and should be considered for a combined approach.15 Neurofibromas with extensive paraspinal involvement have a particularly high recurrence rate. In addition, tumor revision cases have longer operation times and higher complication rates.15 Chordomas and giant cell tumors are rare occurrences in the cervical spine. However, both have a high local recurrence rate with subtotal resection. Total spondylectomy (combined ventral and dorsal approach) has been described for both tumors in this region. Furthermore, total spondylectomy with wide surgical margins followed by adjuvant radiation therapy can lead to oncologic cure.16,17
Ankylosing Spondylitis
Ankylosing spondylitis commonly results in kyphotic deformity. Patients have difficulty looking straight ahead and difficulty chewing. Chronic inflammation, inactivity atrophy, and steroid use are all responsible for osteoporosis of the spine in these patients.18 Ankylosing of the facet joints and ossification of the anulus fibrosus and ligaments render the spine stiff.19 The lower cervical spine is most commonly affected during trauma.19
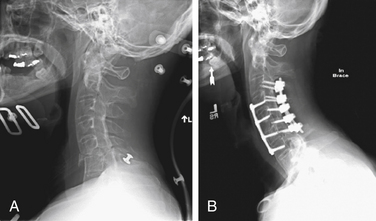
Most cervical fractures in ankylosing spondylitis can be surgically managed with a posterior approach alone. Taggard and Traynelis described their results of posterior instrumentation in a group of seven ankylosing spondylitis patients with cervical fractures. All five patients available at follow-up had 100% fusion. All patients underwent MRI, which evaluated ligamentous injury and epidural hematoma. Epidural hematoma occurs with increased incidence in the ankylosing spondylitis population and can contribute significantly to neurologic deficit. Each patient underwent lateral mass plating at least two segments above and below the level of injury. Due to the extensive fusion that occurs in ankylosing spondylitis, facets may be indistinguishable and can make screw placement difficult. The authors recommend screws of less than 14 mm to avoid nerve root injury. In addition, at C7 and below the authors use a medial trajectory for pedicle incorporation and neural avoidance. None of these cases had significant enough anterior column fracture to warrant an additional ventral approach.20 However, when there is concern about inadequate anterior column support or kyphotic deformity at the fracture site, a combined approach should be considered (Fig. 48-3).
Payer presented his results of four patients managed with a combined ventral and dorsal approach. All patients had transverse fractures at the C6-7 disc level with varying degrees of lordotic opening (8 to 35 degrees). Except for a single case, all patients were managed with posterior fixation three levels above and below followed by anterior single-segment corpectomy and fixation. This patient had a C6-7 level disc transverse fracture with a 38-degree lordotic opening and an 11-mm anterior sagittal gap, ventral epidural hematoma, and cord compression. A ventral approach reduced the lordosis to 26 degrees. Six days later there was back-out of the plate, suggesting inadequate biomechanical construct from a ventral approach alone. Dorsal fixation followed by ventral refixation was performed. All patients had stable fusion constructs during the postoperative observation periods of 6 to 18 months.19
Cervical Spondylotic Myelopathy
Cervical spondylotic myelopathy is a progressive degeneration of the cervical spine associated with disc height loss and facet and uncovertebral joint motion abnormalities. Uncovertebral joint disease leads to disc herniation and osteophyte formation leading to ventral stenosis. Facet disease and dorsal ligamentous hypertrophy lead to dorsal and lateral recess stenosis. The natural history is one of progressive circumferential spinal stenosis resulting in neurologic decline. Ventral and dorsal approaches alone have been performed for cervical spondylotic myelopathy with varying results in fusion, clinical improvement, and adjacent segment motion. In some cases a combined approach may be favorable for adequate decompression of both ventral and dorsal elements causing stenosis.10
In patients needing more than two-level corpectomy, the rate of failure has been shown to dramatically increase.21 Thirty-three patients underwent two-level corpectomy and fusion compared with seven with three-level corpectomy and fusion. The two-level group had two failures (6%) manifesting as pseudarthrosis. The three-level group had five failures (71%) involving graft dislodgement, which were more serious in nature. Three of the patients with three-level and subsequent failure underwent posterior fusion and have all done well. The addition of dorsal instrumentation biomechanically moves the instantaneous axis of rotation dorsally, thus preserving the graft during extension.21 Vaccaro et al. also noted unacceptably high failure rates for three-level versus two-level anterior cervical corpectomy and fusion (50% vs. 9%, respectively).22 Thus circumferential surgery should be considered in patients undergoing long-segment corpectomy reconstruction.
Recently, Mummaneni et al. performed a systematic literature review and evidence-based medicine to describe the efficacy of various anterior and posterior cervical approaches for the treatment of cervical spondylotic myelopathy. Anterior cervical discectomy and fusion (ACDF) and cervical corpectomy and fusion (ACCF), laminoplasty, laminectomy, and laminectomy with fusion have improved functional outcomes. ACDF and ACCF have similar results in multilevel spine decompression for the same level lesion. With anterior plating they have equivalent fusion rates. Without anterior fixation, ACCF may have better fusion rates but also higher graft complication rates than multilevel ACDF (class III). There exists class III evidence for late deterioration with laminectomy compared with laminectomy with arthrodesis. Manuscripts reviewed by the authors were deemed class III evidence for several reasons, including absence of a control group, nonblinded allocation of a control group, nonvalidated outcome measures, and unblinded outcome assessors.23 The importance of a prospective, randomized, controlled clinical trial is validated by the equivalent outcomes with these procedures without good class I or II evidence.
There may be a subgroup of patients who would benefit from a combined ventral and dorsal approach. Acosta et al. studied the biomechanical stability and clinical results of anterior cervical fusion level 3 or higher and circumferential reconstruction using titanium mesh cage (TMC) and dorsolateral fixation. They had 15 patients with cervical spondylotic myelopathy. Each patient had a halo ring secured to a Mayfield frame. Corpectomy and decompression (including posterior longitudinal ligament) was performed. Corpectomy bone was harvested and packed into an appropriate-size TMC. All TMCs had a lordotic curvature. Cervical traction was applied by anesthesia, TMC was inserted, and finally traction was relieved. An anterior plate was inserted in each case. The patient was then turned prone, and posteriolateral screw-rod fixation was performed at least one level above and below the corpectomy. Average follow-up was 33 months. There was a 100% fusion rate, and there was no significant cage subsidence or case of instrument failure.24
Summary
Combined ventral and dorsal cervical spine surgery can be technically difficult with high morbidity. Cervical spine trauma, malignancy, ankylosing spondylitis, kyphosis deformity, and cervical spondylitic myelopathy are all pathologies for which a combined approach may be biomechanically advantageous. Predicting which patients will benefit from this combined approach can potentially improve fusion rates, prevent delayed deformities, decrease hospital readmissions, and thereby be more cost-effective.
Dvorak M.F., Fisher C.G., Fehlings M.G. The surgical approach to subaxial cervical spine injuries: an evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976). 2007;32:2620-2629.
Mummaneni P.V., Dhall S.S., Rodts G.E., Haid R.W. Circumferential fusion for cervical kyphotic deformity. J Neurosurg Spine. 2008;9:515-521.
Mummaneni P.V., Kaiser M.G., Matz P.G., et al. Cervical surgical techniques for the treatment of cervical spondylotic myelopathy. J Neurosurg Spine. 2009;11:130-141.
Nottmeier E.W., Deen H.G., Patel N., Birch B. Cervical kyphotic deformity correction using 360-degree reconstruction. J Spinal Disord. 2009;22:385-391.
Vaccaro A.R., Cook C.M., McCullen G., Garfin S.R. Cervical trauma: rationale for selecting the appropriate fusion technique. Orthop Clin North Am. 1998;29:745-754.
Vaccaro A.R., Hurlbert R.J., Fisher C.G., et al. The sub-axial cervical spine injury classification system (SLIC): a novel approach to recognize the importance of morphology, neurology and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976). 2007;32:2365-2374.
Witwer B.P., Trost G.R. Cervical spondylosis: ventral or dorsal surgery. Neurosurgery. 2007;60(Suppl 1):S130-S136.
1. Dick J., Boachie-Adjei O., Wilson M. One-stage versus two-stage anterior and posterior spinal reconstruction in adults. Comparison of outcomes including nutritional status, complication rates, hospital costs, and other factors. Spine (Phila Pa 1976). 1992;17(Suppl 8):S310-S316.
2. McAfee P.C., Bohlman H.H., Ducker T.B., et al. One-stage anterior cervical decompression and posterior stabilization. A study of one hundred patients with a minimum of two years of follow-up. J Bone Joint Surg [Am]. 1995;77(12):1791-1800.
3. Denis F. Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin Orthop. 1984;189:65-76.
4. McNamara M.J., Devito D.P., Spengler D.M. Circumferential fusion for the management of acute cervical spine trauma. J Spinal Disord. 1991;4(4):467-471.
5. Vaccaro A.R., Cook C.M., McCullen G., Garfin S.R. Cervical trauma: rationale for selecting the appropriate fusion technique. Orthop Clin North Am. 1998;29(4):745-754.
6. Cybulski G.R., Douglas R.A., Meyer P.R.Jr., Rovin R.A. Complications in three-column cervical spine injuries requiring anterior-posterior stabilization. Spine (Phila Pa 1976). 1992;17(3):253-256.
7. Dvorak M.F., Fisher C.G., Fehlings M.G. The surgical approach to subaxial cervical spine injuries: an evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976). 2007;32(23):2620-2629.
8. Vaccaro A.R., Hurlbert R.J., Fisher C.G., et al. The sub-axial cervical spine injury classification system (SLIC): a novel approach to recognize the importance of morphology, neurology and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976). 2007;32(23):2365-2374.
9. Deutsch H., Haid R.W., Rodts G.E., Mummaneni P.V. Postlaminectomy cervical deformity. Neurosurg Focus. 2003;15(3):E5.
10. Witwer B.P., Trost G.R. Cervical spondylosis: ventral or dorsal surgery. Neurosurgery. 2007;60(Suppl 1):S130-S136.
11. Nottmeier E.W., Deen H.G., Patel N., Birch B. Cervical kyphotic deformity correction using 360-degree reconstruction. J Spinal Disord Tech. 2009;22(6):385-391.
12. Sin A.H., Acharya R., Smith D.R., Nanda A. Adopting 540-degree fusion to correct cervical kyphosis. Surg Neurol. 2004;61(6):515-522.
13. Mummaneni P.V., Dhall S.S., Rodts G.E., Haid R.W. Circumferential fusion for cervical kyphotic deformity. J Neurosurg Spine. 2008;9:515-521.
14. Waldron J.S., Cha S. Radiographic features of intramedullary spinal cord tumors. Neurosurg Clin North Am. 2006;17:13-19.
15. Jiang L., Lv Y., Liu X.G., et al. Results of surgical treatment of cervical dumbbell tumors: surgical approach and development of an anatomic classification system. Spine (Phila Pa 1976). 2009;34(12):1307-1314.
16. Currier B.L., Papagelopoulos P.J., Krauss W.E., et al. Total en bloc spondylectomy of C5 vertebra for chordoma. Spine (Phila Pa 1976). 2007;32(9):E294-E299.
17. Junning M., Cheng Y., Dong C., et al. Giant cell tumor of the cervical spine: a series of 22 cases and outcomes. Spine (Phila Pa 1976). 2008;33(3):280-288.
18. Olreud C., Frost A., Bring J. Spine fractures in patients with ankylosing spondylitis. Eur Spine J. 1996;5:51-55.
19. Payer M. Surgical management of cervical fractures in ankylosing spondylitis using a combined posterior-anterior approach. J Clin Neurosci. 2006;13:73-77.
20. Taggard D.A., Traynelis V.C. Management of cervical spinal fractures in ankylosing spondylitis with posterior fixation. Spine (Phila Pa 1976). 2000;25(16):2035-2039.
21. Sasso R.C., Ruggiero R.A.Jr., Reilly T.M., Hall P.V. Early reconstruction failures after multilevel cervical corpectomy. Spine (Phila Pa 1976). 2003;28(2):140-142.
22. Vaccaro A., Falatyn S., Scuderi G., et al. Early failure of long segment anterior cervical plate fixation. J Spinal Disord. 1998;11:410-415.
23. Mummaneni P.V., Kaiser M.G., Matz P.G., et al. Cervical surgical techniques for the treatment of cervical spondylotic myelopathy. J Neurosurg Spine. 2009;11:130-141.
24. Acosta F.L., Aryan H.E., Chou D., Ames C.P. Long-term biomechanical stability and clinical improvement after extended multilevel corpectomy and circumferential reconstruction of the cervical spine using titanium mesh cages. J Spinal Disord Tech. 2008;21:165-174.