CHAPTER 11 Cognitive and Adaptive Disabilities
PURPOSE
The direct and indirect economic costs associated with mental retardation in the United States are significant: $51.2 billion (2003 dollars) for persons born in 2000.1 The proportion of school-aged children classified as having “mental retardation” and receiving services in federally funded educational programs in the United States has stabilized since the early 1990s between 1.26% and 1.28%.2 The Centers for Disease Control and Prevention currently estimate that mental retardation is diagnosed in 12 per 1000 U.S. school-aged children; the result in annual special education costs is $3.3 billion.
TERMINOLOGY DEBATE
The terminology used to describe mental retardation has changed since the 19th century, reflecting an increased sensitivity to the rights of and opportunities for persons with mental retardation, an increased effort to mainstream individuals with mental retardation into society to improve their quality of life, and a decreased tolerance for stigmatizing and limiting “labels” that focus on the disability rather than on the individual. The terms imbecility and idiocy were used in the late 19th century to describe different levels of intellectual functioning on the basis of decreasing language and speech abilities. Less affected individuals were referred to as being “feeble-minded.” At that time, the outcome for individuals with mental retardation was believed to be predetermined; their ability to participate in everyday activities and within typical environments was limited. In the mid-20th century, terms such as trainable and educable were used to characterize persons with mental retardation, often to suggest what type of educational experience was most appropriate. Newer educational interventions that emphasize mainstreaming have reversed this focus on limiting participation and minimizing progress. What has remained, however, is the need to distinguish between a label, the specific difficulties faced by an individual with that label, and the social judgments associated with that label.3 Effective differentiation between the label and the individual and advocacy for the integration of these children and their families into every aspect of society is an essential responsibility of developmental-behavioral pediatricians and every other member of the multidisciplinary teams providing their care.
There are numerous negative connotations associated with the term mental retardation. There is no agreement on a more preferred term at either the international or national level. Other terms that have been proposed include intellectual disability/disabilities, developmental disabilities, mentally challenged, and cognitive adaptive disability or delay. In the United Kingdom, the term learning disability is used, whereas intellectual disability is preferred in Japan and is increasingly the label of choice among the international community.4
As it prepared to revise its 1992 definition for mental retardation, the American Association on Mental Retardation (AAMR) asked for comments and recommendations for an alternative term that would better describe these individuals. One strongly considered proposal was cognitive adaptive disability. Interestingly, this evolving discussion of a “best” or “better” term eventually led to a change in the name of the President’s Committee on Mental Retardation to the President’s Committee on Intellectual Disability. There are very strong arguments that any other term selected to describe this group of individuals will quickly assume similar negative connotations. It is also important to realize that what is “acceptable” to professionals may not be so readily accepted by affected individuals and their families. There have also been concerns that changing the term used to describe these individuals might adversely affect their eligibility for services specifically defined in statute for “persons with mental retardation” (supplemental Social Security payments) and for unique legal protections provided by this diagnosis (death penalty exclusions). The debate over the correct terminology for this condition continues. In January 2007, the American Association on Mental Retardation (AAMR) officially changed the organization’s name to the American Association on Intellectual and Developmental Disabilities (AAIDD). Although they recognize that the condition “mental retardation” they have defined for over 100 years still exists, the AAMR/AAIDD leadership feels that this change is “an idea whose time has come.”
DEFINITION AND CRITERIA
A state of mental defect from birth, or from an early age, due to incomplete cerebral development, in consequence of which the person affected is unable to perform his duties as a member of society in the position of life to which he is born.5
There are two generally well-accepted organizational definitions of mental retardation: the AAMR’s and the American Psychiatric Association’s as described in the Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision (DSM-IV-TR) (Table 11-1).5,6 The two schemes have common elements: the use of standardized measures of intelligence and adaptive abilities to define levels of significant subaverage intellectual and adaptive functioning and evidence of the disability’s presence before 18 years of age. In current definitions, mental retardation is no longer described as a state of “global incompetence.” Instead, they refer to an overall pattern of limitations and describe how individuals typically, not ideally, function in various contexts of their everyday life.
| Feature | AAMR, 2002 | DSM-IV-TR |
|---|---|---|
| Intellectual functioning | Significant limitations in intellectual functioning |
AAMR, American Association on Mental Retardation5; DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders, 4th ed, text revision (American Psychiatric Association6).
In discussions with families, it is very important to remember that cognition, intelligence, and IQ are not synonymous terms; confusion and disagreement often occur when they are used interchangeably. Intelligence is a combination of the ability to learn and to pose and solve problems.7 Various schemas for intelligence have been proposed with complementary and overlapping features.
Levels of Mental Retardation
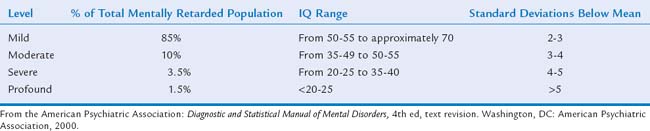
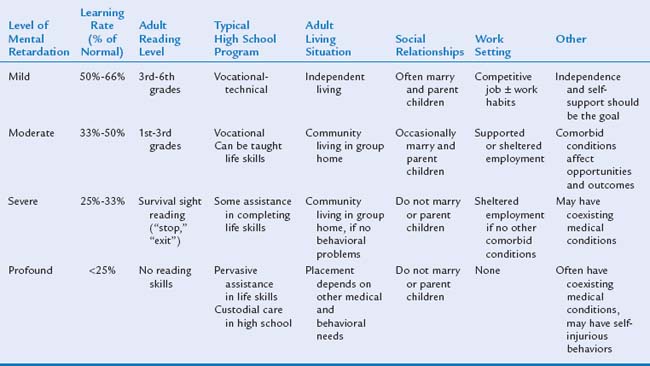
In the traditional classification schema, continued in the DSM-IV-TR system, the number of standard deviations below the mean is its basis (Table 11-2). There are both advantages and disadvantages to this schema. It is often preferable for research purposes because of its ability to better define a “homogeneous” population. However, the fact that a numerical “score” from a standardized measure of intelligence may vary by as much as 5 points higher or lower (95% confidence interval) still limits the effectiveness of a specific score as a method of differentiation across severity levels. In other schemas, particularly for epidemiological analyses, an IQ cutoff score of 50 is used to differentiate between “mild” and “severe” mental retardation.8 The reason for this division was to define and describe individuals who would benefit from a formal/academic education program (mild) from those who would benefit more from a life skills education program (severe). Likewise, the same differentiation could be applied to individuals who would be able to live independently (mild) from those more likely to need a guardian and additional supervision (severe).
Levels of Support
The 1992 edition of AAMR’s definition of mental retardation introduced a significant change in the organizational and descriptive approach to individuals with mental retardation: the concept of “levels of support.” AAMR further developed this concept and proposed the current definition in 2002: “Supports are resources and strategies that aim to promote the development, education, interests and personal well being of a person and that enhance individual functioning.”5
The supports approach purpose is to evaluate the specific needs of the individual and then suggest strategies, services, and supports that will optimize individual functioning across the various dimensions of intellectual functioning. These resources and strategies can be the result of a person’s own efforts or help from other individuals (natural sources), or it can be the result of additional technology, agencies, or service providers (service-based sources). The goal of these interventions is to improve personal functioning, promote self-determination and societal inclusion, and improve the personal well-being and functional abilities and outcomes of a person with mental retardation. In many ways, this method parallels the evolving attention to not only the cognitive and adaptive limitations but also the specific abilities of an individual.5 In an effort to provide a comprehensive assessment, an evaluation is recommended in at least nine key areas: human development, teaching and education, home living, community living, employment, health and safety, behavior, social function, and protection and advocacy. Within these areas, such supports as teaching, befriending, financial planning, employee assistance, behavioral support, in-home living assistance, community access and use, and health assistance may be required. The level of support method recognizes that an individual’s needs and circumstances change over time and are influenced by an individual’s environment. Supports are dynamic.
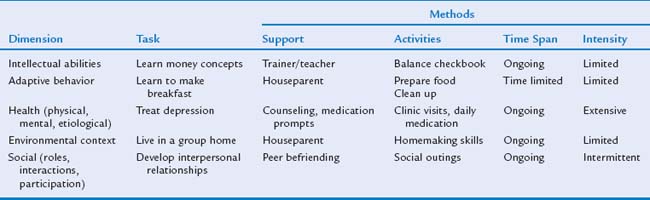
As a support schema is developed, two additional characteristics must be considered: support dimensions and support intensity. Five dimensions of intellectual ability in which an individual may require additional support have been identified (Table 11-3). Each individual has different needs and therefore requires different supports in each of these dimensions. The intensity, frequency, and acuity of what an individual requires in support are also not uniform across these various dimensions (Table 11-4).
| Intellectual abilities | Communication, functional academics, vocational skills |
| Adaptive behavior | Self-care, home living, integrated vocational opportunities |
| Social roles, participation, interactions* | Community living, friendships, self-esteem, social skills, leisure activities |
| Health concerns (physical, mental, etiological) | Etiology and conditions related to biological processes; comorbid disorders |
| Context considerations | Environments, cultures |
From American Association on Mental Retardation. In Luckasson RA, Schalock RL, Spitalnik DM, et al, eds: Mental Retardation: Definition, Classification, and Systems of Support, 10th ed. Washington, DC: American Association on Mental Retardation, 2002, pp 99-121.
TABLE 11-4 Support Intensity Levels
| Intermittent |
*New dimension as of 2002.
From American Association on Mental Retardation. In Luckasson RA, Schalock RL, Spitalnik DM, et al, eds: Mental Retardation: Definition, Classification, and Systems of Support, 10th ed. Washington, DC: American Association on Mental Retardation, 2002, pp 145-168.
The most recent evolution in this method is the AAIDD’s development of the Supports Intensity Scales.9 This instrument provides a direct assessment of the support needed on an individual basis that is not inferred from a “score” derived from other instruments whose norms are based on the general population and not specifically on individuals with disabilities.10
Prevalence
The statistical prevalence of mental retardation is approximately 2% to 3%, although the actual prevalence may be closer to 1%. The estimate varies according to the particular study, specific ascertainment methods, the age of the cohort being studied (lower prevalence among subjects aged <5 years and >18 years—i.e., non-school-aged cohorts), and the level of impairment. Multiple studies and surveys have demonstrated that specific populations are overrepresented; the label “mental retardation” is more likely to be applied to individuals of lower socioeconomic status, ethnic groups, and cultural minority groups; those in institutions; and those with related conditions (cerebral palsy, spina bifida, autism).11–13 The prevalence of severe mental retardation (IQ < 50) has remained stable at approximately 0.4% to 0.5%; it is much more likely to be associated with organic disorders and causes. Because of the more variable upper diagnostic limits, the prevalence of mild mental retardation (IQ of 50 to ≤70-75) is more difficult to ascertain. Nevertheless, the vast majority (approximately 85%) of persons with mental retardation have IQ scores in the “mild” range.
ETIOLOGY
Risk Factors in Mental Retardation
Studies of intelligence with standardized IQ measures have produced evidence for a significant genetic influence, although experience and environment also influence this innate ability: 50% of the IQ test score variation can be attributed to genetic variation.14 Heritability estimates for general intelligence appear to be approximately 0.45 to 0.75; longitudinal studies have shown this factor to increase steadily from infancy through adulthood.15 Different genes may play a role, each with a varying degree of effect (quantitative trait loci).15 Children with birth defects are 27 times more likely to have mental retardation by 7 years of age than are children without a diagnosed birth defect, regardless of the type of defect.16
Different risk factors for mild and severe levels of mental retardation are known. Sameroff and associates17 found that the presence of multiple risk factors at age 4 were an important predictor of children’s IQ at age 13. The cumulative effect of multiple risk factors can have an adverse effect on academic success from 1st through 12th grade, overcoming any bolstering effect of intelligence and positive mental health.18 Low maternal education level continues to be the strongest predictor of mild mental retardation. Women with less than 12 years of schooling are more likely to have a child with a mental retardation placement in school than are mothers with some degree of postsecondary education.19 Women with only high-school diplomas still have an increased, albeit lower, risk. Numerous studies have demonstrated an increased risk for isolated severe mental retardation in boys and men (1.4:1) and in nonwhite populations (2:1).20 Therefore, both nature and nurture play important roles in cognitive development. Genetics appears to provide the cognitive potential that is then shaped and developed by environmental and self-selected experiences that further modify a person’s behavior.
Etiological Diagnosis of Mental Retardation
Efforts to identify specific causes of mental retardation are driven by the hope that defining a cause will improve the ability to prevent mental retardation from that cause. However, an etiological diagnosis is made in less than one half of individuals with mental retardation.21 A major challenge in defining an etiology for mental retardation remains in characterizing the contribution and interaction of various socioeconomic factors and other factors in association with prenatal, perinatal, and postnatal events. The number of cases attributed to specific diagnostic categories varies according to the degree of mental retardation, patient selection criteria (including age of the patient), study protocols, technological advances over time, and definitions of diagnoses.22 Because of these issues, classification systems based only on timing or etiology, although more frequently used, may be incomplete. Moog23 proposed a “dynamic classification system” that distinguishes among genetic, unknown, and acquired causes with additional consideration to the degree of diagnostic certainty.
“Diagnostic uncertainty” has a significant effect on families and their ability to cope with the stresses associated with a child having mental retardation. In one comparison of levels of anxiety, feelings of guilt, and emotional burdens of mothers of children with Down syndrome and mothers of children with an undefined reason for their mental retardation, the latter group was found to be at a significant psychoemotional disadvantage.24 Therefore, defining an etiology goes beyond identifying recurrence risk and intervention planning; the process and its outcome may provide a significant emotional support to that family by addressing issues of guilt and in establishing connections with other similarly affected families through support groups.
MOST COMMON IDENTIFIABLE ETIOLOGIES
The three most common identifiable causes of mental retardation are fetal alcohol syndrome (FAS), the fragile X syndrome, and Down syndrome. In individual children with FAS, IQ measures range from 20 to 120, with a mean of 65.25 In comparison, IQ scores of affected male patients with the fragile X syndrome range from 25 to 65, and those of children with Down syndrome range from 40 to 60.26,27
Fetal Alcohol Syndrome
FAS is the most common preventable, nongenetic cause of mental retardation.28 Mental retardation is the abnormality most often associated with the diagnosis of FAS. Estimates of birth prevalence vary among countries. The critical period for alcohol exposure appears to be in the initial 3 to 6 weeks of brain development. The term fetal alcohol spectrum disorders has been suggested to describe the range of impairments in this disorder.29 Other terms such as fetal alcohol effects, prenatal alcohol effects, and alcohol-related neurodevelopmental disabilities or birth defects have been proposed.29 There is no reliable biological marker for FAS. Therefore, the diagnosis is based on clinical criteria that include evidence of prenatal and postnatal growth deficiency, characteristic facial features, and central nervous system anomalies and/or dysfunction.30 Although a history of maternal alcohol use during the pregnancy should be present, exposure is frequently underreported. The differences in growth and facial features vary with the patient’s age and ethnicity.25 Multiple efforts have been made at establishing a paradigm or tool to evaluate and diagnose these affected children, including the Institute of Medicine’s criteria for FAS/fetal alcohol effects published in 199628 and the four-digit system proposed by Astley and Clarren.31
In comparison with other individuals with an identifiable cause of mental retardation, FAS-affected children are at an increased risk for behavioral and psychiatric disorders. Children with FAS exhibit early deficits in measures of attention, learning, executive functioning, and visual-spatial processing. Their social abilities often plateau at the 6-year-old level. Individuals with FAS/fetal alcohol effects demonstrate significant problems with adaptive behavior, which continue into adulthood. One of the strongest correlates with this adverse outcome was the lack of an early diagnosis.32 Young adults with FAS and normal IQs (>70) demonstrate deficits in the areas of attention, verbal learning, and executive function that are more severe than suggested by IQ alone. FAS-affected children with normal IQ scores may still have significant neurobehavioral and adaptive deficits. Some of these behavioral issues may be complicated by the association between several forms of hearing loss and FAS: delays in auditory maturation, sensorineural hearing loss, and intermittent hearing loss secondary to chronic serous otitis media.
Fragile X Syndrome
The fragile X syndrome (also see Chapter 10B for more information) is the most common inherited form of mental retardation and has been identified in every racial and ethnic group studied. It is the leading cause of inherited mental retardation, affecting approximately 50,000 persons in the United States alone (prevalence, 1 per 4000 boys and men, 1 per 6000 girls and women). X-linked factors are believed to be responsible for 10% to 12% of mental retardation in boys and men.33 Fragile X represents the most common (15% to 25%) of the numerous loci identified on the X chromosome that are associated with mental retardation. The fragile X syndrome is the result of an expansion of an unstable cytosine-guanine-guanine (CGG) repeat within the FMR1 gene at Xq27.3. The reason for this expansion is unknown. Four allele patterns have been defined: normal (6 to 50 repeats), intermediate/“gray” (45 to 50), permutation (55 to 200) and full mutation (>200). Once the expansion reaches 200 repeats, the entire FMR1 gene region is methylated (silenced) and FMR1 protein is not produced. It is the absence of FMR1 protein that leads to the characteristic cognitive and clinical features of the syndrome.34
The cognitive profile in the fragile X syndrome is similar in both affected male and female patients, with observed weaknesses in the areas of short-term memory for complex sequential information, visual-spatial skills, planning, and verbal fluency. Many of these areas are often subsumed under the term executive functioning.35 In the fragile X syndrome, the social deficits that make up part of the full mutation phenotype range from autistic features to social anxiety and pragmatic language deficits. As many as 25% to 35% of individuals with full mutations meet diagnostic criteria for autism.36
Boys and men with the full mutation usually exhibit moderate to severe intellectual impairment, characteristic language disorders (cluttering; stronger receptive than expressive skills), and social and behavioral difficulties, including problems with attention, impulsivity, anxiety, social avoidance, and arousal. There does not appear to be any relationship between the number of CGG repeats and IQ score in boys and men with the full mutation. Boys and men with the fragile X syndrome exhibit a decline in cognitive, language, and adaptive skills measures during the school years. A specific cause of this decline is not known.26
Approximately 30% to 50% of girls and women with the full fragile X mutation have IQ scores in the mental retardation range. In addition, they often exhibit a characteristic behavioral phenotype of extreme shyness and decreased eye contact. The remaining female patients may present with borderline to normal intellectual functioning, learning disabilities related to executive functioning, and/or other psychosocial difficulties. There does appear to be a relationship between IQ score and chromosome X activation scores and between IQ score and FMR1 protein levels in affected women.37
The ability to identify children with the fragile X mutation through genetic testing is of particular benefit to physicians and families. DNA studies for the fragile X syndrome have been readily available since 1991 and should be strongly considered in every affected child, boy or girl, in whom the cause of mental retardation is unknown. Despite the availability of this technology, the average age at diagnosis in boys with the fragile X syndrome is 3 years; it is even later in girls.38 In a survey of 274 families with a child with the fragile X syndrome, a number of variables affected making the diagnosis of the syndrome in a timely manner.38 As is the case in other cause of developmental delay, there is often a lag between when the parent expresses concern and when the professional agrees that there is a problem. More than one half of the families expressing a concern about their child were told to “wait and see; he might improve” or that their child was developing normally. In families with affected children born after 1991, the average time between the parent’s first concern and the ordering of the fragile X test was 18 months. More than 50% of the families had already had another child before the diagnosis of fragile X syndrome was made.38 Although some authorities have argued for its implementation, the fragile X syndrome does not meet the traditional criteria for neonatal screening, because an identifiable intervention that could change the course of the disorder does not exist.
Down Syndrome
Down syndrome occurs in 1 per 800 live births and 1 per 1000 conceptions and is the most common genetic disorder causing mental retardation. It is usually readily identified at or near birth by characteristic physical features: hypotonia, hyperflexibility of joints, flat facial profile, slanted palpebral fissures, poor Moro reflex, excess skin on the back of the neck, abnormal ears, dysplasia of the midphalanx of the fifth finger, and a single palmar crease. Other frequently associated conditions include congenital heart disease (40%) and gastrointestinal abnormalities (5%).39 There exist artistic representations of persons with Down syndrome from as early as 500 A. D. Because no combination of these features is specific to Down syndrome, the diagnosis is confirmed by routine chromosome analysis; three abnormalities are possible. The most common finding on chromosomal analysis is a true trisomy for chromosome 21 (in 95% of affected patients); unbalanced robertsonian translocations (3% to 4%), and mosaicism (1% to 2%) account for the other affected individuals. Triplication of a specific region of the long arm of chromosome 21 (21q22.2) is sufficient to produce the clinical phenotype.40 Although there are many similarities in this group, individual variation must also be recognized. The range of outcome can be quite broad. Most affected patients have mild to moderate mental retardation. Mental retardation in children with Down syndrome is not an “across-the-board” phenomenon; thus, there are strengths, as well as deficits.
The profile of cognitive impairment in Down syndrome appears to differ from that of other forms of mental retardation. In much of the work involving children with Down syndrome, investigators have studied their language difficulties, especially in the areas of phonological, grammar, and syntactic skills. Expressive language skills are often more delayed than are cognitive and receptive language skills.40,41 There is also strong evidence that these patients have specific difficulties in other areas of learning and memory, such as poor verbal working memory. Affected individuals show relative strengths in visual motor skills. Although children with Down syndrome continue to learn new skills, they appear to be subject to instability of acquisition and rapid forgetting. Their rate of learning is not only delayed but appears to follow a different path.42 The measured IQ of individuals with Down syndrome typically declines through the first 10 years of life, reaching a plateau in adolescence that continues into adulthood.43,44 These functional deficits may be explained by differences in the hippocampal and prefrontal cortex regions of their brains.
Although fetal brains of individuals with Down syndrome are normal, they do not develop the increasing dendritic complexity or number seen in unaffected individuals.42 Delayed myelination of these structures is seen in 25% of children with Down syndrome. Anatomical studies have demonstrated neuropathological changes earlier than in the general population. Some of these changes are similar to those seen in association with Alzheimer disease. However, although 100% of individuals with Down syndrome eventually exhibit these changes, only 50% have clinical evidence of the associated dementia.42 Individuals with Down syndrome have behavioral and psychiatric problems but often less frequently than children with other types of mental retardation.40 From childhood and into adolescence, the most frequent problems are disruptive behavior disorders, including attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder. Approximately 5% to 10% also meet criteria for autism.45 As adults, individuals with Down syndrome are more likely to have a major depressive disorder or demonstrate aggressive behaviors.46
TIMING OF CAUSE
Prenatal
Most cases of mental retardation have prenatal causes: 70% of cases of severe mental retardation and 51% of cases of mild mental retardation.47 Children with birth defects, regardless of the type of defect, are significantly more likely to be identified with mental retardation than are children without birth defects; the risk tends to be the highest among children with central nervous system and heart defects.16 Environmental exposures during the prenatal period (e.g., to alcohol) and intrauterine infections (e.g., cytomegalovirus) also contribute to the overall incidence of mental retardation. Placental insufficiency for any variety of reasons may result in fetal malnutrition and subsequent intrauterine growth retardation; in the most significant cases of intrauterine growth retardation, affected infants demonstrate evidence of microcephaly at birth.
Perinatal
Individuals in this group are most often affected by the sequelae of low birth weight (<2500 g) and prematurity (<37 weeks of gestation). These complications represent about 4% of identifiable causes of severe mental retardation and 5% of identifiable cases of mild mental retardation. Perinatal infections, including herpes simplex virus and group B streptococcal infections, also often produce serious long-term cognitive effects.9
NATURE OF INSULT
Genetic
The number of known genetic causes of mental retardation now exceeds 1000 and represents the largest proportion of known causes of mental retardation (also see Chapter 10B). This number is expected to increase as genetic techniques, such as subtelomeric fluorescent in situ hybridization (FISH) and comparative genomic hybridization, evolve and the ability to identify specific entities associated with cognitive impairment improves.48,49 Genetic causes are currently believed to be responsible for 7% to 15% of all cases of mental retardation and for 30% to 40% of cases with known causes.50,51 When a specific cause can be identified, genetic causes are typically identified in 30% of patients with severe mental retardation and in 4% to 8% of patients with mild mental retardation.52
Teratogenic
In utero exposures to teratogenic agents such as valproic acid and hydantoin and the effects of maternal cigarette smoking are associated with an increased risk for mental retardation.52,53 The effects of intrauterine exposure to alcohol may manifest across a spectrum of clinical conditions: fetal alcohol syndrome, alcohol-related birth defects, and alcohol-related neurodevelopmental disorder.54 Postnatal exposure to agents such as lead, methyl mercury, and polychlorinated biphenyls is also of concern.
Infectious
Although the effects of many infectious causes have been dramatically reduced with improved prenatal care and the introduction of several vaccinations (rubella, Haemophilus influenzae), this category still is important when specific causes of mental retardation are considered. Although the human immunodeficiency virus continues to be of concern, the effectiveness of methods to reduce maternal fetal transmission may have lessened its effect.9
Psychosocial
In cases of mild mental retardation, low socioeconomic status, however it is measured, is strongly and inversely related to prevalence.9,52 In theory, this is related to a lack of opportunity and/or stimulation in the home environment. The logical extension of that theory is that these cases are therefore preventable if identified early. It is this conclusion that formed the basis for the initial development of Head Start and other early intervention programs (EIPs).
CLINICAL MANAGEMENT
Importance of Assessing All Developmental Domains
The evaluation of a child with any type of delay in development should begin with a broadly based assessment in which all functional areas, not just the identified area of concern, are considered. This approach is consistent with the American Academy of Pediatrics’ recommendation for pediatricians to survey and screen routinely and repeatedly for development.55 Cognitive deficits may initially manifest as delays in language or social skills. Mental retardation may not be the only reason for this pattern of delay, but it must be considered and not immediately discarded as a “rare” problem in children. Relying on only clinical observation or informal checklists without specific cutoff scores or validation may cause the clinician to overlook affected children, delaying both identification and intervention.55
The level of cognitive involvement may be of primary importance in defining what is “normal” for a particular child in other developmental areas as patterns of developmental delay are described. For example, if a child has delays in both cognitive and social skills, the clinician must determine whether these deficits are similar in level or disparate, which would suggest other possible explanations or diagnoses, such as autism spectrum disorder. The incidence of pervasive developmental disorders in children with mental retardation is between 8% and 20%.56 With the increasing efforts by numerous organizations to identify children with autism spectrum disorder at the earliest possible age, the confounding effect of cognitive delay may be inappropriately ignored or minimized.
Timing of Presentation
NATURE OF PARENTS’ CONCERNS
In every case, it is extremely important for medical providers to listen to and address the concerns of a parent or care provider. It is extremely rare for parents’ chief complaint to be “I think my child is mentally retarded.” Instead they may report their own, or perhaps a teacher’s, concern that the child is “immature.” A child may initially present with behavioral problems, being described as “stubborn” or “oppositional.” The child’s inconsistent performance on structured, multiple-step tasks may be presented as proof that the child could do the work if he or she wanted to. Judgmental decisions by adults that the child is “just lazy” without an effort to assess the child’s true abilities may further delay the diagnosis. Provider reassurances that the child “will grow out of it” or that he or she “looks fine to me” have repeatedly been shown to be significantly frustrating for parents seeking help for their child.57
THE EFFECT OF MENTAL RETARDATION SEVERITY ON MANIFESTATION
Severe mental retardation is often diagnosed by 1 year of age, especially when dysmorphic features are present. In addition, the effects of their associated medical conditions and the greater likelihood of global developmental delays, including motor delay, may explain their earlier identification.58
CLINICAL DIAGNOSIS
A number of misconceptions that have been identified over the years have delayed acknowledgment of “mental retardation” as an appropriate clinical possibility, by both parents and physicians: “cute children” cannot have mental retardation; “ambulatory children” cannot have mental retardation; children younger than a certain age are “too young to test.”59 When these and other barriers are finally overcome, the clinical diagnosis of mental retardation can be considered as a possible explanation for a child’s pattern of developmental differences. A comprehensive and appropriate assessment should then be initiated to confirm the diagnosis.
Establishing the Diagnosis of Mental Retardation with the AAMR Three-Step Assessment
STEP 1
Cognitive tests of infant and early childhood cognitive abilities, except in the most severely affected cases, are poor predictors of later academic success, an ability that is currently best represented by an IQ score. The developmental abilities of typical children in this age range are rapidly changing.60 IQ testing is possible during the preschool years; however, the label “mental retardation” is usually not applied until the child is of school age, because IQ tests are not well correlated with later measures of IQ until 3 to 5 years of age. At that point, formal IQ testing is more reliable, and results better reflect a child’s long-term abilities (see Chapter 7C for more information). Several frequently used instruments are briefly described in this chapter. Lichtenberger61 published a more detailed review of formal measures of preschool cognitive assessment. Whichever particular instrument is selected, it must match the purpose of the assessment: to establish eligibility for services, to assist in planning intervention strategies and programs, or to provide support benefits and/or legal protection. Interpretation of test results always requires careful consideration of several variables: Was this a typical performance for the child? Were all sociocultural biases considered during test development and administration? Did the child understand the test instructions/format? Were special modifications required because of other developmental disabilities (motor, sensory, communication deficits)?61
 Bayley Scales of Infant Development-III: Provides a core battery of five sclaes. Three scales administered with child interaction—cognitive, motor, language. Two Scales conducted with parent questionnaires—social-emotional, adaptive behavior. Used in very young children (aged 1 to 42 months).62
Bayley Scales of Infant Development-III: Provides a core battery of five sclaes. Three scales administered with child interaction—cognitive, motor, language. Two Scales conducted with parent questionnaires—social-emotional, adaptive behavior. Used in very young children (aged 1 to 42 months).62 Stanford-Binet Intelligence Scale (5th edition): Provides a full scale score, two domain scores (verbal and nonverbal IQ), and several factor indexes for individuals aged 2 to 85 years.63
Stanford-Binet Intelligence Scale (5th edition): Provides a full scale score, two domain scores (verbal and nonverbal IQ), and several factor indexes for individuals aged 2 to 85 years.63 Kaufman Assessment Battery for Children II: Provides a global measure of ability (Mental Processing Composite IQ) for children as young as 3 years old. Additional scales and indices are added across the age range of the instrument (3 years 0 months to 18 years 11 months).64
Kaufman Assessment Battery for Children II: Provides a global measure of ability (Mental Processing Composite IQ) for children as young as 3 years old. Additional scales and indices are added across the age range of the instrument (3 years 0 months to 18 years 11 months).64 Wechsler Preschool and Primary Scale of Intelligence III (WPPSI III): Provides Full Scale, Verbal, and Performance scores (FSIQ, VIQ, and PIQ). The latest edition (2002) adds a General Language Composite for measuring both expressive and receptive but not higher order language functioning. For older children (aged 4 years 0 months through 7 years 3 months), a Processing Speed Quotient has been added. The WPPSI III is an appropriate instrument for children aged 2 years 6 months to 7 years 3 months.65
Wechsler Preschool and Primary Scale of Intelligence III (WPPSI III): Provides Full Scale, Verbal, and Performance scores (FSIQ, VIQ, and PIQ). The latest edition (2002) adds a General Language Composite for measuring both expressive and receptive but not higher order language functioning. For older children (aged 4 years 0 months through 7 years 3 months), a Processing Speed Quotient has been added. The WPPSI III is an appropriate instrument for children aged 2 years 6 months to 7 years 3 months.65STEP 2
Step 2 is to describe strengths and weaknesses across the five dimensions of mental retardation.
Describing strengths and weaknesses represented a dramatic shift for the AAIDD and other organizations working with individuals with mental retardation. These organizations began to address the effect of mental retardation on such individuals and on society, focusing on intervention and service planning rather than simply a “level of severity” classification system approach. These five dimensions are a key component of the 2002 AAMR comprehensive model of mental retardation (see Table 11-3). (See also the section “Levels of Support” earlier in this chapter.)
STEP 3
Step 3 is to determine needed supports and classify by intensity of service.
In a supports-based approach to the delivery of necessary services, the individual, rather than a specific program, is the focus. Supports enhance functioning and facilitate an individual’s inclusion in his or her natural community. Characterizing a person’s strengths and weaknesses is of no benefit unless some additional effort is made to define the necessary intensity level of those supports. It is important to recognize that the intensity of supports is independent of the location where the support needs to be delivered and may vary across the various areas of need. The judicious use of supports should improve a person’s level of functioning. Specific levels of support intensity have been defined (see Table 11-4). (See also the section “Levels of Support” earlier in this chapter.)
Identifying strengths and weaknesses across the five dimensions was integrated with the concept of “levels and intensity of support” in the AAIDD’s Supports Intensity Scales.10 There is frequent confusion about how the Supports Intensity Scales differ from a standardized measure of adaptive skills. A key distinction between the two approaches is that adaptive behavior measurements address “skills” needed for an individual to successfully function in society (the level of mastery), whereas the Supports Intensity Scales address activities that a person engages in during the course of participating in everyday life and how much support he or she needs to complete those activities.11
Etiological Diagnostic Workup: “The Search”
OVERVIEW: WHY ASK “WHY?”
Lenhard and associates24 described a number of psychological benefits for families attributed to diagnostic certainty. Families were frequently confronted in their physician’s office with an approach that Lenhard and associates characterized as “diagnostic minimalism”—the argument of health care providers that the assignment of a diagnosis of mental retardation rarely led to more effective treatments. The reluctance of physicians and other professionals (i.e., school personnel) working with the child and family to make and discuss this diagnosis may eliminate essential pathways to facilitate the family’s coping. It is also much easier for parents of children with a specific diagnosis to join and form associations and provide mutual support. Having a name for their child’s condition may improve the family’s access to systems of public support.
There is no standard workup for mental retardation or global developmental delay. There are numerous consensus guidelines regarding the appropriate degree and order of assessment in children diagnosed with mental retardation: two from genetics organizations, one from the American Academy of Neurology, and one from the American Academy of Pediatrics.50,51,70,70a A useful comparison of the similarities and differences among these statements was included in the article by Roberts and colleagues.71
COMPONENTS OF THE SEARCH
Each series of investigations should be tailored to the individual patient. The investigation should be directed by findings from the patient’s history, the family history, and the physical examination. In a systematic analysis, van Karnebeek and associates72 reported the results of several diagnostic investigations. Their recommendations included obtaining a clinical history and physical examination with emphasis on the neurological and dysmorphological examinations, obtaining standard cytological studies in all cases, ordering fragile X studies in all male patients, and requesting FISH subtelomeric studies based on established checklists. Metabolic studies were not recommended as a first-line investigation. Van Karnebeek and associates also concluded that neuroradiological studies had a high yield for identifying brain anomalies but a low yield for establishing an etiological diagnosis.72
HEARING AND VISION EVALUATIONS
Individuals with developmental delay and/or mental retardation are at increased risk for primary sensory impairments: vision abnormalities in 13% to 50% and audiological abnormalities in 18%.51 Formal assessments of hearing and vision are an integral part of the evaluation of these children.
GENETIC TESTING: INDICATIONS AND YIELD
Cytogenetically visible rearrangements are present in about 1% of newborns with a standard karyotype study (500 bands). The clinical significance of these rearrangements is not known. Chromosomal abnormalities are seen in approximately 25% of individuals with mental retardation: 40% of cases of severe mental retardation and 10% of cases of mild mental retardation. The presence of two or more minor dysmorphic features detected on physical examination also increases the likelihood that a chromosomal abnormality will be identified from 3.7% to 20% in affected individuals. The fragile X has been identified in 2% to 6% of male patients and in 2% to 4% of female patients with mental retardation. An increase in diagnostic yield from 2.6% to 7.6% is seen when decisions to obtain DNA fragile X studies are combined with physical examination findings.21
There is an increased percentage of genes in the telomeric regions of the chromosomes. Currently, these areas can best be examined with FISH. This technique identifies differences in 0.9% of normal controls, 1.1% of individuals with mild mental retardation, and 6.6% of individuals with moderate to severe mental retardation. At some point in the future, subtelomeric abnormalities may well become the primary cause of what had previously been described as “idiopathic mental retardation.” A checklist has been developed to improve the diagnostic yield of this method: family history of mental retardation; prenatal onset of growth retardation; postnatal poor growth/overgrowth; two or more facial dysmorphic features; and one or more nonfacial dysmorphic features and/or congenital abnormalities. The most significant predictors of a subtelomeric deletion are intrauterine growth retardation and a family history of mental retardation.73
NEUROIMAGING: INDICATIONS AND YIELD
There is an increased chance of an abnormal finding on head imaging study in the presence of an IQ of less than 50 in a child who has one of the following: microcephaly or macrocephaly, an abnormal cranial contour, midline and/or multiple dysmorphic features, an abnormal neurological examination finding, seizures, neurocutaneous findings, or a history of developmental milestone loss.74,75 Both the American College of Medical Genetics and the American Academy of Neurology recognize these as indications for obtaining a head imaging study. The American Academy of Neurology also recommends a head imaging study in cases of mental retardation associated with intrapartum asphyxia.50,51,58 The current yield from head imaging studies in children with mental retardation ranges from 33% in children without any other signs or symptoms to 63% to 73% in children with both mental retardation and cerebral palsy.21,51
METABOLIC TESTING: INDICATIONS AND YIELD
Relatively few metabolic conditions cause mental retardation in isolation; other neurological symptoms are commonly found (see Chapter 10C for more information). The presence of such symptoms in the child and in family members should be pursued. Many researchers assessing the yield of routine metabolic investigations in the child with mental retardation have concluded that there is little usefulness in such screening.50,51,70 The presence of a positive family history or other specific signs and symptoms identified in the history and physical examination may increase the yield of metabolic screening from 1% to 5%.
Generally accepted indications for additional metabolic investigations in children with mental retardation include episodic vomiting or lethargy, poor growth, seizures, evidence of storage disease, unusual odors, the loss of or a plateau of developmental skills, the presence of a movement disorder (chorea, dystonia), a new sensory loss (especially with retinal abnormality), or an acquired cutaneous disorder. The yield of directed and focused metabolic testing that is based on symptoms and performed in a stepwise manner may approach 14%.76
Expanded neonatal screening, now available in 23 states in the United States, tests for 20 or more of the 29 conditions recommended by the American College of Medical Genetics.77,78 The expansion in neonatal screening has allowed for the identification and treatment of inborn errors of metabolism in many children who might otherwise have died with the conditions undetected or become handicapped before any therapeutic interventions could be initiated. Although 15 states screen for fewer than 10 conditions, screening for congenital hypothyroidism and phenylketonuria is universal. Information from these screening programs should always be included in the evaluation of a child suspected to have mental retardation.
Differential Diagnosis
Breaking the News
The diagnosis and evaluation steps in this process usually have a beginning and an end. Whether the diagnosis occurs in infancy or later, management begins with breaking the news in a sensitive, compassionate, and culturally appropriate manner. When the clinician breaks the news, it is important to emphasize the child’s strengths, as well as the deficits. It is also important to be realistic without taking away hope. Parents should be informed that the child will continue to progress but at a slower pace. In addition, the child’s progress will be dependent on direct training rather than simply on the modeling of parents and siblings. If the child is less than 6 years of age at the time of diagnosis and does not have a syndrome known to be associated with mental retardation, it may be more appropriate to use the term global developmental delay. One problem in using the term delay lies in the fact that some parents may misconstrue the term as indicating that the condition is only temporary and that their child will some day catch up. This may indeed be the case when developmental quotients are marginal and/or unreliable because of the child’s lack of cooperation during testing. For the most part, developmental quotients below 50 in a cooperative child almost always indicate long-term impairment. When the child enters elementary school and standardized testing is more reliable and predictive of long-term cognitive status, the diagnosis may be revised as mental retardation. In any case, it is important to help parents maintain a level of expectation that is consistent with the child’s potential in order to enable the child to reach his or her maximum potential. When the child has a known syndrome that is causing the delays, the family should receive appropriate genetic counseling, be provided with up-to-date literature on the syndrome, and be linked to local (when available) and national syndrome-specific support groups, as well as more general support groups such as Family Voices or The Arc of the United States.79 (See later section on “Parent-Centered Supports.”)
MANAGEMENT
Historical Overview of the Management of Individuals with Mental Retardation and Associated Conditions
On the other hand, the care of individuals with severe mental retardation has markedly changed since the 1950s. These children were readily recognized by their dysmorphic features, although many current syndromes were not known by name, and/or by their severe cognitive and adaptive impairments. At that time, funding to support families raising children with severe disabilities was almost nonexistent. When families felt overwhelmed with their child’s challenging behaviors or when the extra caregiving duties required, parents’ only choice was to relinquish their child with severe mental retardation to an institution. Although the first institutions were built in the 1880s, enrollment in large facilities did not become a matter of routine until the mid-1900s.80 Enrollment peaked in 1967, when these facilities served almost 200,000 individuals.81
Since 1990, family and disability advocates have worked tirelessly to promote inclusion, increase funding for family support, and prevent out-of-home placements. New admissions to institutions, especially of children, have been curtailed, and many adults with mental retardation have moved out of large institutions into community-based group homes or to independent living settings. By 2000, only 15% (43,000) of individuals with severe disabilities lived in state-administrated institutions.81 One of the many goals included in Healthy People 2010, a road map for public health initiatives over the next decade for the entire population, was to “reduce the number of persons with disabilities living in congregate care facilities…to 0 by 2010 for persons aged 21 years and under.”82 The American Academy of Pediatrics supported this Healthy People 2010 goal with the publication of “Helping Families Raise Children with Disabilities at Home.”83 In 2005, several states reported having already met this goal by using innovative strategies such as recruiting support families to help a birth or adoptive family with the day-to-day childrearing activities, as well as providing some extended respite services.80
The concept of providing appropriate supports was not new; what was new was the belief that appropriate supports could improve the functional outcomes of individuals with mental retardation. The introduction by the AAIDD of the supports-based approach in 1992 affected education and adult habilitation programs by promoting a more natural, efficient, and ongoing basis for enhancing an individual’s functional status.84 Despite that document’s emphasis on appropriate supports to improve the functional outcome of individuals with mental retardation, community living, and supported employment, fewer than 10% of the states had fully embraced these concepts by 2000.85 However, a landmark Supreme Court decision (Olmstead v. L.C. Decision (527 U.S. 581, 138 F.3d 893, 1999) upheld the rights of individuals with mental retardation to live in community settings rather than in institutions. The decision emphasized community supports, independent individual assessment, and self-determination and choice as viable principles for persons with mental retardation, even those with severe mental retardation. It was a strong “voice” for a support-based approach. The Developmental Disabilities Assistance and Bill of Rights Act of 2000 (Public Law 106-402) further advanced the case for self-determination. Because of changing societal expectations, legislation, and judicial decisions, management strategies since the 1950s for persons with mental retardation have evolved from segregation (1960 to the 1980s) to deinstitutionalization (1990s) and to the current situation in which community membership—a concept that embraces true participation rather than simply living in community settings—is the norm.5
Health Care
ROUTINE SURVEILLANCE AND CARE
As with typically developing children, children with mental retardation benefit from ongoing health care within the context of a “medical home.”86,87 Health care should be family-centered, accessible, continuous, comprehensive, culturally sensitive, and developmentally appropriate. Unfortunately, the quality of health care for persons with mental retardation has often been significantly below established standards. Because many individuals with mental retardation now live longer, do so in communities rather than institutions, and are at an increased likelihood to live in poverty, these differences in health care have become more obvious. Transitions to adult systems of care have also been difficult for individuals with mental retardation and their families because of both availability and expertise.88 These challenges prompted a working conference and led to the report Closing the Gap: A National Blueprint to Improve the Health of Persons with Mental Retardation.11 This “blueprint,” designed to be an agenda for action, outlined goals to improve health care delivery, including integrating quality health care into communities (as opposed to institutions), improving the current unwieldy system of health care financing, developing more extensive resources, and increasing public knowledge and health professional training regarding the unique and specialized needs of individuals with mental retardation through research and new partnerships. If this agenda can be implemented, the key factors identified during a plenary presentation to that conference will be addressed: access, affordability, availability, and acceptability.11
Parent-professional partnerships are especially important for children with chronic disorders such as mental retardation. In addition to the child’s needs, the needs of the parents should always be given consideration in medical decision making. Except for the extra time and effort needed to communicate with schools and community agencies, the routine health maintenance of children with idiopathic mild mental retardation is very similar to that of typically developing children. The clinician should specifically address safety issues (because the child may not understand danger and environmental hazards), attainment of future developmental milestones, prevention of behavior problems, and early and ongoing promotion of independence through a program of anticipatory guidance.
Particular attention should be given to healthy lifestyles, good nutrition, and physical fitness. It appears that individuals with mental retardation have a much higher prevalence of obesity and cardiovascular disease than does the general population.89,90 These disorders are associated with lower rates of physical exercise, especially after graduation from high school, when there are fewer opportunities for organized sporting events such as the Special Olympics. Primary care physicians should monitor growth curves and advise parents early on when an increase in weight in relation to height is first noticed.
Dental surveillance and preventive care is also a challenging but vital aspect of care that is often neglected. Oral health disorders are more common among children with mental retardation than among the general population: 25% to 56% have caries, and 60% to 90% have gingivitis.91 This increased prevalence is associated with irregular brushing of teeth, the gingival hyperplasia seen with some anticonvulsant medications, and excessive dryness of the mouth caused by the anticholinergic side effects of certain medications. Dental treatment of children with severe mental retardation is more problematic because of the inability of such children to cooperate and their high levels of anxiety. Sometimes, restraints or general anesthesia is needed to facilitate restorative care.92
ROLE OF THE DEVELOPMENTAL-BEHAVIORAL PEDIATRICIAN
More severe mental retardation, especially in children with dysmorphic features and/or neurological deficits, may be diagnosed at birth or during infancy by a geneticist or neurologist. The developmental-behavioral pediatrician may be asked to evaluate a child with severe global developmental delay, especially in language and adaptive skills. However, this pediatrician may not become involved until later when the child’s primary care provider has questions about the developmental or functional status of the child, requests information about supports for the family, or needs assistance with comorbid disorders (health, behavioral, educational) that are unique to the child’s condition. Among the several medical subspecialists caring for a child with mental retardation, accessing and coordinating various systems of care is an area of expertise that is often unique to the developmental-behavioral pediatrician or neurodevelopmental disability physicians.
Management of Associated and Comorbid Disorders
CLASSIFICATION SYSTEMS
In 1980, the World Health Organization developed a model describing how an intrinsic disease could impair body functioning that could result in a disability and put the individual at a social disadvantage (handicap).93,94 This model was later revised to expand the idea that disease resulted in bodily impairments, limitations of activities, and restrictions in societal roles.95 These philosophical constructs are best captured in the International Classification of Functioning, Disability and Health (ICF) (see Chapter 6 for more information).95 On the other hand, the International Classification of Disease (ICD), also developed by the World Health Organization and most recently revised in 1993 as the 10th edition, provides a coding system for both physical and mental diseases.96 Although similar to ICD standards, the guidelines and classification procedures for mental health disorders published in the DSM-IV-TR6 are often preferred by clinicians in the United States (see Chapter 6 for more information). All three systems may play a role in the characterization and care of individuals with mental retardation, especially those with more severe forms of mental retardation. The ICF describes and quantifies the individual’s impairments and disabilities within a functional context, whereas the ICD classifies physical health conditions; the DSM-IV-TR classifies mental health conditions (including levels of mental retardation).
EFFECT OF MENTAL RETARDATION SEVERITY ON COMORBIDITY
The three classification systems (ICF, ICD, DSM-IV-TR) may be much more valuable in characterizing how children with severe mental retardation are likely to be affected and in structuring the care that they require. Environmental factors may not be as significant as the inherent limitations already imposed on them either by the underlying cognitive disability or by the associated physical, medical, and emotional conditions. Severe mental retardation is usually diagnosed during infancy and early childhood. The management of these children is challenging, because they may be nonverbal and unable to localize symptoms or communicate pain. They often have known syndromes or historical insults that affect more than cognition, which renders management more complex as a wider array of services and subspecialists is needed. It is beyond the scope of this chapter to address specific management issues for each of the more than 200 syndromes associated with mental retardation.
ASSOCIATED DISORDERS
Behavior Challenges
Although the behaviors may be obvious and well articulated by the parents, standardized tools may also be helpful. Besides detecting more subtle aspects of the behavior, they may also be useful for characterizing these problems and evaluating intervention effects. However, many have not been specifically studied in children with mental retardation, especially severe mental retardation. In two reviews, the Aberrant Behavior Checklist was singled out as the most reliable.97,98 Other tools thought to be helpful with this population include the Behavior Scale of the Vineland Adaptive Behavior Scale, the Clinical Global Impressions, the Child Behavior Checklist, and the Reiss Screen for Maladaptive Behavior. The Nisonger Child Behavior Rating Form has also been promoted for this purpose.99
Problematic behaviors often appear because a nonverbal child is unable to communicate his or her frustrations. In a nonverbal child, a change in behavior can also be the first sign of a new health concern, such as dental caries, a gastrointestinal disorder, or a skin infection. In fact, a medical concern is the most likely cause of a new disturbance in routine behaviors, especially when an individual is nonverbal and unable to localize pain.100 If a new medical condition has been ruled out and the behaviors are disrupting family functioning or preventing the child from participating in family, school, and community activities, then intervention is indicated.
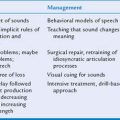
The clinician should always attempt to eliminate the behavior by nonmedical means. A survey of experts rated the three most effective components of psychosocial (nonmedical) intervention to be applied behavioral analysis, patient and caregiver education, and environmental management.98 The timely introduction of behavior management strategies, often by behavior specialists employed by EIPs and schools, by psychologists, and by other mental health professionals, and ideally before a situation gets out of control, provides the various care providers with methods to analyze, modify, and monitor behavioral concerns. Although not every situation can be anticipated, a consistent approach empowers caregivers to be consistent across various settings.
Some challenging behaviors may be refractory to behavioral interventions and/or so disruptive that medical intervention is warranted. The article by Rush and Frances revealed that “psychosocial experts” were much more likely to treat behaviors, even severely challenging ones, with nonmedical means than were the “medication experts.”98 Although the majority of “medication experts” stated that they would treat “self-injurious behaviors with the potential to cause bodily harm” and “aggressive behaviors” with medications as a first-line strategy, fewer than 30% of the “psychosocial experts” would use medication first. In these extreme situations, medical treatment should be just one component of a comprehensive behavior management plan. Even when a medication is prescribed, it is helpful to know the motivation for the challenging behavior. For example, if the child is disruptive during “circle time” at school, it would be helpful to know why. If it is because he or she is very anxious about joining the group, then a selective serotonin reuptake inhibitor (SSRI) might be appropriate. If it is because he or she also has comorbid ADHD type, then stimulant therapy might be more appropriate.
Sleep disorders are probably the most common and challenging example of the behavioral comorbid conditions. Poor sleep is associated with poor daytime learning, poor occupational performance, and increased daytime behavioral challenges. However, the most severe consequence of a sleep disturbance is often the resulting physical and emotional burdens on the child’s family and caregivers.
As in normal children, management of sleep disorders should begin with behavioral strategies to improve sleep hygiene: avoidance of overstimulation at least one half hour before bedtime and implementation of consistent bedtime routines that include a settling ritual (television off; a bath; a bedtime story; and lights off). Zeitgebers, naturally occurring entraining factors that adjust the endogenous sleep-wake cycle, should also be incorporated into the management plan. The most powerful zeitgeber is dark; turning lights off stimulates endogenous melatonin release. Social cues (parental behaviors, noise) and certain foods also function as zeitgebers.101 When problems persist, additional behavioral strategies may be required: sleep scheduling, gradual distancing, extinction, and bedtime fading.
On some occasions, biological interventions, such as exogenous melatonin and other medications, may be needed. Some medications (e.g., antihistamines, sedatives, clonidine) have been used on a long-term basis in children of all ages, whereas others (Ambien) are best reserved for older patients (5 years and older) for short-term use during vacations, scout camp, and sleepovers with friends and/or relatives. Exogenous melatonin is a strong zeitgeber and has been widely studied in children with disabilities; it is, however, not yet approved by the U.S. Food and Drug Administration.102 It has been found to be very effective in both inducing and prolonging sleep.103,104 Although there are no established guidelines, most investigators prescribed between 2 and 10 mg per dose. Short-acting preparations should be used when the child has difficulty falling asleep, and longer acting ones should be used for children with middle-of-the-night awakenings. The short-acting ones are generally in gel form and have an onset of action between 30 and 60 minutes. Drug levels remain higher than endogenous ones for 3 to 4 hours, regardless of nutritional status. The peak level of slow-release tablets is related to nutritional status; taking it on a full stomach may delay the onset of action considerably. Concentrations remain high for 5 to 7 hours. Side effects with melatonin are rare and, when they occur, are minor: headaches, nausea, and lightheadedness. Nightmares have been described, but this is believed to be a function of improved sleep. There is a report of a child with an underlying neurological condition having increased seizure frequency while taking melatonin, whereas another study demonstrated that seizure frequency actually decreased as a result of better sleep and decreased fatigue.105 There are also reports of exogenous melatonin’s having a delaying effect on the timing of puberty.106
Psychiatric Disorders
The prevalence of psychiatric disorders is approximately threefold to fourfold higher in individuals with mental retardation, especially severe mental retardation, than in the general population.5,107,108 It appears to be even higher in individuals raised in institutions than in those raised at home. The types of disorders prevalent in individuals with mental retardation are the same as those in the general populations, the most common ones being anxiety and stress disorders. In adults, these are associated primarily with trauma and incidents of abuse.5,100 Other common disorders include ADHD, depression, obsessive compulsive disorder, and oppositional defiant disorder. Schizophrenia is rare. It has been shown that approximately 15% to 20% of children with known severe mental retardation may also meet full criteria for autism.56 Although it was not mentioned in practice guidelines published in the mid-1990s, it is now thought that about 7% of children with Down syndrome meet criteria for autism.109,110 In these children, social skills, particularly joint attention, and language skills are significantly more delayed than skills in other domains.
There has been a historical tendency to attribute all behavioral and mood changes to the underlying mental retardation diagnosis (“diagnostic overshadowing”).5 The term dual diagnosis is now used when a specific mental illness (with a specific DSM-IV-TR diagnosis) occurs in a person who also meets diagnostic criteria for mental retardation. It is now recognized that such comorbidity is common. When using the DSM-IV-TR, the newest edition of the DSM system, the clinician would code for mental retardation as an Axis II disorder. When the mental retardation is part of a known etiological syndrome, it is coded under Axis III as well. Diagnoses on Axis II do not necessitate psychiatric care, and they do not respond to psychotropic medications; they do improve with supports and treatment. When there is a comorbid mental illness, an appropriate Axis I diagnosis is identified.
When assessing an individual with mental retardation for psychiatric illness, the clinician must take into account the individual’s developmental levels, especially their language abilities. Diagnosis is challenging when communication skills are poor. In nonverbal individuals, the clinician must be attentive to subtle behavioral cues that can lead to the appropriate comorbid psychiatric diagnosis.100 When evaluating a child, the clinician must remember that environmental stressors (change of residence, school, or routine; loss of significant caregiver; overcrowding; noises; physical abuse; teasing, taunts, and bullying) can trigger problems and affect the child’s compensatory mechanisms.
Although some standardized tools are useful for children with mild mental retardation, a comprehensive review commissioned by the National Institute of Mental Health revealed that few tools were reliable for those with more severe forms of mental retardation.97 Aman97 stated that it would take numerous tools to have an adequate armamentarium because those tools would have to address a number of domains while carefully considering the patient’s age and level of mental retardation and the informant’s status (self, caregiver, clinician). Expert consensus guidelines listed standardized rating scales as a second-line evaluation method.98 Some standardized tools can also be useful in assessing efficacy of specific interventions; others are important in assessing side effects, such as tardive dyskinesias. It is important to constantly monitor the medication effects (and side effects) on the child’s functional status and his or her ability to carry out daily activities and to participate in habilitation therapies.
The American Academy of Child and Adolescent Psychiatry’s practice parameter on diagnosis of comorbid mental illness in persons with mental retardation defines key components of a comprehensive assessment: A detailed review of medical, developmental, and behavioral histories, combined with any prior assessments of cognition, adaptive functioning, communication, and social skills, may help focus the evaluation.98,111 New or repeat evaluations may be required if the available information is incomplete or if new methods to define a cause or unusual symptoms have been developed. A functional analysis of behavior or, when not available, very specific and detailed descriptions of behaviors, antecedent events, and environmental circumstances define the specific concern. Describing what has been tried and what has been successful is also important.
Informed consent by the parents or guardian for psychotropic medications, especially those with significant side effects, is always advised.98 The older teenager or young adult with mental retardation should be included in this process if he or she has the capacity to participate. When a medication is chosen, the patient should “start low and go slow.” A poor response may be affected by variations in medication metabolism or compliance. Experts state that initial doses should be lower in children with mental retardation than in the general population and that titration should occur more slowly. However, maintenance and maximum doses are no different from those for the general population.98 The clinician should identify the specific index behavior or condition in advance to better evaluate efficacy of the treatment, especially for nonverbal children. Blood levels, if available, may be especially informative when side effects, poor response, worsening behaviors, and polypharmacy are concerns.
General recommendations from the American Academy of Child and Adolescent Psychiatry guidelines for individuals with mental retardation include using SSRIs as the first-line medication for post-traumatic stress disorder, depression, anxiety, or obsessive-compulsive disorder.98 Neuroleptic agents, especially the newer atypical ones, which have fewer side effects, were noted to be the treatment of choice for schizophrenia and psychosis not otherwise specified. They may also be helpful in children with mental retardation and comorbid behavioral conditions not defined by the DSM-IV-TR, such as self-injurious behaviors, aggression, and disabling stereotypical behaviors.99 For patients who are noncompliant with oral medication regimens, a long-acting depot antipsychotic may be needed. α-Agonists (clonidine, guanfacine) and β-blockers (propranolol) were cited as drugs of choice for disruptive behaviors. Antiepileptic drugs (e.g., valproate and carbamazepine) may be effective in treating agitation, irritability, and mood swings, especially in patients with comorbid epilepsy. Like individuals without mental retardation, those with mental retardation at risk for suicide, severe self-injury, or injury to others or with acute psychotic symptoms should be hospitalized.
The consensus guidelines recommended that patients be seen at least every 3 months and within 1 month of a drug or dosage change. They also provided guidance regarding dosing strategies (primarily in older teenagers and adults) and the duration of a medication trial before a switch to another medication is considered: 3 to 8 weeks for antipsychotics, 1 to 3 weeks for mood stabilizers, and 6 to 8 weeks for SSRIs.98 Although interclass polypharmaceutical treatment is sometimes needed in refractory cases, intraclass polypharmaceutical treatment is rarely justified. Clinicians are advised to minimize certain prescribing practices, including the long-term use of “as needed” medication orders, of benzodiazepines for “anxiety,” and of long- and short-acting sedative hypnotics. Certain antiepileptic medications (phenytoin, phenobarbital, and primidone) are not recommended as psychotropic medications.
Attention deficits, impulsivity, and hyperactivity are common in school-aged children, including those with mental retardation. Although the American Academy of Pediatrics’ Practice Guidelines for evaluation and treatment of ADHD do not address children with mental retardation, it is reasonable and appropriate to prescribe them to this population.112,113 Studies have shown that questionnaires and teachers’ observations are also valid and reliable in children with mental retardation.114,115 The most challenging diagnostic dilemma is determining the degree to which the child with mental retardation is demonstrating true symptoms of ADHD or the effect the child’s lower mental age is having on their clinical presentation. When the child’s inability to function in class appears to result from ADHD and not his or her lower mental age, medical treatment may be indicated. Stimulant therapy has been found to be effective, especially in reducing hyperactivity; results may be less consistent in individuals with more severe forms of mental retardation.98,116
Medical Disorders
All children with mental retardation, especially those with severe mental retardation who are unable to express themselves, should have comprehensive physical examinations at least annually in the context of an established medical home. For the most part, children with mental retardation contract the same illnesses as do children who are developing normally. A new or evolving medical condition might manifest as a change in behavior or routine. For example, self-injurious behavior, especially head banging, might be the only way a nonverbal child can express pain associated with a headache or tooth abscess. The major causes of death are similar to those in the normal population: cardiovascular disease, stroke, and cancer. The incidence of death from respiratory disease is significantly higher in those with severe mental retardation living in institutions than in those living at home. The prevalence of the following conditions may be higher in children with mental retardation than in the general population:5,91,107
SPECIAL HEALTH CONCERNS IN ADOLESCENTS AND YOUNG ADULTS WITH MENTAL RETARDATION
Successful social relationships foster self-esteem and contribute to better quality of life. Teenagers with severe mental retardation may experience difficulty in developing social relationships, for many reasons: stigmatizing dysmorphic features, lack of awareness of social etiquette, inappropriate sexual behavior, comorbid medical or physical disabilities, and overprotection from parents. Social development is chiefly experiential; teenagers with mental retardation, especially more severe forms of mental retardation, may have fewer opportunities to acquire social experience. Teenagers with mental retardation may need formal training in mastering social greetings, telephone skills, and proper etiquette (e.g., inhibition of sexual urges in public settings).
As in normal teenagers, the pediatrician must address issues of puberty and sexuality in teenagers with mental retardation, although explanations should be more basic. Sexuality is a fundamental human right and encompasses more than genital sex. It includes gender awareness and the needs to be liked and accepted, to feel valued and attractive, to display and receive affection, and to share thoughts and feelings. Until the 1990s, the issue of sexuality was rarely addressed in children with mental retardation; the topic was considered “taboo” for fear that the mere mentioning of the topic would unleash inappropriate desires and behaviors. There is now a growing body of literature addressing the topic.119,120 Numerous training programs have been developed to teach appropriate behaviors to teenagers with mental retardation through the use of videos, comic book stories, and role playing. Individuals with mental retardation, especially those with more severe mental retardation, may be less aware of others’ opinions and less inhibited in public settings. Maladaptive behaviors related to sexuality can be a significant barrier to the adolescent’s successful inclusion in school, work, and community settings.
Girls and women with mental retardation, like other girls and women, should strive to become independent in self-care and hygiene; this may be more challenging in those with more severe levels of mental retardation. Some female patients may never accomplish independence and may experience extreme anxiety and fear during menses, being unable to comprehend the concept of periodic benign bleeding. Gynecological care may likewise be complicated by increased anxiety and lack of cooperation during a “routine” pelvic examination. Preparation aided by pictures, role playing, having a trusted caregiver present during the appointment, and the use of alternative positions other than pelvic stirrups may minimize fear and stress.119
Although involuntary sterilization was an option in the past, it is no longer permissible.121,122 The eugenics movement of the early 20th century influenced sterilization policies and led to the passage of laws addressing sterilization in 30 states. These laws allowed, and in some cases required, sterilization of individuals with mental retardation and other disabilities. This level of intervention came about primarily as the result of a U.S. Supreme Court decision upholding Virginia’s authority to involuntarily sterilize “mentally defective” persons housed in state institutions. The decision was influenced, in part, by the mistaken assumption that most, if not all, children born to parents who had mental retardation would also have mental retardation. More than 60,000 men and women were sterilized in the ensuing years. In view of the atrocities of Nazi Germany, attitudes and practices began to change toward the end of World War II; however, states did not begin repealing these sterilization laws until the 1960s. Involuntary sterilization should never be performed on anyone who possesses, or might possess in the future, the capacity to provide valid consent to marriage, the capacity for reproductive decision making, and/or the ability to raise a child. In individuals who permanently and completely lack all of those capacities, sterilization should still be the procedure of last resort. It should be used only when less invasive and temporary alternatives are not possible and when the procedure is necessary and clearly in the best interest of the person with mental retardation. In every case, all possible measures must be taken to ensure a good outcome.122
There are now many effective and reversible alternatives to sterilization. In addition to traditional 28-day-cycle oral contraceptives, long-term contraception is now available and may be helpful in teenagers with limited cognition, limited motivation, and/or limited physical dexterity.123 These include weekly applied transdermal patches, monthly intramuscular injections, and implants and long-term progestin-releasing intrauterine devices that can provide protection for several years. A decision to use these interventions is between the physician, the parents, and, whenever possible, the individual. Possible side effects and drug interactions, especially when the individual is taking medications for treatment of comorbid disorders, must be carefully considered. Although parents may have legitimate concerns, the well-being and religious beliefs of the individual with mental retardation should prevail throughout the decision-making process.
DEVELOPMENTAL, EDUCATIONAL, AND VOCATIONAL SERVICES
Developmental, educational, and vocational services are the mainstays of management for children with mental retardation. Each may assume a position of primary importance, depending on the individual’s age and degree of involvement. For example, health concerns and interventions may be the focus in the very young child with severe mental retardation and comorbid medical conditions. The common focus of each service system is habilitation: to provide equal opportunities so as to facilitate full participation in society for these individuals by identifying and addressing their strengths and weaknesses and to work toward a goal of “normalization.”111
The type and intensity of supports needed are almost always determined through a multidisciplinary process. Professionals with expertise in numerous areas, most far beyond a narrow medical focus, join together to develop a support delivery plan based on the age, developmental level, and other unique characteristics of the child. Those with mild mental retardation usually need fewer services and supports than do those with more severe mental retardation. The focus of the written document, or Individualized Plan, depends on the age of the child. In all cases, it represents the child’s Individualized Support Plan; this umbrella term reflects the AAIDD support paradigm (Table 11-5).5
| Plan | Age | Services Provided |
|---|---|---|
| Individualized Family Support Plan (IFSP) | Children younger than 3 years | Early intervention |
| Individualized Education Plan (IEP) | Children aged 3 to 16 years | Educational |
| Individualized Transition Plan (ITP) | Adolescents aged 14-16 years through graduation | Transition, vocational, independent living |
| Individualized Habilitation (Support) Plan (IHP) | After graduation | Adult support |
Early Developmental Intervention: Part C of the Individuals with Disabilities Education Act (2004)
Severe global delays, especially in children with dysmorphic features, are usually diagnosed in infancy or shortly thereafter, and such children should be referred to an EIP as soon as their medical conditions are stabilized and they are able to participate. EIPs are government-funded developmental programs in which children with developmental delays or with known disabilities are entitled to participate. When a child receives a diagnosis of a syndrome known to be associated with mental retardation (e.g., Down syndrome), he or she becomes eligible for services at the time of diagnosis, even though delays may not yet be evident. On the other hand, a child without a recognizable syndrome is not eligible until a delay becomes evident. A specific, etiological diagnosis is not necessary to access early intervention services; in fact, it is advisable to refer the child to EIPs as soon as a delay becomes evident so that the child can receive appropriate services while the etiological workup progresses.
Evidence of the benefits of EIPs has been demonstrated best in disadvantaged children: that is, children of low-income families in which parents have less than a high school education.124 Outcome studies vary, and the magnitude of their effect appears to depend on several factors, including the appropriateness and intensity of the interventions and on the degree of parental involvement. When surveyed about consumer satisfaction, parents rated EIP programs as having a positive effect on their family’s acceptance of and caregiver abilities for the child.125 There is less conclusive evidence regarding lasting gains from standardized measures of language and cognitive development.
Special Education
PRESCHOOL
Often, children with mild to moderate mental retardation are not identified as such until after the third birthday and do not have the opportunity to benefit from early developmental services. At this point, the child should be referred to the special education department at the local school. Children aged 3 to 6 years are usually served in a Preschool Program for Children with Disabilities, although the 2004 IDEA legislation authorizes states to adopt policies that will provide families the option to remain in an EIP until the child is 5 years old.126 Determination of eligibility is again accomplished through a multidisciplinary team. The team’s evaluation serves as the basis for development of a support plan that is now called an Individualized Education Plan (IEP). The change in terminology from IFSP to IEP reflects a transition in focus from the family to the child.
ELEMENTARY SCHOOL
As the child ages and becomes eligible for elementary school, another evaluation is necessary to determine whether she or he is still eligible for special education services. If so, a new IEP is developed. In addition to describing the type, intensity, and frequency of supports and services recommended, the team also determines the best setting or settings for service delivery. According to the IDEA of 1990 and its subsequent re-authorizations in 1997 and 2004, the child should receive educational services in the “least restrictive environment” appropriate for that individual.126a Children with mental retardation, especially those with mild mental retardation, appear to have better outcomes when they are included in regular classrooms with typically developing peers. The extent of inclusion depends on the level of mental retardation and the extent of maladaptive behaviors (e.g., aggressive, self-injurious). It also depends on the school district’s resources. The child should be included in the regular classroom for as many academic classes as possible and for all nonacademic activities (recess, physical education, music, art, lunch, recess). Children with mild mental retardation usually need additional supports for academic classes during elementary and junior high (middle) school years: adaptations to the classroom, subject content, teaching strategies, and so forth. This may best be accomplished with a specially trained teacher aide who might be shared among several students with special needs. Although the “least restrictive environment” principle is very important, placement in a regular classroom should never prevent a child from receiving the specialized services outlined in his or her IEP.
HIGH SCHOOL
Children with mental retardation may require fewer supports during their junior high (middle school) and senior high school years. Vocational classes targeting their interests and strengths become the focus of training, replacing academic classes. Skills needed for successful independent living and meaningful employment are targeted.127 Although planning activities may begin as early as 14 years of age, teenagers with mental retardation should have an Individualized Transition Plan (ITP) in place by the time they are 16 years old. The ITP is different from the IEP in several specific ways:
Additional Considerations
PERIODIC EVALUATIONS
The following factors should be considered:
RECREATIONAL AND SOCIAL ACTIVITIES
Children and teenagers with mild mental retardation and younger children with more severe mental retardation are not usually excluded from integrated social activities with typically developing peers; teenagers with more severe forms of mental retardation have fewer opportunities for such social interactions. Throughout the school years, it is important that students with mental retardation, regardless of severity, be included in regular school events (dances, fund raisers, pep rallies) and extracurricular activities (band, pep squad, choir) as much as possible. These promote appropriate social skills, self-worth, dignity, and friendships with nondisabled peers. Students with mental retardation often benefit from participation in school- or community-sponsored social and athletic programs, such as the Special Olympics. These programs promote physical health and fitness and improve self-esteem while also providing opportunities for socialization. Many states, with the assistance of federal funding, have contracted with community agencies to develop and implement leadership training opportunities for youths with disabilities. These usually occur during the summer and foster social, self-advocacy, and leadership skills. Developmental-behavioral pediatricians should be aware of opportunities in their state and encourage their teenage patients to participation in these to the maximum extent possible.
COMMUNITY AND PUBLIC SUPPORTS
Supports are resources and strategies that promote development, education, individual functioning, independence, and personal well-being. They are ideally delivered in a systemized manner through an Individualized Support Plan (ISP). The focus of the support plan varies, depending on the child’s age: IFSP, IEP, or ITP (see Table 11-5). Of all health care professionals, the developmental-behavioral pediatrician is often the most knowledgeable about community and public supports and can be helpful to parents as they attempt to navigate a complex menu of services, each with their own unique eligibility criteria, admission procedures, and funding constraints.
Parent-Centered Supports
Supporting parents in their caregiving roles is very important, especially for a child with severe mental retardation, who may need extensive and prolonged care and supervision within the family home. A family’s requirement for additional supports depends not only on the characteristics of the child (i.e., the degree of cognitive impairment, comorbid disorders, behavioral challenges, and degree and duration of dependence) but also on the family’s characteristics: structural (e.g., single-parent household), functional (e.g., coping strategies), and external (e.g., income and work schedules).128 There are critical periods when parents, who might otherwise be doing fairly well with a little help from extended family and friends, need extra support.129 These times are usually ones of major life-status transitions when the child’s differences are most obvious. Early in the child’s life, such periods include the times when the diagnosis is first made, when a younger sibling developmentally surpasses the child with mental retardation, and when the affected child first enrolls in special education. Later in their child’s life, critical periods might include the onset of puberty, with its escalation of behavioral problems and inappropriate sexual behaviors; the graduation from high school, especially in the absence of vocational opportunities and/or community supports; the transition from pediatric to adult providers of health care; the process of determining legal guardianship at their child’s 18th birthday; and the death of a custodial parent. Parents’ coping skills are also challenged when they see their adolescent child being excluded from typical rites of adolescent passage such as social and athletic events, independent dating activities, and driver education classes.
INFORMATION AND EDUCATION
One of the most important early supports to parents is the provision of up-to-date and accurate information about their child’s condition, especially if it is associated with a known syndrome.79 Education empowers and supports parents in their caregiving roles. A survey of parents of children with chronic disorders reported that parents desired much more information than their pediatricians believed was necessary.130 It is hoped that the clinician making the diagnosis involves appropriate subspecialists in the child’s care, such as a developmental-behavioral pediatrician, or is able to provide a wider array of diagnosis-specific parent handouts. If this is not possible, the diagnosing clinician, the primary care provider, or the parents can contact the national organization that represents the disorder. National organizations, and sometimes even state and local chapters, can be found for most of the more common mental retardation-associated syndromes (e.g., the National Down Syndrome Congress). When this is not the case, the parents or physician can contact the National Organization for Rare Disorders for help. These organizations are usually governed by a professional board of directors, often with guidance from a medical advisory council. They may author, edit, or at least oversee the publications and information distributed by the staff or made available through their Web sites. This syndrome-specific information can be very helpful to both parents and professionals as they face the medical, developmental, educational, behavioral, and psychiatric challenges unique to that syndrome. Such organizations may host national conferences for parents and professionals and may assist parents of children with newly diagnosed disorders in contacting other parents of children with the same syndrome. Finally, some disorder-specific organizations maintain a national registry and sponsor bench and/or clinical research.
The Internet has rapidly become an important tool in accessing disability information, inasmuch as both local and national organizations have developed Web sites. Some Web sites include real-time “ask the expert” sessions. Listserve, message boards, and electronic discussion groups allow parents to expand their peer support network across the globe. Unfortunately, information found on Web sites may not be peer reviewed; thus, quality and validity may be questionable. Parents should be warned and advised to use caution in interpreting information from non-peer-reviewed sites. Rosenbaum and Stewart offered guidelines for parents on using the Internet as a source of information.131 Parents should be especially warned about Web sites that offer quick “cures,” usually through an alternative medicine approach. They should be referred to reputable professional sites that provide scientific critiques of alternative medicine interventions (e.g., http://www.quackwatch.org).
COMMUNITY (INFORMAL) SUPPORTS
One of the earliest needs that most parents have, especially if both are employed outside the home, is dependable and affordable childcare. This may not be an issue for the child with mild mental retardation or even one with more severe mental retardation, as long as there are no challenging health or behavior concerns. However, for children needing specialized medical care or individual supervision, accessibility to childcare is often not possible, despite the Americans with Disabilities Act mandates. When specialized childcare is available, it is often expensive, and the cost may outweigh the potential earned income.132 In these instances, one parent often decides to quit his or her job and remain at home to care for the child. The parent may later choose to reenter the work force when the child reaches school age.
Families of children with mental retardation are faced with added caregiving and supervision responsibilities, especially if the child has complicated health care or behavioral needs. Although many parents do well during their child’s early years, their parenting journey may bring them to a point where they are “burned out” with their childrearing role. Parents of all children benefit from occasional breaks in caregiving routines. Parents often turn to extended family members or friends for these breaks. If this is not possible, especially when caregivers with special skills are needed, a family needs to seek the assistance of an agency that provides respite services. Respite service (temporary care of a child with a disability by a trained provider for the purpose of providing relief to the family) is often cited by parents as the most needed support.133,134 Respite care may enable parents to face the caregiving role with renewed vigor. There are various respite care models; however, its availability, like so many other important support services, varies among communities. Respite care options include both home- and center-based care. Although center-based care, with trained caregivers and nurses in facility settings, was popular in the 1990s, newer legislation has provided increasing support for in-home options. There are advantages and disadvantages associated with both models, but a family’s options are often determined by the state’s funding allocation practices rather than by choice. (See the following “Public [Formal] Supports” section.) Family cooperatives, in which parents of children with similar disabilities agree to “swap” care with other families at no cost, may be more flexible because they are not dependent on public funding and are less restrictive. In extreme cases, parents may need an immediate break, or emergency respite care, to cope and, on occasion, as a measure to prevent abuse. Emergency respite care is more costly, requires around-the-clock staff, and is not always available in communities, even large urban ones.
Although not disability-specific, parent-to-parent organizations can assist in linking parents of children with similar disorders. Many parents derive a great deal of comfort from other parents who have encountered the same experiences. They often learn more useful and practical information from other parents than from professionals or published literature. These organizations can also provide parents with valuable information about local services and state disability legislation. Many conduct conferences and train parents in advocacy. Some organizations have become very effective in improving services for children with mental retardation at the local, state and, sometimes, even national levels. Parent Training and Information Centers are now federally mandated and exist in every state. These centers train and disseminate information to parents to help them become active collaborators, partners, decision makers, and problem solvers alongside policy makers, professionals, and agency personnel.128
PUBLIC (FORMAL) SUPPORTS
SSI benefits (distributed by the Social Security Administration since 1974) represented the first financial support for families raising children with severe disabilities, including those with mental retardation, at home. However, it was designed and continues to be a needs-based (i.e., based on income and assets) benefit for low-income families.135,136 Because of this requirement, many children with idiopathic mild mental retardation are not eligible for this support. If both financial need and disability severity criteria are met, the family receives a monthly stipend. Of greater importance is the fact that in most states, the receipt of any stipend amount automatically makes the child eligible for Medicaid. The benefit amount has slowly but steadily is increased since 1974. In 2007, the maximum month subsidy is $623; however, a family might actually receive much less.
In addition to supports provided through SSI, educational, and healthcare programs (Medicaid), families of children with severe mental retardation, especially those with comorbid health and/or behavior conditions may now be eligible for additional supports to assist them in raising their child. In the past, the only way a family could access these supports was to institutionalize their child. In the 1970s, most funding supported large state-operated institutions; however, legislation has subsequently shifted the preponderance of funding to community-based services.81,137 Although funding for community-based supports has been increasing since the 1970s, the degree of funding allocated for these services varies a great deal from state to state. Some states have policies that guarantee that all children with mental retardation will live in family settings, but many states still allocate large sums to institutional settings (state facilities, nursing homes, and intermediate care facilities for individuals with mental retardation).
The most common funding mechanism for in-home supports is the home- and community-based waiver services (HCBS). HCBS funding is available to families through waiver options because consideration of the family’s income and assets is waived for purposes of eligibility; thus, access is equitable across all income levels. Eligibility depends then entirely on the severity of the child’s disability and the effect that the disability imposes on the family. However, many states have long waiting lists. States have developed different mechanisms to distribute their limited resources: “first come, first served” waiting lists, urgency of need, time-limited supports, and a lottery system. Once a child becomes eligible for a funded slot, the family is assigned a case manager. Case managers work collaboratively with families and providers to design an annual service plan that includes choices from a menu of possible supports, such as respite (in-home, center- or camp-based) care, medical equipment, and home modifications for accessibility. The child also typically becomes eligible for regular Medicaid, which, in itself, is a great support to most families.
In addition to HCBS waivers, many states provide direct cash subsidies that enable parents raising their child with a disability at home to purchase services from an approved menu of options similar to those listed previously through the waiver system.132 This funding strategy is sometimes called a voucher program. These services vary significantly among the states and are very vulnerable to budget cuts. Annual distributions in 2000 ranged from $350 to $8500 per family. By 2002, 20 states had designed cash subsidy or voucher programs. Of all current mechanisms, this one provides the parents with the most flexibility and control. In the voucher program, parents themselves recruit, train, and enter into a formal contract with an individual (sometimes an extended family member) or a provider organization. Often, states have opted to provide families with a combination of funding strategies, including both waiver options and cash subsides. One funding stream may predominate over the other, depending on current state policy. For example, the state that provided the lowest annual cash subsidy to families also provided the highest annual waiver funding ($13,600 per family).132
The goal of these various programs is to provide adequate support services so that families do not feel the need for an out-of-home placement for their affected child or adult. A few states have adopted a unique “support family system” similar to shared custody arrangements between divorced couples. The birth family recruits a “support family” from extended family members or from the community, often with the assistance of a state-designated agency.80 The two families plan, in advance, for weekends and other times in which each will care for the child. This gives the birth family scheduled times of extended respite. In this way, costly institutionalization is prevented, and the child enjoys the benefits of growing up in a stable and nurturing family environment.
Youth- and Adult-Centered Supports
During the school years, youth with mental retardation receive most of their public supports from the educational system through development and implementation of an IFSP, an IEP, or an ITP, depending on the age of the child. In addition to the public support that schools supply, there are a number of national and community-based organizations that support children and adults with mental retardation (see Appendix). Examples include organizations such as the Young Men’s Christian Association (YMCA) that sponsor recreational and social activities, religious youth groups that provide opportunities to develop spirituality and new friendships, scouting programs that promote civic awareness, and camps that provide outdoor opportunities.138 Other organizations promote the development of special talents and interests such as painting, acting, singing, dancing, and athletics. Some may sponsor regional, state, and national competitions and even provide opportunities for professional performances. There are also Internet peer group organizations that link teenagers with mental retardation with one another. These opportunities promote independence, self-esteem, and social and leadership skills Other supports might be considered “too simple” and of no real consequence. However, such simple solutions as Velcro fasteners, which facilitate independence in dressing and toileting, and books in which pictures instead of words provide opportunities to garden and cook for those who cannot read do make a difference.139
When young adults with mental retardation graduate, they lose many of the public supports previously developed for them. However, the support paradigm described by the AAIDD has made a significant difference in their management after graduation.5,9,84 Ideally, support needs should still be determined by a multidisciplinary team and implemented as an ISP or, in some cases, an IHP. Needs should be evaluated in several areas: vocational training, home living, community living, employment, health, safety, behavior, social skills, and protection/self-advocacy. Providing necessary supports to adults is now recognized as a way to improve the functional capabilities and to enhance the social well-being of persons with mental retardation. Supports should serve to enhance independence, personal well-being, relationships, and participation in community activities. Supports may include tangible items, home modifications, accessible transportation, job coaching, attendant care, and/or crisis training. Available in all types and varieties, effective supports reduce the mismatch between environmental demands and a person’s capabilities.9,140
Unfortunately, these critical public supports may be lost if the adult with mental retardation receives a monetary gift from a well-meaning relative or an inheritance from his or her parents that causes him or her to no longer meet their specific financial criterion. However, continued access to public supports can be protected with the implementation of a “Special Needs Will and Trust.”141,142 A critical aspect of that document is a statement indicating that the inheritance is to be used only for items and services not covered by Medicaid, SSI, or other federal subsidies. Failure to include this statement will result in the loss of benefits until the amount equivalent to the value of the gift or inheritance is spent. In cases in which such statements are not in place, the individual may be required to repay the government for previously provided services. Siblings’ shares of the inheritance may also be at risk. Various nonprofit advocacy organizations and large life insurance companies employ benefit advisers who are available to inform and guide parents in the preparation of this legal document (see Appendix).
PUTTING A SUPPORT PLAN IN PLACE
As noted in the “Clinical Diagnosis” section, supports may be necessary over an individual’s lifespan in five dimensions: intellectual abilities, adaptive behavior, health, environmental context and participation, and interactions and social roles. Supports must be flexible and tailored to an individual’s intellectual, physical, emotional, and functional needs. Identified supports are needed at varying levels of intensity: limited, intermittent, extensive, or pervasive.5,9 They should also take into account the individual’s cultural, ethnic, linguistic, and economic characteristics.5 Preferences and progress must be monitored and revised when necessary.
For example, an older teenager with Down syndrome has recently graduated, has moved out of his parent’s home, and has been placed in a supported employment program at a local fast food restaurant. He may benefit from an ISP similar to the one described in Table 11-6. The success of this ISP depends on an array of natural, community, and public supports. Natural supports might include the assistance of family, friends, a religious organization, housemates, and peer staff at the restaurant. Community supports might include social activities sponsored by the church youth group, the Arc of the United States, or the local YMCA chapter. The success of the entire system, however, depends strongly on public supports, particularly funding resources, including SSI stipends, Food Stamps, housing subsidies, Medicaid health benefits, and HCBS waiver programs.
Sibling Supports
As with parents, the discovery that a child has mental retardation has a profound effect on siblings. The news can have both positive and negative effects.143 Some evidence suggests that in comparison with families without a child with mental retardation, siblings of children with mental retardation may be more sensitive, helping, emotionally supportive, and accepting of people with differences.144–146 Some have become very effective advocates for disability issues, rising even to national recognition. However, there are also some negative effects. Siblings may feel that they need to compete for their parent’s attention, especially when the child with mental retardation also has significant medical or psychiatric comorbid conditions. The feelings associated with this competition are strongly associated with the parents’ awareness of their actions and the sibling’s cognitive understanding of the disability. Some siblings may perceive increased parental expectations and struggle to be a high achiever to compensate for the child with mental retardation. Unless the parents have adequately explained mental retardation, siblings may harbor misconceptions and fears that they will “catch” the disability as if it was an infectious process. Relationships among siblings with and without disabilities are going to be different; that does not mean that those relationships are inferior or require intervention.147 An older or a younger sibling (if she or he has surpassed the child with mental retardation) may be expected to act as a surrogate parent and experience an accelerated passage to adulthood at the expense of beneficial childhood experiences. Such siblings often assume roles of managers and teachers of the sibling with a disability.148 Finally, siblings, even at a young age, may harbor concerns that they are expected to care for the child with mental retardation after the parents die. Thus, pediatricians should express genuine concern about the siblings themselves and practice vigilance for their well-being. In addition, there are national organizations (Sib Shops) and electronic Web sites created just for siblings (see Appendix).
ADULT OUTCOME
Substantial variability exists in developmental/intelligence test scores from early childhood until about ages 6 to 9 years. If serial testing at that point demonstrates a consistent developmental velocity, the test’s predictive value is enhanced. Although measured intelligence is very important in determining adult outcome, other factors may significantly affect functioning and foster drastically different results.6,149 These factors include coexisting medical and sensory disorders and, more important, behavioral and psychiatric disorders. Environmental factors (degree of inclusion in integrated settings during childhood) are also important, as are parents’ parenting style (i.e., the provision of opportunity, fostering of well-being, and promotion of stability). With increasing age, social and adaptive skills assume a greater importance than do intellectual skills in determining independence and the ability to successfully function in the community.150 Despite the interaction of all of these confounding variables, some very general statements can be made regarding the degree of mental retardation and levels of functioning as an adult (Table 11-7).
It can also be very helpful to graphically correlate chronological age, mental age, and academic grade level when the “natural history” of mental retardation is explained to a family (Fig. 11-1). This graph effectively depicts the widening of the gap between individuals with mental retardation and typically developing peers over time. This may be helpful in reassuring families that their child’s condition is not “getting worse.” It may also be of value in demonstrating why a child with mild mental retardation (the majority of cases) may not be identified until at or near school entry, when the gap reaches a significant level of difference. Finally, it can be a source of encouragement to families as they try to predict what their child is and is not able to do.
FUTURE RESEARCH
Because mental retardation is believed to be the result of the interaction of a number of factors that significantly affect an individual across the lifespan, future research efforts must address issues of etiology, treatment of the primary condition, and the effect of associated comorbid conditions. Genetic discoveries have helped explain the biological reason for several conditions associated with mental retardation, such as fragile X and Rett syndromes. There are ongoing efforts to better understand the interaction between some of these genetic mechanisms and the environment. Will there one day be a role for prenatal gene therapy for conditions responsible for some forms of mental retardation? What other discoveries may be possible with newer imaging techniques such as positron emission tomography and diffusion tensor imaging? There must also be a research focus to consider this disabling condition from its effect on different societal systems: family, health care, work. As the trend away from institutional care continues, what interventions and supports are most effective in maximizing the benefits of home or community based care and living? It is well documented that individuals with mental retardation have poorer access to routine health and preventative care. Methods to ensure appropriate access to care and the inclusion of individuals with mental retardation in health promotion efforts, although already a goal of Health People 2010, must be developed and implemented. Very often the associated comorbid conditions, especially behavior, are what severely limit the ability of an individual with mental retardation to be fully included in society. How can a natural system of supports for inclusion be implemented? For research in mental retardation to be most effective, it must move outside of the laboratory and beyond simply asking the question “Why did this happen?”
CONCLUSIONS
Making a timely diagnosis of mental retardation may depend on a high index of suspicion, especially in a child who looks normal and initially demonstrates only language delays. Diagnosis is a two-part process that includes the clinical diagnosis of mental retardation that is based on DSM-IV-TR and/or AAMR criteria and a systematic search for a medical cause. The diagnostic process can be facilitated by the developmental-behavioral pediatrician, ideally as part of a multidisciplinary team approach. Management begins with genetic counseling (when a cause is known), parent education, and a prompt referral to an infant intervention program or, for older children, to the public education system. Children with mental retardation should be cared for in the context of a medical home and receive ongoing quality physical, behavioral, dental, and mental health surveillance and treatment. The primary care provider should also promote fitness and discourage inactivity and obesity. It is important to consider the well-being of all family members and help them identify and access appropriate community and public supports when necessary, with the realization that those needs change over time. Regardless of the degree of mental retardation, parents should be encouraged to promote independence to the maximum extent possible throughout all stages of their child’s development. If it is financially feasible, parents should initiate long-term planning in the form of a Special Needs Will and Trust early in the child’s life. Developmental-behavioral pediatricians can play important roles as consultants and facilitators of integrated and coordinated care, especially when comorbid conditions or challenging behaviors appear. The developmental-behavioral pediatrician can also provide appropriate anticipatory guidance to prevent secondary disabilities and assist in transitioning the adolescent into adult systems of care that may include education and training of the health providers.
1 Centers for Disease Control and Prevention. Economic costs associated with mental retardation, cerebral palsy, hearing loss and vision impairment-United States, 2003. M MWR Morb Mortal Wkly Rep. 2004;53(3):57-59.
2 Snyder TD, Hoffman CM. Digest of Educational Statistics and Figures (NCES 2003–060). Washington, DC: National Center for Education Statistics, 2002.
3 Finley WML, Lyons E. Rejecting the label: A social constructionist analysis. Ment Retard. 2005;43:120-134.
4 Panek PE, Smith JL. Assessment of terms to describe mental retardation. Res Dev Disabil. 2005;26:565-576.
5 American Association on Mental Retardation. Definition, theoretical model, framework for assessment, and operational Definitions. In: Luckasson RA, Schalock RL, Spitalnik DM, et al, editors. Mental Retardation: Definition, Classification, and Systems of Support. 10th ed. Washington, DC: American Association on Mental Retardation; 2002:5-17.
6 American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed, Text Revision. Washington, DC: American Psychiatric Association, 2000;38-49.
7 Sparrow SS, Davis SM. Recent advances in the assessment of intelligence and cognition. J Child Psychol Psychiatry. 2000;41:117-131.
8 Leonard H, Wen X. The epidemiology of mental retardation: Challenges and opportunities in the new millennium. Ment Retard Dev Disabil Res Rev. 2002;8:117-134.
9 Thompson JR, Bryant BR, Campbell EM. Support Intensity Scale. Washington, DC: American Association on Mental Retardation, 2004.
10 Harries J, Guscia R, Kirby N, et al. Support needs and adaptive behaviors. Am J Ment Retard. 2005;110:393-404.
11 U.S. Public Health Service. Closing the Gap: A National Blueprint to Improve the Health of Persons with Mental Retardation: Report of the Surgeon General’s Conference on Health Disparities and Mental Retardation. Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General, 2002.
12 Larson SA, Larkin KC, Anderson L, et al. Prevalence of mental retardation and developmental disabilities: Estimates from the 1994/1995 national health interview survey disability supplements. Am J Ment Retard. 2001;106:231-252.
13 Bhasin TK, Brocksen S, Avchen RN, et al. Prevalence of four developmental disabilities children aged 8 years-Metropolitan Atlanta Developmental Disabilities Surveillance Program, 1996 and 2000. MMWR Surveill Summ. 2006;55(1):1-9. MMWR Morb Mortal Wkly Rep. 2006;55(4):105-106. [erratum in]
14 Flint J. The genetic basis of cognition. Brain. 1999;122:2015-2031.
15 Plomin R. Genetics, genes, genomics and G. Mol Psychiatry. 2003;8:1-5.
16 Jellife LL, Shaw GM, Nelson V, et al. Risk of mental retardation among children born with birth defects. Arch Pediatr Adolesc Med. 2003;157:545-550.
17 Sameroff AJ, Seifer R, Baldwin A, et al. Stability of intelligence from preschool to adolescence: The influence of social and family risk factors. Child Dev. 1993;64:80-97.
18 Gutman LM, Sameroff AJ, Cole R. Academic growth curve trajectories from 1st grade to 12th grade: Effects of multiple social risk factors and preschool child factors. Dev Psychol. 2003;39:777-790.
19 Chapman DA, Scott KG, Mason CA. Early risk factors for mental retardation: Role of maternal age and maternal education. Am J Ment Retard. 2002;107:46-59.
20 Jelliffe-Pawloski LL, Shaw GM, Nelson V, et al. Risks for severe mental retardation occurring in isolation and with other developmental disabilities. Am J Med Genet A. 2005;136:152-157.
21 van Karnebeek CDM, Jansweijer MCE, Leenders AGE, et al. Diagnostic investigation in individuals with mental retardation: A systematic literature review of their usefulness. Eur J Hum Genet. 2005;13:6-25.
22 van Karnebeek CDM, Scheper FY, Abeling NG, et al. Etiology of mental retardation in children referred to a tertiary care center: A prospective study. Am J Ment Retard. 2005;110:253-267.
23 Moog U. The outcome of diagnostic studies on the etiology of mental retardation: Consideration on the classification of the causes. A m J Med Genet A. 2005;137:228-231.
24 Lenhard W, Breitenbach E, Ebert H, et al. Psychological benefit of diagnostic certainty for mothers of children with disabilities: Lessons from Down syndrome. Am J Med Genet A. 2005;133:170-175.
25 O’Leary CM. Fetal alcohol syndrome: Diagnosis, epidemiology and developmental outcomes. J Pediatr Child Health. 2002;40:2-7.
26 Bennetto L, Pennington B. Neuropsychology. In: Hagerman RJ, Hagerman PJ, editors. Fragile X Syndrome: Diagnosis, Treatment and Research. Baltimore: Johns Hopkins University Press; 2002:206-248.
27 Pennington BF, Moon J, Edgin J, et al. The neuropsychology of Down syndrome: Evidence for hippocampal dysfunction. Child Dev. 2003;74:75-93.
28 Committee to Study Fetal Alcohol Syndrome, Institute of Medicine. Diagnosis and clinical evaluation of fetal alcohol syndrome. In: Stratton K, Howe C, Battaglia F, editors. Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Prevention and Treatment. Washington, DC: National Academies Press; 1996:63-81.
29 Sokol RJ, Delaney-Black V, Nordstrom B. Fetal alcohol spectrum disorder. JAMA. 2003;290:2996-2999.
30 Hoyme HE, May PA, Kolberg WO, et al. A practical clinical approach to diagnosis of fetal alcohol spectrum disorder: Clarification of the 1996 Institute of Medicine criteria. Pediatrics. 2005;115:39-47.
31 Astley SJ, Clarren SK. Diagnosing the full spectrum of fetal alcohol exposed individuals: Introducing the 4-digit diagnostic code. Alcohol Alcohol. 2000;35:400-410.
32 Streissguth AP, Bookstein HM, Barr HM, et al. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J Dev Behav Pediatr. 2004;25:228-238.
33 Crnic LS, Hagerman R. Fragile X syndrome: Frontiers of understanding gene-brain-behavior relationships. Ment Retard Dev Disabil Res Rev. 2004;10:1-2.
34 Terracciano A, Chiurazzi P, Neri G, et al. Fragile X syndrome. Am J Med Genet C Semin Med Genet. 2005;137:32-37.
35 Cornish K, Sudhalter V, Turk J, et al. Attention and language in fragile X. Ment Retard Dev Disabil Res Rev. 2004;10:11-16.
36 Cohen D, Pichard N, Tordjman S, et al. Specific genetic disorders and autism: Clinical contributions toward their identification. J Autism Dev Disord. 2005;35:103-116.
37 Loesch DZ, Huggins RM, Hagerman RJ, et al. Pheno-typic variation and FMRP levels in fragile X. Ment Retard Dev Disabil Res Rev. 2004;10:31-41.
38 Bailey DB, Skinner D, Sparkman KL, et al. Discovering fragile X: Family experiences and perceptions. Pediatrics. 2003;111:407-416.
39 Roizen NJ. Down syndrome: Progress in research. Ment Retard Dev Disabil Res Rev. 2001;7:38-44.
40 Chapman RS, Hesketh LJ. Behavioral phenotype of individuals with Down syndrome. Ment Retard Dev Disabil Res Rev. 2000;6:84-95.
41 Chapman RS, H-K Seung, Schwartz SE, et al. Language skills of children and adolescents with Down syndrome: II. Production deficits. J Speech Lang Hear Res. 1998;41:861-873.
42 Nadel L. Down syndrome: A genetic disorder in bio-behavioral perspective. Genes Brain Behav. 2003;2:156-166.
43 Brown FR, Greer MK, Aylward EH, et al. Intellectual and adaptive functioning in individuals with Down syndrome in relation to age and environmental placement. Pediatrics. 1990;85:450-452.
44 Turner S, Alborz A. Academic attainment of children with Down syndrome: A longitudinal study. Br J Educ Psychol. 2003;73:563-582.
45 Rasmussen P, Borheson O, Wentz E, et al. Autistic disorders in Down syndrome: Background factors and clinical correlates. Dev Med Child Neurol. 2001;43:750-754.
46 Roizen NJ, Patterson D. Down syndrome. Lancet. 2003;361:1281-1289.
47 Hagberg PSG. Aetiology in severe and mild mental retardation: A population based study of Norwegian children. Dev Med Child Neurol. 2000;42:76-86.
48 Xu J, Chen Z. Advances in molecular cytogenetics for the evaluation of mental retardation. Am J Med Genet C Semin Med Genet. 2003;117:15-24.
49 Winnepenninckx B, Rooms L, Kooy R, et al. Mental retardation: A review of the genetic causes. Br J Dev Disabil. 2003;49:29-44.
50 Curry CJ, Stevenson RE, Aughton D, et al. Evaluation of mental retardation: Recommendations of a consensus conference: American College of Medical Genetics. Am J Med Genet. 1997;72:468-477.
51 Shevell M, Ashwal S, Donley D, et al. Practice parameter: Evaluation of the child with global developmental delay: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2003;60:367-380.
52 Murphy CC, Boyle C, Schendel D, et al. Epidemiology of mental retardation in children. Ment Retard Dev Disabil Res Rev. 1998;4:6-13.
53 Drews CD, Murphy CC, Yeargin-Allsopp M, et al. The relationship between idiopathic mental retardation and maternal smoking during pregnancy. Pediatrics. 1996;97:547-553.
54 Sampson PD, Streissguth AP, Bookstein FL, et al. Incidence of fetal alcohol syndrome and prevalence of alcohol-related neurodevelopmental disorders. Teratology. 1997;56:317-326.
55 Council on Children with Disabilities; Section on Developmental Behavioral Pediatrics; Bright Futures Steering Committee; Medical Home Initiatives for Children with Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: An algorithm for developmental surveillance and screening. Pediatrics. 2006;118:405-420. Pediatrics. 2006;118:1808-1809. [erratum in:]
56 de Bildt A, Sytoma S, Kraijer D, et al. Prevalence of pervasive developmental disorders in children and adolescents with mental retardation. J Child Psychol Psychiatry. 2005;46:275-286.
57 Poehlmann J, Clements M, Abbeduto L, et al. Family experiences associated with a child’s diagnosis of fragile X or Down syndrome: Evidence for disruption and resilience. Ment Retard. 2005;43:255-267.
58 Shevell M, Majnemer A, Platt R, et al. Developmental and functional outcomes in children with global developmental delay or developmental language impairment. Dev Med Child Neurol. 2005;47:678-683.
59 Coplan J. Three pitfalls in the early diagnosis of mental retardation. Clin Pediatr. 1982;21:308-310.
60 Saye KB. Preschool intellectual assessment. In: Reynolds CR, Kamphaus RW, editors. Handbook of Psychological and Educational Assessment of Children: Intelligence, Aptitude and Achievement. 2nd ed. New York: Guilford; 2003:187-203.
61 Lichtenberger EO. General measures of cognition for the preschool child. Ment Retard Dev Disabil Res Rev. 2005;11:197-208.
62 Bayley N. Bayley Scales of Infant and Toddler Development, 3rd ed. San Antonio, TX: Harcourt Assessments, 2005.
63 Roid G. Stanford-Binet Intelligence Scale, 5th ed. Toronto: Thomas Nelson Corp, 2003.
64 Kaufman A, Kaufman D. Kaufman Assessment Battery for Children, 2nd ed. Shoreview, MN: AGS, 2003.
65 Wechsler D. Wechsler Preschool and Primary Scale of Intelligence III. San Antonio, TX: Harcourt Assessment, 2002.
66 Wechsler Intelligence Scale for Children. 4th ed. San Antonio, TX: Harcourt Assessment; 2003.
67 Sparrow SS, Cicchetti DV, Balla DA, et al. Vineland Adaptive Behavior Scales, 2nd ed. Shoreview, MN: AGS, 2005.
68 Harrison P, Oakland T. Adaptive Behavior Assessment System-II. San Antonio, TX: Harcourt Assessment, 2003.
69 Bruininks RH, Woodcock RW, Weatherman RF, et al. Scales of independent behavior revised (SIB-R). Toronto: Thomas Nelson Corp, 1996.
70 Battaglia A, Carey JC. Diagnostic evaluation of developmental delay/mental retardation: An overview. Am J Med Genet C Semin Med Genet. 2003;117:3-14.
70a Moeschler JB, Shevell M. AAP Committee on Genetics: Clinical Genetic Evaluation of the Child with Mental Retardation or Developmental Delays. Pediatrics. 2006;117:2304-2316.
71 Roberts G, Palfrey J, Bridgemohan C. A rational approach to the medical evaluation of a child with developmental delay. Contemp Pediatr. 2004;21:76-100.
72 van Karnebeek CD, Scheper FY, Abeling NG, et al. Etiology of mental retardation in children referred to a tertiary care center: A prospective study. Am J Ment Retard. 2005;110:253-267.
73 Baker E, Hinton L, Callen DF, et al. Study of 250 children with idiopathic mental retardation reveals nine cryptic and diverse subtelomeric chromosome anomalies. Am J Med Genet. 2002;107:285-293.
74 Battaglia A. Neuroimaging studies in the evaluation of developmental delay/mental retardation. Am J Med Genet C Semin Med Genet. 2003;117:25-30.
75 Williams HJ. Imaging the child with developmental delay. Imaging. 2004;16:174-185.
76 Papavasiliou AS, Bazigou H, Paraskevoulakas E, et al. Neurometabolic testing in developmental delay. J Child Neurol. 2000;15:620-622.
77 Rinaldo P, Tortorelli S, Matern D, et al. Recent developments and new applications of tandem mass spec-trometry in newborn screening. Curr Opin Pediatr. 2004;16:427-433.
78 Newborn Screening: Toward a Uniform Screening Panel and System. (Available at: ftp.hrsa.gov/mchb/genetics/screeningdraftforcomment.pdf; accessed 11/22/06.)
79 Rahi JS, Manaras I, Tuomainen H, et al. Meeting the needs of parents around the time of diagnosis of disability among their children: Evaluation of a novel program for information, support, and liaison by key workers. Pediatrics. 2004;114:e477-e482.
80 Rosenau N. Family-Based Alternatives. Austin, TX: Every Child, 2005.
81 Braddock D, Hemp R, Rizzolo MC. State of the states in developmental disabilities. Ment Retard. 2004;42:356-370.
82 U.S. Department of Health and Human Services. Healthy People 2010. With Understanding and Improving Health and Objectives for Improving Health. 2nd ed. Washington, DC: U.S. Government Printing Office; 2000.
83 Johnson CP, Kastner TA. Helping families raise children with special health care needs at home. Pediatrics. 2005;115:507-511.
84 American Association on Mental Retardation. Luckasson R, Coulter DL, Polloway EA, et al, editors. Mental Retardation: Definition, Classification and Systems of Supports, 9th ed., Washington, DC: American Association on Mental Retardation, 1992.
85 Denning CB, Chamberlain JA, Polloway EA. An evaluation of state guidelines for mental retardation: Focus on definition and classification practices. Educ Train Ment Retard Dev Disabil. 2000;35:226-232.
86 American Academy of Pediatrics, Task Force on the Medical Home. The medical home. Pediatrics. 2002;113(Suppl):1471-1478.
87 Strickland B, McPherson M, Weissman G, et al. Access to the medical home: Results of the National Survey of Children with Special Health Care Needs. Pediatrics. 2004;113:1485-1492.
88 Blum WB. Improving transition for adolescents with special health care needs from pediatric to adult-centered health care. Pediatrics. 2002;110(Suppl):1301-1335.
89 Pitetti KH, Campbell KD. Mentally retarded individuals: A population at risk? Med Sci Sports Exerc. 1991;23:586-593.
90 Rimmer J: Aging, mental retardation and physical fitness. Arc Newsletter pp 1–7, November 1997. Available at http://www.thearc.org/faqs/fitnessage.html.
91 Horwitz SM, Kerker BD, Owens PL, et al: The Health Status and Needs of Individuals with Mental Retardation. Washington, DC: Special Olympics, 2000. Available at http://www.specialolympics.org/Special+Olympics+Public+Website/English/Initiatives/Research/Health_Research/Health+Status+and+Needs.htm.
92 Fenton SJ, Perlman S, Turner H, editors. Oral Health Care for People with Special Needs: Guidelines for Comprehensive Care. River Edge, NJ: Exceptional Parent, Psy-Ed Corp, 2003.
93 World Health Organization. International Classification of Impairments, Disabilities, and Handicaps. A Manual of Classification Relating to the Consequences of Disease (ICIDH). Geneva, Switzerland: World Health Organization, 1980.
94 World Health Organization. International Classification of Functioning and Disability (ICIDH-2). Geneva, Switzerland: World Health Organization, 2000.
95 World Health Organization. International Classification of Functioning, Disability and Health (ICF). Geneva, Switzerland: World Health Organization, 2001.
96 World Health Organization. ICD-10: International Statistical Classification of Disease and Related Health Problems. Geneva, Switzerland: World Health Organization, 1992.
97 Aman MG. Review and evaluation of instruments for assessing emotional and behavioural disorders. Aust N Z J Dev Disabil. 1991;17:127-145.
98 Rush AJ, Frances A. Expert consensus guidelines on the treatment of psychiatric and behavioral problems in mental retardation [Special Issue]. Am J Ment Retard. 2000;105:159-228.
99 Findling RL, Aman MG, Eerdenkens M, et al. Long term, open-label study of risperidone in children with severe disruptive behaviors and below-average IQ. Am J Psychiatry. 2004;161:677-684.
100 Ryan R. Recognizing psychosis in nonverbal patients with developmental disabilities. Psychiatr Times. 2001;18(12):1-6.
101 Nir I, Meir D, Zilber N, et al. Brief report: Circadian melatonin, thyroid-stimulating hormone, prolactin and cortisol levels in serum of young adults with autism. J Autism Dev Disord. 1995;25:641-654.
102 Arendt J, Skene DJ. Melatonin as a chronobiotic. Sleep Med Rev. 2005;9(1):25-39.
103 Jan JE. Melatonin treatment of sleep-wake cycle disorders in children and adolescents. Dev Med Child Neurol. 1999;41:491-500.
104 Dodge NN. Melatonin reduces sleep latency. J Child Neurol. 2001;16:581-584.
105 Sheldon SH. Proconvulsant effects of oral melatonin in neurologically disabled children. Lancet. 1998;351:1254.
106 Cavallo A. Melatonin and human puberty: Current perspectives. J Pineal Res. 1993;15:115-121.
107 Gillberg C. Practitioner review: Physical investigations in mental retardation. J Child Psychol Psychiatry. 1997;38:889-897.
108 Dosen A, Day K, editors. Treating Mental Illness and Behavior Disorders in Children and Adults with Mental Retardation. Washington, DC: American Psychiatric Press, 2001.
109 Kent L, Evans J, Paul M, et al. Comorbidity of autism spectrum disorder in children with Down syndrome. Dev Med Child Neurol. 1999;41:153-158.
110 Starr EM, Berument SK, Tomlins M, et al. Brief report: autism in individuals with Down syndrome. J Autism Dev Disord. 2005;35:665-673.
111 Szymanski L, King BH. Summary of the practice parameters for the assessment and treatment of children, adolescents and adults with mental retardation and comorbid mental disorders. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychol. 1999;38:1606-1610.
112 Clinical practice guideline. Diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. American Academy of Pediatrics. Pediatrics. 2000;105:1158-1170.
113 American Academy of Pediatrics, Subcommittee on Attention-Deficit/Hyperactivity Disorder and Committee on Quality Improvement. Clinical Practice Guideline: Treatment of the school-aged child with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108:1033-1044.
114 Miller M, Fee VE, Jones CJ. Psychometric properties of ADHD rating scales among children with mental retardation. Res Dev Disabil. 2004;25:477-492.
115 Miller ML, Fee VE, Netterville AK. Psychometric properties of ADHD rating scales among children with mental retardation 1: Reliability. Res Dev Disabil. 2004;25:459-476.
116 Handen BL, McAuliffe S, Caro-Martinez L. Learning effects of methylphenidate in children with mental retardation. J Dev Phys Disabil. 1996;8:335-346.
117 Warburg M. Visual impairments in adult people with intellectual disability: Literature review. J Intellect Disabil Res. 2001;45:424-438.
118 Beckung E, Steffenberg U, Uvebrant P. Motor and sensory dysfunction in children with mental retardation and epilepsy. Seizure. 1997;6(1):43-50.
119 Murphy NA, Young P. Sexuality in children and adolescents with disabilities. Dev Med Child Neurol. 2005;47:640-644.
120 Murphy NA, Elias ER. AAP Committee/Section on Children with Disabilities: Sexuality of children and adolescents with developmental disabilities. Pediatrics. 2006;118:398-403.
121 Sterilization of minors with developmental disabilities. American Academy of Pediatrics. Committee on Bioethics. Pediatrics. 1999;104:337-340.
122 Diekema DS. Involuntary sterilization of persons with mental retardation: An ethical analysis. Ment Retard Dev Disabil Res Rev. 2003;9:21-26.
123 Blum RW. Sexual health contraceptive need of adolescents with chronic conditions. Arch Pediatr Adolesc Med. 1997;151:290-297.
124 Ramey CT, Bryan DM, Wasik BH, et al. Infant health and development for low birth weight premature infants: Program elements, family participation and child intelligence. Pediatrics. 1992;89:454-465.
125 Bailey DB, Hebbeler K, Scarborough A, et al. First experience with early intervention: A national perspective. Pediatrics. 2004;113:887-896.
126 Reiff MI. Comparison of IDEA 1997 and 2004. AAP Section on Developmental and Behavioral Pediatrics Newsletter (Autumn). 2005:15-17.
126a Williamson P, McLeskey J, Hoppey D, Rentz T. Educating students with mental retardation in general education classrooms. Exceptional Children. 2006;72:347-361.
127 McPherson M, Weissman G, Strickland BB, et al. Implementing community-based systems of services for children and youths with special health care needs: How well are we doing? Pediatrics. 2004;113:1538-1544.
128 Johnson CP, Blasco PA. Community resources for children with special healthcare needs. Pediatr Ann. 1997;26:11-16.
129 Taanik A, Syrjala L, Kokkonen J, et al. Coping of parents with physically and intellectually disabled children. Child Care Health Dev. 2002;28:73-86.
130 Liptak GS, Revell GM. Community physician’s role in case management of children with chronic illness. Pediatrics. 1989;84:465-471.
131 Rosenbaum P, Stewart D. Alternative and complementary therapies for children and youth with disabilities. Infants Young Child. 2002;14(1):51-59.
132 Parish SL, Pomeranz-Essley A, Braddock D. Family support in the United States: Financing trends and emerging initiatives. Ment Retard. 2003;41:174-187.
133 Any Baby Can. The Survey of Health Care Experiences of Family of Children with Special Health Care Needs. Austin, TX: Any Baby Can, 1994.
134 Any Baby Can. The Survey of Health Care Experiences of Family of Children with Special Health Care Needs. Austin, TX: Any Baby Can, 1999.
135 American Academy of Pediatrics, Committee on Children with Disabilities. Why Supplemental Security Income is important for children and adolescents. Pediatrics. 1995;95:603-609.
136 American Academy of Pediatrics, Committee on Children with Disabilities. The continued importance of Supplemental Security Income for children and adolescents with disabilities. Pediatrics. 2001;107:790-793.
137 Agosta J, Melda K. Supporting families who provide care at home for children with disabilities. Except Child. 1995;62:271-282.
138 Johnson CP. Camping options for children with disabilities. Pediatr News Updates. 1997;5:8-10.
139 Orth T. Teaching anyone how to cook for themselves. Except Parent. 2003;33(2):30-34.
140 Schalock RL, Stark JA, Snell ME, et al. The changing conception of mental retardation: Implication for the field. Ment Retard. 1994;32:181-193.
141 Brunetti FL. Estate planning: Getting started. Excep Parent. 1995;25(12):41-44.
142 Brunetti FL. Estate planning: Trusts for children with disabilities. Except Parent. 1996;26(12):50-51.
143 Stoneman Z. Siblings of children with disabilities: Research themes. Ment Retard. 2005;43:339-350.
144 Cleveland D, Miller C. Attitudes and life commitments of older siblings of mentally retarded adults: An exploratory study. Ment Retard. 1977;15:38-41.
145 Hannah ME, Midlarsky E. Helping by siblings of children with mental retardation. Am J Ment Retard. 2005;110(2):87-99.
146 Hannah ME, Midlarsky E. Competence and adjustment of siblings of children with mental retardation. Am J Ment Retard. 1999;104(1):22-37.
147 Stoneman Z. Supporting positive sibling relationships during childhood. Ment Retard Dev Disabil Res Rev. 2001;7:134-142.
148 Neely-Barnes S, Marcenko M. Predicting impact of childhood disability on families: Results from the 1995 National Health Interview Survey Disability Supplement. Ment Retard. 2004;42:284-293.
149 Accardo PM, Capute AJ. Mental retardation. In: Capute AJ, Accardo PM, editors. Developmental Disabilities in Infancy and Childhood. Baltimore: Paul Brookes; 1996:211.
150 O’Brien G. Adult outcome of childhood learning disability. Dev Med Child Neurol. 2001;43:634-638.